Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Dental Journal
versión On-line ISSN 0375-1562
versión impresa ISSN 0011-8516
S. Afr. dent. j. vol.78 no.3 Johannesburg abr. 2023
RESEARCH
The marginal gap and internal fit of monolithic crowns milled with different luting spaces
AI Swaid
BDS, MScDent; Department of Oral Rehabilitation, School of Oral Health Science, Faculty of Health Sciences, University of the Witwatersrand. Currently Head, Department of Fixed Prosthodontics, Faculty of Dentistry, Alasmarya University in Zliten, Libya. ORCID: 0000-0002-9481-6232
ABSTRACT
INTRODUCTION: Three of the more promising materials for CAD/CAM restorations are Zirconia (VITA Zahnfabrik, Germany), Enamic (VITA Zahnfabrik, Germany), and the composite material Brilliant Crios (Coltene, Switzerland). Zirconia has been tested for the marginal gap and internal fit; Enamic and Crios have not been tested for marginal gap and internal fit and no studies have tested the effect of different luting spaces
METHOD: A standardised crown preparation on a typodont mandibular first molar tooth was scanned and imaged (CEREC CAD/ CAM, Germany). The marginal gap was measured using a Reflex microscope in both two- and three-dimensions. The internal fit was calculated using the properties of the luting agent and the surface area of the preparation
RESULTS: The 3D measurements were significantly higher, but only on average 10µm higher. The marginal gaps of the crowns milled with a 200µm luting space were significantly smaller than for those milled with a 100µm luting space. The smallest mean gap was recorded by Enamic at 31.7µm followed by Crios at 32.5µm, and Zirconia at 33.1µm. All of these measurements are well within acceptable clinical limits
CONCLUSIONS: All crowns milled, regardless of the luting space used, provided excellent marginal and internal fit, well within clinically acceptable parameters. The 3D measurements are more clinically relevant than 2D measurements. The smallest marginal gaps were found in the crowns milled with a 200pm luting space. However, this can present problems with non-axial seating and so it may be advisable to use the 100pm luting space parameter
Keywords: Marginal gap; Internal fit; CAD/CAM full coverage crowns;
INTRODUCTION
If the fit of a full crown is not accurate, there will be a marginal discrepancy which can lead to cement dissolution and microleakage,1 pulpal involvement,2 retention of plaque,3 changes in the composition of the subgingival microflora4 promoting the onset of periodontal disease.5
A marginal gap has been defined as "the vertical dimension from the finish line of the preparation to the cervical margin of the restoration".6 The internal fit is the internal gap that is the misfit of the crown at the occlusal / incisal and axial surfaces.6 The luting space which represent the internal fit should be uniform in thickness to facilitate cementation without defects in retention and resistance.7,8
Acceptable marginal gaps have been reported as between 7 to 65µm9 and between 50pm and 180µm.10,11 Most researchers agree that marginal gaps below 120pm are clinically acceptable.12-16 The creation of a space between the dental crown and the abutment which represent the internal fit, is clinically important to ensure the proper cementation of crowns and to permit the interposition of an equal thickness layer of dental cement.
Many studies have been measured the marginal gap and internal fit of all ceramic restorations. The mean marginal gap of Nobel Procera zirconia crowns was reported to be between 52µm and 74µm,17 and of those from a commercial laboratory, 44.2µm.18 In a study of lithium disilicate based glass ceramic material using both CAD/ CAM and heat pressed methods, the mean marginal gap was 132.2pm for CAD/CAM and 130.2pm for the heat-pressed group.19 Anadioti (2014) reported that the marginal gap of lithium disilicate crowns was below 90pm.20 In a study in which crowns were fabricated using Cerec3 CAD/ CAM, the marginal gap ranged from 53 to 67pm and the internal fit was within a range of 116 to 162µm.21
The following techniques for the measurement of the marginal gap of either copings or crowns have been reported in the literature:
• Use of an optical microscope with image processing software at magnification of 240 times and measurements selected randomly at a varying number of points.22-27
• Measured at four points (buccocentral, linguocentral, mesiocentral, and distocentral) using a profile projector and the distance between the two points measured by the computer21 or non-destructively using profilometry.28
• Use of a microscope avarying magnifications and usually four landmarks mesial, distal, buccal, and palatal.19,29,30
• Use of a silicone replica technique by luting the crown with a low-viscosity impression material which is subsequently stabilised with a high viscosity material in order to make sections (this method is also used to measure internal fit 18,21,31,32-37
• By luting the crown with dental cement such as zinc phosphate cement38 or chemically cured composite39 or glass-ionomer.29 The crown and die are embedded in epoxy resin and sectioned and the cement layer thickness measured with a three-dimensional microscope.29,32,38,40,41 and image analysis42 and/or scanning electron microscopy. 29,39,43 Measurement has also recently been carried out by microCT.34,44,45
• By digitising the intaglio surface of the crowns and master preparation and merging these images in best-fitting alignment, and then measuring the difference at specific points;20 or by laser videography to digitise the surfaces.17
Gassino et al,. (2004),46 determined that in order to accurately assess the marginal gap,20 measurements spread evenly around the circumference of the preparation were required.
The internal fit of dental crowns has been measured by similar methods, for example:
• As stated above, combined high and low viscosity silicone is sectioned and the thickness of the low viscosity material measured either directly or by the use of photographs
• Similarly, the cementation techniques mentioned above can be used to measure the internal fit
• A measurement of the total internal fit, rather than at specific points, has been made by luting the crown with a low viscosity silicone, and then using the weight and density of that silicone to relate this to the surface area of the preparation.47
The advent of CAD/CAM restorations over the last few decades has resulted in the development of a variety of new materials for the use of full coverage crowns, and whilst many materials have been tested for internal fit and marginal gap, some of the more recent materials do not appear to have been tested. Different manufacturers have recommended different luting gaps and there appears to be no consistency in this.48
Whilst zirconia has been tested for marginal gap and internal fit, the only study to determine the overall fit using a luting agent, was not carried out using zirconia. Enamic, an interpenetrating network ceramic, Brilliant Crios, a composite, have not been tested for marginal gap and internal fit. Therefore, the purpose of this study was to compare the marginal gap and total internal fit of single CAD/ CAM created crowns using Enamic (Vita, Austria), Zirconia (Vita, Austria), and Brilliant Crios (Coltene, Switzerland).
METHODS AND MATERIALS
Tooth Preparation
An acrylic resin typodont mandibular first molar resin tooth was prepared to produce a standardised crown preparation with a total convergence angle of 12 degrees, (as measured digitally from the scanned image) internally rounded shoulder margins of 1.5mm circumferentially, and an occlusal reduction of 1.5mm. All line angles were rounded (Fig 1).
Scanning and milling
The preparation was scanned and imaged with the Omnicam intra-oral scanner (Dentsply Sirona, Germany). The scanned file was used to determine the total surface area of the preparation using FEA software (Solidworks® Dassualt Systèmes Solidworks Corp. Massachusetts, USA). A crown with a flat occlusal surface was designed (Fig. 2) and the same design was used for all crowns. This was so that a constant load could be placed on the crown with a 3kg weight in an axial direction. The crowns were milled with either a luting space of 100μm or 200μm. The MC X5 milling machine (Dentsply/Sirona, Germany) was used to mill all crowns. The materials used were Enamic (Vita, Austria), Zirconia (Vita, Austria), and Brilliant Crios (Coltene, Switzerland).
Statistical Analysis and Sample Size
Marginal gaps of greater than 120μm would be considered the limit of clinical acceptability. Given an expected mean marginal gap of 110μm for any group, and aiming to detect a difference of more than 20% from this, given a within-group relative standard deviation of 22% (which corresponds to an effect size of d = 0.83), 80% power and the 5% significance level, a total sample size of 24, i.e. 4 per group, would be required.49 It was decided, however, to use 5 per group as the expected mean gap may differ from the above. In addition, the milling of 5 crowns would not affect the wear of the burs and therefore this would not be a confounding factor.
Categorical variables were summarised and illustrated by means of bar charts. Continuous variables were summarised by the mean, standard deviation, median and interquartile range, and their distribution illustrated by means of histograms. The effect of material and internal space on the marginal gap required a two-way Analysis of Variance (ANOVA) with the mean marginal gap measured at 20 points around the circumference of the preparation as the dependent variable,46 and material (Zirconia/ Brilliant Crios/ Enamic) and internal space difference (200μm and 100μm), and their interaction, as the independent variables. Outliers were removed, or data transformations were applied as necessary. Post-hoc tests were carried out to determine the material-luting space combinations which had the smallest values for the outcomes. The Tukey-Kramer adjustment for unequal group sizes (to allow for the deletion of outliers) was used, and effect sizes were expressed using Cohen's kappa. Comparison of the marginal gap between matching 2D and 3D measurements (for without-silicone and with-silicone measurements) was done using the paired samples t-test. The proportion of crowns which failed to meet the marginal gap limit of 120μm were to be compared between groups using Fisher's exact test. Test-retest reliability for the continuous outcomes was determined using the Intra-class Correlation Coefficient (ICC). Test-retest reliability for whether or not the marginal gap exceeded 120μm was determined by Cohen's kappa. Data analysis was carried out using SAS version 9.4 for Windows. The 5% significance level was used.
Marginal Gap Measurement
The crowns were first seated onto the master preparation without cementation and the marginal gap (if any) was measured using a Reflex Microscope (Reflex Measurement Ltd., Cambridge, UK), which measures in three dimensions to an accuracy of 4μm. The marginal gap was measured at 20 equi-distant points around the circumference of the crown. Each point was marked 1mm below the margin of the preparation with a bur.
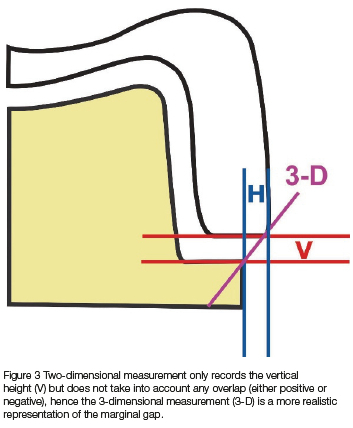
Each crown in turn was filled with light-body polyvinyl siloxane impression material (Express, 3MESPE, Germany), and seated onto the prepared tooth under a constant load for 10 minutes, using a 3kg weight placed on the flat occlusal surface of the crown. After setting, the excess material was removed from the circumference of the crown using a scalpel blade. The marginal gap was then measured using the same 20 measuring points, with the reflex microscope. Because the reflex microscope measures in 3 dimensions, the data points are manipulated in the software to provide measurements in both 2 and 3 dimensions (Fig 3).
Total Internal Fit Measurement
The silicone film was removed and weighed using an electronic scale to calculate its weight. The overall thickness of the silicone represented the total internal gap, calculated using the following equation after Grey et al (1993): 47
Thickness (internal gap) = weight/((surface area x density)
The surface area of the preparation was 183.84mm2 using a stereolithography generated mesh. The density of the 3M light-body polyvinyl siloxane impression material is 1.29g/ml.
RESULTS
Measurement consistency
During initial training in the use of the reflex microscope, it was observed that the researcher had some difficulty with locating the virtual point of light, especially on the z-axis, and so the entire experiment was repeated 3 times on 3 different occasions, in order to assess measurement consistency.
The averaged marginal gap measurements from two of the occasions that had the highest reliability across all the outcomes were used for further analysis. The average within-group relative standard deviation for the marginal gap outcomes (4.0%) was considerably lower (5.5 times) than the relative standard deviation of 22% used in the sample size calculations, confirming the validity of the sample size and the power of the analyses. There was excellent agreement between the three internal fit measurements on all occasions.
Two-dimensional measurements of the marginal gap
Table 1 shows the 2D measurements of the three different materials with and without silicone.
Statistically significantly differences were found between the materials both without (p < 0.0031) and with (p = 0.0008) silicone. The marginal gaps when no silicone was applied between the three materials were statistically significantly different (p < 0.0031), as it was with the silicone (p = 0.0008). In addition, the marginal gap between the three materials was significantly smaller (p < 0.0001 with no silicone, p = 0.0028 with silicone) when the luting space of 200µm was used, compared with 100µm. With the silicone, Crios 200µm and Zirconia 200µm had the smallest marginal gaps compared with all the other experimental combinations.
Three-dimensional measurements of the marginal gap
Table 2 shows the 3D measurements of the three different materials with and without silicone.
There were no statistically significant differences in the marginal gaps between the three materials with and without silicone (p = 0.43 without silicon, p = 0.55 with silicone). The marginal gaps both with and without silicone were significantly smaller (P < 0.0001) when the luting space of 200pm was compared with 100pm. There were no significant interactions (p = 0.60 without silicone, p = 0.83 with silicone) between the materials and the luting space. All three materials at 20pm had the smallest marginal gap compared with the other experimental combinations.
Internal Fit
Table 3 shows the internal fit measurements of the three different materials at the 100 and 200pm milled spaces.
Post-hoc tests revealed that the mean internal fit was significantly higher for the 200pm luting space than for the 100pm luting space for each material. For the 100pm experiments, the mean fit for Zirconia was significantly higher than that for Crios and Enamic. Crios 100pm and Enamic 100pm had the smallest internal fit compared to all the other experimental combinations.
Comparison of matching 2D and 3D measurements
When measuring the marginal gap with no silicone, the 3D measurements were an average of 10.9pm higher than the corresponding 2D measurements (95% confidence interval: 0.0103-0.0114mm; p < 0.0001). With silicone, the 3D measurements were an average of 10pm higher than the corresponding 2D measurements (95% confidence interval: 0.0093-0.0107 mm; p<0.0001).
DISCUSSION
This is the first study to compare the marginal gap and internal fit of CAD/CAM full coverage crowns measured in two and three dimensions, and using different luting spaces (100μm and 200μm).
Marginal Gap
It is generally accepted that a marginal gap of less than 120μm is clinically acceptable but a large variety of values for marginal gaps has been reported. The present study used a three-dimensional measurement method, and the differences between the 2D and 3D measurements were statistically significant, being on average 10μm higher for the 3D measurements. This is therefore a more accurate indication of the amount of luting material to be found at the margin after cementation.
Measuring the marginal gap of cemented or un-cemented crowns can influence the results of the measurement. 50-53 Marginal gap measurements generally increase following cementation;54,55 and the medium for cementing the crown might not facilitate complete seating, resulting in an inadequately closed margin.56 In the current study, all the measurements that were conducted on the specimens cemented with silicone were higher than those cemented without silicone.
The average 2D marginal gap without silicone was 24.7μm for the 100μm luting space, and 20μm for the 200μm luting space. After luting with silicone the average was 27.5μm for the 100μm luting space (a difference of 2.8μm), and 26.2μm for the 200μm luting space (a difference of 6.2μm).
The average 3D marginal gap without silicone was 37.5μm for the 100μm luting space, and 32.5μm for the 200μm luting space. The averages after luting with silicone were 37.9μm for the 100μm luting space (a difference of 0.4μm), and 36.2μm for the 200μm luting space (a difference of 3.7μm).
Although there were differences between the materials in these measurements, all the marginal gaps were well within the clinically acceptable limits.
Internal Fit
An acceptable practical guide for cement films has been suggested as being between 50 and 100μm.57 Many previous studies have not been carried out on milled crowns, and the luting space used has been somewhat arbitrary, using methods such as painting die-spacer on dies to be used for cast restorations. In CAD/CAM, however, the luting space can be defined and is dependent on the milling parameters set in the software. Therefore, this study set out to determine any relationship between the luting space and the marginal gap.
Although internal fit is thought not to be as clinically relevant as the marginal fit, 5,53 it is of importance as it affects the resilience of the crown.34 The proper internal fit of the crown is also critical as it enables the seating of the crown while allowing for both retention and resistance.24 In addition, cementation techniques such as uncontrolled finger pressure or overfilling of the crown with cement, might lead to an uneven flow of cement with one axial wall having a thick film and the opposite wall having a thin film.58 It has also recently been shown that with a larger internal luting space it is possible to seat the crown off-axis, resulting in a wider marginal gap on one side of the crown.59
For the 100μm luting space the smallest internal fit was recorded by Crios at 1.2μm followed by Enamic 1.3μm, and Zirconia at 1.6μm. For the 200μm luting space the internal fit of the three materials was at the same value of 2.1μm. All of these measurements are well within acceptable clinical limits.
The results in this study showed that all marginal gaps were clinically acceptable, and in light of the danger of incorrect seating of the crown at the 200μm luting space,59 it may be advisable to mill at a 100μm luting space for full crowns.
5.3. Limitations
This study used only three materials, but these were considered representative of crowns with different hardness, as this might affect the milling precision. The use of the reflex microscope held some challenges for the researcher, as it requires precise binocular vision. However, by repeating the measurements three times, sufficient reliability was obtained, and this should become a standard procedure when using measuring instruments of this precision. Finally, the cementing medium was a proxy for actual luting cements, and therefore the results may not apply to different luting cements, which should be the subject of further study. In addition, the milling parameters of different CAD/CAM systems may influence the marginal gap as one study did find a difference between the two systems tested. 60
CONCLUSION
Within the limitations of this study, all crowns milled, regardless of the luting space used, provided excellent marginal and internal fit, well within clinically acceptable parameters. The 3D measurements are more clinically relevant than 2D measurements and were always significantly larger, but on average only by an additional 10 μm. The smallest marginal gaps were found in the crowns milled with a 200 μm luting space, however this can present problems with non-axial seating and so it may be advisable to use the 100 μm luting space parameter.
ACKNOWLEDGMENTS
I am grateful to Prof CP Owen for his support and encouragement.
REFERENCES
1. Jacobs MS, Windeler AS. An Investigation of Dental Luting Cement Solubility as a Function of the Marginal Gap. J Prosthet Dent. 1991; 65: 436-442. [ Links ]
2. Goldman M, Laosonthorn P, White RR. Microleakage - Full Crowns and the Dental Pulp. J Endo. 1992; 18: 473-475. [ Links ]
3. Valderhaug J, Heloe LA. Oral Hygiene in a Group of Supervised Patients with Fixed Prostheses. J periodontal. 1977; 48: 221-224. [ Links ]
4. Lang NP, Kiel RA, Anderhalden K. Clinical and Microbiological Effects of Subgingival Restorations with Overhanging or Clinical Perfect Margins. J Clin Periodontol. 1983; 10: 563-578. [ Links ]
5. Felton DA, Kanoy BE, Bayne SC, Wirthman GP. Effect of in Vivo Crown Margin Discrepancies on Periodontal Health. J Prosthet Dent. 1991; 65: 357-364. [ Links ]
6. Kokubo Y, Tsumita M, Kano T, Sakurai S, Fukushima S. Clinical marginal and internal gaps of zirconia all-ceramic crowns. J Prosthodont Res. 2011; 55: 40-43. [ Links ]
7. Tuntiprawon M, Wilson PR. The Effect of Cement Thickness on the Fracture Strength of All-Ceramic Crowns. Aust Dent J. 1995; 40: 17-21. [ Links ]
8. Naert I, Van der Donck A, Beckers L. Precision of Fit and Clinical Evaluation of All-Ceramic Full Restorations Followed Between 0.5 and 5 Years. J Oral Rehabil. 2005; 32: 51- 57. [ Links ]
9. Lofstrom LH, Barakat MM. Scanning electron microscopic evaluation of clinically cemented cast gold restorations. J Prosthet Dent. 1989; 61: 664-9. [ Links ]
10. Coli P, Karlsson S. Fit of a New Pressure-Sintered Zirconium Dioxide Coping. Int J Prosthodont. 2004; 17: 59-64. [ Links ]
11. Chan C, Haraszthy G, Geis-Gerstorfer J, Weber H, Huettemann H. Scanning electron microscopic studies of the marginal fit of three esthetic crowns. Quintessence Int. 1989; 20: 189-93. [ Links ]
12. Mclean JW, Von Fraunhofer JA. The Estimation of Cement Film Thickness by an in Vivo Technique. Br Dent J. 1971; 131: 107-111. [ Links ]
13. Belser UC, MacEntee MI, Richter WA. Fit of Three Porcelain- Fused-to-Metal Marginal Designs in Vivo: A Scanning Electron Microscope Study. J Prosthet Dent. 1985; 53: 24-29. [ Links ]
14. Weaver JD, Johnson GH, Bales DJ. Marginal Adaptation of Castable Ceramic Crowns and Metal Ceramic Crowns. J Prosthet Dent. 1991; 66: 747-753. [ Links ]
15. Karlsson S. The fit of Procera titanium crowns. An in vitro and clinical study. Acta Odontol Scand. 1993 Jun;51(3):129-134. [ Links ]
16. Fonseca JC, Henriques GE, Sobrinho LC, de Góes MF. Stress-relieving and porcelain firing cycle influence on marginal fit of commercially pure titanium and titanium-aluminum-vanadium copings. Dent Mater. 2003; 19: 686-691. [ Links ]
17. May KB, Russel MM, Razzog ME, Lang BR. Precision of Fit: The Procera AllCeram Crown. J Prosthet Dent. 1998; 80: 394-404. [ Links ]
18. Kokubo Y, Tsumita M, Kano T, Sakurai S, Fukushima S. Clinical Marginal and Internal Gaps of Zirconia All-Ceramic Crowns. J Prosthodont. 2010; 55: 40-43. [ Links ]
19. Akin A, Toksavul S, Toman M. Clinical Marginal and Internal Adaptation of Maxillary Anterior Single All-Ceramic Crowns and 2-year Randomized Controlled Clinical Trial. J Prosthodont. 2014; 24: 345-350. [ Links ]
20. Anadioti E, Aquilino SA, Gratton DG, Holloway JA, Denry I, Thomas GW, et al. 3D and 2D Marginal Fit of Pressed and CAD/CAM Lithium Disilicate Crowns Made from Digital and Conventional Impressions. J Prosthodont. 2014; 23: 610-617. [ Links ]
21. Nakamura T, Dei N, Kojima T, Wakabayashi K. Marginal and Internal Fit of Cerec 3 CAD/CAM All-Ceramic Crowns. Int J Prosthodont. 2003; 16(3):244-248. [ Links ]
22. Yeo IS, Yang JH, Lee JB. In Vitro Marginal Fit of Three All-Ceramic Crown Systems. J Prosthet Dent. 2003; 90: 459-46. [ Links ]
23. Akbar JH, Petrie CS, Walker MP, Williams K, Eick D. Marginal Adaptation of Cerec 3 CAD/CAM Composite Crowns Using Two Different Finish Line Preparation Designs. J Prosthodont. 2006; 15: 155-163. [ Links ]
24. Beuer F, Aggstaller H, Richter J, Edelhoff D, Gernet W. Influence of Preparation Angle on Marginal and Internal Fit of CAD/CAM-Fabricated Zirconia Crown Copings. Quintessence Int. 2009; 40: 243-250. [ Links ]
25. Alghazzawi TA, Liu PR, Essig ME. The Effect of Different Fabrication Steps on the Marginal Adaptation of Two Types of Glass-Infiltrated Ceramic Crown Copings Fabricated by CAD/CAM Technology. J Prosthodont. 2011; 21: 167-172. [ Links ]
26. Grenade C, Mainjot A, Vanheusden A. Fit of Single Tooth Zirconia Copings. Comparison between Various Manufacturing Processes. J Prosthet Dent. 2011; 105: 249-255. [ Links ]
27. Rajan BN, Jayaraman S, Kandhasamy B, Rajakumaran I. Evaluation of Marginal Fit and Internal Adaptation of Zirconia Copings Fabricated by Two CAD-CAM Systems: An in Vitro Study. J Indian Prosthodont Soc. 2015; 15:173. [ Links ]
28. Mitchell CA, Pintado MR, Douglas WH. Nondestructive, in Vitro Quantification of Crown Margins. J Prosthet Dent. 2011; 85: 575-584. [ Links ]
29. Biscaro L, Bonfiglioli R, Soattin M, Vigolo P. An in Vivo Evaluation of Fit of Zirconium- Oxide Based Ceramic, Single Crowns, Generated with Two CAD/CAM Systems, in Comparison to Metal Ceramic Single Crowns. J Prosthodont. 2013; 22: 26-41. [ Links ]
30. Johnson R, Verrett R, Haney S, Mansueto M, Challa S. Marginal Gap of Milled versus Cast Gold Restorations. J Prosthodont. 2015; 26: 56-63. [ Links ]
31. Kokubo Y, Nagayama Y, Tsumita M, Ohkubo C, Fukushima S, Steyern PV.Clinical Marginal and Internal Gaps of In-Ceram Crowns Fabricated Using the GN-I System. J Oral Rehabil. 2005; 32) :753-758. [ Links ]
32. Tsitrou EA, Northeast SE, Noort RV. Evaluation of the Marginal Fit of Three Margin Designs of Resin Composite Crowns Using CAD/CAM. J Dent. 2006; 35: 68-73. [ Links ]
33. Lee KP, Park, CW, Kim KH, Kwon TY 2008. Marginal and Internal Fit of All-Ceramic Crowns Fabricated with Two Different CAD/CAM Systems. D Material J. 2008; 27: 422-426. [ Links ]
34. Rungruanganunt P, Kelly JR, Adams DJ. Two Imaging Techniques For 3D Quantification of Pre-Cementation Space for CAD/CAM Crowns. J Dent. 2010; 38): 995-1000. [ Links ]
35. Moldovan O, Luthardt RG, Corcodel N, Rudolph H. Three-dimensional fit of CAD/ CAM-made zirconia copings. Dent Mater. 2011; 27: 1273-8 [ Links ]
36. Cardelli P, Scotti R, Monaco C. Clinical Fitting of CAD/CAM Zirconia Single Crowns Generated from Digital Intraoral Impressions Based on Active Wavefront Sampling. J Dent. 2011; 1783: 1-8. [ Links ]
37. Anunmana, C., Charoenchitt, M., Asvanund C. Gap Comparison between Single Substructures and Three-Unit Bridge Zirconia. J Adv Prosthodont, 2014; 6: 253258. [ Links ]
38. Han HS, Yang HS, Lim HP, Park YJ, 2011. Marginal Accuracy and Internal Fit of Machine-Milled and Cast Titanium Crowns. J Prosthet Dent. 2011; 106: 191-197. [ Links ]
39. Bindl A, Mormann H. Marginal and Internal Fit of All Ceramic CAD/CAM Crown Copings on Chamfer Preparations. J Oral Rehabil. 2004; 32: 4441-447. [ Links ]
40. Souza RO, Ozcan M, Pavanelli CA, Buso L, Lombardo GHL, Michida SMA, et al. Marginal and Internal Discrepancies Related to Margin Design of Ceramic Crowns Fabricated by a CAD/CAM System. JOP. 2012; 21: 94-100. [ Links ]
41. Sachs C, Groesser J, Stadelmann M, Schweiger J, Erdelt K, Beuer F. Full-Arch Prosthesis from Translucent Zirconia: Accuracy of Fit. Dent Mater J.2014; 30: 817823. [ Links ]
42. Mou SH, Chai T, Wang JS, Shiau YY Influence of Different Convergence Angles and Tooth Preparation Heights on the Internal Adaptation of Cerec Crowns. J Prosthet Dent. 2002; 87: 248-55. [ Links ]
43. Vigolo P, Mutinelli S, Biscaro L, Stellini E. An In Vivo Evaluation of the Fit of Zirconium-Oxide Based Ceramic, Single Crowns with Vertical and Horizontal Finish Line Preparations. J Prosthodont. 2015; 24: 603-609. [ Links ]
44. Seo D, Yi Y Roh B. The Effect of Preparation Designs on the Marginal and Internal Gaps in Cerec3 Partial Ceramic Crowns. J Dent. 2009; 37: 374-382. [ Links ]
45. Alfaro DP, Ruse ND, Carvalho RM, Wyatt CC. Assessment of the Internal Fit of Lithium Disilicate Crowns Using Micro-CT. J Prosthodont. 2014; 24: 381-386. [ Links ]
46. Gassino G, Monfrin SB, Scanu M, Spina G, Preti G. Marginal Adaptation of Fixed Prosthodontics. Int J Prosthodont. 2004; 17: 218-223. [ Links ]
47. Grey NJ, Piddock V Wilson MA. In-Vitro Comparison of Conventional Crowns and a New All-Ceramic System. J Dent. 1993; 21: 47-51. [ Links ]
48. Contrepois M, Soenen A, Bartala M, Laviole O. Marginal adaptation of ceramic crowns: a systematic review. J Prosthet Dent. 2013; 110: 447-454 [ Links ]
49. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. BRM. 2007; 39: 175-191. [ Links ]
50. Stappert C, Dai M, Chitmongkolsuk S, Gerds T, Strub JR. Marginal Adaptation of Three-Unit Fixed Partial Dentures Constructad from Pressed Ceramic Systems. Br Dent J. 2004; 196: 766-770. [ Links ]
51. Wolfart S, Wegner SM, Al-Halabi A, Kern M. Clinical Evaluation of Marginal Fit of a New Experimental All-Ceramic System Before and After Cementation. Int J Prosthodont. 2003; 16: 587-592. [ Links ]
52. Okutan M, Heydecke G, Butz F, Strub JR. Fracture Load and Marginal Fit of Shrinkage-Free ZrSiO4 All-Ceramic Crowns After Chewing Simulation. J Oral Rehabil. 2006; 33: 827-832. [ Links ]
53. Suarez MJ, Lozano JF, Salido MP, Martinez F. Marginal Fit of Titanium Metal-Ceramic Crowns. Int J Prosthodont. 2005; 18: 390-401. [ Links ]
54. Byrne G. Influence of Finish Line form on Crown Cementation. Int J Prosthodont. 1992; 5: 137-144. [ Links ]
55. Quintas AF, Oliveira F, Bottino MA. Vertical Marginal Discrepancy of Ceramic Copings with Different Ceramic Materials, Finish Lines, and Luting Agents: an in Vitro Evaluation. J Prosthet Dent. 2004; 92: 250-257. [ Links ]
56. Gu XH, Kern M. Marginal Discrepancies and Leakage of All-Ceramic Crowns: Influence of Luting Agents and Aging Conditions. Int J Prosthodont. 2003; 16: 109116. [ Links ]
57. Martins LM, Lorenzoni FC, Melo AO, Silva LM, Oliveira JL, Oliveira PC, Bonfante G. Internal fit of two all-ceramic systems and metal-ceramic crowns. J Appl Oral Sci. 2012; 20: 235-240. [ Links ]
58. Pilo R, Cardash HS. In Vivo Retrospective Study of Cement Thickness Under Crowns. J Prosthet Dent. 1998; 79: 621-625. [ Links ]
59. Babiolakis GB, Owen CP. The effect of off-axis seating on the marginal adaptation of full coverage all ceramic crowns. SADJ 2020; 75: 301-308 [ Links ]
60. Hamza TA, Ezzat HA, El-Hossaiy MM, Katamish HA, Shokry TE, Rosenstiel SF Accuracy of ceramic restorations made with two CAD/CAM systems. J Prosthet Dent. 2013;109: 83-7 [ Links ]
 Correspondence:
Correspondence:
Dr AI Swaid
Department of Fixed Prosthodontics Faculty of Dentistry Alasmarya University, Zliten,Libya
Email: abdulgaderswaid@yahoo.com; Mobile: 00218917317512














