Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
African Vision and Eye Health
versão On-line ISSN 2410-1516
versão impressa ISSN 2413-3183
AVEH vol.82 no.1 Cape Town 2023
http://dx.doi.org/10.4102/aveh.v82i1.726
ORIGINAL RESEARCH
Experiences and perceptions of South African optometry students toward public eye care services
Noxolo L. Zulu; Diane van Staden
Department of Optometry, Faculty of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Public eye care services in South Africa are relatively underdeveloped. This is, in part, due to optometry services historically being private sector-focussed, as well as a lack of ophthalmologists in the country. Optometry students who engage in service learning at public health facilities are well placed to share their perceptions of this service.
AIM: To investigate the perceptions and experiences of optometry students regarding public eye care services in South Africa.
SETTING: Data were collected on the Phelophepa Health Care Train while it was stationed at Musina and Polokwane in 2019.
METHODS: A qualitative study was conducted using focus group interviews to collect data from South African optometry students. Two focus group sessions were held, with a total sample of 18 representing two different higher education institutions. Interview recordings were transcribed, and data were thematically analysed using interpretive content analysis.
RESULTS: Three main themes emerged, namely 'inability to deliver quality services', 'negative perceptions about public eye care services' and 'potential to improve public eye care services'. Strengthening infrastructure and human resource capacity were seen as fundamental steps to improving public eye care services in South Africa.
CONCLUSION: Strengthening public eye care services in South Africa is necessary in order to improve the experience-based perceptions of optometry students towards this sector. Addressing eye health system weaknesses through appropriate resourcing will likely contribute to attracting this potential future human resource to the sector, and assist in alleviating the shortage of human resources for eye health within South Africa's public health service
CONTRIBUTION: Optometry education and professional practice in South Africa is increasingly adopting a more public health approach. This shift towards strengthening public eye care services and improving human resources capacity for the same is both important and necessary to address unmet eye health needs in the country. However, current gaps and challenges within the public health system may deter new graduates in South Africa from choosing this practice path if the overall challenges of resourcing and capacity to deliver quality services are not addressed.
Keywords: eye care services; optometry students; public eye care; public health; health systems strengthening; health services; optometry; ophthalmology; access to eye care; healthcare resourcing.
Introduction
The World Report on Vision published by the World Health Organization (WHO) in 2019 estimated that there are 2.2 billion people globally suffering from visual impairment (VI).1 Bourne also emphasised that the number of people affected by VI would increase substantially because of population growth and ageing.2 The same study estimated that increased life span would account for a 35% increase in blindness, and the forecasted population growth would result in the tripling of numbers for both blindness and moderate-to-severe VI. The WHO expressed concern over this projected surge in the demand for eye care and the uneven quality of care and workforce shortages which are some of the main challenges in delivering eye care, especially in developing countries.1
In many countries, eye care is not readily available, either because of the inadequacy of trained personnel or the reality that qualified eye care practitioners are usually concentrated in urban areas.3 South Africa also follows this trend, as a large proportion of South Africans live in rural areas.4 Not surprisingly, therefore, availability, accessibility and affordability of optometric eye care services were found to be some of the factors influencing the utilisation of eye care services in rural areas.3 This can be attributed to the fact that most optometry services in the country are in the private sector, making them unaffordable to many citizens, specifically those living in rural areas.5
There are 3879 optometrists registered with the Health Professions Council of South Africa (HPCSA).6 However, recent statistics from the National Department of Health revealed that government only employed 262 of these optometrists (≈6.8%) nationwide; 124 were employed in Limpopo province, with the Western Cape having only one optometrist employed in the public health system (F. Nxumalo, pers. comm., 27 March 2019). This shows the disproportionate distribution of optometrists employed across the different provinces, as well as between private and public sector eye care in South Africa. With most optometrists still practising in the private sector, human resources for eye health within the public sector remain limited.7
The challenge of the shortage of trained personnel for public eye care services is well documented in several studies.3,7 Some studies have been conducted on recruitment and retention strategies for public sector optometrists,8 as well as perceptions of optometry students on related subjects such as the proposed community service for optometrists9 and working in rural areas after graduating.4 De Villiers investigated the views of medical doctors working in public sector hospitals and found that levels of job satisfaction were low, mainly because of the impact of poor working conditions on the quality of care, including excessive workload and lack of management support.10 There is limited research on the experiences and perceptions of optometry students (as the future eye care workforce) towards public eye care services. Therefore, this study aimed to explore the perceptions and experiences of undergraduate optometry students on public eye care services in South Africa.
Methodology
This qualitative, descriptive study was conducted on the Transnet Phelophepa Health Care Train While it was stationed in Musina and Polokwane in 2019. Both towns are situated in Limpopo province, South Africa, with Musina being deeply rural and Polokwane being semirural. The sampling method used was a purposive sampling, with the study sample consisting of two groups of nine final-year optometry students from the University of Johannesburg (UJ) and the University of KwaZulu-Natal (UKZN), respectively, who were allocated to a two-week service placement on the train during data collection. Data were collected by means of focus group interviews, where semistructured discussions were guided by a set of open-ended questions. Each focus group consisted of nine participants from the same university. The duration of the discussions ranged between 30 min and 60 min per group; interviews were audio-recorded, and the interviewer also captured observational notes that provided contextual information on the group dynamic, ease of responses, body language and tone of voice of participants. Data were analysed using an interpretive content analysis, where raw data in the form of the transcribed interviews followed a structured process of interpreting the underlying meaning of the text, beginning first with identifying meaning units, followed by coding and formation of categories from related codes and finally, the emergence of overarching themes.11
Ethical considerations
Ethical clearance to conduct the study was obtained from the University of KwaZulu-Natal's Biomedical Research Ethics Committee (ref. no. BE281/18) and relevant gatekeeper permissions and verbal consent were obtained from participants.
Results
A total of 18 undergraduate optometry students from two universities participated in the study. Most of the participants were women (n = 11) and all were from historically marginalised racial groups in South Africa: Indian (n = 10), black (n = 7) and mixed race (n = 1), based on South Africa's four main racial groups. Areas of interest investigated in the focus groups included perspectives on public eye care services and experiences (if any) of prior exposure to public eye care facilities.
Three main themes emerged from the data, as shown in Figure 1.
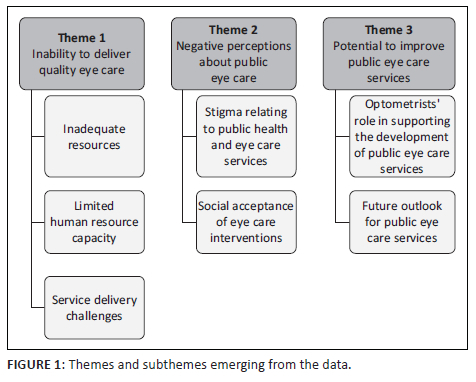
Theme 1: Inability to deliver quality eye care services
Theme 1 highlights the perceived inability of the public health sector to deliver quality eye care services. Factors such as inadequate physical resources, limited human resource capacity and service delivery challenges emerged as subthemes.
Subtheme 1.1: Inadequate resources
Central to any service delivery activity is the availability of resources to enable the services to be delivered to their intended recipients, particularly those who need them the most. Most public eye care facilities in South Africa are under-resourced,8 and this poses great challenges for the delivery of quality eye care services. It was not surprising, therefore, that participants highlighted the lack of resources affecting public eye care services as a major challenge, as evident in the following extract:
'I think public eye care clinics, hospitals, whatever, don't have resources.' (Participant D, African female, 4th year student, University A)
The challenge of a lack of resources can also be linked to the fact that, until recently, eye care services (as part of public health services) did not get the attention that they deserved, and hence the resources were never properly provisioned. Participant experiences highlighted that in many cases, even appropriate space allocation for eye care was a challenge at some public health facilities, as shown in the following quotes:
'That is why you will find that a lot of hospitals don't have a dedicated eye department, [because] it was never there. So, they have had to find somewhere, and it ends up being a corner somewhere.' (Participant B, African male, 3rd year student, University A)
Subtheme 1.2: Limited human resource capacity
All participants had prior exposure to public eye care facilities through in-service learning. Based on their experiences, most participants felt that there were not enough trained eye care personnel in the public health sector, as shown in the following comment from a participant:
'Well, there is, like, two optometrists, which I think is very unrealistic for the whole hospital.' (Participant D, African female, 4th year student, University A)
When clinical services are busy as well as being under-staffed, this has undesirable outcomes for the delivery of quality health care services. In most cases, the demand for services cannot be met, resulting in long patient waiting times, which is in line with the experiences of participants in the study:
'It's often difficult for those people to get to eye care services, and when they get there, they often have to wait in long queues.' (Participant F, Indian female, 4th year student, University B)
Subtheme 1.3: Service delivery challenges
Apart from the lack of resources, students identified other challenges that negatively affect the delivery of eye care within the public health sector:
'I think generally anyone in public services doesn't want to be there.' (Participant B, African male, 3rd year student, University A)
The level of motivation of personnel also goes a long way to ensuring that quality services are delivered. Factors contributing to an unmotivated workforce, as suggested by participants, may include the issues of poor working spaces and an overall frustrating working environment:
'Like, it's really painful having to work there.' (Participant I, African female, 4th year student, University A)
The perceptions of participants also suggest that the lack of prioritisation of optometry services by the government, which is responsible for public health care delivery, can potentially demotivate the future workforce:
'It hasn't been seen as a public health issue, really; they don't see people getting glasses as such a big issue.' (Participant H, Indian female, 4th year student, University B)
Theme 2: Negative perceptions about public eye care services
This theme highlights the stigma related to public health and eye care services.
Subtheme 2.1: Stigma relating to public health services
When asked if they would personally use public services, almost all participants responded that they would not - with the general perception of public health and eye services among optometry students appearing to be negative. The issue of inadequate human resource capacity resurfaced, as well as issues such as low confidence levels in public health services in general, based on experience.
'It [exposure to public eye care services] confirmed what I suspected all along, which is [that] eye care and public eye care in South Africa is dismal; it's not even bad, it's bad-bad.' (Participant I, African female, 4th year student, University A)
Subtheme 2.2: Social acceptance of eye care interventions
Participants also felt that public sector-dependent communities may be reluctant to accept eye care interventions because of preconceived prejudices relating to VI, as well as sociocultural beliefs:
'It's also the stigma that comes with it. Wearing spectacles at a young age is not ideal; you get bullied, called "four eyes" … there is still a stigma that comes with wearing spectacles.' (Participant I, African female, 4th year student, University A)
Students reported witnessing the impact of stigma relating to spectacle wear when doing volunteer work within a specific community project:
'As soon as the child is tested and they need spectacles, you can literally see the others on the outside beginning to mock. So putting a frame onto that child's face is a mission, and you know they might not even wear it afterwards.' (Participant P)
Theme 3: Potential to improve public eye care
This theme highlights the outlook for public eye services among optometry students and the role that optometrists can play in supporting the development of public eye care services in South Africa.
Subtheme 3.1: Optometrists' role in supporting development of public eye care services
There were contrasting views regarding the optometrist's role in supporting the development of public eye care services. Some participants argued that if individual passion is not supported by provision of resources to enable one to do their work, passion alone will be ineffective in bringing about a change in the way eye care services are delivered.
Participants suggested that stakeholder organisations such as the HPCSA should assume more responsibility for playing a role to improve the work conditions for health care practitioners and to improve implementation of existing regulations as they pertain to quality eye care services in all sectors, including the public health sector.
Subtheme 3.2: Future outlook for public eye care services
What does the future of public eye care services look like? The perceptions expressed by participants suggest that despite the prevailing challenges facing public eye care services in South Africa, there is some optimism regarding where the sector is heading. Participants cited the proposed National Health Insurance (NHI) plan as a promising development in the South African health policy.
'We have potential to improve now, with the introduction of the NHI.' (Participant E, Black male, 4th year student, University B)
Participants were optimistic that the NHI carries with it the promise of quality eye care for all. Students further anticipated that the increased use of digital devices will increase the need for eye care services, as many people may start to experience the ocular effects of digital device use, which may prompt governments to prioritise eye care services as a public health issue:
'There is hope; in a few years we are going to start to see the ocular effects of digital screens, and governments worldwide will then start thinking about eye care.' (Participant B, African male, 3rd year student, University A)
Discussion
This study set out to investigate the experiences and perceptions of undergraduate optometry students towards public eye care services in South Africa. The study found that optometry students feel strongly that public eye care services in South Africa are unable to deliver quality eye care services to their communities. Reasons for this perception included several factors, with the major issues being inadequate resources and limited human resource capacity. This is in line with research conducted by Oduntan et al., who found that an absence of eye care personnel, inadequate facilities and poor state funding are hallmarks of public eye care in South Africa.12 The lack of resources is far-reaching, as research by Maake also found that almost 100% of the optometrists working in public hospitals did not fit contact lenses.13 In addition, most optometrists did not perform essential tests, such as tonometry, keratometry or binocular vision assessments, citing a lack of equipment and time constraints. Therefore, patients utilising public eye care services in South Africa are not receiving the minimum expected standard of optometric clinical care as defined by the HPCSA.13
Participants in this study also reported that some hospitals do not have a dedicated eye care department, which is consistent with other research.7,8,9 This may relate to the fact that, historically, eye services did not form part of public eye care services; hence, the necessary resources were never provisioned.13 Even though optometrists now provide eye care as part of the package of health services available to public sector patients in South Africa,14 it is evident that there is a general lack of substantial improvements in public eye care in many districts of South Africa.15 This suggests that if VI is to be reduced, the South African government needs to explore strategies, such as increasing health care budgets, in order to provide for infrastructural needs.3
The perception of optometry students in this study that public eye care services are understaffed is also not new.8,13 Understaffing leads to unmet demand for services, as well as increased patient waiting times. In line with this finding, Scheffler et al.16 reported that Africa has the largest deficit of human resources for health care. This supports the findings of this study that within the public eye care sector in South Africa, limited human resources capacity remains a challenge in the delivery of eye care services. This is a cause for concern, as minimising patient waiting times and queues is one of the National Core Standards for Health.17 The Global Strategy on Human Resources for Health Workforce: 2030 envisages that by 2030, all countries would have made significant progress towards reducing inequalities in accessing health services by approximately 50%. Some of the strategies to achieve this goal include promoting decent work conditions in all settings and optimising health worker motivation, satisfaction, retention, equitable distribution and performance.18 According to the findings of this study, it is apparent that South Africa is falling short in making progress towards achieving this goal, which is in line with the findings of a recent study that found that 54% of optometrists working within public eye care services had an intention to leave or seek employment elsewhere for similar reasons as those identified in this study, which include lack of equipment, infrastructure and funding.19
Lack of motivation of the workforce within the public health sector was found to be one of the factors influencing service delivery. Arguably, the lack of motivation can be secondary to frustrating work environments, as found in one study where personal support and good work environments were motivating factors for health workers.8 The perception that vision care is not a public health priority also has the potential to affect the morale of those employed within the sector. This perception is not far from the reality, as 81% of South African provincial health directorate managers reported that they do not include vision screening in their health promotional programmes.15 Therefore, attention needs to be paid to recruitment and retention strategies for optometrists and the factors that can contribute positively to staff motivation.
Sociocultural factors were found to have an influence on the uptake of available eye care services. In some communities, the wearing of spectacles is still stigmatised, as children who wear spectacles are sometimes bullied and called names,12 as also reported in this study. This may create a reluctance to make use of eye care interventions among children identified with uncorrected refractive error through school health or other programmes - meaning that patients may not adhere to using their vision corrections. Similarly, in a study investigating the impact of eye care services delivered to rural communities of Mankweng in the Limpopo province of South Africa, the authors found that the use of spectacles was considered highly unconventional and was accompanied by the fear of being ridiculed as being blind.20 If communities are not receptive to eye care interventions or have negative perceptions relating to these, it poses a challenge to those trying to deliver the services. Therefore, eye health awareness programmes also need to be considered in the development of public eye care services.
The finding that study participants were unwilling to personally use public eye care services suggests that public health services in South Africa have not earned the trust of members of its society, which is concerning as it could potentially be a widespread view held within communities. When investigating factors that influence utilisation of eye care services, Ntsoane et al. found that among other factors, customer satisfaction was an important factor in sustaining effective utilisation of health resources. They also found dissatisfaction with services to be a barrier to utilisation of eye care services. Furthermore, the authors reported that satisfaction with services received in private eye care practices was much higher than those reported for public services. The authors concluded that efforts should be made not only to increase the quantity of eye care services provided but also the quality, to ensure a sustained utilisation of the available services.12 It is therefore important to understand the basis of the stigma towards public eye care services, so that attempts can be made to remedy the situation and perhaps change the negative perceptions held by members of the public.
Prior to South African democracy, health care services allocation was racially based, with more resources allocated for the white minority and fewer resources allocated for the African majority.21 As a result, the democratic government in 1994 inherited a deeply fragmented and dysfunctional health care system. The right to health care is now enshrined in the Bill of Rights, which is the cornerstone of the Constitution of South Africa. Additionally, the Constitution states that the government must take reasonable legislative and other measures, within its available resources, to achieve progressive realisation of such rights.22 This study found that, years after the inception of democracy, public health care facilities are unable to deliver quality eye care services because of factors such as inadequate resources and limited human resource capacity. While several strides have been made through ongoing advocacy efforts,23 gaps still exist in all components of the eye health system. Resources are insufficient and unequally distributed, and equipment required to deliver comprehensive eye care in public health facilities is insufficient in most cases.19 Appropriate prioritisation of eye care services and relevant provisioning for the same is therefore an urgent priority for the South African government in order to meet its obligations towards quality public eye care services for those in need.
Even though there is insufficient evidence about how health care providers, as agents of change, can influence health systems,24 London argues that policymakers ought to acknowledge health care as a right, as opposed to framing health policy as a service delivery issue. This approach involves effective rights advocacy and reminds the state of its constitutional obligation to progressively realise socio-economic rights.25
South Africa's National Health Act mandated that a statutory Health Professions Council should be established, which should advise the Health Minister on the scopes of practice-registered professions, targets, priorities, norms and standards relating to equitable distribution of health care providers. The Council also has a responsibility to monitor the development, procurement and use of health service technology.26 The finding of this study that advocating for quality eye care for all needs to be part of the responsibilities of all stakeholders to ensure that minimum standards of eye care are adhered to is encouraging. Optometrists holding the Health Professions Council to account will assist in ongoing efforts to ensuring that government health facilities are able to deliver eye care to minimum standards and that when professionals are recruited to facilities, they are able to do their jobs effectively. This is an important consideration, as health care workers are frequently unable to provide adequate access to health care because of systemic factors outside of their control.25
This finding that there is optimism about the future of public eye care services in the country is encouraging. Even though the public eye care sector in South Africa is fraught with challenges, it is still a relatively new sector, and there is hope that strides will be made to improve the delivery of quality, accessible and affordable eye care services. The introduction of the NHI further brings a sense of optimism regarding the future of public eye care in South Africa. The same sentiment was shared by Sithole that new regulations on how eye care services are delivered in South Africa will be developed through the NHI, leading to necessary improvements. However, Sithole cautioned that 'there seems to be no adequate advocacy for eye health to be fully implemented as part of the NHI'.21
As with most facets of life, technological advances are expected to bring changes and new demands in the ophthalmic industry. Computer vision syndrome is a topic that has become important in recent years.27 As highlighted in this study, the increased use of digital screens, which include mobile phones, will likely exacerbate ocular problems relating to their use and therefore result in an increased demand for eye care services. This will create added pressure on governments to pay more attention to eye care, as well as provide adequate capacity for comprehensive, quality service delivery.
While this study provides some insights into the perceptions and experiences of optometry students regarding public eye care services, there are several limitations that should be noted. The sample size was small, with representation from only two of the four training institutions in South Africa. As such, the findings may not be representative of other optometry students' perceptions and experiences of public eye care services in South Africa, particularly in regions not represented in the study. The study sample also included only historically disadvantaged students, which may have had important yet unknown influence on the results. Furthermore, for most students, their exposure to the public health sector and its eye care services would have been limited to their intermittent service placement exposures during training and therefore may not have been extensive enough, which should be considered when interpreting some of the findings herein. Finally, the researcher has worked for several years in public eye care services in South Africa. Therefore, the focus group discussion and subsequent results may have consciously or unconsciously been influenced by the potential bias of the interviewer.
Conclusion
Health care is a basic human right, and it is the responsibility of governments to provide quality, accessible and affordable health care for its citizens. Therefore, the provision of quality eye care services, including the provision of required resources, remains the responsibility of the state. While the perceptions of undergraduate optometry students regarding public eye care services were largely negative, the optimistic outlook of this future workforce is an opportunity for the public health system in South Africa to strengthen primary eye care services in South Africa and therefore attract and retain qualified staff in public health facilities. Factors needed to strengthen the delivery of quality eye care services within the public health sector in South Africa include the provisioning of infrastructural as well as human resources for primary eye care towards the realisation of quality eye care for all.
Acknowledgements
This article was adapted from a master's thesis under the supervision of Dr Van Staden. The authors would like to thank all the optometry students for participating in the study and the Transnet Phelophepa Train management for granting permission to conduct the study on their facility.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
N.Z. conceptualised the project and D.v.S. contributed to the project design, analysis and write-up of the project. Both authors contributed to the preparation of the manuscript.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
Data sharing is not applicable to this article.
Disclaimer
The views and the opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1.World Health Organization. World report on vision [homepage on the Internet]. Geneva: WHO. 2019 [cited 2019 Oct 21]. Available from: https://www.who.int/publications-detail/World-Report-on-Vision [ Links ]
2.Bourne RR, Flaxman SR, Braithwaite T, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: A systematic review and meta-analysis. Lancet Glob Health. 2017;5(9):e888-e897. https://doi.org/10.1016/S2214-109X(17)30293-0 [ Links ]
3.Oduntan OO, Mashige KP, Hansraj R, Ovenseri-Ogbomo G. Strategies for reducing visual impairment and blindness in rural and remote areas of Africa. Afr Vision Eye Health. 2015;74(1):5. https://doi.org/10.4102/aveh.v74i1.25 [ Links ]
4.Mashige KP, Oduntan OA, Hansraj R. Opinions of South African optometry students about working in rural areas after graduation. Afr J Prim Health Care Fam Med. 2015;7(1):1-7. https://doi.org/10.4102/phcfm.v7i1.799 [ Links ]
5.Mashige KP, Naidoo KS. Optometric practices and practitioners in KwaZulu-Natal, South Africa. Afr Vision Eye Health. 2010;69(2):77-85. https://doi.org/10.4102/aveh.v69i2.128 [ Links ]
6.Health Professions Council of South Africa. [cited 2020 Mar 01]. Available from: https://www.hpcsa.co.za [ Links ]
7.Van Staden D. Decentralised clinical training in optometry: A developmental strategy for eye health in KwaZulu Natal? Prim Health Care Res Dev. 2018;20(e35):1-4. https://doi.org/10.1017/S1463423618000397 [ Links ]
8.Ramson P, Govender P, Naidoo K. Recruitment and retention strategies for public sector optometrists in KwaZulu-Natal Province, South Africa. Afr Vision Eye Health. 2016;75(1):1-10. https://doi.org/10.4102/aveh.v75i1.349 [ Links ]
9.Mashige KP, Oduntan OA, Rampersad N. Perceptions and opinions of graduating South African optometry students on the proposed community service. Afr Vision Eye Health. 2013;72(1):11-18. https://doi.org/10.4102/aveh.v72i1.43 [ Links ]
10.De Villiers MR, De Villiers PJT. Doctors' views of working conditions in rural hospitals in the Western Cape. S Afr Fam Pract. 2004;46(3):21-26. https://doi.org/10.1080/20786204.2004.10873056 [ Links ]
11.Erlingsson C, Brysiewicz P. Orientation among multiple truths: An introduction to qualitative research. Afr J Emerg Med. 2013;3(2):92-99. https://doi.org/10.1016/j.afjem.2012.04.005 [ Links ]
12.Ntsoane MD, Oduntan OA. A review of factors influencing the utilization of eye care services. Afr Vision Eye Health. 2010;69(4):182-192. https://doi.org/10.4102/aveh.v69i4.143 [ Links ]
13.Maake ME, Moodley VR. An evaluation of the public sector optometric service provided within the health districts in KwaZulu-Natal, South Africa. Afr Vision Eye Health. 2018;77(1):1-9. https://doi.org/10.4102/aveh.v77i1.407 [ Links ]
14.Ebrahim N, Karim F, Gasa M, Poonvaganum K, Gangat F, Van Staden DB. Public sector optometrists' perspectives on a decentralised model of clinical training for optometry in KwaZulu-Natal, South Africa. Afr Vision Eye Health. 2019;78(1):1-7. https://doi.org/10.4102/aveh.v78i1.489 [ Links ]
15.Lilian RR, Railton J, Schaftenaar E, et al. Strengthening primary eye care in South Africa: An assessment of services and prospective evaluation of a health systems support package. PLoS One. 2018;13(5):e0197432. https://doi.org/10.1371/journal.pone.0197432 [ Links ]
16.Scheffler R, Tulenko K. The deepening global health workforce crisis: Forecasting needs, shortages, and costs for the global strategy on human resources for health (2013-2030). Ann Glob Health. 2016;82(3):510. http://doi.org/10.1016/j.aogh.2016.04.386 [ Links ]
17.Molekoi W, Msibi EB, Marshall C. Recent developments in ensuring quality of care in health establishments in South Africa. S Afr Health Rev. 2013;2013(1):25-32. [ Links ]
18.World Health Organization. Global strategy on human resources for health: Workforce 2030. Geneva: WHO; 2016. [ Links ]
19.Buthelezi LM, Van Staden D. Integrating eye health into policy: Evidence for health systems strengthening in KwaZulu-Natal. Afr Vision Eye Health. 2020;79(1):1-10. https://doi.org/10.4102/aveh.v79i1.549 [ Links ]
20.Oduntan AO, Raliavhegwa M. An evaluation of the impact of the eye care services delivered to the rural communities in the Mankweng Health sub-district of the Northern Province. S Afr Optom. 2001;60:71-76. [ Links ]
21.Sithole HL. An overview of the National Health Insurance and its possible impact on eye healthcare services in South Africa. Afr Vision Eye Health. 2015;74(1):6. https://doi.org/10.4102/aveh.v74i1.18 [ Links ]
22.South Africa. Constitution of the Republic of South Africa. Bill of Rights. Pretoria: Government Printer; 1996. [ Links ]
23.Naidoo KS, Naidoo K, Maharaj Y, Ramson P, Wallace D, Dabideen R. Scaling up the delivery of refractive error services within a district health system: The KwaZulu-Natal, South Africa experience. BMC Health Serv Res. 2013;13(1):361. https://doi.org/10.1186/1472-6963-13-361 [ Links ]
24.Du Toit R, Faal HB, Etya'ale D, et al. Evidence for integrating eye health into primary health care in Africa: A health systems strengthening approach. BMC Health Serv Res. 2013;13(1):102. [ Links ]
25.London L. What is a human-rights based approach to health and does it matter? Health Hum Rights. 2008;10(1):65-80. https://doi.org/10.2307/20460088 [ Links ]
26.South Africa. The National Health Act. Pretoria: Government Printer; 2003. [ Links ]
27.Bali J, Neeraj N, Bali RT. Computer vision syndrome: A review. J Clin Ophthalmol Res. 2014;2(1):61. https://doi.org/10.4103/2320-3897.122661 [ Links ]
 Correspondence:
Correspondence:
Noxolo Zulu
londekazulu1@gmail.com
Received: 02 Dec. 2021
Accepted: 10 June 2022
Published: 22 Aug. 2023














