Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Occupational Therapy
versão On-line ISSN 2310-3833
versão impressa ISSN 0038-2337
S. Afr. j. occup. ther. vol.53 no.3 Pretoria Dez. 2023
http://dx.doi.org/10.17159/2310-3833/2023/vol53n3a9
RESEARCH ARTICLE
Exploring the autism diagnostic Odyssey in the Greater Accra Region of Ghana
Joana Nana Serwaa AkrofiI, II; Yvonne Nanaama BrewII, III; Elaine Diandra CarreonI; lana Yadah CorneliusI; Amber Michelle AngelíI
IOccupational Therapy Department, University of Southern California, United States of America; Joana Nana Serwaa Akrofi: https://orcid.org/0000-0002-7797-1759; Elaine Diandra Carreon: https://orcid.org/0000-0002-1709-7123; Amber Michelle Angelí: https://orcid.org/0000-0002-1186-319X
IIOccupational Therapy Department, New York University, United States of America; https://orcid.org/0000-0001-8881-4188
IIIHead of Department, Child Health at Greater Accra Regional Hospital, Ghana
ABSTRACT
INTRODUCTION: Despite the increasing global prevalence of autism spectrum disorders (ASD), there is limited information about ASD in Africa. Existing research on ASD in Africa shows that autistic children are diagnosed relatively late or not at all. The purpose of this study was to understand the barriers to an autism diagnosis and to engage key stakeholders to action plan steps to reduce the barriers.
METHODS: We conducted a participatory, mixed methods study using semi-structured interviews, a survey, photo elicitation, and focus groups with 11 participants (four parents and seven health professionals) in the Greater Accra region of Ghana.
FINDINGS: Neuro-paediatricians in our study reported that it takes, on average, two to six visits over two weeks to two years or more to diagnose a child. Our thematic qualitative analysis yielded three overarching themes, with barriers and facilitators for each: 1) Systemic, 2) Community, and 3) Parent/Family factors that influence the diagnostic process. The action plan of our stakeholder focus group prioritizes community education to dispel myths and encourage autism acceptance within the Ghanaian community.
CONCLUSION: Knowledge about the diagnostic odyssey can help facilitate early diagnosis and intervention.
IMPLICATIONS FOR PRACTICE
This research study confirmed known challenges to the autism diagnostic process. It contributed nuanced insights into the role of culture, the importance of education, and the need for community involvement in improving the diagnostic process, early occupational therapy intervention, and autism acceptance within the community.
Keywords: autism spectrum disorder, participatory research, nominal group technique, barriers and facilitators, early diagnosis and intervention
INTRODUCTION AND LITERATURE REVIEW
Background
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is widely used in making diagnoses, Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by differences in social communication and interaction and restricted and repetitive behaviours that affect an individual's ability to function in school, work, or other areas of life1. The concept of a "Spectrum" was introduced in the DSM-5, which encompassed the autistic disorder, Asperger's disorder, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDD-NOS)2. Recently, there has been a growing debate on the diagnostic criteria of the DSM-5 and the labels it confers3. Some members of the autistic community have also called for autism researchers to adopt non-ableist and inclusive language4.
Despite the increasing global prevalence of autism spectrum disorders (ASD), there is limited information about the prevalence of autism in Africa5,6. Most of the global narrative on autism is centred on data from high-income Western countries7,8.
Existing research on autism in Africa shows that autistic children are diagnosed relatively late compared to autistic children from higher-income countries9, and most of these children have higher levels of need10,11. This may be attributed to delays in the autism 'diagnostic Odyssey' which Lappe et al.12 describe as a "long eventful journey" to an autism diagnosis, characterized by navigating complex educational, social, and medical systems.
De Vries7 speculates that despite the lack of sufficient epidemiological research on autism in Africa, there may be more autistic individuals in Africa compared to many high-income countries based on the population and geographic size of Africa. Thus, autistic individuals in Africa are likely to either be diagnosed much later in life or may not be diagnosed at all. Below, we review possible barriers to this delay or lack of diagnosis in African contexts as reported in the literature.
Absence of Contextually Relevant Diagnostic Tools
According to Kamp-Becker et al.13, the current diagnostic "gold standard" for autism is a lengthy and time-consuming procedure that involves direct observation using the Autism Diagnostic Observation Schedule (ADOS) and an interview with caregivers using the Autism Diagnostic Interview, Revised (ADI-R). In 2017, Franz et al.8 established that no published studies from Sub-Saharan Africa used a combination of developmental history and observational "gold standard" diagnostic instruments such as the ADI-R and the ADOS-2 as typically used in high-income country autism research cohorts8. Ruparelia et al. identified the general lack of appropriate services and inadequate standard of available educational and medical infrastructure, including baseline screening tools and referral systems, as a significant challenge in identifying autistic children in Africa5.
Lack of Professionals with Expertise in Autism
Fusar-Poli et al.14 stress the importance of clinicians' training and experience in assessing individuals who might be on the autism spectrum. However, this poses one of the major barriers to autism diagnosis in many low- and middle-income countries. Studies in Sub-Saharan Africa have found a lack of autism knowledge and awareness levels amongst health and educational professionals15-18. There are relatively few educational professionals who can confidently identify early signs of autism to facilitate the diagnostic process19. Few resources are dedicated to building the capacity of educational professionals to identify individuals with autism compared to health professionals. The path to diagnosis would be expedited by increased awareness and training about autism amongst the public and health professionals5,7-9,20.
Stigma
Another significant barrier to an autism diagnosis is stigma. A study of Hong Kong Chinese families found that the fear of public condemnation of disability caused families to deny an autism diagnosis and socially isolate themselves due to shame and embarrassment21. Cultural beliefs play a prominent role in the stigma associated with autism8,21. There is usually a delay in seeking orthodox medical help for African children with autism because the aetiology of autism is typically attributed to spiritual causes18,22. Perhaps surprisingly, the stigma surrounding autism is not limited to the general populace. According to Bakare and Munir, many African health professionals also subscribe to supernatural causes of autism. Thus, autistic individuals and their families may be negatively impacted by stigmatizing beliefs, which can deter them from seeking help20,23
Aim of Study
There is a dearth of autism health services research in Ghanaian contexts, and more broadly in other African contexts, on how autistic children are identified and diagnosed. To address this gap, this participatory study aimed at understanding the barriers to an autism diagnosis from stakeholders' perspectives and to engage stakeholders to action plan potential steps to improve early and accurate identification.
METHODS
Study Design
We conducted a three-phase, participatory mixed methods study with 11 participants (four parents of autistic children and seven health professionals) to understand the barriers to autism diagnosis in the Greater Accra region of Ghana. We utilized a participatory approach24,25 to engage key stakeholders in identifying barriers and key action steps to ameliorate the identified barriers. We invited one key informant (second author), who is an advocate for neurodiversity and heads a neuro-developmental clinic in a large hospital in the Greater Accra region, to engage with study activities such as recruitment and data collection. Our research question was: How do healthcare professionals and parents/caregivers describe the barriers, facilitators, and pathways to an autism diagnosis in the Greater Accra region of Ghana?
Population and Recruitment
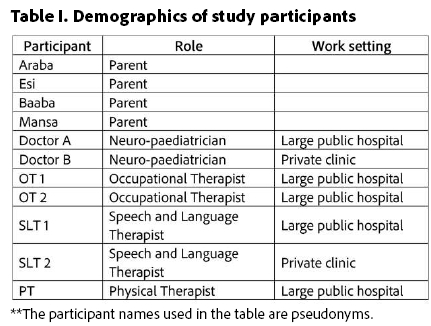
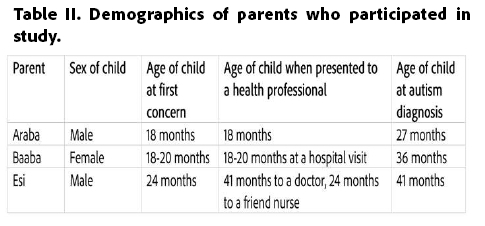
Our key informant helped to purposively recruit and screen parents of autistic children from our study site, a neurodevelopmental unit of a large hospital in Greater Accra, and snowball sampling to recruit healthcare providers involved in identifying and diagnosing autism in the region. All participants were 18 years or older and spoke either English or Twi. Individuals participating in the study had to be parents/primary caregivers of autistic persons who had/were in the process of receiving an autism diagnosis in the Greater Accra region of Ghana or health professionals involved in the identification and/or diagnosis of autism. We recruited a total of 11 participants (four parents of autistic children and seven health professionals). Table I (page 79) below provides demographic information on all the study participants who contributed to all three phases of this research. Table II (page 79) provides more detailed information about the three parents who contributed to phase one (interviews) and their children.
Data Collection and Tools
The study had three phases. During phase one (February to March 2022), the first author conducted semi-structured interviews (see supplemental materials for the interview guide) with three parents of autistic children, asking them to tell the story of how their child came to be diagnosed with autism. Each interview lasted 45-60 minutes and was conducted by the first author via a HIPAA-compliant Zoom platform. At the end of each interview, the first author administered a short survey to the parents to collect quantitative data about the diagnostic Odyssey (e.g., age of early signs and diagnosis, type of early signs). After the interview, we sent each parent a participation stipend.
In phase two, the first author and key informant conducted two focus groups with seven health professionals (two neuro-paediatricians, two occupational therapists, two speech and language therapists, and one physical therapist) via a HIPAA-complaint Zoom platform. At the end of the focus group, the first author asked the health professionals to take photos over the next two weeks of their workspaces, assessment rooms, tools and equipment, and other relevant materials that are useful in the process of diagnosing26 and submit the digital photos to the first author. The audio-recoded interviews were transcribed verbatim (pseudonyms were used for all potentially identifiable names or places); these transcripts, and the first author's notes from the focus groups, were analysed before phase three (see below for details about analysis).
In Phase three, the first author and key informant conducted a final focus group with nine participants (five parents, nine health professionals), using the nominal group technique (NGT)27. During this focus group, the first author presented themain findings from phases one and two and facilitated group discussion to identify and prioritize the major problems and possible solutions for improving early and accurate autism diagnoses in the Greater Accra region of Ghana.
Data Analysis
We used descriptive statistics to analyse the quantitative findings from the parent surveys from phase one.
For the qualitative data (interview transcripts and focus group notes), we used thematic28 and narrative29 analysis, keeping stories intact. Our analysis followed Braun and Clarke's28 thematic analysis, utilizing a 1) theoretical (guided by an a-priori theoretical framework), 2) semantic (focusing on surface-level meanings), and 3) essentialist (theorizing meaning in a straightforward way) design. This approach was chosen based on our research question and study aim, i.e., to understand pragmatic barriers and facilitators to autism diagnosis in this context and to facilitate pragmatic potential solutions to diagnostic barriers. Following the six-step process, the first author manually transcribed the data and read through the data with two other team members to familiarize themselves with the data and jot down initial ideas. The entire team met to generate initial codes based on the a-priori framework and initial readings. The first author and two additional team members coded the transcripts and focus group notes using NVivo; two people coded each document. After all the data was coded, the team met to define and name themes and collaborated on the final report, which was shared with participants during phase 3 for member checking and further discussion. The entire team met throughout the coding process to discuss and clarify codes and collectively analyse the photos from phase two26. Each team member independently reviewed all the photos, after which the entire team met to review the photos together, discuss the significance of each of the photos and select the photos that corroborated the themes from the thematic analysis.
Our a-priori theoretical framework for analysis drew from Bronfenbrenner's Bioecological Theory Revision30 and an adaptation of the US Institute of Medicine's healthcare disparities framework31. Our framework focused on three fundamental levels where barriers or facilitators to health services can occur: system, community, and individual (parent/family)26.
Ethics
The University of Southern California Institutional Review Board (Ethical Clearance Number: UP-21-00992) approved this study. We sought verbal informed consent from all participants before they contributed to each of the study phases. Participants were asked to use pseudonyms in focus groups.
Language
We use identity-first language because it is the preference of many in the autism community32-35
FINDINGS
Diagnostic Odyssey
Two out of the three parents interviewed in this study sought professional medical opinions within the same month of their first concerns, while the third parent waited 17 months to seek a medical professional's opinion. All three parents reported the following traits in their autistic children: did not talk as well as other children, some speech skills were lost, problems with coordination, gross motor skills and/or fine motor skills, sleeping and eating problems, high activity level, and wandering.
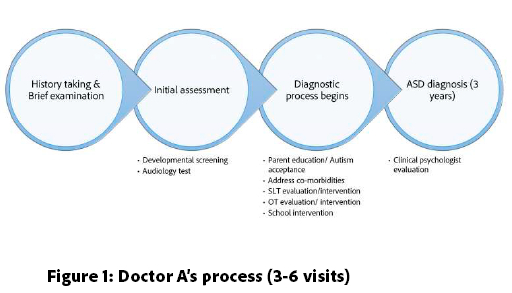
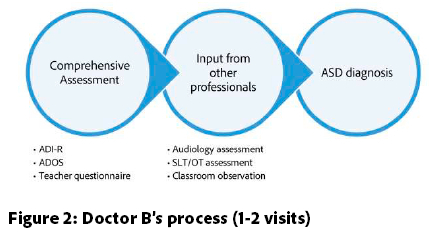
The neuro-paediatricians in this study were the primary health professionals who gave official diagnoses of ASD to patients. They reported coming to the diagnosis with inputs from occupational therapists, speech and language therapists, and clinical psychologists.
"Because we do not have the standardized diagnostic tools, it's very important then to have the input from a lot of professionals before we make a diagnosis, and we make an effort to do that. Our clinic makes an effort to get the input from the occupational therapist, from the speech therapist, and the clinical psychologist if possible." Doctor A, neuro-paediatrician
According to the neuro-paediatricians, it takes an average of two to six visits over a duration of two weeks to two years or more to diagnose (see Figures 1 and 2 below, adjacent). Doctor B, a neuro-pediatrician in a private clinic, described having accessed to standardized diagnostic tools that significantly shorten the diagnostic process.
"so I usually start with an autism diagnostic interview revised schedule which is a detailed interview that helps to diagnose autism and then I do an ADOS, which is an autism diagnostic observation schedule, either from a module 1 to 4 depending on the communication level of the child, and then I usually would add, depending on the unique situation, I would-, I have a teacher interview questionnaire that I put together myself so I either talk to the teacher on the phone, or I give the interview questionnaire to the parents to give to the teacher, and then they fill it and drop it back, and then I add the Gillian Autism Rating Scale which is the GARS, and so I'd usually use these four, so the ADI-R, the ADOS, the GARS, plus the teacher interview before I make up my diagnosis." Doctor B, neuro-paediatrician
Factors Influencing the Diagnostic Odyssey
Our qualitative analysis yielded three overarching themes: 1) Systemic 2) Community and 3) Parent/Family factors influencing the diagnostic Odyssey, each with subthemes on 'Barriers' and 'Facilitators'. Below we describe each theme with illustrative data excerpts.
Theme 1: Systemic Factors Influencing the Diagnostic Odyssey
Systemic Barriers: During the focus group with the health professionals, they noted that there is currently no official policy on diagnosing and managing autistic individuals in Ghana, and this caused the "burden of diagnosing" to weigh on some professionals. This lack of systemic support also caused disruption in service delivery, as some health professionals believed that the government was not doing much to financially compensate and retain professionals who are directly involved in the identification and diagnosis of autistic individuals. One of the neuro-paediatricians also pointed out that the government does not recognize autism as a "multifaceted diagnosis" that requires the resources of multiple sectors, including health, education, and social work, amongst others, which limits the services and supports available to autistic individuals and their families. There was also no governmental provision of autism services throughout the lifespan, and most existing services were tailored to autistic children. Doctor A, a neuro-paediatrician in a large hospital, said:
"Okay so I think one of the main challenges we have is that there's no official policy on the diagnosis and management of children with autism or even other neurodevelopmental issues as well, and so getting the support from the government system is very difficult, so everything depends on the staff who are choosing to make the diagnosis and that doesn't work at all because you need to have support from the government health system, acknowledging that there are children who are having these issues and need to be diagnosed, unlike most other conditions that you just need a clinician or somebody to put a diagnosis on, this a bit more complex so it needs to multidisciplinary, and it's difficult if the system where you work does not recognize the value of the multidisciplinary action need for autism. So, for me, I see that as a very big gap, because when you even make a diagnosis, autism is not just a clinical diagnosis, it's a social diagnosis, it's an educational diagnosis, you know... it comes with a lot of issues, so if you label a child, then what next? Which school is that child going to go to? Which social services are available to support the child and the parents? So, you know, it's difficult. Handling it as a clinical diagnosis when it should rather be a multifaceted diagnosis, you know with a lot of people coming in to provide the support" Doctor A, neuro-paediatrician
Parents confirmed that they were only referred to receive medical services like occupational therapy and speech and language therapy after their children had been formally diagnosed with autism. Additionally, they had to bear the entire financial cost throughout the diagnostic process because autism, as a diagnosis, is not covered under the current National Health Insurance Scheme in Ghana. Araba, the mother of an autistic boy, described her financial ordeal:
"Our neuro-paediatrician put us on some medications, in which I earlier said, his father hardly cooperates; sometimes he'll buy it, sometimes he won't buy... then I have to go and look for funds and buy." Araba, parent
These parents therefore resorted to seeking out additional services and supports like diet modifications, spiritual consultations and interventions from religious leaders and special school enrolments outside the public health service to compensate for the insufficient governmental support. One of the parents, Araba, described how having limited options for services and support led her to reluctantly enrol her child in a special school because she felt pressurized by the recommendation of a therapist:
"So, I went to a speech and hearing centre somebody directed me to... They also did their assessment, and said he needs to be in a special school, that they would monitor him, they would help him with OL. and those things, and I told them that, I want him to be in a regular school so that he would do the therapies in addition,but they were like, looking at his state, he needs to be in that facility...So since they are also professionals, I didn't want to... you know, not listen to their advice, so we had to enrol him at the special school." Araba, parent.
During the focus groups, health professionals also stated that the diagnostic and assessment tools needed for autism were costly and required trainings, making them inaccessible to the average practitioner in Ghana. This led to heavy reliance on multidisciplinary assessments, which were often prolonged due to limited collaboration and coordination amongst professionals. One of the two neuro-paediatricians who participated in the study used the ADI-R and the ADOS for diagnosing (see Figure 2 page 80) in addition to input from other professionals, she mentioned that she had received access to the "gold standard" tools and training when she travelled outside the country, whilst the other neuro-paediatrician stated that relied on mainly on the DSM-V, assessments from multidisciplinary professionals and free screening tools available on the internet including the Childhood Autism Spectrum Test36, Modified Checklist for Autism in Toddlers (M-CHAT)37, Checklist for Autism in Toddlers38, Social Communication Questionnaire39, and the Diagnostic and statistical manual of mental disorders: DSM-540. The assessment tools do not include the gold-standard diagnostic materials and have yet to be validated or contextualized for the Ghanaian population.
Other health professionals described using tools they downloaded off the internet or received from visiting colleagues from the global north. All health professionals acknowledged that they had to modify or adapt the tools they used because they were not entirely culturally sensitive. They explained that the way some of the questions in these assessments are phrased makes them difficult for clients to understand, thereby causing clients to answer inaccurately and skewing the results of the assessments. Also, due to cultural differences in activities, a child who is asked to roleplay a task like bathing a doll in an assessment may not meet all the requirements set by an assessment tool validated in a society where the task is performed differently.
Systems Facilitators
Participants listed neuropediatric specialist care, occupational therapy, speech and language therapy, behaviour therapy, and special education as the services available to autistic individuals. Educational and health professionals with knowledge of autism frequently referred clients to specialists who offered these services. Community health workers who were sometimes the first point of contact for autistic individuals and their families were particularly instrumental in the diagnostic process. Baaba, a parent of an autistic girl, narrated her experience with a public health nurse:
"For [my daughter's] diagnosis, we chanced upon it. She started school quite early, I think about a year and two months, and then here in Ghana, we have public health nurses who visit the various schools to give them their immunization when they are due, so one of the nurses observed her countenance in class, I think that was when she was a year and six months. So, they invited us-, the parents, they wanted to speak to us, so we went to the school, and she told us that she thinks our daughter is autistic..." Baaba, parent
Health professionals from our focus groups also reported referring clients to one another, thus promoting multidisciplinary assessments and interventions. Some of these professionals worked in clinics which had designated multidisciplinary teams that worked with autistic individuals and their families. One of the neuro-paediatricians said:
"So, what helps the process is, if you are in a place...where most of the therapists and specialists are at the same place, that's very easy, so you can have everything done, even if it's not on the same day, it's in the same vicinity and people are knowledgeable to know and direct you as to where to go. So, I think that has been good facilitation, especially for Greater Accra." Doctor A, neuro-paediatrician
The health professionals also pointed out that technological advancement made it easier to schedule assessments virtually and provide increased support for autistic individuals and their families. Doctor B, who is a neuro-paediatrician in a private clinic, said:
"Technology too has been very good for me. So, technology like, me just picking up the phone and calling the teacher, or me asking them to send me a video, so sometimes they'll say, "Oh, he does this thing." And we're doing [a] one hour [session] and he doesn't do it [within the session]. And then I say, "Okay, when you go home and he does it, take a video", and they'll take the video and send it to me on WhatsApp. So, technology has played a good role. I've done a couple of assessments by zoom also, it wasn't my comfort zone, but I've had to do some like that, and I think that's something we could look into, telehealth for diagnosis." Doctor B, neuro-paediatrician
Parents also reported that they had frequent contact with health professionals outside scheduled appointments, and this facilitated the parent-professional relationship and made the diagnostic process easier.
Theme 2: Community Factors Influencing the Diagnostic Odyssey
Community Barriers: Participants expressed that limited knowledge and understanding about autism, including 'early signs,' usually led extended family members, friends, and other members of the community to trivialize the parents' concerns. Esi, mother of an autistic boy, said:
"I realized, no, he's different....and I kept complaining to relatives and friends who were also coming to pick their wards, but then all they said was, "Oh, he's just a kid, he's going to improve with time." And I realized, I asked, "Kwame, how are you?" and he wouldn't say anything. "Kwame, how are you?" he wouldn't say anything... But I realized the other kids would respond, and my friends kept telling me, "Oh, he's just two [years old], with time he'll start talking...you need to be patient," but I was still worried."
Esi, parent
Community members also had the tendency to attribute autistic traits to spiritual causes, making it difficult for families to initially accept diagnoses, often leading to social isolation of autistic individuals and their families. Baaba, who has an autistic daughter, said:
"We informed our family members, but they also didn't have an idea as to what the autism was a bout...So, they quickly related it to witchcraft...and it became a serious issue amongst our family... my husband's side and my side." Baaba, parent
Baaba also described her experience of community spaces that were not sensory-friendly and accommodating for her autistic daughter, leading the family to limit the use of these facilities.
"When we go to Church and there's music, the loudspeaker, [my daughter will] start screaming....when we're in a crowded area... when we sit in a public transport, she hates heat...and when we sit in public transport and then the car stops-, she likes to be in constant motion...So maybe when there's traffic and the car halts, she'll scream till the car moves, but now she's stopped all these things, maybe it's because we're trying to stop taking public transport." Baaba, parent
Parents identified school enrolment as key to assessing their child's milestones and development. However, some participating health professionals pointed out that teachers and other educational professionals were not well equipped to identify early signs in autistic children and would repeatedly misinform parents about their children's school performance. Esi said,
"I think the first teacher I told, she was saying, 'Oh, with time he'll be better... it could be a delayed development,' that's all they were telling me, that with time he'll be better." Esi, parent
Community Facilitators. Participants described a Ghanaian culture of communal engagement and mentioned receiving support and assistance in caregiving roles from family members and friends who understood the autism diagnosis. After receiving an autism diagnosis for her child, Esi described receiving support provided by the teaching staff at her child's mainstream school:
"Because he's slow in getting what is taught in class, after class, the teacher pulls him to her side and then they go over the work all over again, yes, to make sure he understands what is being taught, so I realized an improvement in his academics, yeah."
Esi, parent
Additionally, health professionals noted that there was an increasing trust in orthodox healthcare amongst the Ghanaian community, as individuals were more likely to patronize orthodox health services in addition to traditional medicine or spiritual intervention.
Theme 3: Parent/Family Factors Influencing the Diagnostic Odyssey
Parent/Family barriers: Both parents and health professionals identified denial of theirchild's autism as the major barrier to the diagnostic process. The parents' denial was mainly attributed to a lack of understanding of autism's aetiology and prognosis. Baaba described how she struggled to come to terms with her child's diagnosis and how this resulted in her being slow to follow through with the recommendations and interventions of health professionals'.
"When they said autism, quickly it was Down's Syndrome that came to mind... but after reading and then watching videos [about autism], it was difficult. I told you that we were in the denial stages, until about three, four, we had to accept that this is it... so when she [the doctor] diagnosed her, we were sad, but we knew that we had come to the crossroads and this is what we had to do, so we accepted it... we cried, cried, cried and then we moved on..." Baaba, parent
Other parent/family barriers identified were the absence of spousal support, time and financial constraints.
Parent/Family facilitators: All parents described a personal resolve to gain knowledge on autism and seek professional support once they had come to an understanding. They talked about reading books, seeking out resources, and consulting people with similar experiences. Esi said:
"I decided to read more about it, yes, I decided to read more on the net, to read more about autism..., what I can do to help calm him down, yes, so I read about it, and I realized, looking at the behaviours, I realized it's true he has autism, so I have to just accept it." Esi, parent
All three parents also talk about adopting multiple intervention approaches to address autism including seeking orthodox medical services, diet modifications and spiritual interventions. Araba said,
"As we are praying, I am also doing the therapy, visiting the doctor, making sure he gets his medication, you know." Araba, parent
Baaba talked about how her husband assumed fulltime caregiving responsibility to assist her autistic daughter when there were not getting the needed services.
"So when my husband came, he resigned from his job to look after her at home... so my husband was in the house, taking care of her, training her... how to hold a cup to drink water, if she's thirsy where she'll go and fetch the water, and all those basic things, you know... feeding her properly, training her on how to eat, we had to train her ourselves at home... so that's what we did after we took her from that school. So, for two years, my husband singlehandedly managed her at home." Baaba, parent
Action Steps to Facilitate the Diagnostic Odyssey
During the second focus group with parents and health professionals, participants discussed key findings from phases one and two, came up with action steps, and voted on the order of prioritization of the actions. During the discussion, participants shared that whilst gaining a diagnosis was important, because as a diagnosis does not necessarily lead to funded services or supports, the Ghanaian population may benefit more from communal engagement and education about autism. In other words, early diagnosis may not be a top priority in this context but rather increased awareness and efforts to reduce stigma associated with autism. Because of this stigma, the focus group attendees also shared that some parents and families may prefer to seek private services and supports without a diagnosis as they come to terms with their child's diagnosis.
Based on the information presented and the discussion, the group members were asked to identify key actions to address the barriers and facilitate early and accurate autism identification in Ghana. The group identified four key action points and voted to prioritize them (see Figure 3 adjacent). The group prioritized in descending order, 1) Educating the larger Ghanaian population on autism, 2) Building the capacity of professionals to diagnose, 3) Educating families/stakeholders on caring for autistic individuals, and 4) Collaboration with international organizations to build research capacity in Ghana.
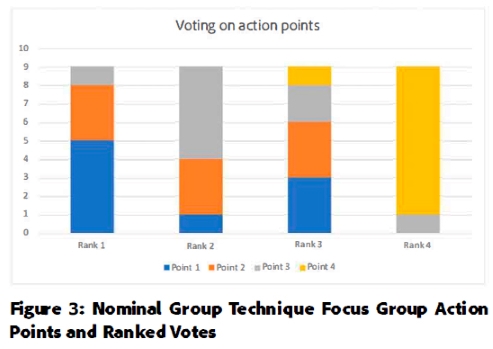
Five participants voted 'Educating the larger Ghanaian population on Autism' as the top priority, five participants voted that 'Building capacity of professionals to diagnose' be prioritized before 'Educating families/stakeholders on caring for autistic individuals, and 8 participants voted 'Collaboration with international organizations to build research capacity in Ghana' as the last priority among the action points raised.
DISCUSSION
In this study, we triangulated multiple data sources to map how autism is identified in the Greater Accra region of Ghana from the perspectives of parents and health professionals, identifying key barriers and facilitators influencing the diagnostic process. This study's findings largely corroborate the existing literature on autism in Sub-Saharan Africa and other developing countries and provide nuanced information on some intersecting factors influencing the autism diagnostic process.
Our study found that there was increasing awareness of autism in Ghana. Despite limitations, health professionals like neuro-paediatricians, medical doctors, occupational therapists, and speech and language therapists contribute to the diagnostic process with the available knowledge and resources. Consistent with other studies, we found that the barriers to the diagnostic process included: assessment and diagnostic tools used in Ghana are not validated for the local population5,8 there are few professionals in the region equipped to identify and diagnose autism15-18, and that there is a significant stigma associated with autism18-22. These challenges are more acute in the Ghanaian setting mainly because of the limited governmental support for autistic individuals and their families. Research has found that autism costs are high in developed and well-resourced countries mainly due to special education and medical care over the lifespan41. While most of these costs are subsidized by governments in developed countries, families and individuals in Ghana must pay out-of-pocket for limited services and support.
Through our qualitative analysis, and in line with previous research, we found that culture plays a role in participants' understanding of and response to an autism diagnosis42-44. Denial amongst parents of autistic individuals45,46 was fuelled by a lack of basic information and the desire to dissociate from the structural stigma47 surrounding autism. In their state of denial, parents isolated and excluded themselves from their communities. This was particularly problematic as participants in our study described a Ghanaian culture that values communal engagement and socialization. Previous studies have found that families of autistic individuals benefit from having strong social networks48,49. It is, therefore, not surprising that the highest-ranking action point from our nominal group technique focus group was community education to dispel myths and encourage autism acceptance within the Ghanaian community.
Our study revealed that it was only after parents understood the diagnosis that they could accept it50,51. Therefore, during the diagnostic process, professionals involved had to educate and counsel families of autistic individuals continuously. Parents also showed resilience and innovation by seeking out information and resources during the 'diagnostic Odyssey'52.
Limitations
Study limitations include a small sample size of parents and health professionals and the absence of the perspectives of educational professionals and autistic individuals. Because we recruited parents from a neurodevelopmental clinic, the ages of diagnoses may not be representative of the general population. Future studies should include larger sample sizes and more diversified stakeholder participation. Researchers should also consider exploring the use of complementary and alternative medicine and therapies associated with autism in countries like Ghana, where there is limited information on the diagnosis and interventions. The strengths of the study include multiple perspectives and data sources, as well as the use of participatory approaches that enabled the identification of potential solutions and priorities that have social validity and are directly applicable to this setting.
CONCLUSION
This mixed methods study describes how autism is identified and diagnosed in the Greater Accra region of Ghana, highlights key barriers and facilitators to the process, and provides stakeholder-identified action steps to improve early and accurate identification, as well as understanding and acceptance of autism, in this context. The barriers and facilitators are grouped under systemic, community, and family factors, showcasing how multilevel intersectional factors contribute to the diagnostic Odyssey. Systemic factors included resources and funding from the government, access, and affordability of services. Community factors included support networks and community education and awareness. Family factors included autism awareness and acceptance, financial status, and help-seeking behaviours. Stakeholders in the study prioritized community education to dispel myths and increase autism acceptance in the Ghanaian community.
Recommendations
Based on the findings of the study, we recommend that there should be a multi-level approach to addressing the barriers to obtaining an autism diagnosis. On the systemic level, there needs to be a multidisciplinary collaboration to develop, adapt and validate autism assessment and diagnostic tools for the local population. Collaborative partnerships between healthcare professionals, educators, and community leaders can go a long way to bridge gaps in understanding and services and create a holistic support system for individuals with autism.
Governmental policies that prioritize research on autism within the Ghanaian context are needed. Efforts should be made to seek funding opportunities to support autism research and improve autism-related initiatives. This could involve funding services, therapies, and interventions to alleviate the financial burden on families and improve access to necessary resources.
At the community level, campaigns and educational initiatives that focus on dispelling misconceptions, emphasizing inclusivity, and encouraging communal support networks for families of autistic individuals should be implemented to reduce the stigma associated with autism and related conditions.
On the individual level, health professionals should play an active role in providing information, guidance, and emotional support to parents as they come to terms with the diagnosis. Efforts should be made to ensure families have easy access to accurate and reliable information about autism. This can empower parents to seek resources, understand their child's needs, and make informed decisions.
Authors' contributions
Joana Akrofi, Yvonne Brew, and Amber Angelí conceptualised and planned the study, drafted and edited the manuscript. All authors contributed to the data collection and analysis and critically reviewed and approved the final manuscript.
Conflicts of interest
The authors declare no conflicts of interest
Acknowledgements
We would like to acknowledge the DREAmS Lab at the Mrs. T. H. Chan Division of Occupational Science and Occupational Therapy at the University of Southern California for the invaluable feedback and support during this research project. We would also like to acknowledge our participants for their time, contribution, and feedback.
REFERENCES
1. American Psychiatric Association D, Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. Vol. 5. American psychiatric association Washington, DC; 2013. doi: https://doi.org/10.1176/appi.books.9780890425596 [ Links ]
2. Hodges H, Fealko C, Soares Ν. Autism spectrum disorder: Definition, epidemiology, causes, and clinical evaluation. Vol. 9, Translational Pediatrics. AME Publishing Company; 2020. p. S55-65. doi: https://doi.org/10.21037/tp.2019.0909 [ Links ]
3. Masi A, DeMayo MM, Glozier N, Guastella AJ. An Overview of Autism Spectrum Disorder, Heterogeneity and Treatment Options. Vol. 33, Neuroscience Bulletin. Science Press; 2017. p. 183-93. doi: https://doi.org/10.1007/s12264-017-0100-y [ Links ]
4. Bottema-Beutel K, Kapp SK, Lester JN, Sasson NJ, Hand BN. Avoiding Ableist Language: Suggestions for Autism Researchers. Vol. 3, Autism in Adulthood. Mary Ann Liebert Inc.; 2021. p. 18-29. doi: https://doi.org/10.1089/aut.2020.0014 [ Links ]
5. Ruparelia K, Abubakar A, Badoe E, Bakare M, Visser Κ, Chugani DC, et al. Autism Spectrum Disorders in Africa: Current Challenges in Identification, Assessment, and Treatment. Journal of Child Neurology. 2016; 31(8): 1018-26. doi: https://doi.org/10.1177/0883073816635748 [ Links ]
6. Abubakar A, Ssewanyana D, Newton CR. A systematic review of research on autism spectrum disorders in sub-Saharan Africa. Behavioural Neurology. 2016.1-14. doi: http://dx.doi.org/10.1155/2016/3501910 [ Links ]
7. De Vries PJ. Thinking globally to meet local needs: Autism spectrum disorders in Africa and other low-resource environments. Current Opinion in Neurology. 2016; 29(2): 130-6. doi: https://doi.org/10.1097/wco.0000000000000297 [ Links ]
8. Franz L, Chambers N, von Isenburg M, de Vries PJ. Autism spectrum disorder in sub-saharan africa: A comprehensive scoping review. Autism Research. 2017; 10(5): 723-49. doi: https://doi.org/10.1002/aur.1766 [ Links ]
9. Bakare MO, Munir KM. Autism spectrum disorders (ASD) in Africa: A perspective. African Journal of Psychiatry. 2011; 14(3): 208-10. doi: https://doi.org/10.4314/ajpsy.v14i33 [ Links ]
10. Belhadj A, Mrad R, Halayem M. Etude clinique et paraclinique d'une population d'enfants autistes Tunisiens. A propos de 63 cas [A clinic and a paraclinic study of Tunisian population of children with autism. About 63 cases]. Tunis Med. 2006;84(12):763-7 [ Links ]
11. Mankoski RE, Collins M, Ndosi NK, Mgalla EH, Sarwatt V V, Folstein SE. Etiologies of autism in a case-series from Tanzania. Journal of Autism and Developmental Disorders. 2006; 36(8): 1039-51. doi: https://doi.org/10.1007/s10803-006-0143-9 [ Links ]
12. Lappé M, Lau L, Dudovitz RN, Nelson BB, Karp EA, Kuo AA. The diagnostic Odyssey of autism spectrum disorder. Pediatrics. 2018,141: S272-9. doi: https://doi.org/10.1542/peds.2016-4300c [ Links ]
13. Kamp-Becker I, Tauscher J, Wolff N, Küpper C, Poustka L, Roepke S, et al. Is the Combination of ADOS and ADI-R Necessary to Classify ASD? Rethinking the "Gold Standard" in Diagnosing ASD. Frontiers in Psychiatry. 2021;12:727308-727308. doi: https://doi.org/10.3389/fpsyt.2021.727308 [ Links ]
14. Fusar-Poli L, Brondino N, Rocchetti M, Panisi C, Provenzani U, Damiani S, et al. Diagnosing ASD in Adults Without ID: Accuracy of the ADOS-2 and the ADI-R. Journal of Autism Developmental Disorders. 2017; 47(11): 3370-9. doi: https://doi.org/10.1007/s10803-017-3258-2 [ Links ]
15. Gossou KM, Koudema A, Kpoffon K, Adjiwanou V. Knowledge about Autism among Graduate Students in Togo. Journal of Autism and Developmental Disorders. 2021; 52(2): 877- 89. doi: https://doi.org/10.1007/s10803-021-04972-3 [ Links ]
16. Igwe MN, Ahanotu AC, Bakare MO, Achor JU, Igwe C. Assessment of knowledge about childhood autism among paediatric and psychiatric nurses in Ebonyi state, Nigeria. Child and Adolescent Psychiatry and Mental Health. 2011; 5(1):1-8. doi: https://doi.org/10.1186/1753-2000-5-1 [ Links ]
17. Sampson WG, Sandra AE. Comparative Study on Knowledge About Autism Spectrum Disorder Among Paediatric and Psychiatric Nurses in Public Hospitals in Kumasi, Ghana. Clinical Practice & Epidemiology in Mental Health. 2018;14(1):99-108. doi: https://doi.org/10.2174/1745017901814010099 [ Links ]
18. Bakare MO, Munir KM. Excess of non-verbal cases of autism spectrum disorders presenting to orthodox clinical practice in Africa - a trend possibly resulting from late diagnosis and intervention. South African Journal of Psychiatry. 2011;17(4):118-20. doi: https://doi.org/10.4102/sajpsychiatry.v17i4.295 [ Links ]
19. Taresh S, Ahmad NA, Roslan S, Ma'rof AM, Zaid S. Pre-school teachers' knowledge, belief, identification skills, and self-efficacy in identifying autism spectrum disorder (ASD): A conceptual framework to identify children with ASD. Brain Sciences. 2020; 10(3): 165. doi: https://doi.org/10.3390/brainsci10030165 [ Links ]
20. Wannenburg Ν, van Niekerk R. Early diagnosis and intervention for autism spectrum disorder in Africa: Insights from a case study. African Health Sciences. 2018; 18(1): 137-46. doi: https://doi.org/10.4314/ahs.v18i1.18 [ Links ]
21. Tait Κ, Fung F, Hu A, Sweller N, Wang W. Understanding Hong Kong Chinese Families' Experiences of an Autism/ASD Diagnosis. Journal of Autism and Developmental Disorders. 2016; 46(4): 1164-83. doi: https://doi.org/10.1007/s10803-015-2650-z [ Links ]
22. Gona JK, Newton CR, Rimba K, Mapenzi R, Kihara M, van de Vijver F, et al. Parents' and professionals' perceptions on causes and treatment options for Autism Spectrum Disorders (ASD) in a multicultural context on the Kenyan coast. PLOS ONE. 2015;10(8):e0132729-e0132729. doi: https://doi.org/10.1371/journal.pone.0132729 [ Links ]
23. Oti-Boadi M, Dankyi E, Kwakye-Nuako CO. Stigma and Forgiveness in Ghanaian Mothers of Children with Autism Spectrum Disorders (ASD). Journal of Autism and Developmental Disorders. 2020; 50(4):1391-400. doi: https://doi.org/10.1007/s10803-020-04366-x [ Links ]
24. Taylor RR, Suarez-Balcazar Y, Forsyth K, Kielhofner G. Participatory Research Approaches. In: Kielhofner's Research in Occupational Therapy. Jason LA, Keys CB, Suarez-Balcazar Y, Davis Ml, Editors. Philadelphia: F.A. Davis Company; 2017 p. 424-36. [ Links ]
25. Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R, et al. Community-based participatory research: A capacity-building approach for policy advocacy aimed at eliminating health disparities. American Journal of Public Health. 2010;100(11):2094-102. doi: https://doi.org/10.2105/ajph.2009.170506 [ Links ]
26. van Auken PM, Frisvoll SJ, Stewart SI. Visualising community: Using participant-driven photo-elicitation for research and application. Local Environment. 2010;15(4):373-88. doi: https://doi.org/10.1080/13549831003677670 [ Links ]
27.McMillan SS, Kelly F, Sav A, Kendall E, King MA, Whitty JA, et al. Using the Nominal Group Technique: how to analyse across multiple groups. Health Services and Outcomes Research Methodology. 2014;14(3):92-108. doi: https://doi.org/10.1007/s10742-014-0121-1 [ Links ]
28. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006; 3(2):77-101. doi: https://doi.org/10.1191/1478088706qp063oa [ Links ]
29. Cortazzi M. Narrative Analysis. Narrative Analysis. Newbury Park, CA: Sage Publications; 2014.1-162 p. (Qualitative research methods; v. 30). [ Links ]
30. Vélez-Agosto NM, Soto-Crespo JG, Vizcarrondo-Oppenheimer M, Vega-Molina S, García Coll C. Bronfenbrenner's Bioecological Theory Revision: Moving Culture From the Macro Into the Micro. Perspectives on Psychological Science. 2017; 12(5):900-10. doi: https://doi.org/10.1177/1745691617704397 [ Links ]
31. Institute of Medicine. Assessing Potential Sources of Racial and Ethnic Disparities in Care: Patient- and System-Level Factors. In: Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. National Academies Press; 2003. p. 125-59. [ Links ]
32. Kenny L, Hattersley C, Molins B, Buckley C, Povey C, Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism. 2016 May 1;20(4):442-62. doi: https://doi.org/10.1177/1362361317727125 [ Links ]
33. Gernsbacher MA, Raimond AR, Stevenson JL, Boston JS, Harp Β. Do puzzle pieces and autism puzzle piece logos evoke negative associations? Autism. 2018 Feb 1;22(2):118-25. [ Links ]
34. Dunn DS, Andrews EE. Person-first and identity-first language: Developing psychologists' cultural competence using disability language. American Psychologist. 2015 Apr 1;70(3):255-64. doi: https://doi.org/10.1037/a0038636 [ Links ]
35.Botha M, Hanion J, Williams GL. Does Language Matter? Identity-First Versus Person-First Language Use in Autism Research: A Response to Vivanti. Vol. 53, Journal of Autism and Developmental Disorders. Springer; 2023. p. 870-8. doi: https://doi.org/10.1007/s10803-020-04858-w [ Links ]
36.Scott FJ, Baron-Cohen S, Bolton P, Brayne C. The CAST (Childhood Asperger Syndrome Test): preliminary development of a UK screen for mainstream primary-school-age children, doi: https://doi.org/10.1177/1362361302006001003 [ Links ]
37.Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. Journal of autism and developmental disorders. 2001;31:131-44. doi: https://doi.Org/10.1023/a:1010738829569 [ Links ]
38.Baron-Cohen S, Wheelwright S, Cox A, Baird G, Charman Τ, Swettenham J, Drew A, Doehring P. Early identification of autism by the Checklist for Autism in Toddlers (CHAT). Journal of the royal society of medicine. 2000 Oct;93(10):521-5. doi: https://doi.org/10.1177/014107680009301007 [ Links ]
39.Rutter M. Social communication questionnaire. 2003. [ Links ]
40.American Psychiatric Association DS, American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association; 2013 May 22. doi: https://doi.org/10.1176/appi.books.9780890425596 [ Links ]
41.Buescher AVS, Cidav Z, Knapp M, Mandell DS. Costs of Autism Spectrum Disorders in the United Kingdom and the United States. JAMA Pediatrics. 2014;168(8):721-8. doi: https://doi.org/10.1001/jamapediatrics.2014.210 [ Links ]
42.Ennis-Cole D, Durodoye BA, Harris HL. The Impact of Culture on Autism Diagnosis and Treatment. The Family Journal. 2018; 21(3): 279-87 doi: https://doi.org/10.1177/1066480713476834 [ Links ]
43.Ravindran N, Myers BJ. Cultural Influences on Perceptions of Health, Illness, and Disability: A Review and Focus on Autism. Journal of Child and Family Studies. 2011; 21(2):311-9. doi: https://doi.org/10.1007/s10826-011-9477-9 [ Links ]
44.Neely-Barnes SL, Hall HR, Roberts RJ, Graff JC. Parenting a Child With an Autism Spectrum Disorder: Public Perceptions and Parental Conceptualizations. Journal of Family Social Work. 2011; 14(3):208-25. doi: https://doi.org/10.1080/10522158.2011.571539 [ Links ]
45.Dababnah S, Parish SL. "At a moment, you could collapse": Raising children with autism in the West Bank. Children and Youth Services Review. 2013; 35(10):1670-8. doi: https://doi.Org/10.1016/j.childyouth.2013.07007 [ Links ]
46.Altiere MJ, von Kluge S. Searching for acceptance: Challenges encountered while raising a child with autism. Journal of Intellectual & Developmental Disability. 2009; 34(2):142-52. doi: https://doi.org/10.1080/13668250902845202 [ Links ]
47.Hatzenbuehler ML. Structural Stigma and Health Inequalities: Research Evidence and Implications for Psychological Science. American Psychologist. 2016;71(8):742. doi: https://doi.org/10.1037/amp0000068 [ Links ]
48.LaRoche G, Des Rivières-Pigeon C. From Close Connections to Feeling Misunderstood: How Parents of Children with Autism Spectrum Disorder Perceive Support from Family Members and Friends. Canadian Journal of Family and Youth / Le Journal Canadien de Famille et de la Jeunesse. 2022;14(1):1-22. doi: https://doi.org/10.29173/cjfy29758 [ Links ]
49.Ekas Ν V, Lickenbrock DM, Whitman TL. Optimism, social support, and well-being in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2010; 40(10): 1274-84 doi: https://doi.org/10.1007/s10803-010-0986-y [ Links ]
50.Smith-Young J, Chafe R, Audas R. "Managing the Wait": Parents' Experiences in Accessing Diagnostic and Treatment Services for Children and Adolescents Diagnosed With Autism Spectrum Disorder. Health Services Insights. 2020;13:117863292090214 doi: https://doi.org/10.1177/1178632920902141 [ Links ]
51.Jacobs D, Steyaert J, Dierickx K, Hens K. Implications of an Autism Spectrum Disorder Diagnosis: An Interview Study of How Physicians Experience the Diagnosis in a Young Child. Journal of Clinical Medicine. 2018; 7(10): 348. doi: https://doi.org/10.3390/jcm7100348 [ Links ]
52.Abbey G. Help-Seeking Behaviour of Parents of Children with Autism Spectrum Disorder in Accra, Ghana. 2018 (Doctoral dissertation, University of Ghana). [ Links ]
 Correspondence:
Correspondence:
Joana Akrofi
ja4547@nyu.edu
Submitted: 26 October 2022
Reviewed: 23 June 2023
Revised: 23 August 2023
Accepted: 27 August 2023
Editor: Blanche Pretorius; https://orcid.org/0000-0002-3543-0743
Data availability: From the corresponding author
Funding: This study was funded by the University of Southern California, Mrs. T. H. Chan Division of Occupational Science and Occupational Therapy and the USC Chan DREAmS Lab














