Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.54 n.1 Pretoria Apr. 2024
http://dx.doi.org/10.17159/2310-3883/2024/vol54n1a5
RESEARCH ARTICLE
Cultural perspectives and experiences of mental healthcare in Kwa-Zulu Natal, South Africa
Ashira MoonsamyI; Thavanesi GurayahII
IAkeso Clinic, Umhlanga, Kwa-Zulu Natal, South Africa. University of Kwa-Zulu Natal, Westville Campus, Durban, South Africa https://orcid.org/0000-0002-0305-3226
IIUniversity of Kwa-Zulu Natal, Westville Campus, Durban, South Africa https://orcid.org/0000-0001-9005-6355
ABSTRACT
BACKGROUND: Healthcare systems reflect worldviews, specifically in mental health, where norms dictate what is normal and abnormal. The era of coloniality promoted Western dogma over collectivist cultures, which were marginalised. This study explored the perspectives and experiences of Black, isiZulu-speaking, South Africans who utilised multidisciplinary services, based on a Western-based therapy model at a private psychiatric facility in KwaZulu Natal.
METHODS: A qualitative descriptive design was utilised. Purposive sampling was utilised to recruit 10 participants. Data was collected through semi-structured interviews. Braun and Clarke's six phases of thematic analysis were used to guide the data analysis.
FINDINGS: Three themes with sub-themes emerged from the data: personal perceptions, which explored how isiZulu-speaking people made sense of mental health and mental illnesses. Cultural perceptions were the collectivist method of problem-solving, which stressed the importance of spiritual beliefs. Health-seeking behaviour considered the experience of the isiZulu-speaking mental health care user. Cognitive dissonance prevailed due to the difference between westernised mental health treatment and traditional healing systems.
CONCLUSION: The family and community are intertwined in participation, reputation, and healing. There is an emphasis on enduring hardship and following traditions, which are preserved by valued elders. Disregarding these norms can outcast the Zulu individual who strives toward inclusion within the community.
IMPLICATIONS FOR PRACTICE:
• Intervention cannot only be at individual level but also community level.
• Including the family in psychoeducation and therapeutic goal settingwould be beneficial to the Zulu MHCU.
• Group programmes should address gender-specific issues.
• Occupational therapists must recognise the importance of participating in spirituality for the healing of the Zulu MHCU and appropriately include it in intervention.
• Mental health resources and awareness programmes need to be disseminated atcommunity level.
• Competency in the isiZulu language is recommended.
Keywords: mental health; mental illness; Zulu culture; cultural perspectives; culturally appropriate healthcare.
INTRODUCTION
Healthcare systems reflect worldviews, beliefs, customs and strategies for good health, appropriate diagnosis, and the prevention and cure of illness1. Systems such as these were created during the colonial era when power and privilege were afforded to Western culture and created a Western hegemonic discourse2. The hegemonic discourse surrounding culture and its use in guiding practice has become critical to explore3 in a diverse country such as South Africa.
Worldviews are deeply connected to how people perform and the meaning they ascribe to their occupations; hence, culture is of great interest to the client-centred occupational therapy profession3.
Considering mental health interventions specifically, these have been based upon attitudes and beliefs that govern or define what is normal and abnormal, or that which requires intervention. These norms and ideals are essential to the development of theoretical models and frameworks that guide psychiatric intervention both globally, as well as locally in South Africa.
Culture refers to perspectives, beliefs, knowledge, values, attitudes, assumptions, norms, and customs associated with belonging to a specific group of people, which, in turn, guides thinking, understanding, and behaviour4,5. Cultural dimensions need not be restricted to ethnicity or race but could include other factors of diversity such as class, gender, sexuality, and ability4. These dimensions which influence meaning attributed to occupation, also, unfortunately, render people unequal in society and affect the privilege, power, and opportunities they are afforded4.
Analysing occupational therapy theories in multicultural societies has become necessary for decolonizing occupational therapy theory and practice to incorporate diverse worldviews, mainly from the global South6. Decolonisation calls for disrupting the norm and questioning the appropriateness and utility of practices. Occupational consciousness becomes a central concept for disrupting the cycle of oppression through occupation2. It entails building an awareness of the dynamics of hegemony and recognising how this might be sustained in everyday occupational performance7.
Unfortunately, a wide variety of research thus far focused on the occupational therapist's challenge of working in diverse societies, rather than understanding the client's culture and how it influences their understanding of health, health-related behaviour and experiences5.
Furthermore, much research that looked at Traditional theories of ill health are outdated. One such study from Durban South Africa, was done by Edwards et al.8 in 1983. It highlighted the various theories underpinning mental illness of African clients compared to those of their Western counterparts. They found differences between Traditional and Western theories but also congruency in the differentiation between psychotic and non-psychotic disorder8. The Crawford & Lipsedge9 study of 2004 highlighted information about isiZulu cultural definitions of illness and the role that ancestors are believed to play in the construction of illness among Zulu people.
When researchers engage in research with the utmost respect for the perspectives and experiences of diverse cultures, they will move toward culturally safe theories that are inclusive of the truths that clients hold4. This study explored the mental health perspectives and experiences of mental health interventions among isiZulu-speaking, Black South African mental health service users (MHCUs), who participated in Western-based occupational therapy programmes. Thus, critical reflection will be engaged regarding the question: are mental health occupational therapy services appropriate for this dominant cultural group?
LITERATURE REVIEW
The existing literature related to this research has been divided into four sections as shown in Figure 1 below:
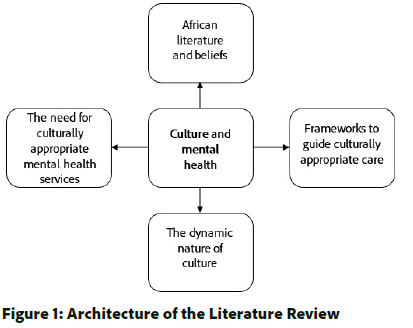
The dynamic nature of culture
Culture is dynamic, evolving and developing as the world evolves and develops, and as different cultures tend to coexist in shared spaces over some time4, thus necessitating consistent re-thinking and re-exploration. Factors such as language, personal experiences, and the environment among others, contributes to the construction of culture. As these factors shift and morph over time, so too will the culture. Cultural groups interact and these interactions will also contribute to a reconstruction of culture over time10. To comprehend what is of importance and relevance to the people, as well as to evaluate cultural safety and the appropriateness of occupational therapy practices, information must come from the sources themselves4.This study therefore aimed to gain insights into the suitability of current services for MHCUs from the Zulu culture in urban areas in KwaZulu Natal.
The need for culturally appropriate mental health services
Studies conducted globally have identified evidence of culturally inappropriate mental health services and their adverse effects on the people they were meant to serve11, 12, 13. These studies depicted the potential damage caused by well-intentioned services that neglected the clients' perspectives. Collectivist cultures view individuals as interconnected within their communities and place less emphasis on autonomy or independence14. Critical reflection and research are therefore imperative before providing services for people from collectivist cultures, or they risk undermining traditional and meaningful cultural beliefs and practices.
In pre-1994 South Africa, the apartheid government strongly disseminated the Western worldview as the ideal15. This "epistemicide", or near destruction of indigenous knowledge12 did not result in the abandonment of traditional and westernised health systems15, perhaps as a reflection of the meaning they still found in traditional practice.
In efforts to understand this diversity manifesting within mental health, five critical components from collectivist cultures were found:
• A reluctance to use talk therapy in the case that it would lead to more suffering;
• The shame of having a mental illness causing further reluctance to seek professional help;
• The power differentials between therapist and client;
• Collectivism as the preferred method of support; and
• Religion or spirituality as the root cause or utilised as a coping mechanism16,17.
Regardless of this knowledge of cultural diversity and mental health, most of the approaches toward intervention and counselling remain Eurocentric on a global level.
African literature and beliefs
A discourse analysis18 solidified the necessity of African research into cultural perspectives. Findings indicated a contradiction between traditional Zulu and Western theories of mental illness, leaving African individuals with the complex decision between two healthcare systems. Stigma towards mental health care users (MHCUs) developed through cultural beliefs and attitudes, and also significantly influenced how they were perceived and reacted to within their communities. Moreover, this stigma contributed to individuals with mental illness reducing their treatment adherence and health-seeking behaviours which increased their risk of relapse19. A study from 2004 in rural KZN identified that Zulu beliefs concerning ill health and suffering were closely linked to their religious beliefs, history, social relationships, and cosmology9. Beliefs around medical doctors were that they could understand and treat disorders known as "umkhuhlane" (illness by natural causes), but other disorders known as "ukufa kwabantu" (illness by supernatural causes), could only be recognised and treated by traditional healers.
This ideology still existed as recently as 2017 when Molot20 compared Western versus traditional treatment of mental illness in KZN. Explanations for the root causes of mental illness by traditional healers often included ancestral beliefs. Traditional healers also reported that they exclusively treated those bewitched or in trouble with their ancestors through methods such as burning "imphepho" (incense), cleansing, or traditional medicines. Ancestors are highly regarded and often linked to the wellbeing of the Black African individual and family9,20,21. Ancestors are the souls of the deceased elders who guide the living. When ancestors express displeasure or communicate with the family, they usually do so in the form of illness, suffering, dreams, or nightmares that must be appeased by specific rituals21
African culture reveres fundamental moral values such as patience, perseverance, modesty, industriousness, obedience, and respect for elders22. An individual creates their sense of self through others. The proverb "umuntu ngumuntu ngabantu", which translates to "a person is a person through other persons", fully encapsulates this belief22. Hence sources of motivation for the African individual include bringing honour to their name or clan, overcoming the limitations of their background, competing with others in their age group to achieve worth, appeasing the ancestors, and having the desire to be part of a community and receive social support22.
Frameworks to guide culturally appropriate care
Frameworks utilised in occupational therapy practice possibly achieved dominant status due to the influence and power accrued by the Western culture4. Initially, cultural competence was utilised as a framework for mental health professionals to practise efficiently within culturally diverse settings. It required practitioners to become familiar with the cultural values, customs, and traditions of the people they served. However, research has indicated that these cultural competence models are insufficient and can be problematic due to their ignorance of the dynamics of power and oppression4,16,23. Cultural humility has been proposed as more appropriate as it requires therapists to become critical thinkers. It is an awareness of one's own positionality and understanding of how this influences perspectives which may differ from others, and posits that cultural differences lie within the therapist-client relationship and not only from the clients' perspective only4. Developing this entails evaluating intersecting identities and the scrutiny of common knowledge that is defined as truth. This redresses the power imbalance within the client-therapist relationship and enhances the therapy process4,23.
METHODOLOGY
Study design
This study employed a descriptive qualitative approach. This approach was useful in the exploration of the perspectives and experiences of Black, isiZulu-speaking South Africans who had utilised multidisciplinary services at a private psychiatric facility, underpinned by a western-based therapy model in KwaZulu Natal. A qualitative design was best suited to this study that explicated the concepts of meaning and experience from the clients' point of view regarding the healthcare system in KZN24.
Selection and sampling strategy
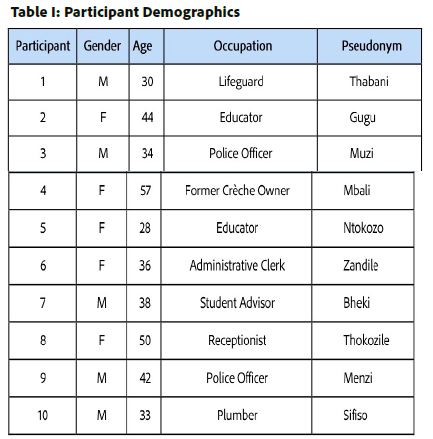
Purposive sampling was used, where a group of people is intentionally selected to best answer the research question posed25,26. There were 10 participants in this study and data saturation was reached. All participants were ex-patients of the facility. Participants were required to be Black South African individuals of Zulu cultural heritage, i.e., an isiZulu-speaking person who grew up embedded within the culture. Participants had to have attended their group therapy programme provided by the facility which included occupational therapy services. Participants were above the age of 18, and had access to a video-call compatible device such as a laptop, computer, or cell phone. See participants' demographic details in Table I (below):
Research setting
This study occurred in the KwaZulu Natal province of South Africa, specifically in the city of Durban. The predominant cultural group residing in KZN are the Zulu people. The study focused on MHCUs from the Zulu culture who were previously admitted to a private psychiatric facility based in one of the more upmarket areas of Durban. However, the client population comes from all over the city and country. MHCUs seeking assistance at the clinic present with depression, anxiety disorders, post-traumatic stress disorder and other psychotic disorders. Participants were informed about the study prior to discharge and allowed to participate by leaving their contact details with the therapist during the discharge group.
Data collection procedure
A pilot study was conducted with two participants to ensure that questions would be understandable to participants and that they would elicit the responses required to answer the research question. The pilot study revealed that the questions were appropriate. An interviewer matching the description of a Black, isiZulu-speaking South African was contracted to conduct the interviews, while the first author acted as a moderator during the interview, noting observations of the participants. This created a more comfortable interview space for the participants and allowed them to express themselves in isiZulu.
A semi-structured interview schedule drawn up by the researcher was used to guide the conversation during a virtual interview. Open-ended questions were designed to elicit responses relevant to the research question and allowed participants to diverge into new concepts that arose during the conversation. Interview questions explored attitudes and beliefs surrounding mental health, mental-health-related practices, and experiences of the mental health programmes at a private psychiatric facility.
Trustworthiness
The semi-structured interview schedule questions were utilised to redirect participants who strayed off the topic. Questions were rephrased to confirm or enhance the understanding of either the interviewer or the participant. Participants reserved the right to withdraw their participation at any time before disseminating the results. The researcher worked through transcriptions and interpretations multiple times, and debriefed with the supervisors of the study. The researcher engaged in reflection through journaling to evaluate her positionality as an Indian female who was an outsider to the Zulu culture, to uncover preconceived personal ideologies and to identify how it may impact interpretations of the data. An audit trail of the recordings and transcriptions was kept for record purposes.
Ethical Considerations
This research study was approved by the Biomedical Research Ethics Committee (BREC) at the University of Kwa-Zulu Natal (Ref. no. BREC/00002882/2021). The research process was carried out according to the research guidelines to ensure scientific integrity. Gatekeepers' permission was obtained from the facility, and participation in the research study was voluntary. Telephonic or virtual interviews were more cost-effective. Participants were blind to each other as individual interviews were used. This offered them confidentiality. Participants' stress was minimised by fully informing them about the study during a discharge group and then again during the interview. Participant information sheets were issued to and discussed with them. Participant names and all other identifying features were not included in reporting the data. Participants were treated with respect and sensitivity, and their cultural viewpoints were respected.
Data Analysis and Findings
Data Analysis
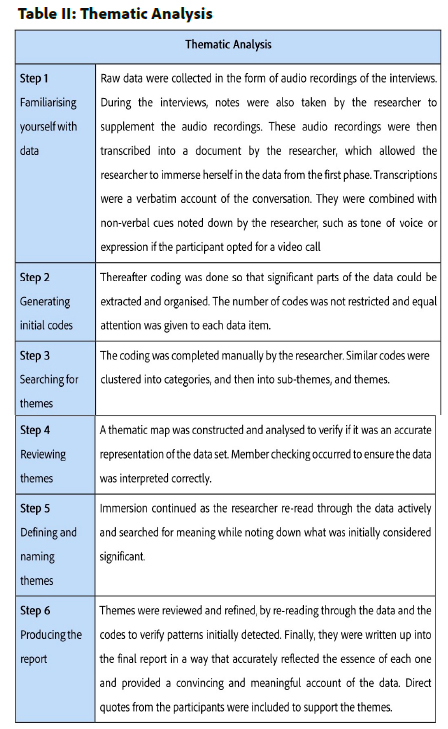
A thematic analysis (Table II, below), of the data were conducted. Thematic analysis has the potential to reflect the current reality and uncover what underlies it, which is in line with the aim of this research. The six steps of thematic analysis were followed as outlined by Braun & Clarke27. Thereafter a deductive analysis was conducted using the Ecology of Human Performance Model28.
FINDINGS
This section presents the themes derived from the results this study. The findings of this study were viewed through the lens of the Ecology of Human Performance Model. The basic tenets of the model include the person, the context and the task28. Findings relating to these concepts are presented, integrated and discussed. Three themes were derived, namely Personal perspectives, Cultural perspectives, and Health-seeking behaviours. Each theme and its sub-themes are depicted in Figure 2 (below).
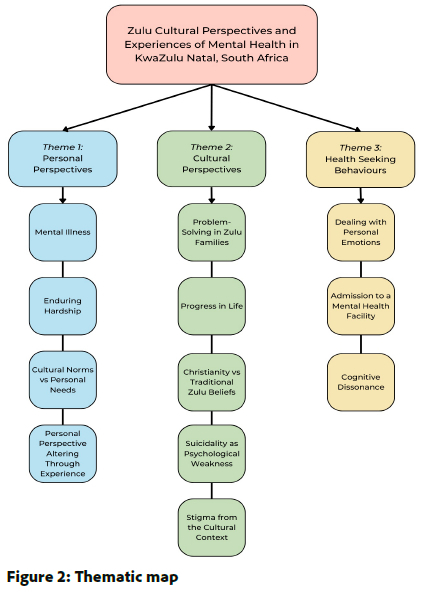
Theme 1: Personal Perspectives
This theme considered the aspects of the Zulu individuals' perspectives concerning mental illness and some of the causal factors described by the participants. The sub-themes that emerged under this theme were mental illness, enduring hardship, cultural norms versus personal needs, and personal perspective altered through experience. The personal perspectives of Zulu people are created in relation to societal perspectives.
Mental illness
Participants expressed that the concept of mental illness does not naturally emerge in Zulu culture and is regarded as a Western concept. This makes it difficult for MHCUs to be understood and supported as needed. Healthcare for physical ailments is recognised, but mental health services are not. Participants expressed that, prior to being referred to the facility, they were not aware of these services being available under Western healthcare. Mental illness, when recognised, is seen asa "white person's problem".
"Then when it comes to mental health, according to our culture there is no such a thing called stress or depression... if you said you are stressed or you are having a depression, they think that you are having a drama, you are westernised, you are colonised, they think all of those things, they think maybe you think you are a better person than them." (Thokozile)
Enduring hardship
Enduring hardship is presented as a core characteristic required of the Zulu individual. It is expected to be displayed in different ways by each gender. In traditional Zulu families, the eldest male is regarded as the family's provider, decision maker and leader. Male participants expressed that this role required them to present as emotionally strong and worthy of respect. A man must not disclose incapacity in order to lead the family, or handle situations that arise, lest he loses respect, as seen in Bheki's narrative which follows:
"...in difficult moments as a male you're not supposed to cry. People are looking up to you and must find hope in you so you must find a coping mechanism. If you're the one crying, what about the children, what about the wife, the sister or someone. So, if you cry, you go into a corner somewhere and cry alone. But in front of everyone, everything should be ok." (Bheki)
Leaving a marital relationship would be construed as a sign of weakness for a female. Even in times of injustice, Zulu females were expected to remain as caregivers and submissive wives. While this ideology is still present, they are currently afforded opportunities to education and work, supporting themselves and their families. With these shifts, the expectation of financial provision is no longer restricted to males, as females can now be educated, employed, and are expected to provide for their families financially. Thus, both males and females are held to the expectation of being strong and not expressing hardship.
"I feel obligated, I don't know how. I feel obligated to take care of them because you are the only one who is educated you know... Hawu, why is she coming and asking us for rice, why, when there is a teacher in that house, you know" (Ntokozo)
Cultural norms versus Personal needs
Zulu culture promotes collectivism and the practice of Ubuntu, which can override or conflict with the needs of an individual in this interdependent culture. It was expressed that in a Zulu family, people were raised to be givers and helpers. A popular act was self-sacrificing for the well-being of others, even when one was not in a position to assist. Participants, therefore, struggled with setting healthy boundaries.
"What I can say about what led me here is firstly I wanted time out. I give and I give and I give and I give until there is no me."... "we call it in isiZulu nika nika." (Ntokozo)
This also materialised as "Black tax", defined as an unspoken obligation to help others or an extended family when you have achieved well yoursef29.
"Black tax is when you, they feel you are, same word, obligated to do certain things because you are earning more or you are more educated. Black tax is like blackmail towards your mind, towards your soul and how you see things." (Ntokozo)
Due to the Zulu culture being a collectivist culture, informational support usually came from someone in the individuals' network who had experienced mental health services themselves. Alternatively, they would get referred to a traditional healer.
Personal perspective altering through experience.
Participants saw a need to adapt their mindsets after their experience of a mental health service. Participating in the programme at the facility altered their perceptions of mental illness from being non-existent within Zulu culture to being existent and treatable.
"We are not in the era where our grannies, grandfathers and ancestors were. We are in an era whereby we need to use the tools that are there, yeah. So, we need to shift our mindset, not forget our roots but shift our mindset and try to accommodate the new change that is around us." (Ntokozo)
The older generation, who had different educational opportunities or grew up in rural contexts, were not easily convinced about the benefits of seeking mental health services.
"I don't think I'd even try with him (participant's father) because that absolutely... it never existed in his mind so I think now with the younger generation the more we go to school... eh... the better we understand. But with the elderly people or with the people especially from rural areas... like real rural areas, they'll not attend a psychologist. I don't think you can convince one to attend" (Bheki)
Theme 2: Cultural perspectives
This theme considers how Zulu people are socialised to conduct themselves in their cultural context, specifically when it concerns hardship or mental illness. The sub-themes that emerged were problem-solving in Zulu families, progress in life, Christianity versus traditional Zulu beliefs, suicidality as a psychological weakness and stigma within the cultural context.
Problem-solving in Zulu families
Problems are dealt with collectively within the Zulu culture. Maintaining honour and reputation in a family are important21, and thus issues would not be expressed outside of the family space. Issues experienced by the Zulu person must be taken to the elders, who will advise that they must be dealt with internally. Discussing problems with an individual external to the family is regarded as shameful. It was also expressed that, often, the elders in the family would instruct them to remain silent about what they were experiencing.
"Normally the elders they come together and then they said this thing should be for the family and must not go out". (Thokozile)
Progress in life
Zulu individuals and their families value progress in terms of social status, finances and assets. The progress of the individual means progression for the family. Thus, there is an unspoken expectation and drive to progress. The pressure is felt through subtle societal expectations or comparisons with their peers.
"...you want to progress in life. Can you imagine you grew up... and you 35 or 40 years and you still stay at home? That's not right, by that time you need to have your own house, have your own family." (Menzi)
Christianity vs Traditional Zulu beliefs
Each participant expressed some form of spiritual belief system. Many behavioural shifts or changes in a person are initially attributed to spiritual causes in the Zulu culture.
"Oh! They think maybe you are crazy or you are a witch because they don't know anything about mental illness." (Gugu)
Spirituality is an essential concept to all Zulu people, some believing in God, some in ancestors and others having a dual belief system, combining the concept of God and ancestors. For some individuals, a conflict exists between cultural beliefs and God, which is seen as a Western concept.
"Some people chose to pray only to God and then obviously the majority uh, stayed with the ancestors and the rituals. Uhm, and then a part of the people would just mix the two, they would have like, they would pray to God, for God to help them connect with their ancestors or the other way around..." (Muzi)
Ancestors were either regarded as protectors and providers, or as negotiators between the tangible and intangible realms or God.
"We do these things to make sure they protect us from sicknesses, illnesses..." (Menzi)
"Our thing is they negotiate. They are like the negotiator between us and God. It's how we grew up." (Ntokozo)
Participants who believed in their ancestors believed that they could express dissatisfaction with them, through mental illness and specific rituals that need to be completed to appease them.
"...there were certain things that were done at home, rituals and maybe now you are the older one, or you have your own family... we are not following those proceeding stuff so whatever that is not right, that is happening to you, it might be pinned to that...if she can do this and this because it's what was required of her, then things will come back to normal." (Bheki)
Whether they described themselves as Christians or revering ancestors, most participants had expressed a sense of respect for their ancestors. Some combined the belief systems, while others merely acknowledged their ancestors.
"I am a Christian. But praying to God, but that doesn't mean I cannot do uh our cultural things... there are things that as Zulu nation you need to do... whether you are Christian or not, you need to do it, it's a must." (Menzi)
"The only thing that I believe is that there is God, and if you pray, you will receive what you are praying for." (Thokozile)
Suicidality as psychological weakness
Poor coping skills and inadequate emotional support can lead to a sense of hopelessness and possibly suicidality which is viewed as a weakness in the Zulu culture. Due to the expectation to withstand and persevere through hardship, an individual may be reluctant to ask for help. As with other cultures, there is a major concern about suicide in the Zulu culture. Many people turn to it after feeling there is no way out of their problems. Multiple participants expressed that suicide was seen as a weakness, but the underlying causes were often overlooked:
"...some people they even commit suicide you know. Because whatever that they going through they think they can handle it, until they cannot handle it anymore and then their only solution is to take their life." (Menzi)
Participants expressed that a specific ritual of beating the dead body of a person who commits suicide must be carried out to ensure that the spirit of the person who committed suicide does not infect the other family members. This solidifies the concept of suicide being seen as a weakness instead of an act of hopelessness, an act associated with mental illness.
Stigma within the cultural context
Participants expressed that stigma within their cultural context emerged in the form of terms to describe mental illness (MI). Descriptive concepts of MI include expressions of:
"uhlanya" (Zandile)which translates to 'crazy', "islima", and "ustupito" (Zandile), which translates to' stupid', "ziyarara", (Zandile), which is understood as a person having 'bees buzzing in their heads'.
These words convey stigma, misrepresent MI and outcast the MHCU. MHCUs are labelled by these words and are often not taken seriously due to these labels. A consequence of this is that the participants were reluctant to disclose their mental illnesses. Adverse or dismissive reactions to emotional expressions adversely impacted the participants' mental health.
"That is why I am here, my husband wasn't supporting me, he started not speaking with me, he started ignoring me, he started telling me...he started like rejecting me because I was suffering from depression and anxiety and he told me that "No you don't have a problem, it's just that you want attention from us and you won't get it".". (Zandile)
Theme 3: Health-seeking behaviours
This theme outlined the processes of dealing with mental illness for the Zulu individual when it became overwhelming and difficult to ignore. The sub-themes discussed hereafter include dealing with personal emotions, admission to a mental health facility and cognitive dissonance.
Dealing with personal emotions
This sub-theme explores the explanations of how overwhelming emotions were dealt with by the Zulu MHCU prior to admission. Many participants reported that they only noted a decline in their health once they experienced physical symptoms of MI or irregular behaviours such as isolating themselves. These symptoms are what often prompted health-seeking behaviour.
"...losing weight, having headaches, not feeling to talk to other people, most of the time I was sleeping, not wanting to talk to anyone....They didn't find what made me sick until they brought the psychiatrist." (Thokozile)
Admission to a mental health facility
This subtheme details the experience of Zulu MHCUs who were admitted to an inpatient programme. The participants were initially reluctant to access the mental health services they learnt about, and when they did, they described their internal conflicts.
"The first time I attended a psychologist, I felt terrible in a sense. I asked myself, am I ok? What's wrong with me? Something's wrong with me. I'm attending a psychologist and now I need to say and open up to someone and maybe that person will also see me and think "No, this guy is weak"." (Bheki)
A profound response from each participant was that they were astounded by the fact that they were not alone in what they were experiencing.
"I think I realised that it, it's like whatever that I'm going through I'm not alone in this ...and all these people are also dealing with so many things, and that's why they are here." (Muzi)
Participants felt relief at the validation they received from each other. They found that understanding the problem and solving it practically with support was helpful. Speaking to someone who can provide perspective or understanding improved their wellbeing. The facility was seen as a healthy distraction from their challenging or sometimes toxic environments, and they could think more rationally. The facility was a safe space to express their vulnerability, where someone would listen attentively, care about what was being expressed, and be non-judgemental. The facility allowed and encouraged a focus on the self, specifically allowing them to express themselves without fear of criticism or judgement for going against cultural norms. Participants found value in the diversity of available group therapies.
"...it makes me feel better Too much. I am feeling better because of it. Those activities as well as the talking with others, but before I went to (the facility), I don't get to do all that" (Mbali)
"And I get a chance to learn about so many things that will boost my self-esteem and also that will help me find out who I was and what I really want." (Thabani)
Participants recommended that spirituality be integrated into the care they received due to it being so pivotal to most of their lives. However, this is acknowledged as challenging, due to the diversity of spiritual beliefs.
"Yes, spirituality, yes yes yes. We need that, it's lacking, but I think so...not exactly Christian but someone must be fair...you can't just bring Christianity and leave others. We need some spirituality. Yes, I would suggest that." (Zandile)
There are culturally specific issues that need to be expressed. To truly express oneself, the isiZulu language is necessary.
"Yes, language plays a huge role, you know English is not our mother tongue so there are things that we want to say or express but we can't express them in English... So, what happens now? You keep quiet... So, you come to (the facility) with a problem, you go home with the very same problem." (Menzi)
Participants felt a need for an increased length of stay in the facility to enhance their understanding, identify problems, and improve their skills and coping strategies. The duration of admission reported by the participants was up to two weeks. There was also a need for external support. This type of experience was more accessible in private rather than public facilities, estranging those without access to medical aid or funds.
Cognitive dissonance
Zulu MHCUs who had experienced a Western mental health services expressed that their experiences differed. This cognitive dissonance caused participants to express anger at their culture for not acknowledging and educating them about mental health and illness.
"Black culture! Black culture, what I can say...they are emotional abusers." (Zandile)
Participants felt that culture acknowledged the change in tangible aspects, but did not readily recognise or adapt according to intangible factors like mental illness.
"For example, like uhm having lobola, lobola used to be walking cows, it was a must that it must be walking cows. Now I live in (the city), there is no grass (laughter). I can't make it a cow; it will be like eyoh what is she doing and the cows will be gone in the morning. So, what do I do? You must give me money instead of the cows. Each cow has its own money value so we adapt... change. Why can't we adapt to that change and adapt to all changes concerning culture. When it comes to money we are like yes, yes, its fine but when it comes to uh certain things like mental health- no, no, no it's not okay." (Ntokozo)
Participants further emphasised the need for education and awareness surrounding mental health. Beyond the treatment of the Zulu MHCU, there was a need for education with families.
"So, what I would suggest, we need to go back to the families, to teach them about depression and anxiety and about triggers" (Ntokozo)
DISCUSSION
Participants expressed that experiencing mental illness and participating in westernised treatments conflicted with their culture. Mental illness and mental health services were described as unfamiliar to most participants. Explanations for the behaviours related to mental illness were often linked to beliefs in the spiritual dimension. These spiritual dimensions differed, either revering God, ancestors or a combination of both. This confirmed their beliefs of a human and spiritual plane within which activity occurs21. The rituals participated in ranged from traditional, where the use of a sangoma* or an inyanga** was required, to religious rituals, where the church and prayer to God were leaned upon for wisdom. Personal spiritual beliefs were a source of strength and a coping mechanism for the Zulu individua16, 17. Treatment in the facility often did not include spirituality, and participants felt strongly that it should be introduced into the treatment programme.
Another critical concept of the Zulu culture was the ideology that each individual must possess strength. Participants in this study specifically referred to an individual's emotional or psychological strength. It was found that each gender was expected to display strength in different ways. Traditionally, Zulu males felt the pressure to present as symbols of strength. They believed they could not to express emotions or vulnerability in front of others as this was considered a weakness32. Males generally dealt with their emotions through substance use, which was seen as more acceptable, or displayed aggression as an emotional outlet. Female strength was measured by persevering through marriage and family. Women are traditionally required to be submissive and dependent on the Zulu patriarch, and are subjected to silence when enduring injustice for fear of loss of provision. With temporal shifts in the context, females now have access to education and work that they did not always access previously. Educated females are now subject to similar expectations of provision and strength within the household. However, educated females who provide for their families still do not receive the respect or honour afforded to a male provider.
The expectation of strength is further tied in with the need to progress and improve the family's reputation. This progress would be measured in terms of the status, financial position, or assets of the individual. However, the Zulu individual's reputation is linked to their family or community's reputation22. They are therefore required to follow customs or norms22 lest they bring shame to their collective name. The issue arose where the need to progress in life is so entrenched that it necessitates creating more hardship to maintain the image of progression. An inability to admit to experiencing adversity emerged, and consequently a sense of helplessness. With a reluctance to ask for help and an inability to cope, some might turn to suicidal acts. Suicidality was not considered an act of helplessness, but rather a personal weakness. Participants expressed that they could not explain mental illness or psychological distress to their families. The Zulu individual created their sense of self within their community22, thus silence and isolation can be counterproductive to the Zulu MHCU's healing.
Experiencing emotional hardship is therefore not easily admitted to or spoken about. However, when admitted to the facility, talking about their issues and developing solutions were seen as an enhancement to their state of mind. If there was a need to talk about an issue, the Zulu individual must approach their close family, especially their elders.
Elders in the Zulu culture pass on rich cultural knowledge but an insufficient understanding of mental health. Being a historically marginalised group, the effects remain evident. Elders whose voices are central in advising or problem-solving promote strength and coping through endurance, strategies they were forced to implement under the apartheid regime and continue to pass on18. Thus, discussing issues within a mental health facility conflicted with their cultural norms.
This was concerning as family or community-related issues are often causal factors of MI for the Zulu community. Zulu people are raised to be helpers and givers, with the spirit of Ubuntu instilled within them30. However, this sometimes translated into a lack of boundaries and being taken advantage of by those who do not reciprocate the concept of Ubuntu. 'Black tax' was an example of this. If an individual was advancing in their career or earning well, they were obligated to provide for the extended family29. Participants expressed that this placed a significant burden on them, and they struggled to take care of their own needs versus their community's.
The importance of forming part of a community was emphasised by participants. Stigmatised names within the community context, attached to MI, caused more reluctance to reveal illness or seek help for the Zulu individual18. Due to the fear of being cast out or labelled and not valued in their communities, many would remain silent. For younger or urban participants, the perspective could alter through experience, but more entrenched cultural beliefs existed within rural communities and older generations. To avoid the loss of community, the Zulu individual may attempt to manage emotions in isolation. When negative emotions overwhelmed the Zulu individual, and no outlet for expression was available, they had to be suppressed. As previously described, unhealthy coping mechanisms were employed, such as substance use or displays of aggression.
Despite this reluctance to admit to experiencing hardship, support, in whichever form, was primarily sought from each other in the Zulu culture17. In communities, considering sickness a spiritual issue was often more acceptable than acknowledging it was a mental illness. Thus, Zulu individuals and their families would seek help from their spiritual community. For the Christian Zulu, this would be their pastor; for the traditional Zulu, it would be a sangoma or traditional healer. Rituals or prayers that were performed did have a positive impact on the mental state of most Zulu individuals. Referral to westernised mental health services occurred either when symptoms manifested physically, such as headaches or poor appetite, and did not improve; or when peers, familiar with mental health, noticed their symptoms. Being admitted to the facility left these isolated individuals relieved by the feeling of "I am not alone". Solidarity was advantageous to the Zulu MHCU's healing31, and this was found in the facility. Moreover, the facility presented a healthy distraction and a safe space to learn, share and heal through vulnerability.
The cognitive dissonance was heightened when they realised, they were experiencing mental illness. This aroused anger towards their own culture when faced with Western versus traditional healthcare systems. Mental illness which was initially regarded as 'a white person's problem', was found to exist in them as well. However, Zulu culture cannot be blamed for the lack of recognition of mental health, especially when it was introduced by a culture that neglected to take their worldviews into account and silenced their voices18. However, considering it a "white person's illness" built a stigma and was counterproductive to health-seeking behaviour. Understanding that MI exists within all cultures but can be treated in various ways due to the different causal factors enhances health-seeking behaviour.
Time in the facility was often reported as minimal as the process of altering perspectives and improving their mental state, for the Zulu individual, was a more complex and time-consuming task. Many Zulu individuals expressed the need for more time to learn about mental illness, understand its causes and apply it directly to themselves before learning contextually appropriate skills. Most participants verbalised that their two-week stay was insufficient. This indicated a need for outpatient or community-level mental healthcare services and resources.
Moreover, the isiZulu language was inseparable from the culture, and their experiences could, at times, only be efficiently described using their 'mother tongue'. Participants expressed that there were cultural concepts that were interrelated with their wellbeing. One such concept was that of 'black tax'.
Private mental health services were not easily available and excluded those without access to medical aid. Thus, a large proportion of the Zulu community were unable to access healthcare for issues such as depression and anxiety. It was deemed that only the individual with 'very severe' psychotic features belonged in a public mental healthcare facility. This could perpetuate the discourse that mental health was a "white persons' problem."
The Zulu culture has been subjected to adaptation with temporal shifts. However, the tangible adaptations tended to be more easily integrated, such as female and male roles, as well as Lobola. Intangible shifts, such as the understanding of mental health, tend to be viewed as out of their control, and was a stumbling block to change. To promote understanding of MI and reduce stigma, there is an urgent need for the dissemination of mental health awareness campaigns within the Zulu communities. While the causal factors and healing activities may differ for the Zulu culture, the understanding of mental health could significantly enhance the Zulu MHCUs mental health seeking and treatment. Both systems of healing, Western and traditional, seem to be beneficial to the Zulu MHCU.
Recommendations
• Occupational therapists intervening with people from the Zulu culture must account for the collectivist nature of the culture by designing interventions that includes the family or community. Intervention for the Zulu MHCU must be culturally appropriate and reflect their context.
• The Zulu culture is a strongly collectivist culture where the individual, their participation and issues are inextricably linked back to their context and so is their healing. Including the family in psychoeducation or therapeutic goals would be of benefit to the Zulu MHCU.
• There is an ingrained idea of strength through silent endurance of hardship, which was appropriate under the apartheid regime, but is no longer beneficial to the Zulu community whose voices must be highlighted. Occupational therapists in mental health would do well to promote the development of resilience and healthy coping strategies among Zulu MHCUs.
• Understanding spirituality and diversity are essential in occupational therapy education. This ensures holistic care and respect for diversity. Occupational therapists must be equipped to respond to spiritually diverse populations and promote meaningful participation. Each individual will differ in belief, and occupational therapists can explore this as a coping mechanism for their clients.
• There are defined gender roles in the Zulu culture, and each has different issues. Group programmes that include gender-specific discussions are necessary.
• Mental health awareness and resources need to be disseminated at the community level to decrease the doctrine of isolation and helplessness when experiencing MI.
• The isiZulu language is essential to the expression of issues experienced, and resources or therapies carried out in isiZulu would be beneficial.
• There is scope for research within rural communities to compare their constructs of mental illness to urban communities.
• Group-centred therapy has been beneficial for Zulu MHCUs admitted to the facility and are an appropriate mechanism to facilitate healing.
Limitations
The study was limited in that participants were mainly from an urban background who had access to private mental health care. Only one facility and its programme were studied to reduce confounding variables. Culture in urbanised settings differ from rural settings due to the difference in interaction with other cultures. Thus, findings of the study would not be inclusive of persons in rural areas where there is decreased cultural diversity.
CONCLUSION
Culture contributes to creating norms and provides occupational constraints and opportunities depending on the person's identity. The privilege of safely and acceptably practising occupation in a way that is seen as culturally appropriate depends on the power afforded to that culture, and the acceptance of it in society, as well as the positionality of the person concerned. This study will help therapists to understand factors that affect the Zulu MHCU's mental health and how to better equip them with skills, while maintaining culturally appropriate interventions. A significant cognitive dissonance occurs for the Zulu individual whose cultural norms differ from westernised mental health services. While these health services are beneficial, the Zulu MHCU risks going against cultural norms and does not want this to impact their inclusion into their communities. Zulu individuals create their sense of self through interaction with their communities and value their acceptance. Therefore, the community or families of the Zulu MHCU are essential to include in intervention programmes to keep them informed, create awareness and increase the sustainability of the interventions. With consistent research into the perspectives and experiences of the Zulu community an enhanced understanding of their participation can be built. This contributes to improved service provision and does not perpetuate the marginalisation of their viewpoints and indigenous knowledge.
Acknowledgements
The authors would like to acknowledge the psychiatric facility involved and the participants for their participation, and T. Lingah for her valuable guidance as co-supervisor if this study.
Competing interests
There are no competing interests to declare.
Author contributions
The research study was conceptualised as an action of the researcher for her postgraduate research as well as the collaboration of her supervisors as part of a master's degree programme. T. Gurayah co-supervised the study and provided feedback throughout the process (i.e. literature review; protocol; data collection and interpretation; and findings). A. Moonsamy contributed to the writing of the research article and T. Gurayah reviewed and edited the research article.
REFERENCES
1. Benedict, A. O. (2014). The perception of illness in traditional Africa and the development of traditional medical practice. International Journal of Nursing, 1(1), 51-59. Available: Microsoft Word-5.doc(ijnnet.com). [ Links ]
2. Kessi, S., Marks, Z., & Ramugondo, E. (2020) Decolonizing African Studies. Critical African Studies, 12(3), 271-282, https://doi.org/10.1080/21681392.2020.1813413. [ Links ]
3. Castro, D., Dahlin-Ivanoff, S., & Mârtensson, L. (2014). Occupational therapy and culture: a literature review. Scandinavian Journal of Occupational Therapy, 21(6), 401-414. https://doi.org/10.3109/11038128.2014.898086. [ Links ]
4. Whalley Hammell, K. R. (2013). Occupation, well-being, and culture: Theory and cultural humility/Occupation, bien-être et culture: la théorie et l'humilité culturelle. Canadian Journal of Occupational Therapy, 80(4), 224-234. https://doi.org/10.1177/0008417413500465. [ Links ]
5. Zango Martin, I., Flores Martos, J. A., Moruno Millares, P., & Björklund, A. (2015). Occupational therapy culture seen through the multifocal lens of fieldwork in diverse rural areas. Scandinavian Journal of Occupational Therapy, 22(2), 82-94. https://doi.org/10.3109/11038128.2014.965197. [ Links ]
6. Ramugondo, E. (2018). Healing work: intersections for decoloniality. World Federation of Occupational Therapists Bulletin,74(2),83-91. https://doi.org10.1080/14473828.2018.1523981. [ Links ]
7. Ramugondo, E. L. (2015). Occupational consciousness. Journal of Occupational Science, 22(4), 488-501. https://doi.org/10.1080/14427591.2015.1042516. [ Links ]
8. Edwards, S. D., Grobbelaar, P. W., Makunga, N. V., Sibaya, P. T., Nene, L. M., Kunene, S. T., & Magwaza, A. S. (1983). Traditional Zulu theories of illness in psychiatric patients. The Journal of Social Psychology, 121(2), 213-221.https://doi.org/10.1080/00224545.1983.9924491. [ Links ]
9. Crawford, T. A., & Lipsedge, M. (2004). Seeking help for psychological distress: The interface of Zulu traditional healing and Western biomedicine. Mental Health, Religion & Culture, 7(2),131-148.https://doi.org/10.1080/13674670310001602463. [ Links ]
10. Hassim, J., & Wagner, C. (2013). Considering the cultural context in psychopathology formulations. South African Journal of Psychiatry, 19(1), 7. https://doi.org/10.4102/sajpsychiatry.v19i1.400. [ Links ]
11. Al Busaidy, N. S. M., & Borthwick, A. (2012). Occupational therapy in Oman: the impact of cultural dissonance. Occupational Therapy International, 19(3), 154-164. https://doi.org/10.1002/oti.1332. [ Links ]
12. Nyamnjoh, F. B. (2012). Blinded by Sight: Divining the Future of Anthropology in Africa. Africa Spectrum, 47(2-3), 63-92. https://doi.org/10.1177/000203971204702-30. [ Links ]
13. Greene, M. C., Jordans, M. J., Kohrt, B. A., Ventevogel, P., Kirmayer, L. J., Hassan, G., Chiumento A., van Ommeren M. & Tol, W. A. (2017). Addressing culture and context in humanitarian response: preparing desk reviews to inform mentalhealthandpsychosocial support.Conflict and Health, 11(1), 1-10. https://doi.org/10.1186/s13031-017-0123-z [ Links ]
14. Van Dyk, G., & De Kock, F. (2004). The relevance of the individualism - collectivism (IC) factor for the management of diversity in the South African national defence force. SA Journal of Industrial Psychology, 30(2). https://doi.org/10.4102/sajip.v30i2.155. [ Links ]
15. Mokgobi, M. G. (2014). Understanding traditional African healing. African journal for physical health education, recreation, and dance, 20(Suppl 2), 24. https://doi.org/10520/EJC162333. [ Links ]
16. Gopalkrishnan, N. (2018). Cultural diversity and mental health: Considerations for policy and practice. Frontiers in public health, 6, 179. https://doi.org/10.3389/fpubh.2018.00179. [ Links ]
17. Hechanova, R., & Waelde, L. (2017). The influence of culture on disaster mental health and psychosocial support interventions in Southeast Asia. Mental health, religion & culture, 20(1), 31-44. https://doi.org/10.1080/13674676.2017.1322048. [ Links ]
18. Daniels, A. L., & Isaacs, D. (2022). Cultural constructions of the mentally ill in South Africa: A discourse analysis, part one. Culture&Psychology,0(0).https://doi.org/10.1177/1354067X221131998. [ Links ]
19. Egbe, C. O., Brooke-Sumner, C., Kathree, T., Selohilwe, O., Thornicroft, G., & Petersen, I. (2014). Psychiatric stigma and discrimination in South Africa: perspectives from key stakeholders. BMC psychiatry, 14(1), 1-14. https://doi.org/10.1186/1471-244X-14-191. [ Links ]
20. Molot, M. (2017). Discourses of Psychiatry and Culture: The Interface Between Western and Traditional Medicine in the Treatment of Mental Illness. Independent Study Project (ISP) Collection.2582. Available: https://digitalcollections.sit.edu/cgi/viewcontent.cgi?article=3605&context=isp_collection [ Links ]
21.Kpanake, L. (2018). Cultural concepts of the person and mental health in Africa. Transcultural psychiatry, 55(2), 198-218. https://doi.org/10.1177/1363461517749435. [ Links ]
22. Nwoye, A. (2017). An Africentric theory of human personhood. Psychology in Society, (54), 42-66. https://doi.org/10.17159/2309-8708/2017/n54a4. [ Links ]
23. Whalley Hammell, K. R. (2015). Client-centred occupational therapy: the importance of critical perspectives. Scandinavian Journal of Occupational Therapy, 22(4), 237-243. https://doi.org/10.3109/11038128.2015.1004103 [ Links ]
24. Hammarberg, K., Kirkman, M., & de Lacey, S. (2016). Qualitative research methods: when to use them and how to judge them. Human reproduction, 31(3), 498-501. https://doi.org/10.1093/humrep/dev334. [ Links ]
25. Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches. Third Edition. Sage publications. [ Links ]
26. Moser, A., & Korstjens, I. (2018). Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. European Journal of General Practice, 24(1), 9-18. https://doi.org/10.1080/13814788.2017.1375091. [ Links ]
27. Braun, V., & Clarke, V. (2006) Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2). pp. 77-101. ISSN 1478-0887 Available from: http://eprints.uwe.ac.uk/11735 [ Links ]
28. Dunn, W., Brown, C., & McGuigan, A. (1994). The ecology of human performance: A framework for considering the effect of context. American Journal of Occupational Therapy, 48(7), 595-607. https://doi.org/10.5014/ajot.48.7.595. [ Links ]
29. Whitelaw, E. & Branson, N. (2020). Black Tax: Do graduates face higher remittance responsibilities? Southern Africa Labour and Development Research Unit (SALDRU) University of Cape Town. Available: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved =2ahUKEwiy95KV6Mv7AhVMg1wKHfchCC0QFnoECA4QAQ&url=https%3A%2F%2Fwww.saldru.uct.ac.za%2Fwp-content%2Fuploads%2FBlack-tax.pdf&usg=AOvVaw3fzy1EMgtrN1zvZZGb8xKA. [ Links ]
30. Mtshelwane, D., Nel, J., & Brink, L. (2016). Impression management within the Zulu culture: Exploring tactics in the work context. SA Journal of Industrial Psychology, 42(1), 13 pages. https://doi.org/10.4102/sajip.v42i1.1325 [ Links ]
31. Thwala, J. D., Hermann, C., Edwards, M., Edwards, D. J., & Edwards, S. D. (2020). COVID-19 Coping Experiences in a South African isiZulu speaking sample. International Journal of Innovation, Creativity and Change, 30, 37-49. Available: (PDF) COVID-19 study of Zulu people's coping and resilience in the pandemic (researchgate.net) [ Links ]
32. Hadebe, L. (2010). Zulu masculinity: culture, faith and the constitution in the South African context (Doctoral dissertation). [ Links ]
 Correspondence:
Correspondence:
Ashira Moonsamy
Email: ashira274@gmail.com
Submitted: 15 December 2022
Reviewed: 29 July 2023
Revised: 6 September 2023
Accepted: 7 January 2024
Editor: Pamela Gretschel: https://orcid.org/0000-002-7890-3635
Data availability: Upon reasonable request from corresponding author.
Funding: No funding was received for this study
* Traditional healer through communication with ancestors
** Traditional healer through divination and herbal medicine














