Services on Demand
Journal
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Surgery
On-line version ISSN 2078-5151Print version ISSN 0038-2361
S. Afr. j. surg. vol.63 n.3 Cape Town 2025
https://doi.org/10.36303/SAJS.03375
SRS ABSTRACTS
Abstracts from the 52nd Meeting of the Surgical Research Society of South Africa
Held on the 19th to 20th June 2025 at the Double Tree by Hilton Hotels, Upper East Side and hosted by the Division of General Surgery, University of Cape Town
Usefulness of smart glasses for Lichtenstein open inguinal hernia repair skills training in junior surgical registrars: a pilot study
N Hazakis (Registrar), M Brand
University of Pretoria, South Africa
Introduction: Smart glasses offer an alternative teaching method compared to traditional surgical training methods. This pilot study compared whether they are a viable alternative with similar outcomes. A comparison between two teaching methods, for the same operation we identified a potentially novel teaching method in the South African setting. An open inguinal hernia Lichtenstein repair was taught under similar working conditions, with an objective assessment of the surgeon's practical skills and a subjective evaluation of their teaching experience. This pilot study indicates exciting opportunities in the future regarding surgical training and assessment methods.
Objectives: To compare the surgical proficiency of the experimental group with the control group using OCHRA (Observational Clinical Human Reliability Assessment) scores for Lichtenstein open inguinal hernia repair. Perceptions on the use of smart glasses vs traditional apprenticeship intra-operatively using Likert score-based questionnaires.
Methods: A comparative qualitative and quantitative experimental pilot study was conducted between surgical registrars at the university of Pretoria, who were taught using the traditional apprenticeship (control) model versus those using smart glasses (experimental). Two groups of five surgical registrars each were randomly assigned to either the traditional apprenticeship method or to the smart-glasses device method of teaching. Registrars were taught and performed open inguinal hernia repairs and assessed on their surgical technique using a standardised checklist; Observational Clinical Human Reliability Assessment (OCHRA) checklist. Qualitative questionnaires to assess the users perceptions as well as the validated checklist were used to assess the differences between the two groups.
Results: Registrars taught with smart glasses had comparable scores compared to those taught by a traditional method. Both groups had similar pre-operative experience and similar training based on their questionnaire responses. The perceived experiences of both groups were comparable.
Conclusion: The pilot study identified surgical smart glasses as a possible training and assessment tool for surgical registrars.
Role of 2-hydroxybutyrate in clinical inflammatory processes of pancreatic ductal adenocarcinoma cancer
N Elebo,1,2 EA Abdel-Shafy,2,3 JAO Omoshoro-Jones,1,4 S Cacciatore,2 EE Nweke1,5
1 Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, South Africa
2 Bioinformatics Unit, International Centre for Genetic Engineering and Biotechnology, South Africa
3 National Research Centre, South Africa
4 Hepatopancreatobiliary Unit, Department of Surgery, Chris Hani Baragwanath Academic Hospital, South Africa
5 Department of Life and Consumer Sciences, College of Agriculture and Environmental Sciences, University of South Africa, South Africa
Background: PDAC is characterised by metabolic alterations which can influence inflammation and evasion of the immune response. Therefore, understanding the mechanisms behind this is critical for identifying biomarkers for early detection and for developing new therapeutic strategies. 2-Hydroxybutyrate (HB) levels have been implicated in tracking β-cell dysfunction, lipid oxidation and heightened oxidative stress levels. This study sought to associate 2-HB levels with inflammatory processes and patient outcomes.
Methods: Upon ethics approval, we conducted an untargeted metabolomics study using Nuclear Magnetic Resonance spectroscopy on plasma obtained from consenting individuals (81 PDAC (57 Resectable PDAC, 15 Locally Advanced PDAC and 9 Metastatic PDAC), 6 Chronic Pancreatitis, and 6 healthy participants). Reactive oxygen species (ROS) levels were assessed using N, N- diethyl -para-phenylenediamine (DEPPD) sulphate. Wilcoxon and Kruskal-Wallis rank-sum test was used to compare differences between the controls and PDAC groups. The Spearman's correlation and Kaplan-Meier tests were conducted for correlation and survival analyses. P-value < 0.05 was considered significant.
Results: This study showed elevated levels of 2-HB (p = 0.004) and acetoacetate (p = 0.009) with worsening tumour stage. Patients were stratified into high and normal/low groups. The "high group" was selected by identifying the top 25% of PDAC patients with the highest levels of 2-HB. Consequently, patients with lower levels of 2-HB survived longer.
Conclusion: 2-HB levels were associated with patient survival in this cohort of patients, suggesting its potential role as a biomarker. Ongoing analyses seek to establish the potential role of 2-HB in influencing inflammation during tumour progression.
Enhanced Recovery After Trauma Surgery (ERATS): a randomised controlled trial
D McPherson, A Nicol, S Edu, P Navsaria
Trauma Center, Groote Schuur Hospital, University of Cape Town, South Africa
Background: Enhanced Recovery After Surgery (ERAS®) represents a patient-centred, evidence-driven paradigm in perioperative care and has been proven effective in elective surgical settings. The aim of this RCT was to investigate the effects of an early recovery program implemented in patients undergoing emergency laparotomy for trauma.
Methods: Hemodynamically stable patients who sustained penetrating abdominal wounds and underwent emergency laparotomy at Groote Schuur Hospital Trauma Centre were randomised to either the standard treatment group or the ERATS group between March 2018 and December 2022.
Results: We included 42 patients in the ERATS group (G1) (9.52% female, mean age 29.5 years, SD 7.8) and 45 patients in the standard protocol group (G2), (6.6% female, mean age 30.3 years, SD 9.0). There was no statistical difference regarding demographics as well as trauma scores (ISS, RTS, TRISS, PATI) and GCS between the groups. In both groups, the majority of patients sustained abdominal gunshot wounds (57.1% vs 60.0%). Intraoperative vital signs as well as blood loss were comparable between the groups. G1 showed significantly shorter duration to nasogastric tube removal (p = 0.014), to solid diet intake (p < 0.001), to urinary catheter removal (p < 0.001), time to flatus and time to stool (p < 0.001). The mean time to mobilisation (p = 0.213) as well as overall pain scoring postoperatively (p = 0.829) was comparable between G1 and G2. There was no statistical difference regarding postoperative mortality (p = 0.862) and reoperation rate (p > 0.99) between the groups. G1 showed a significantly reduced time to discharge compared to G2 (p = 0.002). We assessed a non-significantly higher re-admission rate in G2 (p = 0.222).
Conclusion: The modified ERATS protocol is safe, associated with certain clinical benefits, and provides a promising avenue for improved recovery and reduced hospital stays in trauma patients undergoing emergency laparotomy.
Non-cirrhotic hepatocellular carcinoma has a distinct metabolomic fingerprint in a sub-Saharan African cohort: Are we looking at a different disease?
S Sobnach,1 S Cacciatore,2 M Bernon,1 E Jonas,1 LF Zerbini2
1 Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
2 International Centre for Genetic Engineering and Biotechnology (ICGEB), South Africa
Background: Although non-cirrhotic hepatocellular carcinoma (NC-HCC) is common in sub-Saharan Africa (SSA), its disease biology remains poorly understood.
Aim: To investigate the disease profile and outcomes of cirrhotic HCC (C-HCC) and NC-HCC in a SSA cohort using a metabolomics approach.
Methodology: All patients diagnosed with HCC in the Surgical Gastroenterology Unit at Groote Schuur Hospital, Cape Town, South Africa were included in the study. Age and gender-matched healthy volunteers were recruited as controls. Using a standard protocol, blood samples were collected in heparinised tubes. Plasma samples were then analysed using a 500 MHz Bruker Advance III HD Nuclear Magnetic Resonance (NMR) spectrometer. A standard nuclear Overhauser effect spectroscopy pulse sequence was used to quantify the concentration of 37 metabolic parameters.
Results: We profiled the plasma metabolome of 31 patients (NC-HCC:16, C-HCC: 15); plasma from eight healthy volunteers served as controls. Cirrhotic HCC and NC-HCC are characterised by different levels of metabolic inflammatory parameters. The NMR inflammatory marker GlycA was significantly higher in the NC-HCC group (p = 0.0033, FDR = 0.0303). Histidine levels were significantly lower in the NC-HCC patients (p = 0.0045, FDR = 0.0303) which further support the presence of an inflammatory milieu. On the contrary, C-HCC patients had lower levels of proteins as measured by NMR spectroscopy (p = 0.0001, FDR 0.0062), suggesting lower albumins level in this group.
Conclusions: NC-HCC and C-HCC are two distinct diseases based on their NMR metabolomic profiles. NC-HCC is significantly associated with higher levels of inflammatory markers. This potentially explains its aggressiveness and poorly clinical outcomes in sub-Saharan Africa.
Virome restructuring in HIV-helminth co-infection reveals potential biomarkers for colorectal cancer in a South African cohort
BP Damane,1,2 TV Mulaudzi,1 P Naidoo,2,3 Z Dlamini,4 ZL Mkhize-Kwitshana3,5
1 Department of Surgery, Steve Biko Academic Hospital, University of Pretoria, South Africa
2 Department of Medical Microbiology, College of Health Sciences, School of Laboratory Medicine & Medical Sciences, Nelson R. Mandela School of Medicine, University of KwaZulu-Natal, South Africa
3 Division of Research Capacity Development, South African Medical Research Council (SAMRC), South Africa
4 SAMRC Precision Oncology Research Unit (PORU), DSTI/NRF SARChI Chair in Precision Oncology and Cancer Prevention (POCP), Pan Africa Cancer Research Institute (PACRI), University of Pretoria, South Africa
5 Biomedical Sciences Department; School of Life and Consumer Sciences, College of Agriculture and Environmental Sciences, University of South Africa, South Africa
Background: Colorectal cancer (CRC) in immunocompromised individuals, such as those co-infected with HIV and helminths, may be influenced by alterations in the gut virome. Identifying distinct viral biomarkers could enhance early CRC detection in such populations.
Aim: To characterise the gut microvirome composition across infection groups and identify viral taxa associated with CRC in HIV-helminth co-infected individuals.
Methods: This retrospective cross-sectional sub-study utilized stored stool samples from 62 consenting participants stratified into five groups: uninfected controls (n = 10), CRC-positive (n = 10), HIV-only (n = 14), helminth-only (n = 15), and HIV-helminth co-infected (n = 13). Samples were purposively selected based on infection status and data completeness. Viral DNA was extracted, sequenced, and analysed to determine viral diversity and taxonomic composition. Alpha and beta diversity indices were assessed using Kruskal-Wallis and Wilcoxon rank-sum tests. Co-occurrence network analysis was used to explore virome structure. Ethics approval was obtained from the UKZN Biomedical Research Ethics Committee (BREC/00005458/2023).
Results: Shannon diversity was significantly higher in CRC compared to healthy controls and helminth-only groups (p < 0.05). Beta diversity revealed significant clustering between CRC and HIV-helminth groups compared to controls (p < 2.2 × 10-16). The HIV-helminth group showed distinct viral profiles, including higher abundance of Podoviridae and Unclassified Caudovirales. A shared core virome of 26 OTUs was identified, while the HIV-helminth group exhibited unique taxa. Network analysis revealed hub viral genera (e.g., Myoviridae, CrAss-like viruses) central to co-infection-associated virome shifts.
Conclusion: HIV-helminth co-infection is associated with gut virome restructuring that mirrors viral profiles observed in CRC, suggesting convergent microbial alterations due to immune dysregulation. These shared viral signatures support the concept of an "onco-microvirome" and may serve as non-invasive biomarkers for early CRC risk in these populations.
Presentation, treatment and long-term outcomes of hepatocellular carcinoma in patients with and without HIV: a comparative observational cohort study
I Kim, E Jonas, M Bernon, M Emmamally, S Sobnach
Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa
Background: There are limited data detailing the outcomes of hepatocellular carcinoma (HCC) in patients with human immunodeficiency virus, particularly in sub-Saharan Africa (SSA).
Aim: This study explores the epidemiology, treatment and outcomes of HCC in a SSA cohort, comparing patients with and without HIV.
Methodology: A retrospective cohort study of patients treated for HCC from 1 February 2011 to 29 February 2024 at Groote Schuur Hospital, South Africa was performed.
Results: Of the 501 HCC patients, 75 (15.0 %) were people living with HIV (PLWH). The PLWH were younger (43.7 ± 9.7 vs. 52.9 ± 15.3 years, p < 0.00001), had more frequent chronic hepatitis B virus (HBV) co-infection (85.3 % vs. 51.6 %, p < 0.00001) and no hepatitis C virus co-infection (0 % vs. 6.8 %, p = 0.013). More PLWH presented with Barcelona Clinic Liver Cancer Stage D disease (43.6 % vs. 27.7 %, p = 0.007). Similar proportions of PLWH and HIV-negative patients received curative-intended treatments, life-prolonging therapies and best supportive care. In PLWH, the median survival was lower (44 [IQR: 16-163.7] vs. 78 [IQR: 26-191] days, p = 0.010), and patients with HIV-HBV co-infection had the lowest survival (39 [IQR: 14.7-155.2] days).
Conclusion: In a SSA HCC cohort, patients with HIV were significantly younger, had more advanced disease and HBV co-infection resulted in the lowest survival. Earlier detection through aggressive HCC screening is key to improving outcomes in PLWH.
Outcomes after damage control laparotomy ("clip-and-drop" surgery) compared to primary surgery in neonatal necrotizing enterocolitis
A Bin Hidarah, M Arnold, A Mbonisweni
Division of Pediatric Surgery, Red Cross War Memorial Children's Hospital, University of Cape Town, South Africa
Background: Damage control laparotomy ("Clip-and-drop" surgery, "C&D") instead of primary surgery (PS) in Necrotizing Enterocolitis (NEC) may facilitate survival and primary anastomosis after stabilisation but outcomes are poorly documented.
Aim: To assess mortality and morbidity after C&D for NEC.
Methods: A retrospective medical record review of all patients with NEC undergoing bowel resection at a free-standing tertiary paediatric surgical centre [Red Cross War Memorial Children's Hospital; Cape Town], between 01.01.2015 and 31.12.2022, compared C&D to PS. Inclusion criteria: laparotomy for NEC. Exclusion criteria: Incomplete records, > 44 weeks gestation, no bowel resection. Descriptive statistics (Excel, Microsoft® 2010) and comparative statistics (SPSS® v30, IBM 2024:Mann-Whitney U, Chi2, odds ratio) determined statistical significance if alpha < 0.05 with 95% confidence interval. Ethics committee approval: UCT HREC (217/2024).
Result: Out of 144 patients operated for NEC, 35/103 (34%) had C+D and 67/102 (65%) had PS. Forty-two were excluded (missing data, wrong diagnosis, no bowel resection, or pan-intestinal necrosis). Definitive surgery was similar (p = 0.3) for survivors with mostly stoma formation [C+D 21/35 (77%) vs PS 44/67 (65%)] and primary anastomosis [C+D 6/35 (22%) vs PS 23/66 (34%)] despite higher baseline serum lactate at index procedure in C&D (mean 4.6 vs 2.5, p = 0.009). Mortality was higher in C+D [30-day: 11/35 (31%) versus PS,10/67 (14%); p = 0.1; 6-month:18/35 (48%) vs P,15/67 (22%); p = 0.001].
Conclusion: Despite high mortality associated with poorer baseline physiology, C&D survivors had comparatively good outcomes, with similar subsequent primary anastomosis rates. Larger multicenter research is warranted.
A document review of the development and implementation of the online undergraduate surgical teaching module at the University of KwaZulu-Natal due to covid-19 containment measures
S Ebrahim,1,2 M Motala,3 JM Van Wyk3,4
1 Department of Surgery, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
2 Health Systems Research Unit, South African Medical Research Council, South Africa
3 Department of Clinical and Professional Practice, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
4 Department of Health Sciences Education, University of Cape Town, South Africa
Background: The COVID-19 pandemic prompted the transition of all teaching and learning of final-year General Surgery students to an online platform.
Aim: A document review was conducted to determine the essential aspects of the teaching and learning programme that needed to be retained, proposed modifications, and implementation of an online surgical module.
Methods: The documents considered for inclusion were curriculum guides, module templates, assessment policies, resources on transition to remote learning and implementation plans. The 'READ' approach was used to analyse the documents. Steps included readying the materials, extracting and analysing the data, and distilling the findings. This study was approved by the Biomedical Research Ethics Committee of UKZN (BREC/00002686/2021).
Results: Thirty-three curriculum and policy documents were reviewed. The main online instructional methods comprised video-based instruction on core surgical topics, including lectures, case-based discussion, pre-recorded clinical and procedural skills videos delivered via the Moodle learning management system (LMS) and an assessment of knowledge and skills (weekly quizzes on Moodle). The assessment format for the clinical component also changed from a clinical case examination and oral viva voce examination pre-COVID-19 to a written, structured clinical case scenario examination.
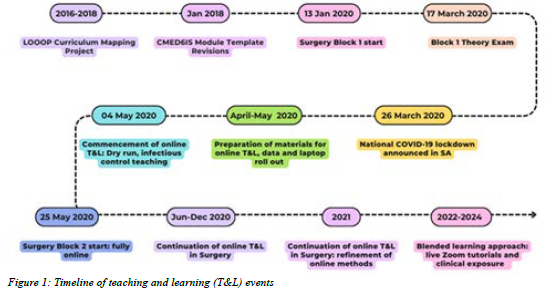
Conclusions: This document review provided a comprehensive understanding of the existing surgery curriculum at UKZN and the events and policies that influenced the changes implemented due to the COVID-19 pandemic. It does not reflect the teaching and learning experiences of faculty and students; however, it provides a valuable point of departure for further studies to understand the teaching and learning experiences better.
Associations within hospital mortality after injury in four South African hospitals
T MacQuene, K Chu
Equi-Injury South Africa Group, Global Surgery, Stellenbosch University, South Africa
Background: Injury is a major cause of mortality in South Africa and poses a critical challenge to public health systems. This study aims to describe characteristics of injured patients and determine risk factors associated with in hospital mortality in 4 South African hospitals.
Methods: Data were collected prospectively from admitted injured patients from four regional or tertiary hospitals in the Western Cape and Eastern Cape provinces. Descriptive statistics and multivariable regression were used to assess the association with mortality.
Results: From February 2023 to July 2024, 2 382 injured patients were enrolled, 1 565 (76.2%) were male and the median age was 32 years (IQR = 25-42). Intentional injury was n = 978 (42.7%). Orthopaedic (n = 847, 41.8%) and soft tissue (n = 639, 31.5%) injuries were most common. 630 (36.3%) patients were moderately to severely injured based on Kampala score and n = 1 695 (81.1%) had an operation. In-hospital mortality was n = 168 (7.1%). On multivariable logistic regression, severe injury (OR 7.76, p < 0.001), orthopaedic (OR = 0.04, p < 0.001), and neurosurgical injuries (OR = 2.86, p < 0.001) were more likely to be associated with in-hospital mortality.
Conclusion: Injury severity and type are significantly associated with mortality in South Africa. These findings may support more targeted interventions and policy development to reduce injury relate death and highlight the need to improve access to timely injury care.
Emergency theatre prioritisation - are we speaking the same language?
JP Scholtz, M De Kock
Department of Surgery, Faculty of Health Sciences, University of the Free State, South Africa
Background: Strategies for prioritising patients that require emergency surgery include categorising patients preoperatively by urgency. No specific guidelines exist in South Africa for the triage of emergency surgical cases (ESCs). Difficulties in applying standardised triage protocols of existing global guidelines are due to conflicts between specialties.
Aim: The aim of the study is to determine the interpretation of urgency of ESCs amongst doctors at UAHC to assess the need for implementing a standardised emergency triage theatre tool. To identify clinical and patient parameters that influence the interpretation of triage for ESCs and logistical challenges for booking ESCs.
Methods: A cross-sectional analytic survey-based study was conducted. The study involved five ESC scenarios triaged first with presenting pathology according to urgency and priority, followed by re-triage of the same scenarios with added clinical and patient parameters.
Results: Of the 86 study participants, 53.25% agreed between the five scenarios on presenting pathology and 45.35% agreed on the triage order for each scenario after patient and clinical parameters were added. A large proportion (74.43%) of participants changed the triage order after clinical and patient parameters were added. An even larger proportion (96.51%) concluded that a standardised triage tool for ESCs is needed.
Conclusion: The interpretation of urgency of emergency theatre cases differs amongst colleagues treating patients with ESCs. Hence, there is a need for implementing a standardised theatre triage tool to improve decision making when prioritising patients for theatre, which will decrease patient and resource related complications.
Surgical metrics in routinely collected health data in South Africa
E Lutge,1,2 N Moodley,1 D Clarke1,2,3
1 KwaZulu-Natal Department of Health, South Africa
2 University of KwaZulu-Natal, South Africa
3 University of the Witwatersrand, South Africa
Background: Surgical care is increasingly recognised as a public health issue. A substantial portion of the global disease burden, measured by disability-adjusted life years (DALYs), is related to surgically treatable conditions. Data is crucial in public health because it enables the monitoring of trends, and informs evidence-based interventions. However, surgical conditions are poorly represented in South African health information systems.
Aim: To describe the current status of surgery in the main routine data collection system in South Africa, the District Health Information System (DHIS), and to discuss the implications for the management and monitoring of surgical conditions
Methodology: A descriptive analysis of the indicators of the DHIS was undertaken. The National Indicator Dataset (NIDS) and the Provincial (KwaZulu-Natal) Dataset were included.
Results: The vast majority of indicators in both the NIDS and PIDS related to HIV and maternal and child health. Less than 5% of indicators in each related to general surgery or trauma. No information on the types of surgery performed is collected. Trauma indicators were introduced into the NIDS in 2023, after being collected in KZN for a decade.
Conclusion: Surgical conditions and their management are poorly monitored in the public sector in South Africa. Given that surgery is a public health concern, and that surgery is a significant cost driver in any health system, this is an important omission.
Proteomic mapping of macrophage polarisation toward an anti-tumour phenotype: enhancing treatment strategies
TN Augustine,1 T Mackade,2 N Altriche,2 KR Xulu,2 S Buthelezi3
1 Department of Anatomical Pathology, School of Pathology, Faculty of Health Sciences, University of the Witwatersrand, South Africa
2Department of Anatomical Sciences, School of Biomedical Sciences, Faculty of Health Sciences, University of the Witwatersrand, South Africa
3Next Generation Health, Council for Scientific and Industrial Research, South Africa
Macrophages are key players of innate immunity and wound healing, with subversion of their role fundamental in shaping the tumour microenvironment (TME). Macrophages (M0) are able to polarise into either anti-tumorigenic (M1) or protumorigenic (M2) phenotypes, depending on TME cues. We propose that shifting the polarisation status of macrophages may be a useful strategy to limit tumour progression. This in vitro study firstly investigated the impact of known polarising agents and time, on the proteome of M1 and M2 macrophages. This was followed by assessing the effects of Tamoxifen, the gold standard for management of hormone-dependent breast cancers, and Cannabidiol (CBD), an ethnomedicine used in symptomatic relief of selected side-effects, on the direct polarisation of macrophages.
SWATH-mass spectrometry demonstrated M0, M1 and M2 macrophages have distinct proteomic signatures, that may be temporally defined. However, their plasticity points to the importance of maintaining polarisation cues for anti-tumour function. Furthermore, Tamoxifen and CBD, particularly in combination, induce macrophage polarisation to the M1 phenotype. This is characterised by enrichment of pathways, including those involved in cytokine production, regulation of MAP-kinase and IFN-γ signalling, cellular metabolic processes and phagocytosis. The latter was also demonstrated by functional assays showing increased nitric oxide production and enhanced clearance of the MCF7 breast cancer cell line. Our findings suggest that CBD and Tamoxifen may synergistically modulate the TME, promoting M1 macrophage polarisation and inhibiting tumour cell growth, holding promise as an approach to enhance treatment strategies and positively impact the course of breast disease.
Follicular thyroid cancer in South Africa: Insights from 103 cases
Z Pienaar,1,2 W Conradie, 1,2 L Martin1,2
1 Department of Surgery, Tygerberg Hospital, Stellenbosch University, South Africa
2 Thyroid Cancer Group of South Africa, South Africa
Background: Follicular thyroid carcinoma (FTC) represents 17%-20% of well-differentiated thyroid cancer (WDTC) worldwide. In South Africa (SA), FTC is more common than international reports. However, available South African studies included small patient numbers. This multi-institutional study comprehensively describes FTC patients who underwent surgery over a 5-year period, focusing on presentation, diagnosis, management, and short-term outcomes.
Methods: This is a retrospective review of all patients with FTC operated at 13 academic hospitals throughout SA between January 2015 and December 2019. The Thyroid Cancer Group of South Africa (TCGSA) collectively entered data on the presentation, diagnosis, management, and short-term outcomes of 464 thyroid cancer patients into a REDCap database. Descriptive statistical analysis was performed.
Results: Of 464 cases captured in the database, 103 (22.1%) were FTCs. WDTC was reported in 87.9% (408/464) of operations, with FTC comprising 25.2% (103/408). Of the 103 patients, 83.3% (n = 85) were female and 16.7% (n = 17) male. The mean age was 51.8 years (SD 17.3). Over half of the patients presented with T3 (53.9%) tumours. Distant metastases were found in 12.6% (13/90) of patients. Thyroid lobectomy was the most performed procedure (57.4%, 58/103), followed by total thyroidectomy (37.6%, 38/103). The recurrent laryngeal nerve injury rate was 1.2% (2/159).
Conclusions: SA presents a multifaceted picture of FTC, with a higher incidence than in developed countries but lower than some other African nations. Patients frequently present with symptoms compared to high-income countries (HIC), which may predict worse outcomes. Surgery is the primary treatment for FTC in SA. Reported complication rates align with global standards.
A 10-year analysis of pulmonary metastatic hepatocellular carcinoma in South Africa: a matched cohort study with radiological analysis
M Emmamally, K Venter, R Khan, S Sobnach, E Jonas
Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
Background & Aim: Hepatocellular carcinoma (HCC) is a leading cause of mortality globally. Pulmonary metastases (PM) represent an advanced stage of disease, yet little is known about their clinical behaviour and management in these contexts.
Methodology: We conducted a retrospective matched cohort study at Groote Schuur Hospital, South Africa, including 77 patients with PM and 299 non-metastatic HCC patients between 2014 and 2023. Propensity score matching based on age, sex, and Child-Pugh grade yielded 77 matched pairs. Clinical characteristics, risk factors, and survival outcomes were compared. Kaplan-Meier (KM) survival analyses and radiological sub-analyses of metastatic burden, including lesion count and total tumour volume (TTV), were performed.
Results: Matched cohorts had similar clinical and prognostic scores (MELD, ECOG, BCLC), as well as similar laboratory parameters. Treatment was significantly more common in non-metastatic patients, while PM patients predominantly received best supportive care only (p = 0.0299). Survival was shorter in the PM group (mean 100.34 vs. 181.75 days, p = 0.024), but when comparing untreated PM to untreated non-metastatic patients, survival was equivalent (p = 0.986). Radiological sub-analysis revealed that patients with 1-3 pulmonary lesions had significantly better survival (p = 0.041), and those with TTV < 10 mm trended toward improved outcomes, though not statistically significant (p = 0.089).
Conclusion: PM HCC patients in our setting present with similar disease characteristics to non-metastatic cases but face limited treatment options. Survival differences appear driven by treatment access rather than disease severity. Selected patients with low metastatic burden may benefit from active intervention.
A prospective crossover multicentre study of the evaluation and accuracy of intra-operative ultrasonography versus standardised intra-operative cholangiography in a low middle-income country
J Buitendag,1 S Hofmeyr,1 E Jonas2
1 Stellenbosch University, South Africa
2 University of Cape Town, South Africa
Introduction: Gallstone-related disease frequently requires cholecystectomy, with intra-operative imaging essential for detecting CBD stones and preventing bile duct injuries. IOC is the traditional gold standard but has limitations, including radiation exposure and contrast-related risks. IOUS offers a non-invasive, radiation-free alternative with growing utility.
Methodology: In a prospective crossover study at two South African tertiary hospitals, 134 high-risk patients undergoing cholecystectomy will receive both IOUS and IOC. Data will be collected on diagnostic accuracy, procedural time, safety, workflow impact, and cost. IOC serves as the reference standard. (This is an ongoing study, only preliminary results will be presented. Currently we have 40 patients. Hopefully there will be more at the time of presentation.)
Results (Anticipated): IOUS is expected to demonstrate comparable accuracy to IOC in identifying CBD stones and delineating biliary anatomy, with advantages in procedural efficiency, reduced complication risk, and improved integration into surgical practice. It will also provide an alternative manner to image the biliary tract if a subtotal cholecystectomy is performed. (This has been proven based on preliminary results.)
Conclusion: IOUS appears to be equally as accurate and more efficient than IOC, and will be able to image the biliary tree in clinical scenarios that IOC cannot be used, i.e. subtotal cholecystectomy with a cystic duct orifice that cannot be safely cannulated.
A retrospective review of the treatment and outcomes of managing pancreatic ascites in chronic pancreatitis at Groote Schuur Hospital
B Misoi, M Bernon, E Jonas
Hepatopancreaticobiliary Surgical Unit, University of Cape Town, South Africa
Introduction: Pancreatic ascites is a rare complication of chronic pancreatitis (CP). Proximal pancreatic duct obstruction with distal disruption with protein rich fluid loss into the peritoneal cavity establish persistent ascites. Patients present with malnutrition from exocrine insufficiency and protein loss. Conservative treatment is associated with high failure rates. Endoscopic treatments are a viable alternative to surgical drainage procedures with less morbidity.
Methods: Patients with pancreatic ascites on the background of chronic pancreatitis who were treated at Groote Schuur Hospital, Cape Town South Africa, between 1st of January 2012 to 30th March 2025 were included in this study. Patients with pancreatic ascites secondary to malignancy, acute pancreatitis, iatrogenic causes or trauma were excluded. Data collected included demographics, baseline patient characteristics, investigation findings, management and outcomes and overall survival.
Results: Six of the nine patients were male with a median age of 40 (range 30-51). Alcohol overuse was the most common Aetiology of CP (8 out of 9). The most common presentation was abdominal distension and weight loss. All patients had an attempt at endoscopic management. Out of 5 successful pancreatic duct stenting, 3 had complete resolution of ascites, with 1 mortality and 1 with persistent pancreaticopleural fistula. All four patients who had surgery had an uneventful outcome.
Conclusion: Interventional treatments for pancreatic ascites in CP have a high success rate and should be attempted where technically feasible.
A systematic review of the management and outcomes of pancreatic ascites in chronic pancreatitis
B Misoi, M Bhana, M Bernon, E Jonas
Hepatopancreaticobiliary Surgical Unit, University of Cape Town, South Africa
Introduction: Pancreatic ascites in the setting of chronic pancreatitis associated with leakage from a disrupted pancreatic duct is rare with limited evidence on optimal management. Conservative management has high failure rates while surgical procedures are often limited by patients' poor condition. Endoscopic intervention is an alternative when technically feasible.
Methods: A literature search was performed as shown in Table 1. Cohort studies, case series and case reports in any language were included. Patients with acute pancreatitis and isolated pancreatic pleural effusions were excluded.
Results: A total of 93 studies were included. The mean age was 36.9 years, and the majority (136, 77.7%) were male. The most common aetiology was alcohol. Most patients presented with abdominal distension (145, 82.9%) and/or weight loss (50, 28.6%). The most common imaging findings were, apart from ascites pancreatic pseudocysts. Duct disruption was identified on endoscopic retrograde pancreatography in 79.7% of patients. A total of 65 (37.1%) patients underwent intervention surgically with a drainage procedure or left pancreatectomy, and 33 (18.9%) endoscopically via trans papillary pancreatic duct stenting, while the rest (77, 44%) were managed conservatively. The success rates for endoscopic and surgical management were 63.6% and 76.9% respectively without need for further intervention. Definitive non-interventional conservative management was associated with high rates (67.2%) of failure.
Conclusion: Conservative management of pancreatic ascites in chronic pancreatitis is associated with high failure rates. Endoscopic and surgical management strategies should be pursued in appropriate patients.
Beyond the scope: Outcomes of an endoscopic approach for the definitive management of major bile duct injuries
M Bhana, E Jonas
Hepatopancreaticobiliary Surgical Unit, University of Cape Town, South Africa
Background: Traditionally major bile duct injuries (MBDIs) have been managed with surgery, due to favourable long- term outcomes. Endoscopic treatment for MBDIs has more recently been performed with comparable results and lower morbidity rates, but data regarding long-term outcomes is lacking.
Patients and methods: This is a retrospective review analysing the short- and long-term outcomes of endoscopic management in 14 patients treated at our centre.
Results: Fourteen patients were included with a median age of 40 years (range 26-55 years), of whom 11 (79%) were female. The most common cause of injury was a misadventure during LC (n = 12, 86%) while the remainder was for penetrating trauma (n = 2, 14%). The most common presenting symptoms were pain (n = 9) and bile leaks (n = 9). The most common injury was a Strasberg E2, found in eight patients (57%). In seven (50%) patients endoscopic stenting was performed while the remained underwent the combined endoscopic and radiologic approach. Successful endoscopic management was achieved in all patients. Complications included cholangitis and pancreatitis, which were mild. In the patients still alive, none developed stenosis during a median follow-up of 22 months.
Conclusions: The definitive endoscopic management of patients with MBDIs represents a major advance in the management of these injuries. Endoscopic management is a safe and durable intervention for patients with MBDIs, with outcomes comparable to those ascribed to a surgical reconstruction. A broader view of management in these patients should be considered at a multidisciplinary team and considered for inclusion in treatment algorithms of MBDIs.
Dawn of the duck: a novel animal model for the study of hepatocellular carcinoma - a pilot study
S Sobnach, M Bernon, E Jonas, NB Leech
Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
Aim: There is a paucity of animal models to study hepatocellular carcinoma (HCC) globally. Traditional large animal models (Porcine, Woodchuck) are expensive and difficult to acquire. Hepatocellular carcinoma is well documented in hepatitis B virus (HBV)-infected Pekin ducks (Anas platyrhynchos domesticus). Moreover, there are similarities in human and duck HBV genomes. Pekin ducks can provide a cost-effective, and reproducible model for the study of HCC if the segmental anatomy is consistent, at least partially mirrors the segmentation of human livers and if major hepatectomies would be technically feasible. The aim of this study was to describe the surgical anatomy of the Pekin duck liver.
Methodology: Coloured-resin corrosion casts of the intra-hepatic vascularity (arterial and portal and hepatic veins) were performed in three Pekin duck livers, acquired from a local, licensed abattoir, where the ducks were slaughtered for commercial purposes.
Results: The casts consistently showed left and right liver lobes, consisting of three and four segments respectively. An additional lobe posterior, adjacent to the vena cava was found. Right and left hepatic arteries and portal veins supply their respective anatomical lobes. The middle and right hepatic veins drain the right lobe and left hepatic vein into the left lobe. There are two main bile ducts, and a gallbladder draining into the right duct.
Conclusion: Pekin ducks have a consistent hemi-liver and segmental configuration which technically would allow major resections. The pekin duck is potentially a cost effective animal model to further study liver regeneration in HCC.
From Metroticket to a Cape-to-Khartoum pass: Reimagining liver transplantation criteria for high-income countries in sub-Saharan Africa
S Sobnach, U Kotze, I Kim, T Du Toit, E Jonas
Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
Background: Current liver transplantation (LT) criteria and the Metroticket model were developed in high-income countries (HICs) and may not be appropriate for hepatocellular carcinoma (HCC) patients in sub-Saharan Africa (SSA).
Aim: To develop a regionally adapted LT framework for SSA through an exploratory cohort
Methodology: A retrospective observational cohort study of 647 HCC patients managed at Groote Schuur Hospital, Cape Town, South Africa was performed. Our LT experience and outcomes were reviewed, and current transplant criteria (Milan, University of California San Franciso, extended Toronto) were applied to non-transplanted patients.
Results: Six (0.9%) patients underwent LT with a median survival of 2557.5 (range:1049-3076) days. In the non-transplanted group, 31(4.8%) met at least one LT criterion, of whom 19 (61.3%) were eventually treated with resection (12) and ablation (7). The exploratory cohort (n = 140) was predominantly male (84.2%) with advanced HCC (BCLC stage C/D in 79.2%), but preserved liver function (median MELD-Na of 10 and Child-Turcotte-Pugh grade A disease in 61.4%). Only 16.2% of the exploratory cohort received curative-intended therapies. Patients who underwent LT survived significantly longer than the two other patient groups (p < 0.001).
Conclusion: This study highlights the potential limited applicability of current LT criteria in SSA, where applying criteria, less than 5% of HCC patients qualify. We propose a novel Cape-to-Khartoum framework incorporating clinical and biological parameters, including tumour markers, tumour differentiation and multi-omic profiling. This model may broaden LT eligibility and improve outcomes for HCC in SSA and warrants further validation through multicentre studies across the region.
Hepatocellular carcinoma in pregnancy: outcomes from a South-African cohort
K Venter, U Kotze, I Kim, S Sobnach, E Jonas
Department of Surgery, Faculty of Health Sciences, Surgical Gastroenterology Unit, Groote Schuur Hospital, University of Cape Town, South Africa
Introduction: Hepatocellular carcinoma (HCC) is a leading cause of cancer-related mortality worldwide. HCC during pregnancy is exceedingly rare, with only a few case reports and series published to date. We present a 30-year experience of HCC in pregnancy at a single tertiary academic centre -currently the largest of its kind.
Methods: We conducted a retrospective cohort study to describe the epidemiology, presentation, management and outcomes of pregnant patients diagnosed with HCC. Data were obtained from a long-standing institutional registry. All patients diagnosed with HCC during the perinatal period were included in the analysis.
Results: Of 728 patients, 192 (26.37%) were female, among whom 10 (5.21%) were diagnosed with HCC during the perinatal period. The mean age at diagnosis was 32.3 ± 4.98 years. Seven patients were diagnosed prenatally, but only two through routine antenatal screening. None received treatment during pregnancy; six initiated treatment postpartum, two with curative intent. Most patients died shortly after delivery, though three survived beyond one year, including two who surpassed 10-year survival. Intrauterine foetal demise occurred in four cases, and one pregnancy was electively terminated at diagnosis. The remaining pregnancies resulted in live births without complication.
Conclusion: Though exceptionally rare, HCC in pregnancy presents a dual mortality risk. This study outlines the characteristics of a vulnerable South African cohort, reflective of broader sub-Saharan African trends, given the shared biological and epidemiological context of HCC in the region.
Improved survival with TACE compared to sorafenib and best supportive care in a matched cohort of patients with BCLC stage C and D disease: A South African perspective
S Sobnach,1 S Cacciatore,2 M Bernon,1 LF Zerbini,2 E Jonas1
1 Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
2 International Centre for Genetic Engineering and Biotechnology (ICGEB), South Africa
Background & Aim: This study explores the use of transarterial chemoembolisation (TACE) as a palliative option for hepatocellular carcinoma (HCC) patients with BCLC-C and D disease.
Methodology: A single centre retrospective observational cohort study was performed.
Results: The study cohort comprised 478 patients; 310 (64.9%) patients had BCLC stage C and 168 (35.1%) had D disease. There were 352 (73.6%) men, with a median age of 49 (IQR: 38-63) years. The majority of patients (360/478, 75.3%) received BSC only. Fifty-eight (12.1%) were treated with TACE and 40 (8.4%) received sorafenib. Survival analyses of matched cohorts showed that patients with advanced HCC benefited from TACE treatment with a hazards ratio (HR) of 0.296 (95% CI: 0.180-0.487; p < 0.0001). To further elucidate the impact of the identified risk factors on TACE survival, patients were risk stratified into two groups: low-risk group (Gamma-glutamyl transferase (GGT) < 800 IU/L and portal vein tumour thrombosis (PVTT) absent) and high risk group (GGT > 800 IU/L or PVTT present). In the high-risk group, the comparison between BSC and sorafenib-treated patients' survival did not reach statistical significance (p = 0.053) In the low-risk group, only TACE showed a substantial OS benefit (p-value < 0.0001) compared to sorafenib and BSC, with a HR of 0.174 (95% CI: 0.084-0.360) (Figure 1).
Conclusion: GGT levels and PVTT are critical risk factors to consider when determining treatment strategies for HCC patients in SSA. Patients without these factors can significantly benefit from TACE as an alternative to sorafenib or best supportive care.
Outcomes of endoscopic management approach for major bile duct injuries
M Bhana, E Jonas
Hepatopancreaticobiliary Surgical Unit, University of Cape Town, South Africa
Introduction: Major bile duct injuries (MBDI's) remain a devastating complication. Endoscopic management is the treatment of choice for minor bile duct injuries, but is not yet widely accepted as definitive treatment for major injuries.
Aim: The aim of this review is to assess outcomes of MBDI's managed endoscopically.
Methodology: Eligible studies published between 1984 and 2024 were reviewed systematically. In addition, all patients treated endoscopically at our institution from January 2015 to December 2024 were identified from an ethics-approved registry. Long term outcomes of a definitive stent strategy were assessed.
Results: A total of 1 132 patients, 198 with complete transections (CT) and 934 with partial injuries (PI) were identified. We included a further 14 patients with MBDI's (8 CT and 6 PI) as a case series in the systematic review. Long term treatment success was achieved in 92% of complete transections and 94% of partial injury patients. The mean follow up period was 21 months for complete injuries and 29 months for partial injuries, and the mean stent duration was 9 and 8 months respectively. In 90% of patients in published studies, associated vascular injuries were not investigated for. The post stent stricture rate was 5% and cholangitis was the most common complication (19%).
Conclusion: The results of our study suggest that outcomes comparable to surgical treatment can be achieved with a definitive endoscopic management strategy in selected MBDI patients. A classification system to identify patients with MBDI's who are potential candidates for endoscopic management will aid optimal patient selection.
The management and outcomes of 620 consecutive cases of hepatocellular cancer at a large academic centre in Sub-Saharan Africa: the university of Cape Town experience
M Bernon, M Emmamally, K Venter, E Jonas, S Sobnach
Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
Background: Hepatocellular carcinoma (HCC) is a leading cause of mortality in sub-Saharan Africa (SSA). Unfortunately, there exists a paucity of outcomes studies from SSA in the literature.
Aim: To review the management and outcomes of HCC management at a large academic centre in South Africa.
Methodology: Demographic, clinical, management and outcomes data were sought from a prospectively maintained HCC database at Groote Schuur Hospital, Cape Town, South Africa. The study period was from June 1990 to June 2023.
Results: Six hundred and twenty patients comprised the study. Most were male (72%) and the mean age at presentation was 50 (range:13-89) years. In 268 (48%) patients, the Child Pugh Grade was A, and 56% were BCLC Stage C. The mean MELD score was 14 (range: 6-38). Only 110 (18%) patients underwent curative-intended therapy; 82 (13%) patients underwent liver resection, 20 (3%) patients had ablation and eight (1%) were transplanted. Trans-arterial therapies were performed in 122 (19%) patients. The remaining 278 (49%) patients were offered palliative treatment, the majority only receiving best supportive care (BSC). The median overall survival was 68 days (SD ± 503).
Conclusion: HCC is a fatal disease of the young in South Africa. Most patients present with advanced disease and only 18% benefit from curative-intended therapies. The overall survival is poor. This study represents the most comprehensive experience of HCC in SSA.
A single centre review of outcomes of delayed admission to a burns unit
Q Isaacs, A Muganza, C Sofianos
University of the Witwatersrand, South Africa
Background: Delayed admission to a Burn Unit delays in optimal treatment, resulting in worse outcomes for the patient. Delay to transfers for Level 1 trauma and Burns unit have been well studied internationally but there is limited research in South Africa. There has been a shift from assessing mortality to assessing length of hospital stay to measure unit's outcomes.
Aim: This study aims to assess if delay greater than 24 hours from time of burn to admission is associated with length of stay and number of complications.
Methods: A retrospective cross-sectional study was conducted, included all burns patients admitted over 5 year period to Chris Hani Baragwanath Academic Hospital adult (2018-2022). The date of burn and date of admission to determine those with delayed admission (> 24 hours), the primary outcome was length of stay (days) and secondary outcomes included sepsis and mortality. The Wilcoxon rank-sum test to compare continuous variables between groups, and the Chi-square test for categorical variables. Ethics approval was granted.
Results: Total of 123 files found. Seventy-one (58%) of patients were admitted under 1 day. Median length of stay was 14 days and no statistical difference in length of stay between the two groups (p value 0.7) Overall mortality rate was 13% with 68% within the early admission group.
Conclusion: Delayed admission to a burn unit had no effect on length of stay and no statistical significance in mortality rate or sepsis. There was no significant difference between in the rate of sepsis, between early and late admission to the burns unit.
Analysis of time to care and cost of damage control laparotomies in a tertiary centre in South Africa
HJ Kruger, E Steyn, GVE Oosthuizen
Department of Surgery, Tygerberg Hospital, Stellenbosch University, South Africa
Background: Damage control laparotomy [DCL] is a life-saving strategy for the management of hemodynamically unstable abdominal injuries. Although the indications are well established, factors specific to local trauma ecosystems lead to delays to DCL.
Methods: A retrospective review of prospectively collected data identified all patients who underwent DCL for trauma indications at Tygerberg Hospital between 1 January 2016 and 31 December 2020. A hybrid costing model was used to determine the cost of DCL.
Results: 131 Patients were included, of which 96.9% were male and the mean age was 33.4 years. Gunshots were the most common mechanism of injury (77.9%), followed by vehicular collisions (9.9%) and stabs (7.9%). The in-hospital mortality was 41.5%. The median time from incident to arrival at the trauma centre was 3 hours 7 minutes (187 minutes) and patients waited a median of 6 hours (360 minutes) for surgery once in hospital. The median duration of surgery was 120 minutes and the median time to relook laparotomy was 59 hours. The median ICU and ward stay was 9.7 days and 25.7 days, respectively. Cost was calculated using a hybrid costing model, with the cost of care for survivors estimated at R 464,951 (USD $25,200) and for non-survivors R 307,827 (USD $16,684). Total cost of care for this cohort was R 42,160,625 (USD $2,285,129).
Conclusion: Delay to surgical care for DCL patients is worse for patients treated in our unit compared to those in other units, with associated cost placing significant economic burden on the healthcare sector.
Clinical outcomes following bowel eversion in penetrating abdominal trauma
S Makhadi, T Ubisi, MS Moeng
University of the Witwatersrand, South Africa
Background: Bowel evisceration is associated with a high incidence of hollow viscus injuries. Laparotomy remains the standard of care. This study aims to review and characterise the nature of injuries related to bowel evisceration.
Methods: This study involved retrospective data collection from adult trauma patients presenting with omental evisceration at Charlotte Maxeke Academic Hospital over three years, utilising Medibank medical records. Data were analysed using descriptive statistics, normality testing with the Shapiro-Wilk test, and inferential statistics-including Fisher's exact test, univariate, and multivariate analyses- conducted with STATA version 18. Ethical approval was granted by the University of the Witwatersrand Human Research Ethics Committee and the hospital CEO (ethics number M201134).
Results: A total of 85 patients were analysed, with a mean age of 30 years. One patient died. Sixty-four point seven per cent of patients had bowel injuries with associated omental evisceration. Eight per cent were injured during nighttime hours. Sixty-four per cent were transferred from clinics or district hospitals. The vast majority-ninety-one per cent- sustained stab wounds, with the remaining eight from gunshot wounds. The mean base excess was -5.45, and lactate levels averaged 3.7. Eight patients presented with peritonitis. Injuries involved the stomach (n = 13), small bowel (n = 46), and colon (n = 15). Solid organ injuries included the spleen (n = 4), liver (n = 9), and kidney (n = 5). Nineteen per cent underwent damage control laparotomy. The mean operative time was 70 minutes (range 52.5-105)-twenty-five per cent required intensive care unit admission.
Conclusion: Laparotomy remains the definitive management for bowel evisceration. The most frequently injured organs were the small and large intestines.
Outcomes of daytime versus night-time emergency abdominal surgical (ES) procedures: A Western Cape Metropole perspective
M Alkhanbouli, S Rayamajhi, PH Navsaria
Trauma Centre, Groote Schuur Hospital, University of Cape Town, South Africa
Background: Abdominal emergency surgery is a common procedure with high morbidity and mortality. The aim of this study was to assess if the time of surgery (day versus night and weekend) affects the morbidity and mortality in an urban middle-to- low-income resource setting.
Methods: A retrospective study was conducted in four University of Cape Town teaching hospitals over a one-year period (01 September 2020-31 December 2021). Patient demographics and clinical characteristics, time of laparotomy, and postoperative outcomes were recorded. Chi-square and Wilcoxon rank sum tests were used to determine factors and outcomes associated with time of surgery. Logistic regression was used to determine factors associated with mortality. (HREC/UCT: 524/2022)
Results: One thousand four hundred and seventy-one (1471) patients underwent ES. The majority of patients were male (n = 952, 64.7 %), with median age of 36 years (IQR: 25, 45). Overall, 960 (65.2%) patients had comorbidities: smokers (n = 557, 37.8%), human immunodeficiency virus (n = 160, 10.9%), and illicit drug uses (n = 243, 16.5%), Characteristics were similar between patients operated at daytime and those operated at night/weekend. Of the 1471 patients who underwent emergency surgery, 885 (60.2%) patients were operated during the daytime, 585 (39.8%) patients were operated during the night and on the weekend. Common diagnoses were appendicitis (n = 434, 29.5%), trauma laparotomy (n = 467, 31.7%) and gastrointestinal perforations (n = 88, 5.9%). The overall mortality rate was 8%, of which 5% of patients were operated during day and 3% of patients were operated during night and weekends (p = 0.441). Overall, the morbidity rate was 17.3% for those operated during the day compared with 11.2% in patients operated during night/ weekends (p = 0.655). After controlling for confounding factors, there was no association between time of operation and mortality or morbidity.
Conclusion: Morbidity and mortality associated with emergency surgeries are high but the time of day for emergency surgery did not affect outcome in University of Cape Town referral hospitals.
Cumulative incidence and management of enterocutaneous fistulae owing to laparotomy for penetrating abdominal trauma: a single centre experience
A Sekason, L Moschides, YH Docrat, D McPherson, A Boutall, A Nicol, PH Navsaria
Trauma Centre and Colorectal Unit, Groote Schuur Hospital, University of Cape Town, South Africa
Background: Enterocutaneous fistula (ECF) owing to laparotomy for penetrating abdominal trauma is rarely reported. The quoted incidence in two recent publications is 1.9% and 1.5%, in 2 224 and 2 373 patients, respectively.
Advances in trauma surgery including damage control surgery and the use of open abdomen techniques, have led to concerns of increasing fistula rates in the trauma patients. The purpose of this study was to determine the incidence and outcomes of patients with ECF resulting from penetrating abdominal trauma.
Methods: A retrospective study including patients who underwent laparotomies for penetrating abdominal trauma (PAT) between 01 January 2015 and 31 August 2018 (44 months) was performed. GSH Trauma Centre RedCap, GSH Intestinal Failure Unit and the Stomatherapy department databases were scrutinised by folder review.
Results: Of a total of 965 patients with PAT, 597 underwent laparotomies and 586 had hollow viscus injury (HVI). Twenty-six patients (4.4%) developed an ECF or an anastomotic leak. Thirteen (50%) patients underwent damage control laparotomy. Fistulas and leaks occurred in small bowel 13 (50%), large bowel 7 (26.9%), duodenum 6 (23.1%). Five patients with ECF spontaneously resolved with medical treatment. Six patients (42.9%) with ECF were managed in the intestinal failure unit and required surgical intervention. Five anastomotic leaks were addressed at early relook laparotomy, with a mortality rate of 58.3%.
Conclusion: The anastomotic leak / ECF rate in penetrating abdominal trauma in our centre is 4.4% and is associated with a high mortality of 30.8%.
Outcome of damage control laparotomy in abdominal trauma at Steve Biko Academic Hospital and Kalafong Provincial hospital
T Ravele, B Jackson BI Monzon
University of Pretoria, South Africa
Background: Damage control surgery (DCS) remains a cornerstone in managing severely injured abdominal trauma patients. Despite advancements in surgical and critical care, mortality remains significant, particularly among patients requiring repeated interventions or experiencing postoperative complications.
Aim of study: To identify clinical, surgical, and physiological predictors of mortality in patients undergoing damage control laparotomy for abdominal trauma.
Material and Methods: This retrospective descriptive study analysed 107 patients who underwent damage control surgery at Steve Biko academic hospital and Kalafong provincial hospital. Demographic data, injury characteristics, vital signs, laboratory values, surgical interventions, and postoperative complications were examined. Mortality was the primary outcome, and statistical associations were assessed using chi-square and t-tests, ethic approval from university of Pretoria.
Results: The overall mortality rate was 15%. A statistically significant association was observed between mortality and the number of laparotomies performed (p = 0.009), with 19% of deaths occurring in patients who underwent four laparotomies. Mortality was also associated with physiological parameters: lower systolic blood pressure (p = 0.037), depressed Glasgow Coma Scale scores (p < 0.001), and trends toward metabolic acidosis (pH and base excess, p ~ 0.05-0.06). Postoperative complications including sepsis (50% in deaths vs. 26% in survivors, p = 0.076), fistula formation (13% vs. 2.2%) and ARDS (19% vs. 6.6%) were more frequent among those who died, though not statistically significant due to limited sample size.
Conclusion: Repeated surgical intervention, hypotension, impaired consciousness, and infectious or respiratory complications are key predictors of mortality in patients undergoing damage control surgery for abdominal trauma. Early identification and aggressive management of these risk factors may improve patient outcomes.
Routine laparotomy in cases of omental evisceration: retrospective review of a level 1 trauma unit
S Makhadi, T Ubisi, MS Moeng
Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, South Africa
Background: Omental evisceration suggests peritoneal penetration. The incidence of hollow viscus injuries varies in the literature. In Johannesburg, such cases are managed with mandatory laparotomy. This study aims to review the patient profile and laparotomy findings.
Methods: This study involved the collection of data from adult trauma patients with omental evisceration at Charlotte Maxeke Johannesburg Academic Hospital over three years, utilising Medibank medical records. Data analysis included descriptive statistics, normality testing with the Shapiro-Wilk test, and inferential statistics such as Fisher's exact test, univariate, and multivariate analyses conducted using STATA version 18. Ethical approval for the research was granted by the University of the Witwatersrand Human Ethics Committee and the hospital CEO, under ethics number M201134.
Results: A total of 97 patients were identified. The median age was 30 years (IQR 25-36). Eighty-three patients (86%) had stab wounds, and 14 had gunshot injuries. Sixty per cent sustained associated hollow visceral injuries. On arrival, the median base excess was -4.3, and the median lactate was 2.9. Half of the patients exhibited peritonitis. Eighteen per cent sustained stomach injuries. Thirty-five per cent had stomach injuries. Twenty-two per cent sustained colon injuries. Seventeen per cent had mesenteric injuries. Thirteen per cent had associated chest injuries. Eleven per cent of patients underwent damage control laparotomy. The average theatre time was 84 minutes.
Conclusion: The high incidence of major visceral injuries associated with omental evisceration supports a policy of routine exploratory laparotomy. Omental evisceration warrants suspicion of potentially serious injury and reinforces the recommendation for routine laparotomy or laparoscopy.
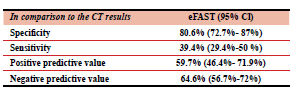
The correlation between eFAST findings and CT findings in a tertiary centre within KwaZulu-Natal
BR Govender, T Hardcastle, N Dlamini
Albert Luthuli Hospital, University of KwaZulu-Natal, South Africa
Background: In the setting of a high burden of trauma within a resource-stricken country such as South Africa, eFAST represents an affordable, non-invasive procedure with an exponential benefit in the setting of trauma to screen for patients who may benefit from early surgery or further imaging.
Methods: A retrospective, quantitative chart review was performed at the tertiary trauma centre of Inkosi Albert Luthuli Central Hospital (IALCH) in KwaZulu-Natal, South Africa between 2017 and 2019. The eFAST and CT findings were in the database were compared which resulted in Positive predictive values (PPV), Negative predictive values (NPV) as well as sensitivity and specificity data for eFAST in relation to CT in a trauma setting. The initial raw data was from an University of KwaZulu-Natal Ethics approved Class Approval Database (BCA207-09). The values were compared against international studies.
Results: 863 files were reviewed, of which 223 files met the inclusion criteria. The median age was 30 years with a distribution of 76.7% of male patients and 23.3% of female patients. MVA/PVA was demonstrated as the dominant method of injury at 76.23%. The mortality rate was 26% given the ISS scores that demonstrated the very severe (> 25 score) category as the predominant category at 80.26%. This study's PPV, NPV, Sensitivity and Specificity results were 59.7%,64.6%, 39.4% and 80.6% respectively. These results were then compared to international values with PPV, NPV, sensitivity and specificity ranges of (87-98%), (64-98%), (42-90%) and (84-100%) respectively.
Conclusion: This study depicted eFAST's importance in ruling in pathology and need for further imaging in ruling out pathology based on the results as well as in comparison to international findings.
Train-related injuries in a developing country setting: Epidemiology and management
A Khamajeet, A Diab, K Paresh, A Nicol, P Navsaria
Trauma Centre, Groote Schuur Hospital, University of Cape Town, South Africa
Introduction: Train-related injuries represent a significant yet underreported public health challenge in developing countries, particularly in sub-Saharan Africa, where contemporary data are scarce. This study characterises the epidemiology, clinical presentation, and outcomes of train-related trauma at a South African Level I trauma centre, with a focus on identifying predictors of severe outcomes and informing context-specific interventions for this high-risk population.
Method: A retrospective analysis was conducted on 63 patients presenting to Groote Schuur Hospital between April 2008 and June 2013. Data collected included demographics, injury mechanisms, clinical findings, and outcomes. Multivariable logistic regression was performed to evaluate the association between key severity markers (GCS < 8, hypotension, mangled extremities) and ICU admission.
Results: The cohort was predominantly male (96.8%) with a median age of 26 years (IQR: 22-33). Injuries clustered during winter months (April-October), with 62% occurring between 4:00 PM and midnight. The most common mechanisms were boarding or alighting from moving trains (46.2%) and interpersonal assault (33.3%). Lacerations were the most frequent soft tissue injury (69.8%), while lower (25.4%) and upper limb (22.2%) fractures were the predominant orthopaedic injuries. The amputation rate was 20.6%, strongly associated with mangled extremities. Median hospital stay was 6 days (IQR: 1-17), extending significantly for patients with spinal trauma. Severe traumatic brain injury (GCS < 8) was independently associated with ICU admission (adjusted OR 15.0; 95% CI: 2.7-82.4; p < 0.001). Mangled extremities and hypotension were not significantly associated with ICU requirement.
Conclusion: Young male commuters are more likely to sustain severe, preventable train-related injuries. Significant musculoskeletal trauma, head, and spinal injuries increased hospital stay, underscoring the need for comprehensive assessment to reduce morbidity and improve outcomes. Our findings support protocolised neurosurgical and orthopaedic triage and targeted prevention strategies in resource-limited settings.
The role of psoas density measurement in CT scan as a predictor of outcome in severely injured trauma patients in low- and middle-income countries. Our experience at a tertiary hospital in South Africa
R Roos,1 H Kluyts,2 L Swanepoel-Stassen1
1 Department of General Surgery, Sefako Makgatho Health Sciences University, South Africa
2 Department of Anaesthesiology, Sefako Makgatho Health Sciences University, South Africa
Aim: Predicting the outcome in the severely injured trauma patient is crucial and plays a central role in planning intervention and postoperative support. Several studies have suggested that psoas muscle density, indicative of sarcopenia, may be associated with poorer outcome in surgical patients. To determine whether psoas density measurement of severely injured trauma patients predicts outcome.
Materials and methods: A prospective observational analysis of severely injured trauma patients was performed.
Severely injured trauma patients were defined as P1 and P2 patients, as well as patients with an injury severity score (ISS) of > 9. Patients not subjected to abdominal computed tomography (CT) scans and < 18 years of age were excluded from the study. The demographics, physiological parameters in the Emergency Department, psoas density and morbidity and mortality were analysed.
Results: A total of 105 patients were recruited for this study but only 58 complied with the inclusion criteria. Significantly more patients survived with a psoas density of > 50 compared to a density of < 50 (76.3% vs 15.0%; p < 0.001). There was a significant difference of 6 days length of intensive care unit (ICU) stay between the mean values of patients who presented with psoas densities of < 50 and > 50.
Conclusions: Psoas density measurement shows promise as a potential predictor of outcome in the severely injured trauma patient. In the absence of other rapid tools in assessing nutritional status, psoas density measurement on CT scan might become invaluable to the trauma surgeon.
Leucocytosis as prognostic indicator for renal replacement therapy in crush syndrome
A Vorster, OY Matsevych
Department of General Surgery, Sefako Makgatho Health Sciences University, South Africa
Background: Crush injuries, frequently stemming from mob justice, are a common cause of trauma-related admissions in South African emergency departments. These can progress to crush syndrome, marked by rhabdomyolysis and acute kidney injury (AKI). While venous bicarbonate (VB) is an established prognostic marker for renal replacement therapy (RRT), the role of leukocytosis (elevated white cell count, WCC) as a predictor remains insufficiently explored.
Objective: To determine whether an elevated WCC on admission predicts the need for RRT in patients with crush syndrome.
Methods: A retrospective cohort study was conducted at two public hospitals in Gauteng, South Africa, including 143 adult patients with crush syndrome admitted between January and December 2022. Data collected included demographics, injury mechanisms, and laboratory values (WCC, urea, creatinine, VB, CK, potassium). Correlation analyses were used to assess associations between WCC and RRT, renal biomarkers, and mortality.
Results: The cohort was predominantly male (96.5%) with a median age of 29.3 years. Elevated WCC (mean 14.67 × 109/L) significantly correlated with increased urea and creatinine and inversely with bicarbonate (p < 0.001), indicating a link with renal dysfunction and acidosis. No correlation was found with potassium or CK. Six patients (4.2%) required RRT; two of these patients died. Although the association between WCC and RRT was not statistically significant (p = 0.727), RRT recipients had higher mean WCC.
Conclusion: Leukocytosis may serve as a supplementary marker for early risk stratification in crush syndrome. Further prospective studies are needed to validate its predictive utility.
Determining the spectrum of comorbidity in a South African achalasia cohort
AK Nyarko, GE Chinnery, MF Scriba, E Jonas, J van Zyl
Upper Gastrointestinal (UGI) Surgery Unit, Groote Schuur Hospital, University of Cape Town, South Africa
Background: Achalasia is a rare oesophageal motility disorder characterised by a lack of peristalsis of the oesophageal body with failure of lower oesophageal sphincter (LES) relaxation due to degeneration of inhibitory innervation of the myenteric plexus (of Auerbach). While the aetiology is still unclear, an autoimmune background is suspected.
Methods: A retrospective review of the clinical presentation and patient comorbidities at the time of achalasia diagnosis by a single investigator motility service using high resolution manometry (HRM) between August 2012 and September 2024. The objective of this study was to investigate the spectrum of co-morbidities present within a Sub-Saharan African cohort of confirmed achalasia patients. All adult patients (> 18 years of age) diagnosed on HRM with achalasia during the study period were evaluated for possible inclusion. Patients with other oesophageal motility disorder were excluded
Results: During the 12-year study period 352 patients underwent HRM for achalasia. The mean age of the cohort was 46.5 (SD ± 17.9) years with a slight female majority (198; 56.3%). In the newly diagnosed achalasia patients, the presenting duration of symptoms was a median of 24 months (IQR 12-72 months). At time of achalasia diagnosis 45% (160) of patients were being treated for one or more co-morbidities. Sixteen patients had a known autoimmune condition
Conclusion: Several achalasia sufferers had been diagnosed with a comorbid conditions including autoimmune diseases prior to presentation.
Helicobacter pylori resistance to clarithromycin and fluoroquinolones in South Africa
JDD de Freitas, G Chinnery, M Scriba, J Wojno
Division of General Surgery, University of Cape Town, South Africa
Background: Helicobacter pylori is a group 1 carcinogen and the most common chronic infection worldwide. Eradication has become a cornerstone for the treatment and prevention of recurrence of peptic ulcer disease. Limited data exists on the prevalence of infection and antibiotic resistance burden in South Africa.
Method: We conducted a retrospective database review of all gastric and duodenal biopsy specimens submitted for genotypic testing at a private national laboratory in South Africa between 1 January 2019 and 31 December 2023 to determine the H pylori prevalence, clarithromycin, and fluoroquinolone antimicrobial resistance.
Results: We identified Helicobacter pylori in 2305 (81.2%) of 2 840 specimens. We detected fluoroquinolone, clarithromycin and dual resistance in 54.3%, 45.0%, and 29.2% of this sample, respectively. Increasing age and female sex were associated with higher prevalence of resistance.
Conclusion: This is the largest study of Helicobacter pylori prevalence and resistance in South Africa to date. The high infection prevalence alongside exceedingly high levels of resistance to clarithromycin and fluoroquinolones, should serve as an urgent call for further research in this area and guideline revision to determine a new approach to identification and eradication of this group 1 carcinogen in our at risk population.
Outcomes of band ligation for prevention of variceal upper gastrointestinal bleeding
LM Ramatladi, K Mathonsi, NM Latakgomo
Department of General Surgery, Pietersburg Hospital University of Limpopo, South Africa
Background: Upper gastrointestinal bleeding (UGIB) is defined as bleeding from the mouth until proximal to the ligament of Treitz, it is a common and challenging emergency with an annual incidence of 50 to 150 per 100,000 of the population (Primignani, 2001). Chalasani et al defined portal hypertension as a hepatic venous pressure gradient (HVPG) of more than 5 mmHg with varices forming and starting to bleed at a portal pressure of more than 12 mmHg. The common complications of portal hypertension are gastroesophageal varices and variceal haemorrhage. Prevention of first variceal haemorrhage will depend on the size and characteristics of the varices, medium or large varices can be treated with B-blockers or oesophageal band ligation (Meara, 2015). Endoscopy is done as soon as possible within 12-24 hours after presentation after adequate resuscitation. The Baveno VII guidelines recommend endoscopic band ligation to prevent first variceal bleeding in compensated patients with high-risk varices who have contraindications or intolerance to non-selective beta-blocker (Clarke, 2010).
Objective: To determine the number of banding sessions required to eradicate varices, to assess the rebleeding rate, the mortality and morbidity rate associated with variceal UGIB bleeding.
Methods: A retrospective quantitative cohort study design comparing the outcomes of patients presenting with variceal UGIB presenting to Pietersburg Tertiary Hospital from January 2018 to December 2022. This included all patients above 18 years who present with variceal UGIB, all elective and emergency case presentations. Patients who are bleeding from isolated gastric or ectopic varices where excluded.
Results: The median follow up period was 24 months with a total of 144 patients having recurrent bleeding, 63% of the episodes where related to portal hypertension. We also had a few encounters whereby some patients deferred banding sessions due to lack of resources at that time. A total of 96 patients had recurrent bleeding and some of the reasons are attribute to lack of resources. Major complications were noted in 43 patients who ended up requiring admission and blood transfusion. 12 deaths were related to variceal bleeding.
Conclusion: The results confirm that in our population, endoscopic band ligation is a safe and effective technical approach. The study also shows that using EBL as an emergency therapy together with vasoactive drugs is associated with a less mortality and morbidity rate. Variceal band ligation is effective and safe when beta-blockers are contra-indicated or not tolerated for preventing first variceal bleeds.
The perturbations of duodenal Paneth and Goblet cells in benign and malignant obstructive jaundice in black South African adult population
HY Sani,1 JA Johnson,1 EF Mbajiorgu,1 T Marumo,2 TE Luvhengo2
1 Department of Anatomical Sciences, School of Biomedical Science, University of the Witwatersrand, South Africa
2 Department of Surgery, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, South Africa
Background: Obstructive jaundice (OJ) is biliary tract disease characterised by mechanical obstruction that disrupts the normal flow of bile in the intrahepatic or extrahepatic ducts. Additionally, OJ is characterised by the absence of bile in the gastrointestinal tract, leading to failure to control and regulate the gut microbiome, a process which is mitigated by the release of antimicrobial peptides and reconstruction epithelial and glandular by Paneth cells. Therefore, this study investigated the histomorphology changes in Paneth cells in benign and malignant OJ.
Patients and Methods: Biopsies from were collected from the duodenum distal to ampulla of Vater during upper GIT endoscopy or endoscopic retrograde cholangiopancreatography (ERCP) of male and female patients aged twenty years and above with or without benign and malignant jaundice. Biopsies were processed with routine haematoxylin and eosin (H & E) and semi-quantitative analyses of Paneth cells granules were done. The study received prior approval ethical clearance (MED23-10-333).
Results: A total of 60 biopsies were taken. A decrease in Paneth cell granules was shown in benign (25%) and malignant (40%) OJ compared to the control. Overall, results also showed less Paneth cell granules (25%) with increased goblets cells (45%) in males than in females.
Discussion: These results point to the potential of obstructive jaundice to alter the duodenal antimicrobial homeostasis / milieu and protective mucous barrier properties, especially amongst males, and calls for differential care in their clinical management.
Upper GIT Endoscopy Training
I Musa, G Chinnery, M Scriba
Upper Gastrointestinal (UGI) Surgery Unit, Groote Schuur Hospital, University of Cape Town, South Africa
Background: Upper gastrointestinal endoscopy (UGE) is a vital skill for general surgeons, yet the adequacy of training in low-resource settings like South Africa remains unclear. This study assesses endoscopy training for general surgery registrars at Groote Schuur Hospital, with a focus on the impact of the COVID-19 pandemic.
Methods: A retrospective analysis of the Upper Gastrointestinal Surgery Registry was conducted from 1 April 2018 to 30 September 2024. Data on diagnostic and interventional UGEs were reviewed across three periods: pre-COVID-19, during COVID-19, and post-COVID-19. Registrar exposure was evaluated based on the number of procedures performed during a standard three-month rotation. Descriptive and comparative statistical methods were applied (p < 0.05).
Results: Of 12,455 UGEs, 6,901 (55.3%) were performed by registrars. Diagnostic procedures accounted for 66.9% of all UGEs, with registrars performing 64.1%, while interventional procedures made up 33.1%, with 37.8% performed by registrars. Training during the COVID-19 period was significantly reduced, with only two registrars completing full rotations, compared to the usual 12-18. Although procedural volume increased post-COVID-21.8% for diagnostic and 60.2% for interventional UGEs-median registrar exposure per rotation dropped from 131 pre-COVID to 112 post-COVID. This indicates that despite increased service delivery, registrar training opportunities did not return to pre-pandemic levels.
Conclusion: General surgery registrars at Groote Schuur Hospital receive substantial endoscopy exposure; however, the COVID-19 pandemic disrupted training significantly. Enhancing simulation-based learning and optimising rotations are crucial to ensure adequate competency in UGE.
Aspartate Aminotransferase-to-Platelet Ratio Index (APRi) as Biomarker for Liver Damage in Biliary Atresia (BA): A Meta-analysis
E Brits,1 S Brown,2 L Botes,3 JB Sempa,4 M Pienaar5
University of the Free State, Bloemfontein, South Africa
1 Division of Paediatric Surgery, Department of Surgery, School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, South Africa
2 Division of Paediatric Cardiology, Department of Paediatrics and Child Health, School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, South Africa
3 Department of Health Sciences, Faculty of Health and Environmental Sciences, Central University of Technology, South Africa
4 Department of Biostatistics, Faculty of Health Science, University of the Free State, South Africa
5 Division of Critical Care, Department of Paediatrics and Child Health, School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, South Africa
Background: Biliary atresia (BA) is a rare paediatric liver disease requiring early diagnosis and surgical intervention. The aspartate aminotransferase-to-platelet ratio index (APRi) has emerged as a potential non-invasive biomarker of liver fibrosis, yet lacks a standardised threshold for clinical use.
Aim: To assess the diagnostic accuracy of APRi for liver fibrosis and cirrhosis in BA and determine appropriate cut-off values.
Methods: A systematic review and meta-analysis were conducted using PRISMA guidelines. Studies were identified via EBSCOhost and other databases (2003-2024). Inclusion: original studies in children with BA reporting histological liver fibrosis and APRi at diagnosis or Kasai portoenterostomy (KPE). Exclusion: post-KPE follow-up studies, non-human data, and insufficient APRi metrics. Data were analysed using R (v4.3.2) with heterogeneity assessed by I2 and Cochrane Q. Ethics approval was obtained from the University of the Free State.
Results: Fourteen studies (10 retrospective, 3 prospective, 1 cross-sectional) were included. APRi cut-off values for advanced fibrosis (F3) ranged from 0.7 to 2.26. Meta-analysis of four studies (n = 209) yielded pooled APRi means: 1.16 (95% CI: 0.57-1.75) for favourable histology (< F2) and 2.10 (95% CI: 1.67-2.52) for unfavourable histology (> F3). Significant heterogeneity was noted in the former group.
Conclusion: APRi shows potential as a non-invasive biomarker for liver fibrosis in BA. However, due to variability in thresholds and overlapping confidence intervals, it cannot yet replace liver biopsy in clinical decision-making. Further studies are needed to validate context-specific cut-offs.
The role of cow's milk protein allergy in refractory gastroesophageal reflux disease in infants: a scoping review
E Brits
Division of Paediatric Surgery, Department of Surgery, School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, South Africa
Background: Cow's milk protein allergy (CMPA) is a common food allergy in infants and may underlie up to 50% of cases of refractory gastroesophageal reflux disease (GERD). Symptom overlap between GERD and CMPA complicates diagnosis, particularly in non-IgE-mediated cases.
Aim: To evaluate and map the current evidence on the role of CMPA in refractory GERD in infants, and identify diagnostic and therapeutic challenges.
Methods: A scoping review was conducted using Joanna Briggs Institute methodology and reported according to PRISMA-ScR. The review included studies from 2014 to 2024 reporting on CMPA in infants with GERD. Eligible studies included human paediatric patients (< 18 years), with GERD and/or CMPA, evaluating the impact of CMPA on GERD management. Studies with congenital, neurological, or surgical causes of GERD were excluded. Searches were conducted across EBSCOhost, Scopus, and Google Scholar. Data were managed using REDCap and analysed narratively. Ethics approval was granted by the University of the Free State (UFS-HSD2024/2131).
Results: Twenty studies were included. CMPA contributed to up to 50% of refractory GERD cases. Symptom resolution was frequently observed with CMP elimination or hypoallergenic formulas. Diagnostic challenges were prominent, especially in non-IgE cases. Key knowledge gaps included the lack of standardised diagnostic tools, long-term safety data, and nutritional outcomes of elimination diets.
Conclusion: CMPA is a significant contributor to refractory GERD in infants. Early elimination trials and use of hypoallergenic formulas are effective first-line strategies. Standardised diagnostic protocols and further research are essential to improve outcomes.
Proteomic mapping of macrophage polarisation toward an anti-tumour phenotype: enhancing treatment strategies
TN Augustine,1 T Mackade,2 N Altriche,2 KR Xulu,2 S Buthelezi3
1 Department of Anatomical Pathology, School of Pathology, Faculty of Health Sciences, University of the Witwatersrand, South Africa
2 Department of Anatomical Sciences, School of Biomedical Sciences, Faculty of Health Sciences, University of the Witwatersrand, South Africa
3 Next Generation Health, Council for Scientific and Industrial Research, South Africa
Macrophages are key players of innate immunity and wound healing, with subversion of their role fundamental in shaping the tumour microenvironment (TME). Macrophages (M0) are able to polarise into either anti-tumorigenic (M1) or pro-tumorigenic (M2) phenotypes, depending on TME cues. We propose that shifting the polarisation status of macrophages may be a useful strategy to limit tumour progression. This in vitro study firstly investigated the impact of known polarising agents and time, on the proteome of M1 and M2 macrophages. This was followed by assessing the effects of Tamoxifen, the gold standard for management of hormone-dependent breast cancers, and Cannabidiol (CBD), an ethnomedicine used in symptomatic relief of selected side-effects, on the direct polarisation of macrophages.
SWATH-mass spectrometry demonstrated M0, M1 and M2 macrophages have distinct proteomic signatures, that may be temporally defined. However, their plasticity points to the importance of maintaining polarisation cues for anti-tumour function. Furthermore, Tamoxifen and CBD, particularly in combination, induce macrophage polarisation to the M1 phenotype. This is characterised by enrichment of pathways, including those involved in cytokine production, regulation of MAP-kinase and IFN-γ signalling, cellular metabolic processes and phagocytosis. The latter was also demonstrated by functional assays showing increased nitric oxide production and enhanced clearance of the MCF7 breast cancer cell line. Our findings suggest that CBD and Tamoxifen may synergistically modulate the TME, promoting M1 macrophage polarisation and inhibiting tumour cell growth, holding promise as an approach to enhance treatment strategies and positively impact the course of breast disease.
Outcomes of breast cancer in patients with positive family history
M Muvhango, D Montwedi
University of Pretoria, South Africa
Background: Breast cancer is common amongst women is south Africa. A positive family history of breast cancer is an important risk factor. Patients with familial breast cancer are known to present at an earlier age, high grade tumours and poorer survival. Studies investigated outcomes of breast cancer in patients with a positive family history and found conflicting results. Aim of this study was to determine presentation and outcome of breast cancer in patients with positive family history.
Methods: 361 patients were enrolled in the study. Patients presenting with a first degree relative with breast cancer (n = 102) compared with patients without a family history (n = 259). Data was collected prospectively from January 2017 to January 2020 and a follow up of three years. The two cohorts were compared in terms of age, stage at presentation, tumour biology and survival.
Results: Patients with first degree relative presented at significantly younger age compared to those without family history. Patients with a family history of breast cancer presented commonly with histological grade 3 breast cancer (46.0% vs 30.1%). The overall survival was worse in patients with locally advanced cancer and a positive first degree relative at 3 years (p = 0.02) The overall survival (83%) and disease-free survival (88.8%) for early and metastatic breast cancer was the same at 3 years amongst the two groups
Conclusions: The survival outcomes in patients with positive history were worse for locally advanced cancer.
Stemness-mediated changes to ER, PR and Ki67 in breast cancer cell lines exposed to hormone therapy
KR Xulu,1 S Gallant,1 TN Augustine2
1 Department of Anatomical Sciences, School of Biomedical Sciences, University of the Witwatersrand, South Africa
2 Department of Anatomical Pathology, School of Pathology, Faculty of Health Sciences, University of the Witwatersrand, South Africa
Introduction: Breast cancer heterogeneity is mediated by the intrinsic stemness displayed in subpopulations. Stemness markers, including CD44 and CD133, mediate multipotency, cell communication, metastasis, and drug resistance.
Aim: To characterise the plasticity of common diagnostic markers such as oestrogen receptor variants (Era & Erß), proliferation marker Ki-67 and progesterone receptor (PR) in tumour subpopulations of luminal A breast cancer cell lines (MCF7 & T47D) following exposure to hormone therapy.
Methods: Breast cancer cells were cultured using a standard procedure. Magnetic cell sorting was undertaken to isolate subpopulations displaying stemness as follows: CD44+CD133+; CD44-CD133+; CD44+CD133- and CD44-CD133-. The subpopulations were propagated in a specialised medium to maintain their stemness features. Subsequently, flow cytometry was conducted to verify the stemness phenotype. Cells were treated with 2 liM Tamoxifen and 16 ng/ml Anastrozole for 24 hours. Then, immunocytochemistry was conducted to localise the protein expression of Era, Erß, Ki-67 and PR. The images were taken using an Olympus iX35 fluorescent microscope and an Olympus BX63 fluorescent microscope. Fluorescence was qualitatively analysed using Cell Profiler, and statistical analysis was performed.
Results: The findings indicate differential changes in the expression of Era, Erß, Ki-67 and PR in subpopulations following treatment with tamoxifen and anastrozole. CD133-mediated stemness in MCF7 cells and associated with better drug outcome. In contrast, CD44-mediated stemness in T47D cells and associated with drug resistance.
Conclusion: Luminal A breast cancer cell lines display stemness plasticity which may affect hormone therapy outcome.
Targeting breast cancer stemness: Enhancing macrophage anti-tumour immunity with tamoxifen and CBD co-treatment
N Altriche,1 KR Xulu,1 TN Augustine2
1 Department of Anatomical Sciences, School of Biomedical Sciences, Faculty of Health Sciences, University of the Witwatersrand, South Africa
2 Department of Anatomical Pathology, School of Pathology, Faculty of Health Sciences, University of the Witwatersrand, South Africa
Introduction: Macrophages, which polarise into anti-tumour (M1) or pro-tumour (M2) phenotypes, can mediate the stemness profile of breast tumour cells. This may influence tumour response to standard therapies, such as Tamoxifen, and ethnomedicines, such as Cannabidiol (CBD). While both drugs independently induce non-stem-like tumour cell death, it remains unclear how the interactions of stem-like tumour cells and macrophages influence tumour response to co-treatment.
Aim: To investigate how macrophages impact the stemness-mediated response of breast tumour cells to Tamoxifen and CBD co-treatment.
Methods: MCF7 breast cancer cell viability following co-treatment was assessed using the neutral red and MTT assays. Stem-like and non-stem-like cells were magnetically isolated from an MCF7 parent population, and CD44/CD133 expression was phenotypically assessed. Cells were treated in monoculture or co-culture with RAW 264.7 macrophages. Macrophage phagocytic capacity and nitrite production, and changes in MCF7 epithelial-to-mesenchymal transition (EMT)-related gene expression, were analysed. HREC: W-CP-230316-01.
Results: Co-treatment reduced parent MCF7 cell viability; however, surviving cells were morphologically mesenchymal, typical of stem-like phenotypes. Stem-like cells expressed higher CD44 and CD133 and were less susceptible to direct Tamoxifen and CBD treatment. This was abrogated upon co-culture with macrophages, which effectively targeted stem-like cells through enhanced phagocytosis and nitrite synthesis. Macrophages influenced treatment-induced changes in MCF7 ß-actin, vimentin and beclin-1 expression, which was reduced in stem-like cells thus reflecting altered cytoskeletal and autophagic dynamics.
Conclusion: The efficacy of Tamoxifen and CBD co-treatment in promoting stem-like tumour cell death is enhanced by treatment-induced macrophage anti-tumour function, thus affirming a potential role for the co-treatment in anti-tumour immunity.
The outcome of hookwire-guided breast conserving surgery at Charlotte Maxeke Johannesburg Academic Hospital breast unit
D Ferrar, B Phakathi, N Mabe, J Edge, D Kruger
Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, South Africa
Background: Improved breast cancer awareness, screening and radiological technology have led to an increasing detection of impalpable breast cancers. The gold standard for treating impalpable cancers is breast-conserving surgery (BCS), which requires pre-operative localisation. At our institution, hookwire-guided localisation, a method of wire guided localisation (WGL), is the only method available. This study aims to assess if our practice of WGL aligns with international standards and to identify factors influencing recurrence.
Methods: We retrospectively reviewed records of patients who underwent hookwire guided BCS of breast carcinoma from 1 January 2016 to 31 May 2024 using the Charlotte Maxeke Johannesburg Academic Hospital (CMJAH) breast cancer database.
Results: A total of 119 patients were eligible, with 55 having had malignancies excised via hookwire guidance. 76.7% presented with a self-palpated mass, and 14.5% were detected via screening. Most patients (50.9%) received neoadjuvant chemotherapy (NAC) to shrink the tumour. The median size of masses was 19 mm. Of those undergoing hookwire guided BCS, 58.18% received radiation, with a median of 216 days from surgery to radiation (IQR 175-357). Margin positivity and re-excision rates were 10.9% and 12.7%, respectively. The recurrence rate was 25.5%, higher than international standards. TNBC (triple negative breast cancer) and NAC significantly increased the likelihood of recurrence.
Conclusion: Hookwire guided BCS at CMJAH has acceptable margin adequacy and re-excision rates compared to international standards. The higher recurrence rate likely results from delayed adjuvant radiation access. TNBC molecular subtype was a significant tumour-specific risk factor increasing recurrence risk.
Assessing the shift in breast cancer stage from anatomical staging classification to the clinical prognostic staging system in a low middle-income country
R Thomas, T Augustine, N Mabe, J Edge
Faculty of Health Sciences, University of the Witwatersrand, South Africa
Introduction: There is a trend to incorporating tumour biology into the traditional TNM staging system for breast cancer. The study investigates the change in breast cancer stage when using the anatomical staging system compared to the clinical prognostic staging system.
Objectives: We assessed whether the stage at diagnosis changed significantly when the biology of the tumour was included in the staging system.
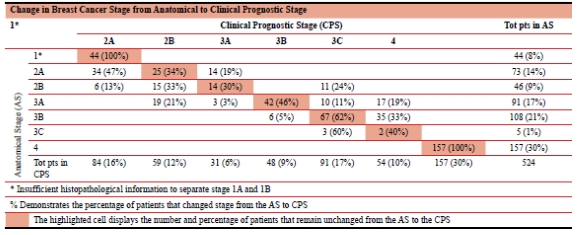
Method: This is a single-centre pilot study using South African Breast Cancer and HIV Outcomes (SABCHO) database from the CMJAH Breast Unit. This study evaluated all newly diagnosed breast cancers from 01.01.2022 to 31.05.2024. HREC WITS M250463
Results: Five hundred and twenty-four cancers in 521 patients met inclusion criteria for this study. The mean age was 54 (20-94). Sixteen percent of our population is RVD reactive with median age of diagnosis of 48 yrs, at least 6 years earlier than their RVD non-reactive counterparts. The most common histological subtype was Invasive carcinoma of no special type (91.98%). In our population our most common molecular subtype was Luminal B (35.36%), Luminal A (31.43%), TNBC (21.22%) and HER2 Enriched (11.98%). Using the anatomical TNM classification, 44 patients (8%) were stage 1, 73 patients (14%) stage 2A, 46 patients (9%) stage 2B, 91 patients (17%) stage 3A, 108 patients' stage 3B (21%), 5 patients (1%) stage 3C and 157 patients (30%) stage 4. When clinical prognostic staging was used, our study demonstrated significant changes in breast cancer stage, with stage 2 demonstrating about 65% change (either up/down-staged) and stage 3 demonstrating about 50% change from the anatomical stage to the clinical prognostic stage.
Conclusion: Our data resembles that of international literature1. There is a potential impact on management, especially due to the significant change in the Stage 2B and 3A which were down-staged by 46% and 24% respectively.
Profile of tobacco usage amongst breast cancer patients at a tertiary academic hospital in South Africa
PC Mapunda, T Naidoo, MZ Koto
Department of General Surgery, Sefako Makgatho Health Sciences University, South Africa
Introduction: Breast cancer is now the most common malignancy among South African women, with a rising incidence that has surpassed cervical cancer in mortality. Despite strong evidence linking tobacco exposure to breast cancer, limited local data exists on the prevalence and patterns of tobacco use in this population.
Aim: To determine the prevalence of tobacco use in this patient population and explore the potential correlation between smoking and breast cancer.
Materials and methods: A retrospective cross-sectional study was conducted at the Breast Clinic of Dr George Mukhari Academic Hospital (DGMAH), including all female patients aged > 18 years with histologically confirmed breast cancer from 1 January 2020 to 31 December 2023.
Results: There are significantly more non-smokers than smokers among the African population (99.4% vs 0.6%; p = 0.002). Within the white population, there are more smokers than non-smokers (93.9% vs 4.1%; p = 0.026). The mean age was 54.9 years for the participants who identified as smokers and 53.7 years for those who reported being non-smokers. Most patients reported using smokeless-sniffing-tobacco (68.7%) rather than smoking cigarettes (30.3%). There were statistically significant differences observed in the luminal subtypes between smokers and non-smokers. Statistically significant differences were observed in the prevalence of the triple-negative subtype between smokers and non-smokers (18.4% vs 9.9% respectively).
Conclusions: This study found that tobacco use is prevalent among breast cancer patients at DGMAH in South Africa. The predominant form of tobacco consumption is smokeless tobacco. Additionally, this study provides evidence of an association between triple-negative breast cancer and smoking.
HER-2/NEU overexpression and clinicopathological features of breast cancer in treatment naïve breast cancer patients at a tertiary hospital in Gauteng
LC Makhuvha, DH Mokone, NC Kalenga
Department of General Surgery, Sefako Makgatho Health Sciences University, South Africa
Aim: Breast cancer is a significant global health concern. HER2 overexpression, found in 15-20% of invasive cases, is associated with poorer prognosis, higher tumour grade, larger size, and increased metastasis. To determine the relationship between the HER-2 receptors and the clinicopathological features of breast cancer in patients at a tertiary hospital.
Methods: A retrospective cross-sectional review was done of patients' records at the breast oncology clinic over five years. The study population comprised all newly diagnosed breast cancer patients seen at Breast Oncology Clinic from 01 June 2018 to 30 June 2023.
Results: The study included 206 patients with HER2-positive breast cancer. Findings revealed that 24.15% were HER2-positive, with most having T4 tumours (69.42%). T2 and T3 tumours were less common (both 13.11%), while T1 and T0 tumours were rare (3.88% and 0.49%, respectively). The majority (67.29%) had regional lymph node involvement, with 37.86% classified as N1 and 26.21% as N2. Distant metastasis was observed in 18.45% of patients. Most graded patients were grade 2 (52.78%), followed by grade 3 (38.89%). In terms of Ki67 index, 51.26% had < 20%, 36.68% between 20-50%, and 12.06% > 50%.
Conclusion: The incidence of HER2-positive breast cancer was determined to be 24.15% and is associated with aggressive traits, including larger tumour sizes, lymph node involvement, distant metastases, and high tumour grading. HER2-enriched cancers are more aggressive than HER2 luminal B subtypes. A thorough study in diverse and underrepresented populations could reveal regional differences in incidence and outcomes.
Microductectomy under local anaesthetic for pathological nipple discharge. Is it time to change practice?
A Khamajeet
Department of General surgery, Groote Schuur Hospital, University of Cape Town, South Africa
Background: Pathological nipple discharge (PND) is a common clinical concern that requires careful evaluation to rule out malignancy. Microductectomy is the gold-standard surgical intervention for both diagnosis and symptom relief. In most centres, it is usually performed under general anaesthesia. This study aims to assess the feasibility, efficacy, and safety of performing microductectomy under local anaesthesia without sedation, a technique adapted during the COVID-19 pandemic to address resource constraints.
Methods: A retrospective review was conducted on all patients who underwent microductectomy under local anaesthesia at Groote Schuur Hospital between January 2021 and December 2022. Data were collected on demographics, imaging used, imaging findings, biopsy results, and histological diagnoses.
Results: A total of 23 patients were included, with a median age of 55 years (IQR 45-60). All patients presented with spontaneous nipple discharge (ND), with 75% reporting bloody ND. Dual imaging (mammography and ultrasound) was performed in 78.2% of cases, while 39.1% of patients underwent preoperative biopsy. Histology revealed intraductal papilloma in 65.2% of cases, ductal hyperplasia in 39.1%, and ductal ectasia in 21.7%. One patient (4.3%) was diagnosed with papillary ductal carcinoma in situ (DCIS). No invasive malignancy was detected, and no complications were reported postoperatively.
Conclusion: Microductectomy conducted under local anaesthesia without sedation appears to be a safe, effective, and minimally invasive method for managing PND. It benefits resource-limited settings by decreasing reliance on general anaesthesia while preserving diagnostic and therapeutic efficacy. Further prospective studies with larger sample sizes incorporating patient satisfaction, procedure duration, diagnostic yield, recurrence rates, and completeness of excision are advised to evaluate long-term outcomes and patient experiences.
Acute pain management in trauma patients at a tertiary academic hospital in the Gauteng Province: a prospective cross-sectional observational study
S van der Spuy, P Daya, S Leathwhite, Z Mangena, T Motaung, M Naidoo, A Pretorius, TE Luvhengo
Unit of Undergraduate Medical Education, Department of Surgery, University of the Witwatersrand, South Africa
Background: Poorly managed pain increases the risk of complications in patients admitted following trauma or a surgical procedure. This study investigated how effectively pain is managed in patients admitted to our trauma unit.
Patients and Methods: This was a prospective observational study and participants were patients admitted following trauma. Data collected included demography, nature of injury, co-morbidities and pain, depression and anxiety screening scores. Adequacy of pain control was assessed using the Numeric Rating Scale (NRS). Statistical analysis included tests of associations between pain management adequacy and comorbidities. A p-value < 0.05 was deemed statistically significant. The study received ethical clearance (M231036 MED23-10-26).
Results: The study included 143 participants with 81.1% (116) males, and 33.9% (48) admitted following penetrating injury. Most, 78.6% (112) of the participants with severe pain were treated with paracetamol and/or Tramadol. Majority, 62.9% (90) of the participants reported moderate to severe pain despite treatment. Co-morbidities had no statistically significant influence on pain perception and adequacy of pain control (p > 0.05). Similarly, anxiety, depression and history of prior substance use had no statistically significant influence on adequacy of pain control (p > 0.05).
Conclusion: Paracetamol and tramadol are the most frequently prescribed analgesic drugs in the trauma unit regardless of the severity of acute pain, and 63% of the patients experience moderate to severe pain despite treatment. The mechanism of injury, co-morbid conditions, depression and anxiety levels, and history of drug abuse do not influence the intensity of pain perception before or after administration of analgesics.
Investigating stemness and cell cycle progression: A combined flow cytometry approach in TNBC cell lines
MS Mothupi,1 L Khambule,2 TN Augustine,3 KR Xulu1
1 Department of Anatomical Sciences, School of Biomedical Sciences, University of the Witwatersrand, South Africa
2 Department of Chemical Pathology, School of Pathology, University of the Witwatersrand, South Africa
3 Department of Anatomical Pathology, School of Pathology, University of the Witwatersrand, South Africa
Background: Triple-negative breast cancer (TNBC) is an aggressive breast cancer subtype lacking hormone receptors. It is classified into six molecular subtypes, with basal-like types being the most common. Basal-like 1 (BL 1) is marked by high expression of cell cycle and DNA repair genes, while basal-like 2 (BL 2) is enriched in growth factor signalling. TNBC's aggressiveness is driven by uncontrolled proliferation, partly due to the evasion of quiescence and the presence of cancer stem cells, which typically express CD24, CD44, and CD133 surface markers.
Aim: To investigate the relationship between stemness-associated surface marker expression and cell cycle progression in TNBC cell lines
Methods: MDA-MB-468 (BL 1) and MDA-MB-231 (BL 2) cells will be cultured in DMEM with 10% FBS and 0.1% penicillin-streptomycin at 37°C and 5% COi. To perform the combined analysis of surface marker expression and cell cycle progression, cells will be labelled with CD24-AF647, CD44-FITC, and CD133-BV421. Following staining, cells will be fixed and incubated overnight. The next day, they will be stained with FxCycle™ PI/RNase Solution at room temperature for 30 minutes in the dark. Data will be acquired using the LSR Fortessa flow cytometer and analysed statistically.
Ethics: W-PR-20240801-01(HREC, Wits)
Results: The analysis is expected to reveal an increased expression of the markers (CD44 and CD133) in the G2/M phase, indicating their involvement in cell proliferation. Additionally, differences in stemness are expected between the BL 1 and BL 2 phenotypes of TNBC.
Conclusion: This study will highlight the interplay between stemness and cell cycle progression in TNBC.
Nonoperative management of penetrating liver trauma
K Kapnias (medical student),1 PH Navsaria,1 S Saar,2 M Kivilo2
1 Trauma Centre, Groote Schuur Hospital, University of Cape Town, South Africa
2 University of Tartu, Estonia
Background: Nonoperative management (NOM) of penetrating liver injuries is infrequently practised. The aim of this study was to assess the safety of selective NOM of penetrating liver injuries.
Patients and Methods: A prospective, protocol-driven, HREC approved study, was conducted over a 52-month period (April 2015-July 2019). Patients with right-side thoracoabdominal, and right upper quadrant (RUQ) penetrating wounds with or without localized RUQ tenderness underwent contrasted abdominal CT scan evaluation to detect the presence of a liver injury. Patients who required immediate laparotomy were excluded from the study. Outcome parameters included need for delayed laparotomy, complications, length of hospital stay and survival.
Results: Seventy-seven patients (53 gunshot and 24 stabbed) with liver injuries were selected for nonoperative management. The mean injury severity and PATI scores were 18.9 (range 1-75) and 9.2 (range 1-25), respectively. Simple liver injuries (Grades I and II) occurred in 33 (42.9%) patients and complex liver injuries occurred in 44 (57.1%) patients.
Associated injuries included 25 (32.5%) kidney, 45 (58.4%) diaphragm, 53 (68.8%) lung contusion, 38 (49.4%) rib fractures, and 58 (75.3%) hemo/pneumothorax. Liver-related complications included: bile leak (7), biliary fistula (4), liver abscess (3), hepatic artery false aneurysm (3), biloma (2), hepatic AV fistula (1), and hepatic subcapsular haematoma (1). Five (5) patients required delayed laparotomy. The overall median hospital stay was 6 [IQR: 4-9] days. The successful nonoperative management rate was 93.5%.
Conclusion: The nonoperative management of appropriately selected patients with penetrating liver injuries is safe and associated with minimal morbidity.
Multi-omic analyses of the tumour microenvironment of South African pancreatic ductal adenocarcinoma patients
S Dubazana,1 P Naicker,2 S Ngwenya,3 N Elebo,1 J Omoshoro-Jones,1 S Buthelezi,4 EE Nweke1,5
1 Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, South Africa
2 Department of Proteomics, ReSyn Biosciences, South Africa
3 Division of Anatomical Pathology, School of Pathology, Faculty of Health Sciences, University of the Witwatersrand, South Africa
4 Department of Future Production: Chemicals, Council for Scientific and Industrial Research, South Africa
5 Department of Life and Consumer Sciences, College of Agriculture and Environmental Sciences, University of South Africa, South Africa
Background: Pancreatic ductal adenocarcinoma (PDAC) ranks among the most aggressive malignancies globally, with a 5-year survival rate of only 13%. This study conducted multi-omic analyses of archived FFPE tissues to identify potential biomarkers and elucidate molecular mechanisms of disease progression in our patient population.
Methods: For the proteomics aspect, a comparison of sample preparation methods (Barocycler, Pixul+DTT, Pixul+Sonication and Pixul-only) was conducted for optimal protein extraction. Using the selected optimised method, 78 FFPE PDAC (22 paired tumour and normal, 34 unpaired tumour) tissues were processed to determine differentially expressed proteins. Limma was used for the differential expression analyses. DNA and Total RNA were subsequently extracted from 28 tissues (14 paired tumours and normal tissues) and Whole exome and RNA sequencing were performed, respectively.
Results: The Pixul+Sonication method yielded the highest number of identified proteins (20,804.5 peptides and 3,349.5 protein groups) followed by the Pixul-only method with 20,769,5 peptides and 3,300.5 protein groups). The difference between methods was insignificant; we chose the Pixul-only workflow for its high-throughput efficiency and minimal steps, reducing error probability. From the FFPE PDAC tissues, a total of 39 dysregulated proteins (17 downregulated and 22 upregulated) were identified. Key pathways such as extracellular matrix organisation, platelet activation and fibrosis-related pathways were identified.
Conclusion: Utilising this optimised method, key proteins and pathways associated with PDAC progression were demonstrated. These findings underscore the potential of archived tissue-based proteomic analysis for biomarker discovery, providing critical insights into PDAC pathophysiology and novel therapeutic targets. The analyses of the sequencing data are ongoing.
Outcomes and complications of traumatic bladder injuries: a retrospective review of a level 1 trauma centre
S Makhadi, T Ubisi, MS Moeng
University of the Witwatersrand, South Africa
Background: Management of bladder injuries in LMICs varies, with mortality rates of 2.3% in Nigeria and 5% in South Africa. Bladder injury repair complications are higher in LMICs (2.25%) compared to HICs (3.9%). Few studies have evaluated outcomes in LMICs; this study aims to assess traumatic bladder injury outcomes at Charlotte Maxeke Johannesburg Academic Hospital, contributing to the limited literature.
Methods: A retrospective review over 6 years (2015-2019) included adult trauma patients with diagnosed bladder injuries, excluding iatrogenic cases. Data on demographics, injury mechanism, injury type, diagnostics, management, and associated injuries were analysed using STATA version 18, with statistical significance set at p < 0.05.
Results: Blunt trauma caused 46.05% of injuries, primarily from motor vehicle accidents. Penetrating trauma accounted for 51.32%, mainly gunshot wounds. Most injuries were extraperitoneal (39.47%) or intraperitoneal (38.16%). Management involved conservative treatment in blunt cases and surgical repair, often two layers, mainly using absorbable sutures. Outcomes highlight the variability in injury mechanisms and management approaches in this LMIC setting.
Conclusion: This study underscores the diverse injury mechanisms and management strategies for bladder injuries in LMICs, with outcomes influenced by mechanism, injury severity, and resource availability. The relatively high complication rates emphasise the need for standardised protocols and improved trauma care systems. Enhancing diagnostic facilities and surgical training could improve patient outcomes. Overall, these findings contribute critical data to the limited literature on bladder injury management in LMICs, advocating for resource-appropriate strategies to reduce morbidity and mortality associated with traumatic bladder injuries in such settings.
The efficacy of glycerol processing method in the preparation and Preservation of human amniotic membrane
C Ndhlovu
University of the Witwatersrand, South Africa
Background: Human amniotic membrane (hAM) is a widely used biological dressing for burn care due to its antimicrobial, moisture-retentive, and biocompatible properties. In low-resource settings with limited cadaveric skin availability, optimised preservation methods are essential.
Aim: This study aimed to evaluate the efficacy of a glycerol-based processing method in preserving the structural and functional integrity of hAM.
Methods: This in vitro experimental study was conducted at MagiTech Science Laboratories and Charlotte Maxeke Johannesburg Academic Hospital. hAM samples from 142 donors were processed using > 99.5% molecular biology-grade glycerol with slow agitation (100 rpm) at 37 °C for 3 hours, repeated three times with saline rinses. Paired unprocessed and processed samples from 71 placentas were tested for tensile strength and strain (Instron 5966), transparency (PerkinElmer Lambda 750s), thickness (digital calliper), and antimicrobial activity (disk diffusion against five burn-related bacteria). Statistical analyses included paired t-tests, repeated measures ANOVA, and Cohen's d.
Results: Processed hAM showed a non-significant 3.66% reduction in tensile strain (p = 0.262) and a modest 6.6% decrease in strength. Transparency significantly improved (90.82% to 97.07%, p < 0.0000000000589; d = 0.92).
Although thickness reduction was significant (p = 0.001), the actual change (0.001 mm) was clinically negligible (d = 0.50). Antimicrobial activity varied by species, with strongest inhibition against S. aureus and K. pneumoniae (p < 0.001).
Conclusion: Glycerol processing effectively preserves and enhances the functional characteristics of hAM, particularly transparency and antimicrobial efficacy, without clinically significant compromise to mechanical strength or thickness. These findings support the utility of processed hAM as a viable and scalable biological dressing for burn wound management in resource-limited settings.
Audit and application of Clavien-Dindo classification to complications in a Major Trauma unit in Johannesburg: Our early experience
HD Makhubele, MS Moeng, TE Luvhengo
Department of Surgery, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, South Africa
Background: The Clavien-Dindo classification is derived from five traditional grades. These are therapies used to adjust or correct a specific complication and rank a complication in an objective and reproducible manner. The primary aim and outcome of this study was to audit, evaluate and apply the CD classification to complications of patients who presented and were admitted to Charlotte Maxeke Johannesburg Academic Hospital (CMJAH).
Methods: Data was collected retrospectively from 1 January 2018 to 31 December 2019. We excluded all patients under the age of 18 years and patients whose clinical records were incomplete or missing. This data was from hospital databases and CMJAH surgery Redcap. The association between each continuous variable and complication was evaluated using the Pearson's chi-square or Fisher's exact test. A P-value < 0.05 was considered statistically significant. STATA version 16 was used for analysis. Ethics clearance was granted by HREC of the University of the Witwatersrand (M221189).
Results: 196 records met inclusion criteria, from which 87.2% were male. Their median age was 32 years. Complications were reported in 2.2% of the patients and the most frequent complication was wound infection 21%. Complications were related to a surgical procedure in 64.8% across all CD grades of complications, which was statistically significant (p-value 0.002). 34.18% of the patients had CD Grade 1 complications. The overall mortality was 9.2%. Table 1 outlines the breakdown of demographics and related complications
Conclusions: We found the application of the Clavien-Dindo classification to our complication rates allowed for better quantification of the morbidities seen in trauma, and enhanced our quality control measures.
Intensive care patient outcomes at a tertiary academic institution in the western Cape in South Africa using a cloud-based international electronic registry
HA Tariq,1 J Piercy,2 A Beane,3 I Joubert,2 D Thomson1,2
1 Department of Surgery, Groote Schuur Hospital, University of Cape Town, South Africa
2 Division of Critical Care, Groote Schuur Hospital, University of Cape Town, South Africa
3 Centre for Inflammation Research, University of Edinburgh, Scotland, United Kingdom
Background: Intensive care unit (ICU) registries are databases collecting standardised data from participating ICUs for outcomes monitoring, quality improvement (QI), and inter-ICU comparisons. South Africa lacks a coordinated ICU registry. APACHE II and Electronic Tropical Intensive Care Score (eTropICS) are clinical scoring systems that quantify illness severity and predict mortality in critically ill patients.
Aim: This study describes the case mix, ICU admission, and outcomes over six months using an international cloud-based electronic registry.
Methods: A retrospective study of prospectively collected data from ICU admissions at Groote Schuur Hospital (GSH). Dedicated data capturers collected data for the Critical Care Africa Asia (CCAA) ICU registry. Automated reports provided demographics, quality indicators, and outcomes. APACHE II scores and eTropICS were calculated and standardised mortality ratios (SMR) was produced for each score. The University of Cape Town (UCT) human research ethics committee approved the research protocol (HREC:536/2023).
Results: Data were captured for 758 patients in 5 ICUs. 61.70% were male, with a median age of 40 years. The median length of stay was 4 days (IQR 3-8). 74.08% required respiratory support, and 10.82% needed inotropic support. ICU mortality was 10.42%, and overall in-hospital mortality was 11.35%. eTropICS predicted higher ICU mortality (SMR < 1), while APACHE II predicted lower mortality (SMR > 1).
Conclusion: This study, using an electronic registry with data capturers, described critically ill patients in South Africa and reported outcomes, providing a basis for future research. We showed a difference in SMR assessments between the two scoring systems.
Investigating the association of procalcitonin levels and mortality in severely injured trauma patients
TB Kgalema, F Paruk, T Mulaudzi
University of Pretoria, South Africa
Background: In severely injured trauma patients, the risk of developing complications and mortality risk is very high. This is driven by the substantial systemic inflammatory response (SIRS) to the injury. Prompt recognition and aggressive treatment of the underlying injury or insult dampens the magnitude of the SIRS response. Procalcitonin (PCT), a pro-inflammatory biomarker, is usually elevated early in the inflammatory phase post traumatic injury.
Objectives: To investigate the association between PCT levels and mortality in severely injured trauma patients within the first seventy-two (72) hours; as well as to determine the level of PCT that offers the best predictor cut-off value for mortality. Additionally, to determine the association between injury severity score (ISS) on the first day, in predicting mortality and whether the change in PCT levels (difference between day 3 and day 1 procalcitonin), has an impact on mortality.
Methods: This study is a retrospective cohort study, to be conducted at Steve Biko Academic Hospital. A random consecutive sample of trauma patients admitted to the Steve Biko Academic Hospital surgical high dependency units (intensive and high care units) from 01 January 2019 to 31 December 2023. The sample size for the study is 266 patients.
Results: 501 trauma patients were admitted to the surgical high dependency units (SHDU) during the study period. 266 patients met the inclusion criteria for the study, of which 86% of the patients were males, with a mean age of 36.33±11.50 years. The average ISS was 27.92±10.17 with a mean length of SHDU stay of 12.69±9.88 days. Motor vehicle accidents accounted for 38%; pedestrian vehicle accidents accounted for 26%; penetrating trauma 23%; blunt trauma and other mechanism of injury accounted for 7% each of the overall cases. The mean PCT was significantly higher in the demised group (non-survivors) as compared to the survivors (p < 0.001: 89.91 vs 29.56). The mean marginal effect for mortality of 60.35, is significant (p < 0.001), demonstrating an association between PCT and mortality. PCT levels were also significantly higher at 24, 48 and 72 hours post traumatic injury, in the demised group. The level of PCT that yielded the best predictor cut-off at 24 hours was PCT > 7.133; at 48 hours it was PCT > 6.256; and at 72 hours is PCT > 5.073. The change in PCT levels (the difference between PCT levels at 72 and 24 hours) was -0.900 vs 0.120 (p < 0.004) for survivors and non-survivors respectively. The ISS was lower in survivors, being 26.14 vs 31.84 (p < 0.001) in non-survivors respectively.
Conclusion: This study confirms that in the first seventy-two hours following traumatic injury, there is an association between PCT and mortality. There is also a significant association between the change in PCT within the first seventy-two hours and mortality. Among the patients that survived, PCT levels stabilised while in the demised group PCT levels continued to rise. A high ISS is also associated with a higher mortality risk.
Prevalence, microbiological cultures and impact of intra-abdominal sepsis in ICU trauma patients at Charlotte Maxeke Johannesburg Academic Hospital
J Huang, D Kruger, MS Moeng
University of the Witwatersrand, South Africa
Background: Intra-abdominal infections following trauma-related relook laparotomies are associated with significant morbidity and mortality, especially in low- and middle-income countries (LMICs) where interpersonal violence drives high rates of penetrating injuries. Managing these infections effectively requires understanding pathogen profiles and antibiotic resistance patterns.
Aim: This study aimed to identify the microorganisms present in trauma-related relook laparotomies, evaluate their antibiotic sensitivity, and assess the impact of intra-abdominal infections and sepsis on 28-day mortality and hospital length of stay.
Methods: This retrospective study analysed adult trauma patients requiring relook laparotomies admitted to the ICU at Charlotte Maxeke Johannesburg Academic Hospital between January 2018 and December 2019. Data on demographics, injury type, pathogens, antimicrobial use, and outcomes were collected. Statistical analysis was conducted using STATA V14.5. A p-value of 0.05 was considered significant.
Results: Of 137 patients (90.5% male, 83.2% with penetrating trauma), 62.8% developed intra-abdominal infections, with Gram-negative bacilli as the predominant pathogens. Antibiotic sensitivity declined with repeated laparotomies, indicating increased resistance. Patients receiving empiric antibiotics had higher rates of mortality, septicaemia and infections. Intra-abdominal sepsis significantly extended hospital stays and increased 28-day mortality, while septicaemia showed no clear correlation with mortality.
Conclusion: Intra-abdominal infections remain a critical challenge in trauma care, especially in LMICs. The progressive rise in antimicrobial resistance with successive procedures emphasises the need for targeted therapies and robust antibiotic stewardship. Optimised surgical management and infection control strategies are essential for improving outcomes. Further research is needed to explore the link between intra-abdominal infections and systemic sepsis in resource-limited settings.
Relook laparotomy and laparoscopy - A review of practices in a resource-limited setting
NC English, L Pohl, DB Nel, A Boutall, JC Kloppers
Department of Surgery, University of Cape Town, South Africa
Introduction: Non-trauma relook laparotomy/laparoscopy are commonly performed. It increases complications and costs.
Aim: To review current practices of relooks at a multi-centre, resource-constrained academic institution.
Methodology: Retrospective review of prospectively collected data from 01/2021-01/2022. Primary outcomes included the incidence of relooks, hospital length-of-stay (LOS), and 30-day morbidity and mortality rates. Multivariate logistic regression models were constructed to determine predictors of relooks and factors associated with mortality. The study protocol was approved by the UCT HREC (HREC/REF: 429/2022).
Results: Of 931 patients included, 107 (11.5%) underwent relooks. Relook patients were older (44.7 vs. 39.3 years; p < 0.05) and more likely male (70.1% vs. 53.5%; p < 0.05) compared with non-relooks. Relook patients had a significantly longer index operation (116.0 vs. 94.4 minutes; p < 0.05) which was more likely via laparotomy (53.3% vs. 43.2%; p < 0.05). Compared with non-relooks, relook patients experienced more deep surgical site infections (12.1% vs. 1.9%; p < 0.05), had significantly longer LOS (19.1 vs. 6.8 days, p < 0.05), and a > 3-fold higher mortality rate (23.4% vs. 7.5%; p < 0.05). In addition to older age and male sex, intra-abdominal contamination conferred increased odds of undergoing a relook (AOR 3.04, 1.901-4.856; p = 0.001). Those who demised following relooks were more likely ASA III (48.0% vs. 8.5%; p < 0.05) and inotropic-dependent during their index operation (28.0% vs. 3.7%; p < 0.05) compared with their counterparts. Finally, undergoing > 2 relooks (AOR 4.416, 1.200-16.792; p = 0.038) and planned relooks (AOR 5.839, 1.075-32.556; p = 0.025) were associated with mortality.
Conclusion: Older age, male sex, prolonged index operation, and intra-abdominal contamination were associated with relooks. Undergoing multiple and planned relooks were predictors of mortality.
Assessing patient knowledge and practices in diabetic foot ulcer prevention
T Mukheli,1 TP Mokoena,2 A Fourie,3 SB Kagodora,4 TE Luvhengo5
1 Oral Health and Therapeutic Services, Gauteng Department of Health, South Africa
2 Department of Podiatry, Charlotte Maxeke Johannesburg Academic Hospital, South Africa
3 Department of Physiotherapy, Charlotte Maxeke Johannesburg Academic Hospital, South Africa
4 University of the Witwatersrand, South Africa
5 Department of Surgery, School of Clinical Medicine, Faculty of Health Sciences, Charlotte Maxeke Johannesburg Academic Hospital, University of the Witwatersrand, South Africa
Background: Diabetic foot disease is a major complication of diabetes mellitus, characterised by neuropathy, ischemia, and infection leading to foot ulceration and potential amputations. Despite the availability of evidence-based guidelines for diabetic foot care, gaps in patient knowledge and practices contribute to the high prevalence of foot ulcers and amputations.
Objective: This study aims to assess the knowledge of diabetic mellitus patients regarding diabetic foot care.
Methods: A descriptive cross-sectional observational study was conducted at public healthcare facilities within the Charlotte Maxeke Johannesburg Academic Hospital Cluster (CMJAH) in Gauteng Province, South Africa. Surveys were administered to diabetic mellitus patients attending these facilities, and data were analysed using descriptive and inferential statistics. The study received prior ethics approval (M190563).
Results: Most participants were female (70%) and had primary education (61%). Type II diabetes patients demonstrated significantly higher good knowledge about foot care (85%) compared to Type I patients (15%), with the difference being statistically significant (p = 0.007). The duration of diabetes significantly affected knowledge levels; those diagnosed for less than ten years had a higher proportion of bad knowledge compared to only 5% in patients diagnosed for over thirty years (p = 0.047). Treatment methods also influenced awareness; patients using insulin alone compared to those on oral medications or a combination had varied awareness of foot care, with statistically significant differences (p = 0.002). Age also played a role in awareness, with older participants being statistically less knowledgeable regarding appropriate foot care than the younger ones (p = 0.0033).
Conclusion: Significant gaps in patient knowledge regarding diabetic foot care were identified, and education from healthcare providers emerged as a critical factor influencing knowledge levels.
Investigating the role of HIV status on outcomes of emergency abdominal surgery
J Gqada, A Boutall
Division of General Surgery, University of Cape Town, South Africa
Introduction: Despite advances in diagnostic modalities and surgical techniques, the morbidity for emergency laparotomy is high, and mortality is in the order of 15%. Approximately 71% of the world's HIV positive population reside in sub-Saharan Africa, where HIV/AIDS remains a common cause of death despite increasing access to anti-retroviral therapy. In patients requiring acute surgical intervention, there is no opportunity to optimise their nutritional state, further compounding their immunocompromised state. We therefore hypothesised that HIV positive patients who undergo emergency abdominal surgery may have an increased morbidity and mortality.
Methods: Outcome data of consecutive patients who underwent emergency abdominal surgery in the hospitals of the Cape Metro West Subdistrict over a 1-year period were prospectively collected. A retrospective analysis was performed of outcome differences between the HIV positive (+) and HIV negative (-) cohort. Approval for the study was granted by the UCT Faculty of Heath Sciences Human Research Ethics Committee (UCT HREC 076/2023).
Results: 1477 patients underwent emergency abdominal surgery during the study period in question. 160 patients were confirmed HIV+ and 486 were confirmed HIV-. There was no significant difference between the HIV+ and HIV- cohort with regards to 30-day mortality (5.6% vs 8.5% respectively), length of hospital stay (6 vs 5 days respectively), postoperative ICU admission (10% vs 10.9%), or blood transfusion. The HIV+ group had a higher morbidity rate (36.3% vs 27.7%).
Conclusions: HIV status alone cannot be used as an independent risk factor for differential outcomes after emergency abdominal surgery. Widespread access to antiretroviral therapy may contribute to this. More research is required to assess the role of viral load.
Major amputation and mortality in diabetic foot sepsis: a retrospective cohort study
S Hartmannsgruber,1,2 BD Katusica,3 K Chiman,3 DM Fleishman,1,4 B Hart,1,2 MC Molewa,1,2 TE Luvhengo2
1 Edenvale Regional Hospital, South Africa
2 University of the Witwatersrand, South Africa
3 University of Pretoria, South Africa
4 University of Cape Town, South Africa
Background: Diabetic foot sepsis (DFS) is the leading cause of lower extremity amputation (LEA), significantly contributing to morbidity and mortality. The global variation in 3-year survival rate ranges from 20% to approximately 70%, which underscores the urgent need for enhanced data surveillance and targeted management strategies. This study investigated the association between level of amputation and various other factors with the 3-year-mortality rate in patients who received surgical treatment for DFS.
Methods: Retrospective study of cohort of patients managed over a 4-year period with DFS. Further data was collected through telephonic interviews. Mortality data was collected through telephonic interviews with family members of the deceased patients. Data collected included demographic information, baseline clinical parameters and levels of amputation(s). The study received ethics approval (M190563).
Results: Records of 101 patients were found and 59% were male. The mean age of patients was 58 years. The 3-year-mortality rate was 24.7%. Association of major amputation and mortality was not statistically significant, unlike age, HbA1C and serum albumin level. Adjusted survival curves demonstrated no significant difference in mortality by level of amputation or gender. Two thirds (17/25) of mortalities occurred within the first 6 months post LEA and diabetic associated causes of mortality accounted for 84% (21/25) of deaths.
Conclusions and Relevance: Major level of amputation did not influence 3-year mortality. Most deaths occurred within the first 6 months post-operatively. Improved access to diabetic health services and focused allied healthcare at a primary and secondary level would likely limit disease progression, improve patient compliance and mortality rates.
Mortality and morbidity of appendectomy in a low to middle income urban district
C Keen, S Rayamajhi, C Kloppers
University of Cape Town, South Africa
Background: Appendicitis is the most common abdominal emergency globally. The aim is to evaluate mortality of appendectomies in a low to middle income urban center (LMIC) and identify predictors of poor outcomes.
Methodology: A retrospective analysis of a multi-center, prospectively maintained, ethics approved registry over a one-year period (January 2021-January 2022) in four hospitals in the Western Cape metropole serving a population of around five million. Ethics reference number 206/2023. Logistic regression analysis was used for a multivariate analysis.
Results: A total of 438 patients had an appendectomy of which 63.7% were complicated appendicitis. The mean CODMAN risk-score pre-operatively was 4.04. The surgery was performed laparoscopically in 374 with 44 converted. The median time to surgery from admission in the uncomplicated appendicitis cohort was 1.6 days and 1.2 days for the complicated. No significant difference in timing to surgery and morbidity (p = 0.88) and mortality (p = 0.27). The mean length of hospitalisation was 5.21 days. Fifty cases were relooked and the majority were on demand. At relook surgery, the main findings were collections, both pus and serous (72%). Seventy-six (17.4%) cases of surgical complications, classified by Clavien Dindo (grade 1-5), were noted. The overall mortality at 30 days was 3.0%. Thirty day morbidity included percutaneous drains (2.7%); intra-abdominal collections (4.1%), surgical site infections (6.7%) and enterocutaneous fistulas (0.2%).
Conclusion: In LMIC settings complicated appendicitis appears to be prevalent with a high mortality and morbidity rate. Higher age, BMI, ASA score more than two and presence of perforation significantly predicted worse outcomes.
Outcomes of complicated acute appendicitis at a central academic hospital in Johannesburg South Africa
I Bogiages, T Luvhengo, D Kruger
University of the Witwatersrand, South Africa
Background: Laparotomy remains the most practiced approach for complicated appendicitis in some countries, including South Africa. This study compared the outcomes of patients who had a laparotomy or laparoscopic surgery for complicated acute appendicitis.
Methods: A retrospective review of patient records that had either a laparotomy and appendectomy or a laparoscopic appendectomy was undertaken. Data collected included demographic information, duration of symptoms, length of hospital stay, time to surgery, type of surgery, need for ICU admission, number of relooks, microbiology and outcomes.
Results: Records of 200 patients of whom 62 patients (31.0%) had a laparoscopic appendectomy and 138 patients (69.0%) had an open appendectomy were included. Eighty-two patients (59.4%) who had an open appendectomy had a midline laparotomy. Postoperative complications developed in 46.4% of laparotomy vs 17.7% of laparoscopy patients (p < 0.001). The mortality rate was 9.5% overall, with significantly higher mortality in the laparotomy group at 13.0% vs 1.6% in the laparoscopic group (p = 0.009). Patients who died had significantly higher rates of complications and need for relook surgery (p < 0.001). Histology showed a normal appendix in 13/138 patients (9.4%), granulomatous lesions and parasitic infection each in 5 patients (3.6%).
Conclusion: The majority of patients with complicated acute appendicitis had a appendectomy via laparotomy and this group of patients developed significantly more postoperative complications. The mortality rate was also significantly higher in patients who underwent a laparotomy.
Thirteen consecutive years of adolescent hepatocellular carcinoma at Groote Schuur Hospital, Cape Town, South Africa
I Kim, S Sobnach, U Kotze, M Bernon, E Jonas
Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
Aim: Hepatocellular carcinoma (HCC) is a fatal disease, often affecting young adults in South Africa. Adolescent HCC is rare, with limited data in the current literature. The aim of this study is to present our experience with adolescent HCC at a major academic centre in sub-Saharan Africa.
Methodology: Adolescent (age:10-19 yr.) patients treated at Groote Schuur Hospital from 2012 to 2024 were studied. Data were extracted from a prospectively maintained database and included the following: demographics, clinical presentation, investigations, treatment and survival.
Results: Of the 726 HCC patients treated at Groote Schuur Hospital, five (0.5%) were adolescents. Three were females and the median age at presentation was 18 (IQR:17-19) years. The aetiology of HCC was chronic hepatitis B virus (HBV) infection in all five. Pain was the predominant symptom (60%), and an abdominal mass was the main clinical finding (40%). All patients had advanced disease, with four (80%) having Barcelona Clinic Liver Cancer (BCLC) stage C disease and one (20%) had BCLC stage D disease. Two (40%) patients had extrahepatic metastases and three (60%) had portal vein tumour thrombosis. Treatment modalities included liver resection (1), sorafenib (1), Lenvatinib (1) and best supportive care (2). At the time of this study, only one adolescent was alive and the median survival of the cohort was 137 (IQR:58-249) days.
Conclusion: Adolescent HCC was HBV-related in all five patients. The disease presents late, and extrahepatic metastases and macrovascular invasion limit curative-intended therapies. The overall survival is very poor.
Sub-Saharan African and Scandinavian experience in treating hepatocellular carcinoma: retrospective bi-centre study
S Sobnach,1 H Bayadsi,2 U Kotze,1 O Hemmingsson,2 E Jonas1
1 Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
2 Department of Surgical and Perioperative Sciences, Umeã University, Sweden
Background and Aim: To compare the demographics, clinical presentation, treatment modalities and outcomes of patients with hepatocellular carcinoma (HCC) managed at a tertiary referral centre for liver surgery in South Africa (Groote Schuur Hospital [GSH]) and a specialised liver unit in Sweden (Umeâ University Hospital [UHH]).
Methodology: Retrospective cohort study of all adult patients diagnosed with HCC between July 1 2012 and December 31, 2023, at both centres.
Results: The study cohort comprised 959 (GSH = 455, UHH = 504) patients. Patients at GSH were younger than their UHH counterparts (51 ± 15 vs. 70 ± 10 yr., p = 0.0001) and predominantly hepatitis B virus (HBV) positive (60% vs. 4%, p = 0.0001), whereas UHH had more frequent hepatitis C virus infection (17% vs. 6%, p = 0.0001). Most GSH patients (88%) had advanced disease (Barcelona clinic liver cancer [BCLC] C & D disease, and received best supportive care only (69%). The UHH patients were more frequently treated with curative-intended therapies (ablation (14% vs. 3%, p = 0.0001), resection (27% vs. 5%, p = 0.0001), liver transplantation (6% vs. 0.2%, p = 0.0001)). The five (4% vs. 26%, p < 0.001) and 10-year (2% vs. 17%, p < 0.001) survival rates were lower in the GSH cohort. Mean survival following liver resection were similar in GSH and UHH patients (1271 ± 1291 vs. 1580 ± 1209 days, p = 0.252).
Conclusion: This is the first head-to-head comparison showing significant healthcare disparities between sub-Saharan and European HCC cohorts. Patients in sub-Saharan Africa have a distinct aggressive disease phenotype driven by HBV. This study highlights the need for urgent region-specific surveillance and treatment algorithms to address healthcare disparities and improve outcomes.
Secretory and non-secretory AFP, CEA and CA 19-9 in hepatocellular carcinoma: Impacts on diagnosis, clinical presentation, metastatic patterns and survival
M Emmamally, K Venter, R Khan, S Sobnach, E Jonas
Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
Background: Hepatocellular carcinoma (HCC) is a significant global health challenge, with disproportionately high mortality rates in low-income countries (LICs). In these regions, the diagnostic use of tumour markers such as alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA), and carbohydrate antigen 19-9 (CA 19-9) remains high due to a limited access to advanced imaging technologies.
Aim: To explore the role and impact of AFP, CA19-9 and CEA in a cohort of HCC patients in South Africa.
Methodology: This retrospective study at Groote Schuur Hospital in Cape Town, South Africa spanned the period from 2010 to 2024, assessing the roles of AFP, CEA, and CA 19-9 in diagnosing and predicting the prognosis of HCC.
Results: The study included 501 patients, with elevated AFP and CA 19-9 levels significantly linked to aggressive disease features. Elevated AFP correlated with chronic hepatitis B virus (HBV) infection, hepatomegaly, and pulmonary metastases, while elevated CA 19-9 was associated with more advanced liver disease. Survival analysis confirmed shorter survival for patients with elevated AFP and CA 19-9 levels compared to normal levels (p < 0.001 for both), demonstrating their prognostic value. Elevated CEA levels had no significant impact on survival. Patients with "triple-negative" markers had the longest survival, compared to those with multiple elevated markers (p < 0.001).
Conclusion: AFP and CA 19-9 play key roles in diagnosing and prognosticating HCC in resource-limited settings, aiding in prioritising patients for scarce healthcare resources. The findings highlight the importance of multimodal diagnostic approaches integrating imaging and histopathology with biomarker testing.
Outcomes of flush endovenous laser ablation of the superficial venous system at a tertiary academic hospital in Pretoria, South Africa
MY Docrat, SS Ngema, TT Kgopane, L Shelile
Department of General Surgery, Sefako Makgatho Health Sciences University, South Africa
Introduction: Endovenous laser ablation (EVLA) is a common treatment for superficial venous reflux due to its low morbidity. Flush EVLA might prevent recurrence at the cost of a higher risk of endovenous heat-induced thrombosis (EHIT). Data on flush EVLA outcomes are limited internationally and absent in South Africa.
Research aim: To evaluate the safety of flush EVLA by assessing complication rates and EHIT incidence at two weeks post-procedure.
Materials and methods: This retrospective, single-centre cross-sectional study included 64 patients (age > 18, CEAP C2-C6) who underwent flush EVLA of the great saphenous vein at Dr George Mukhari Academic Hospital, Pretoria (October 2021-October 2023). Patients with incomplete procedures were excluded. Data included demographics, CEAP classification, and post-operative outcomes (especially EHIT). Analysis was descriptive, and ethical approval was obtained (SMUREC/M/453/2023:PG).
Results: The mean age was 56 years, and 72% of patients were female. CEAP classes ranged from C2 to C6, with C2 (35%) and C6 (31%) most common. Technical success was 100%. 25 patients were noted to have minor bruising, and 2 patients were noted to have haematoma formation, with no major complications. Follow-up duplex ultrasound at two weeks showed no EHIT or residual reflux.
Conclusions: Flush EVLA was performed safely and effectively in this series, with 100% technical success and no EHIT at two-week follow-up. Flush EVLA performed in a tertiary institution in South Africa shows a comparable safety and feasibility profile. A more robust study is needed to show long term outcomes.
Outcomes of laparoscopic inguinal hernia repairs: an eleven-year experience in a private surgical practice
KA Naidu,1 SB Ismail,1 S Ebrahim1,2
1 Department of Surgery, Nelson R Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, South Africa
2 Health Systems Research Unit, South African Medical Research Council, South Africa
Background: Inguinal hernia repairs are among the most common surgeries worldwide.
Aim: This study evaluated the outcomes of laparoscopic inguinal hernia repairs performed by a single surgeon.
Methods: A retrospective clinical audit was conducted on 188 consecutive adult patients who underwent laparoscopic groin hernia repair between January 2010 and December 2020 at a private surgical practice. Data on patient, procedural characteristics and outcomes were collected from hospital records and following telephonic contact. All data was entered and managed using the Microsoft Excel programme. Data analysis was conducted using the R Core Team's R Statistical Computing software (2020), and results were presented in the form of descriptive and inferential statistics. The study was approved by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (BREC/00005605/2023).
Results: The study included 188 patients (91.5% male, median age 49 years). All repairs were performed using the Total Extra Peritoneal (TEP) approach for unilateral and bilateral hernias. Conversion to open surgery occurred in 13.8% of cases. The median procedure time was 94.9 minutes, the postoperative hospital stay was two days, and the return to work was two days. At the end of the follow-up period 2024, 20.2% (38/188) were lost to follow-up. Of the remaining 150 contactable patients, 88.7% had no further complications, 4.7% had hernia recurrence, 4.0% reported inguinodynia, and 2.7% had demised.
Conclusion: Laparoscopic inguinal hernia repair, even for primary cases, is feasible with shorter operative times and low complication and hernia recurrence rates when performed by an experienced surgeon.
Knowledge, attitudes and current practices regarding LI-RADS®: A survey from 14 countries in sub-Saharan Africa
R Segobin,1 S Sobnach,2 D Creamer,2 E Jonas,1 S Moosa2
1 Division of Radiology, Department of Radiation Medicine, University of Cape Town, South Africa
2 Division of General Surgery, Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
Background: The Liver Imaging Reporting and Data System (LI-RADS®) plays a critical role in the diagnosis, treatment and surveillance of hepatocellular carcinoma (HCC) globally. The adoption and routine use of LI-RADS® in sub-Saharan Africa (SSA) remains unclear and has not been explored before.
Aim: To assess the knowledge, attitudes and practices related to LI-RADS® among medical professionals in SSA, with a view to identifying barriers and informing futur educational strategies.
Methodology: A 21-item anonymous electronic questionnaire was distributed via SurveyMonkey to medical professionals across SSA. Responses were analysed using descriptive statistics.
Results: A total of 134 participants from 14 SSA countries responded. Radiologists demonstrated higher knowledge of LI-RADS®, particularly regarding its purpose (65.6% vs. 38.2%, p = 0.0007), arterial phase hyperenhancement definition (90.3% vs. 59.8%, p = 0.004) and size criteria (77.4% vs. 45.1%, p = 0.003). A substantial portion of both groups failed to recognise LI-RADS® limitations. Only 34.3% reporting using LIRADS® as a standard, and fewer than 25% of reports adhered to it in most practices. Despite this, 78.3% of participants preferred standardised LI-RADS® reporting for liver lesions at risk of being hepatocellular carcinoma (HCC). The most common barriers to adoption were lack of consistency (44.8%) and unfamiliarity (27.6%).
Conclusion: Despite its perceived value, LI-RADS® is underutilised in SSA due to knowledge gaps and its inconsistent application. Targeted education and training are essential to improve its use and standardise HCC reporting in SSA.
Intestinal stomas: Timing to closure and outcomes post closure of stomas
K Naidoo, D Montwedi
University of Pretoria, South Africa
Background: The creation of a stoma is often deemed as a "simple" procedure during general surgery residency training. The psychological impact on the patient is exceptional. Multiple studies have shown that the frequency of stomas created, out numbers the frequency of closure of stomas. This reality is true for patients in a resource limited country. Aim of the study was to determine timing to closure of stomas and complications of surgery.
Methods: This was a retrospective study for patients who underwent stoma closure between 2017-2019. Timing to stoma closure and outcomes post stoma closure were analysed from hospital records.
Results: A total of 338 stomas were created in the study period. Only 79 stoma reversals were done during this period of which 67 met the inclusion criteria. Majority of the patients were male (78%). The common indication for stoma creation was trauma-related pathology (37%), Malignancy (22%). The average time to stoma closure was approximately 11.10 ± 9.74 months. Post closure complication rate was 30%, this included wound sepsis (18%), stoma necrosis (3%) and stoma prolapse (3%), Others (6%). Older age was associated with increased complications post stoma reversal. No mortalities were noted post stoma closure.
Conclusion: This study confirmed that the number of stomas created far out-numbers the number of stoma reversal performed. Timing to closure is long. Older age was associated with complications.













