Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Occupational Therapy
versión On-line ISSN 2310-3833
versión impresa ISSN 0038-2337
S. Afr. j. occup. ther. vol.54 no.1 Pretoria abr. 2024
http://dx.doi.org/10.17159/2310-3833/vol54no1a7
RESEARCH ARTICLE
Occupational therapists' perspectives on knowledge transfer in clinical practice in the Free State, South Africa
Azette SwanepoelI; Corlia Janse van VuurenII; Shoba NayarIII
IOccupational Therapy Department, Faculty of Health Sciences, University of the Free State, South Africa https://orcid.org/0000-0002-0939-0776
IISchool of Health and Rehabilitation Sciences, University of the Free State, South Africa https://orcid.org/0000-0002-4146-6937
IIIIndependent academic https://orcid.org/0000-0002-9777-5915
ABSTRACT
BACKGROUND: The transfer of all types of knowledge in occupational therapy practice is complex, and there is little agreement globally on the most important types of knowledge that inform clinical practice. This study aimed to uncover the perspectives of occupational therapists in the Free State, South Africa on knowledge transfer in clinical practice.
METHODOLOGY: Q methodology was used to collect data from 14 occupational therapists utilising Q Method Software.
RESULTS: Factor analysis revealed two factors with eigenvalues of greater than 1. Factor 1 had an eigenvalue of 2.97, and factor 2 had an eigenvalue of 1.48. These two factors were constructed from six and five participants' Q Sorts respectively, with the highest factor loads for factor 1 and factor 2. Thematic content analysis of these two factors identified two themes, namely: client-centred philosophy and practice informed through clinical reasoning.
CONCLUSION: The strategic use of Q methodology presented empirical evidence of the transfer and utilisation of all types of knowledge in clinical practice in the Free State, South Africa. The results indicated the transfer of propositional, procedural, personal, and client knowledge strengthens client-centred practice and manifests in clinical reasoning. Furthermore, the results indicate an interdependence between the types of knowledge, meaning that it is important that therapists utilise all types of knowledge and not rely on only one form of knowledge when they work with patients to promote well-being.
IMPLICATIONS FOR PRACTICE:
• Q Methodology is an ideal research method to identify the subjective perspectives of participants where different opinions on a topic might exist.
• Clinicians hold a wealth of practice experience and personal knowledge that should be shared and captured through research.
• The client's voice needs to be heard more often to ensure client-centred practice is not only an idea on paper.
Keywords: Q methodology, theory and research, practice experience, patient-therapist relationship, patient voice, occupational therapy clinical practice
INTRODUCTION AND LITERATURE REVIEW
Various processes describe how knowledge is used to inform clinical practice. These processes include knowledge transfer, knowledge translation, and knowledge exchange1,2. Much has been published on the different concepts of knowledge-to-action and authors have argued about the difference between the often-interchangeable use of the terms; knowledge translation, knowledge transfer, and knowledge exchange. Table I (below, page 55) provides an overview of some of the definitions of knowledge transfer indicating the different perspectives that exist.

Knowledge transfer, which is the focus of this paper, is seen as a subcategory of the knowledge translation process which occurs in clinical practice. The authors furthermore argue that knowledge transfer consists of all types of knowledge not only research evidence.
According to the literature, the transfer of knowledge is considered to be a bilateral activity or a two-way process2 of knowledge informing practice, and can include any combination of the types of knowledge described in literature (see below). If compared with some of the definitions of knowledge translation and exchange, knowledge transfer uses both, empirical evidence to guide practice, procedural - as well as personal knowledge. Knowledge is, therefore, not transferred to practice by researchers; rather transferred in practice between clinicians, clients, and other stakeholders. Because of its all-encompassing nature, knowledge transfer as a method to inform practice was the focus of the study.
Occupational therapists use different types of knowledge to understand the complexity of human occupation to guide clinical reasoning for assessment and intervention and inform ethical practice7-9. Often, in clinical practice, the occupational therapist draws on a combination of the types of knowledge to inform their clinical reasoning10,11. These interrelated types of knowledge include propositional (or theoretical/empirical) knowledge,8,12, procedural knowledge (practice experience)5,12 personal theory (referred to as personal knowledge henceforth)8,12, and espoused knowledge2. Propositional knowledge includes theoretical knowledge and research evidence8,12; while procedural knowledge refers to the occupational therapist's clinical experience8,13. Fish and Boniface8 describe personal theory as the clinician's values and beliefs that influence their practice, while espoused knowledge is propositional knowledge that therapists agree with because of their personal knowledge. It is, therefore, the theory they understand or feel comfortable with and which they will use in practice. Client knowledge refers to the knowledge a client has of their occupational profile, context, likes, and dislikes14.
There are, however, differing perspectives on what is the types of knowledge to ensure meaningful occupational engagement for the client. This is achieved by recognising the relationship between the person, environment, and occupation and the types of knowledge arising from it.
Over the past few decades, researchers have strongly advocated for the use of propositional knowledge (evidence-based knowledge) to inform clinical practice13,16-18. These authors argue that, to inform practice and ensure quality service delivery evidence-based knowledge is necessary. However, the knowledge that is transferred to clinical practice might also include (or be derived from) clinical skills, cognitive skills such as judgement, problem-solving, and decision-making that developed from occupational therapy practical experience2, contextual knowledge acquired from clients (client-knowledge)15, and the personal values and beliefs of the occupational therapist. It could, thus, be dangerous to focus on a single form of knowledge transfer, furthermore, to ignore the interrelated nature of knowledge transfer.
Knowledge transfer in clinical practice is a dynamic process that involves occupational therapists, their clients, other relevant stakeholders, such as other team members, family, and/or caregivers accessing and sharing all types of knowledge. The transfer of knowledge is, therefore, considered to be a bilateral activity or a "two-way process"2:16 of knowledge informing practice, which suggests collaboration between the occupational therapist and client in clinical practice19. Davis and Polatajko14 and Park et al.20 also refer to the value of collaboration, where the occupational therapist acknowledges the clients' occupational stories, and use it to inform contextually relevant occupation-based practice. Indeed, it has been argued that it is often the transfer of the expert knowledge of a client or their caregivers about their context and occupational realities that informs practice19,21 as well as allows for client-centred service delivery.
Yet, understanding the interrelated nature of knowledge transfer is a complex undertaking, especially given the varied perspectives on the transfer of the different types of knowledge in clinical practice. What authors do agree on, however, is the importance of knowledge for informing clinical practice. To date, limited documentation exists on the perspectives of South African occupational therapists on the type and content of the different types of knowledge that are transferred in clinical practice. The aim of this article is to determine the perspectives of occupational therapists practicing in the Free State, South Africa, regarding knowledge transfer in clinical practice.
METHODOLOGY
Ethical approval for the study was received from the Health Science Research Ethics Committee (UFS-HSD2021/1454/2610) of the University of the Free State.
Study Design
To determine the occupational therapists' perspectives on knowledge transfer in clinical practice, a mixed method Q methodology was utilised. Q methodology was developed by psychologist William Stephenson in 1935,22 and identifies participants' subjective perspectives regarding a specific topic of interest, about which different opinions may exist23,24.
The Q methodology consists of six steps, and the work of Webler et al.25 is referenced in this study.
Step 1: Determine the objective of conducting the Q methodology
The objective was to determine the perspectives of occupational therapists in the Free State, South Africa on knowledge that is transferred in their clinical practice.
Step 2: Preparation to create the concourse
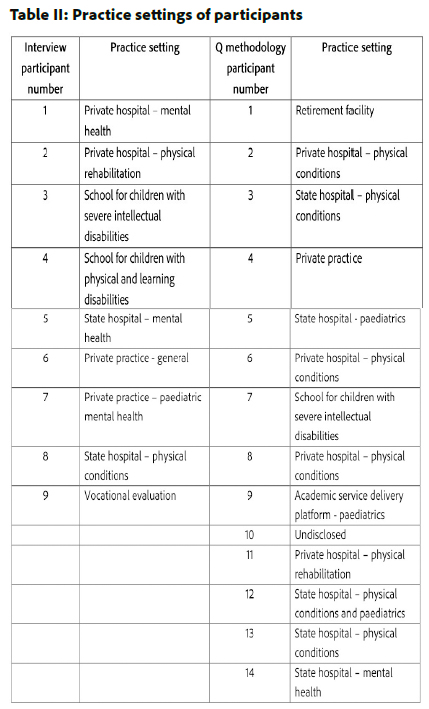
A concourse is a collection of possible statements that, for this study, related to the occupational therapists' knowledge transfer in clinical practice. To build the concourse for the Q sample, published resources and semi-structured interviews are included, as recommended24. For this study, a scoping review was undertaken to determine the landscape of knowledge transfer in occupational therapy clinical practice. The scoping review was followed by semi-structured, digitally audio-recorded interviews with nine occupational therapists from different practice settings (see Table II, adjacent, page 57) in the Free State, South Africa, to gain insight into the content of the knowledge that is transferred in their clinical practice. Interview participants were provided with a definition and an explanation of each of the four types of knowledge that had been identified in occupational therapy literature, namely, propositional knowledge (theoretical/empirical), procedural knowledge (practice experience), personal knowledge (own world view, values, and beliefs), and client knowledge. Inductive thematic analysis was performed to extract statements made by participants in the interviews, to form the concourse25. Statements were also extracted from the literature identified by the scoping review. From the concourse, a Q sample of statements was developed. Including only participants from the Free State, South Africa was a limitation of this study. It is recommended that a follow-up study is conducted amongst occupational therapists practicing in the whole of South Africa.
Step 3: Identify, select, and edit Q statements
The concourse initially consisted of 80 statements representing the four types of knowledge: propositional (n = 20), procedural (n = 32), personal (n = 14), and client (n = 14) knowledge. To identify, select and edit the Q statements, the researcher and a co-coder, who is familiar with Q methodology, went through all the statements to retain, combine, or remove statements. The included final Q statements adhered to the qualities of a "good Q statement" in (a) being meaningful to the participants (occupational therapists), (b) understandable, (c) having the potential to be interpreted in various ways, and (d) giving participants something to think about25:16. The final Q sample consisted of 42 statements relating to the four types of knowledge: propositional (n = 8), procedural (n = 15), personal (n = 10), and client (n = 8) (see Table II page 58).
After finalising the Q sample, each statement was allocated a number between 1 and 42. The study was set up using QMethod Software26 and the statements were loaded onto the platform in the same sequence as each statement had been numbered during the preparation phase. A Q grid was set up in an inverted pyramid comprising 42 blocks (Figure 1, adjacent)
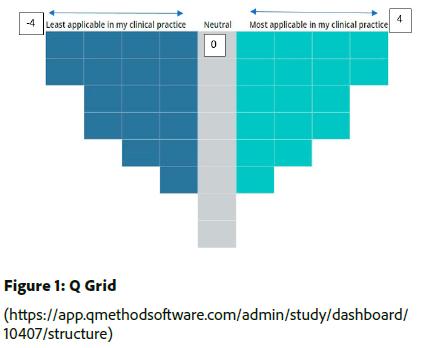
QMethod Software provide a forced normal distribution with an equal number of blocks on either side of the neutral column. Statements must be placed in each block before the survey continues. This normal distribution forces participants to carefully reflect on their perspectives of knowledge transfer in their specific clinical practice26 and place a statement in the applicable block of the Q grid (see Figure 1, above).
Step 4: Recruit participants
Convenience and snowball sampling were used to recruit participants. Twenty occupational therapists known to the researcher and practicing in the Free State, South Africa were invited via email to take part in the Q method survey. Through snowball sampling the participants were requested to share the invitation with colleagues who might be interested in the study. The researcher did not specify the number of invitations to be shared with colleagues. Webler et al.25 suggest that participants should hold various perspectives on the topic under investigation. For this reason, occupational therapists were recruited from various clinical fieldwork settings in the Free State, South Africa. Table II (below) shows the clinical practice setting of the two groups of participants of the semi-structured interviews and the Q method survey.
Step 5: Conducting the Q sorts
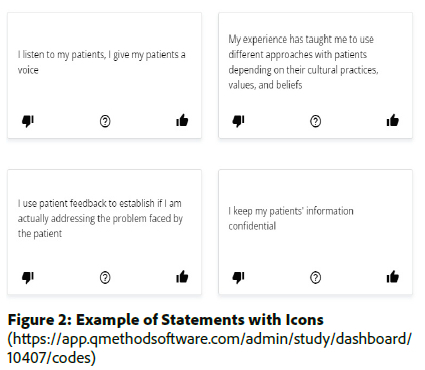
Participants used a link provided by the researcher to access the QMethod Software platform and were requested to provide an individualised participation code (also provided by the researcher). The first landing page of the survey requested participants to consent to participation in the study by choosing between the options 'agree' or 'not agree'. In the next step, participants were instructed to rank each of the statements by choosing an icon (thumbs up, neutral, thumbs down) with regard to the applicability of the statement to their clinical practice setting (Figure 2, below). The statements were automatically placed in three piles, to be used in the next step.
Once the initial sorting had been done, participants continued to a page where the Q grid appeared (Figure 1, page 56). Each of the statements in the three piles were subsequently placed on the grid, by each participant, according to perception of a statement - from most to least applicable to the participant's clinical practice. Statements could be removed and replaced until the participants were satisfied with the placement of their statements. The final placement of the statements by each participant is known as the participant's Q sort placed from most to least as applicable to their clinical practice. The last landing page of the survey, a short post-sort section, invited participants to comment on their Q sorts and the placements of the statements on the Q grid. Participants were given the option to provide feedback by commenting in the QMethod software, or to send a reflection to the researcher via email or to have a short online discussion with the researcher. Only six participants provided feedback, which is a limitation of the study. The researcher recommends in person reflection with each participant take place to ensure the valuable input from participants are not lost.
Step 6: Using factor analysis to arrive at perspectives of knowledge transfer in clinical practice
Factor analysis was used to identify patterns from the Q sorts of each participant25. The final sorts, also known as factors, are combinations of the diferent participants' Q sorts. The first step of the factor analysis was to decide on a method to extract the factors, either centroid or principal components analysis. In this study, centroid analysis was used25 to account for the indeterminacy of its solutions. This means that the same participants would not have the same Q sort twice227. The second step was to choose a rotation method to ensure the best results. In this study, Pearson correlation and Varimax rotation were done to ensure that participants' Q sorts were considered for only one factor25. The last step of the factor analysis was to decide on the number of factors. The Kaiser-Guttman criterion was used to determine the number of factors to be extracted. Two factors with eigenvalues greater than 1.0026 were chosen, the statements from these two factors with sort values of four, three, and two (Table IV, page 58) were thematically analysed by the researcher to determine the participants' perspectives on knowledge transferred in their clinical practice.
Q methodology was designed as a rigorous method to determine participants' subjective opinions or perspectives on specific matters28, which made this the most suitable research method for this study. Content validity was assured by using literature and interviews to compile the final Q sample. The natural-language statements extracted from the semi-structured interviews and statements from literature assured face validity. A pilot study was conducted to further assure content and face validity. No changes were required, and the results of the pilot study were included in the main study. Q sort validity was obtained, and each participant's Q sort represented their own perspectives. Reliability had been confirmed through test-retest procedures in previous studies29. Regarding trustworthiness of the study; credibility was ensured through method, data, and theory triangulation. Transferability was ensured through a description of knowledge transfer in clinical practice as well as a specific procedure of data collection and analysis were utilised. Dependability was ensured though audit trails and systematic documentation, management, and storage of data.
RESULTS
Results of the two data collection processes described above are included in this paper (see Table II, page 56). The first set of results was obtained from the Q methodology survey itself, with 14 occupational therapists practicing in the Free State, South Africa. The second is based on the qualitative data obtained from the semi-structured interviews conducted with nine experienced occupational therapists, to determine the initial Q statements.
In total 20 occupational therapists in the Free State, South Africa, indicated their interest in taking part in the Q method survey and were sent an information document. This was accompanied by a link to the QMethod Software web page, and a different participation code for each participant randomly created by the platform. In the end, only 14 occupational therapists from different clinical practice settings completed the Q sort and were included in the study. Webler et al.25 recommends recruiting one participant for every three Q statements; therefore, 14 participants were deemed sufficient for this phase of the study. Six participants provided written reflective feedback regarding their Q sorts. At this stage, it was not known whether a participant's Q sort would be flagged for inclusion in the final factors.
Two factors with eigenvalues greater than 1.00 were extracted. Factor 1 had an eigenvalue of 2.97, while Factor 2 had an eigenvalue of 1.48. A factor represents the collective perspectives of a group of participants27. The final factors are combinations of the statements used in the study. Factor 1 was constructed by Q sorts of participants 3, 9, 10, 12, 13, 14 while Factor 2 was constructed by Q sorts of participants 1, 4, 5, 7, 8. (see Table III, adjacent). Automatic flagging of a Q sort is done to, first, indicate which participants' Q sorts have the highest factor loads and, second, to correlate a participant's Q sort with the final factor25,30.
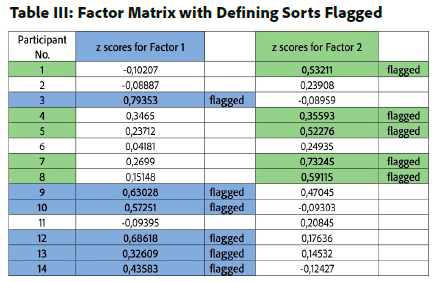
Table IV (below) shows the final factors with the z-scores and sort values of each statement that contributed to the factor. A sort value of 4 represents a statement that is most applicable to a participant's clinical practice. Only statements with a sort value between 4 and 1 are included in Table IV statements with sort values of 0 to -4, which represent neutral or least applicable to a participant's clinical practice, are not included.
The results indicate a low correlation of 0.334 between factors 1 and 2. This is of importance, because it indicates that there are differences between the two sets of factors. The z sores in Table IV (below) indicate the priority statements of each factor. The final factors represent participants' perspectives and include all the types of knowledge transferred in occupational therapy clinical practice in the Free State, South Africa. The thematic analysis of the statements with sort values of 4, 3, and 2 delivered two themes namely: client-centred philosophy (Factor 1) and practice informed through clinical reasoning (Factor 2).
The qualitative findings, as shown in Table V (below), were extracted from the semi-structured interviews and the post-survey comments of the Q methodology. The verbatim quotes obtained from the semi-structured interviews is referred to as I participants, whilst data from participants included in the post survey comments of the Q methodology referred to as Q participants. The verbatim quotes of the participants support the two themes identified from Factors 1 and 2.
DISCUSSION
Q methodology was designed to measure the participant's subjective perspectives on an issue, and to challenge participants' thoughts on the matter25. Participants had to carefully consider what type of knowledge was most or least applicable in their clinical practice setting, which confirms the existing perspective that different types of knowledge inform clinical practice7-9,19. The thought processes facilitated by the Q methodology re-affirmed the importance a client-centred philosophy and clinical reasoning for occupational therapists in clinical practice, through the two themes identified and discussed below.
Client-centred philosophy
The client-centred philosophy, firstly, manifests in clinical practice through the utilisation of propositional knowledge (theory and research) of the patient's pathology. Designing interventions relevant to each patient's needs by choosing theory ensures evidence-based practice. Utilising theory pertaining to pathology, combined with applicable theoretical frames of references, allows occupational therapists to understand the impact of a pathology better, and provide them the opportunity to work towards functional treatment outcomes with their patients3.
Secondly, "Putting the patient first" (Factor 1, statement no 15) reflect participants' world views, values and beliefs, and ethical perspectives which inform and influence the way they approach their patients8,12. This personal knowledge develops through reflective practice that influences and might even change a therapist's personal beliefs of patients, their contexts and challenges31. The complex integration of procedural knowledge (experience) and personal knowledge occurs as a result of reflective practice. The integration enables a therapist to identify best practice, transfer contextual relevant propositional knowledge to their clinical practice while maintaining a holistic view of the patient32.
Restall and Egan33, thirdly, urged therapists to realise the importance of collaborating and building relationships with their patients. Embodying the client-centred philosophy of the occupational therapy profession might lead to a patient-therapist relationship developing. This relationship is, however, dependent on the engagement of both the patient and their therapist. Where pathology allows, shared problem-solving gives autonomy back to the patient and restores their dignity, because patients contribute to discussions about the total care process of which they are the recipient. Sumsion and Law34 argued, in a patient-therapist relationship, the therapist should be aware of the power relationship in the therapeutic process. By collaborating and communicating treatment goals, the balance of the power relationship might be more equal35. Participants stated that, in this collaborative relationship, they used examples from their own experiences, which further demonstrates the equalisation attempt suggested by Sumsion and Law34.
Fourthly, patient might transfer their expert client knowledge of their own occupational stories, contexts, and support systems to clinical practice. Each patient's environment and context are unique, and intervention plans should not be blindly duplicated from one patient to the next based on similar pathology or geographical context14. A patient's occupational engagement is often guided by their cultural roles, rituals, and/or routines. Differences in, amongst others, role expectations, cultural practices, spirituality, contexts, and environments, should always be considered, whereby ensuring occupational justice for each patient33. Therapist often rely on practice experience while being cognisant of the client knowledge transferred by their patient to ensure client-centred service delivery.
Practice informed through clinical reasoning
The skill of applying clinical reasoning is the product of clinical experience and develops throughout the occupational therapist's profession. It informs the occupational therapy process from the evaluation-, intervention planning-, treatment implementation-, and outcome measure phases. Furthermore, propositional knowledge forms the foundation of occupational therapists' knowledge base, and influences their clinical reasoning, which manifests in clinical practice. Each therapist holds personal world views, values and beliefs, life experiences, and ethical perspectives that influence their clinical reasoning and the way they approach their patients8,12.
Chapparo and Ranka36 proposed the use of clinical reasoning to clarify and explain the occupational challenges patients experience because of their disability. This can be achieved, firstly, by an in-depth evaluation of the patient's occupations, client factors, performance patterns, as well as their context and environment36 which constitute client knowledge. Secondly, utilising propositional knowledge (theoretical and/or research evidence) regarding the patient's pathology, procedural knowledge combined with the above-mentioned assessment outcomes a therapist might be able to determine the long-term treatment needs of a patient334. Participants indicated such transfer of a combinations of propositional and procedural knowledge in clinical practice. Teoh37 supported the notion that knowledge has the potential to be created through an integration of theory knowledge and clinical experience through reflective practice. This view is supported by Carrier et al.38 who proposed clinical reasoning to be informed by propositional, procedural, personal, and client knowledge.
CONCLUSION
The aim of the paper was to determine the perspective of occupational therapists practicing in the Free State, South Africa, regarding knowledge transfer in clinical practice. The study utilised Q methodology that allows for the identification of different perspectives on an issue. The results indicated the transfer of propositional, procedural, personal and client knowledge strengthens client-centred practice and manifests in clinical reasoning. Being aware of the potential to integrate these types of knowledge is a strength of this study and meets the aim set out by the researcher. The clinical experience and personal values, beliefs, and world views of an occupational therapist contribute to unique patient-therapist relationships. No two patients are the same and a relationship must be developed with each of the patients to inform an occupation-based intervention plan for the patient. The occupational therapy process is, subsequently, reliant on an effective patient-therapist relationship. The two themes should not be considered in isolation, rather, a client-centred philosophy is dependent on clinical reason and Vise Versa through the transfer of all types of knowledge in clinical practice.
Author Contributions
Azette Swanepoel conducted the study under the supervision of Corlia Janse van Vuuren (second author) and Shoba Nayar (third author). The second and third author contributed to the conceptualisation and study design. Final revisions of the manuscript were done by the first author. All the authors agreed on the final revised manuscript.
Acknowledgements
The authors would like to acknowledge Anke van der Merwe, who conducted the semi-structured interviews, and Jani du Preez, who assisted in compiling the final Q sample of 42 statements from the original concourse of 80 statements.
Conflicts of interest
The authors have no conflicts of interest to declare.
REFERENCES
1. Canadian Institute for Health Research. Guide to knowledge translation planning at CIHR: Integrated and end-of-grant approaches [Internet]. 2015 [cited 2022 Mar 19]. Available from: https://cihr-irsc.gc.ca/e/45321.html. [ Links ]
2. Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: Time for a map? J Contin Educ Health Prof. 2006;26(1):13-24. https://doi.org/10.1002/chp.47. [ Links ]
3. Atwal A, Spiliotopoulou G. Knowledge transfer: Developing guidelines for occupational therapists working with people with lower limb amputations. Br J Occup Ther. 2011;74(March):4276. https://doi.org/10.4276/030802211x12996065859120. [ Links ]
4. Kiefer L, Frank J, Ruggiero E Di, Dobbins M, Manuel D, Gully PR, et al. Fostering Evidence-based Decision-making in Canada. Can J PublicHealth. 2005;0-19. [ Links ]
5. Pentland D, Forsyth K, Maciver D, Walsh M, Murray R, Irvine L, et al. Key characteristics of knowledge transfer and exchange in healthcare: Integrative literature review. J Adv Nurs. 2011;67(7):1408-25. https://doi.org/10.1111/j.1365-2648.2011.05631.x. [ Links ]
6. Stratton Johnson L. From knowledge transfer to knowledge translation: Applying research to practice. Occup Ther Now. 2005;(July/August):11-4. [ Links ]
7. Duncan EAS. An introduction to conceptual models of practice and frames of reference. 4th ed. Duncan EAS, editor. Foundation for practice in occupational therapy. Edinburgh: Elsevier Churchill Livingston; 2006. 59-66 p. [ Links ]
8. Fish D, Boniface G. Reconfiguring professional thinking and conduct: A challenge for occupational therapist in practice. In: Boniface G, Seymour A, editors. Using occupational therapy theory in practice. West Sussex, UK: John Wiley & Sons.; 2012. p. 10-7. https://doi.org/10.1002/9781118709634.ch13. [ Links ]
9. Kielhofner G. Conceptual foundation of occupational therapy in practice. 4th ed. Philidelphia: F.A. Davis; 2009. [ Links ]
10. Bryant W, Parsonage J, Tibbs A, Andrews C, Clark J, Franco L. Meeting in the mist: Key considerations in a collaborative research partnership with people with mental health issues. Work. 2012;43(1):23-31. https://doi.org/10.3233/wor-2012-1444. [ Links ]
11. Haag HL, Sokoloff S, MacGregor N, Broekstra S, Cullen N, Colantonio A. Battered and brain injured: Assessing knowledge of traumatic brain injury among intimate partner violence service providers. J women's Heal. 2019;28(7):990-6. https://doi.org/10.1089/jwh.2018.7299. [ Links ]
12. Turpin M, Iwama MK. Using occupational therapy models in practice: A field-guide. Turpin M, Iwama MK, editors. Edinburgh: Elsevier Churchill Livingstone; 2011. 13-25 p. [ Links ]
13. McKay MH, Pickens ND, Medley A, Cooper D, Evetts CL. Comparing occupational adaptation-based and traditional training programs for dementia care teams: An embedded mixed-methods study. Gerontologist. 2021;61(4):582-94. https://doi.org/10.1093/geront/gnaa160. [ Links ]
14. Davis JA, Polatajko HJ. Capturing occupational knowledge: Enabling powerful outcomes for our clients. Occup Ther Now. 2008;10(5):10-2. https://caot.in1touch.org/document/3901/OTNow_Sept_08.pdf. [ Links ]
15. Law M. Learning by doing: Creating knowledge for occupational therapy. World Fed Occup Ther Bull. 2010;62(1):12-8. https://archive.wfot.org/wfot2010/docs/Mary_Law_ENG.pdf. [ Links ]
16. Caldwell E, Fleming J, Purcell A, Whitehead M, Cox R. Knowledge translation in cancer services: Implementing the research and evidence in practice model. Br J Occup Ther. 2011;74(11):535-9. https://doi.org/10.4276/030802211x13204135680947. [ Links ]
17. Jutai JW, Teasell RW. The necessity and limitations of evidence-based practice in stroke rehabilitation. Top Stroke Rehabil. 2003;10(1):71-8. https://doi.org/10.1310/crda-pgfw-khel-20e1. [ Links ]
18. Lin SH, Murphy SL, Robinson JC. Facilitating evidence based practice: Process, strategies, and resources. Am J Occup Ther. 2010;64(1):164-71. https://doi.org/10.5014/ajot.64.L164. [ Links ]
19. Metzler MJ, Metz GA. Analyzing the barriers and supports of knowledge translation using the PEO model. Can J Occup Ther. 2010;77(3):151-8. https://doi.org/10.2182/cjot.2010.77.3.4 [ Links ]
20. Park E, Forhan M, Jones CA. The use of digital storytelling of patients' stories as an approach to translating knowledge: A scoping review. Res Involv Engagem [Internet]. 2021;7(1):1-19. https://doi.org/10.1186/s40900-021-00305-x. [ Links ]
21. Strong DM. Supporting the "Casa Lar" social educator: A case study of a consultation using intercultural knowledge translation. Cad Bras Ter Ocup [Internet]. 2018;26(3):692-701. https://doi.org/10.4322/2526-8910.ctore1704. [ Links ]
22. Ramlo S. Mixed method lessons learned from 80 years of Q methodology. J Mix Methods Res. 2016;10(1):28-45. https://doi.org/10.1177/1558689815610998 [ Links ]
23. Damio SM. Q Methodology: An overview and steps to implementation. Asian .J Univ Educ. 2016;12(1):105-77. https://eric.ed.gov/?id=EJ1207820 [ Links ]
24. Walker BB, Lin Y, McCline RM. Q methodology and Q-perspectives® online: Innovative research methodology and instructional technology. TechTrends. 2018;62:450-61. https://doi.org/10.1007/s11528-018-0314-5 . [ Links ]
25. Webler T, Danielson S, Tuler S. Using Q method to reveal social perspectives in environmental research. SERI. 2009. [ Links ]
26. Lutfallah S, Buchanan L. Quantifying subjective data using online Q-methodology software. Ment Lex. 2019;14(3):415-23. https://doi.org/10.1075/ml.20002.lut. [ Links ]
27. Newman I, Ramlo S. Using Q methodology and Q factor analysis in mixed methods research. In: Tashakkori A, Teddlie C, editors. SAGE handbook of mixed methods in social & behavioral research. Thousand Oaks: SAGE; 2010. p. 505-29. https://doi.org/10.4135/9781506335193. [ Links ]
28. Brown SR. A primer on Q methodology. Operant Subj. 1993;16(3/4):91-138. [ Links ]
29. Akhtar-Danesh N, Baumann A. Q-Methodology in nursing research: A promising method for the study of subjectivity. West J Nurs Res. 2008;30(6):759-73. https://doi.org/10.1177/0193945907312979. [ Links ]
30. Rahma A, Mardiatno D, Hizbaron DR. Q methodology to determine distinguishing and consensus factors (a case study of university students' ecoliteracy on disaster risk reduction). In: e3s-conference.com. 2020. https://doi.org/10.1051/e3sconf/202020001003. [ Links ]
31. Carrier A, Levasseur M, Bédard D, Desrosiers J. Community occupational therapists' clinical reasoning: Identifying tacit knowledge. Aust Occup Ther J. 2010;57(6):356-65. https://doi.org/10.1111/j.1440-1630.2010.00875.x. [ Links ]
32. Alers V. Clinical reasoning psychiatric occupational therapy. In: Crouch R, Alers V, editors. Occupational Therapy in psychiatry and mental health. 5th ed. Chichester: John Wiley & Sons, Incorporated; 2014. p. 67-81. https://doi.org/10.1002/9781118913536.ch7. [ Links ]
33. Restall GJ, Egan MY. Collaborative relationship-focused occupational therapy: Evolving lexicon and practice. Can J Occup Ther. 2021; 88(3): 220-30. https://doi.org10.1177/00084174211022889. [ Links ]
34. Sumsion T, Law M. A review of evidence on the conceptual elements informing client-centred practice. Can J Occup Ther. 2006;73(3):153-62. https://doi.org/10.1177/000841740607300303. [ Links ]
35. Bailliard AL, Dallman AR, Carroll A, Lee BD, Szendrey S. Doing occupational justice: A central dimension of everyday occupational therapy practice. Can J Occup Ther. 2020;87(2):144-52. https://doi.org/10.1177/0008417419898930. [ Links ]
36. Chapparo C, Ranka J. Clinical reasoning in occupational therapy. In: Higgs J, Jones M, Loftus S, Christensen N, editors. Clinical reasoning in the health professions. 3rd ed. Philidelphia: Butterworth Henemann Elsevier; 2008. p. 265-77. [ Links ]
37. Teoh JY. How occupational therapy practitioners use virtual communities on the Facebook social media platform for professional learning: A critical incident study. Scand J Occup Ther [Internet] .2021;29(1):58-68. https://doi.org/10.1080/11038128.2021.1895307. [ Links ]
38. Carrier A, Levasseur M, Bedard D, Desorsiers J. Clinical reasoning process underlying choice of teaching strategies: A framework to improve occupational therapists' transfer skill interventions. Aust Occup Ther J. 2012;59(5):355-66. https://doi.org/10.1111/j.1440-1630.2012.01017.x. [ Links ]
 Correspondence:
Correspondence:
Azette Swanepoel
Email: swanepoela@ufs.ac.za
Submitted: 23 May 2023
Reviewed: 8 November 2023
Revised: 18 January 2024
Accepted: 19 January 2024
Data available: Upon reasonable request, from corresponding author
Editor: Blanche Pretorius https://orcid.org/0000-0002-3543-0743
Funding: The study from which this manuscript originated was funded by the University of the Free State Staff Doctoral Programme (USDP).
















