Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Occupational Therapy
versão On-line ISSN 2310-3833
versão impressa ISSN 0038-2337
S. Afr. j. occup. ther. vol.53 no.3 Pretoria Dez. 2023
http://dx.doi.org/10.17159/2310-3833/2023/vol53n3a4
RESEARCH ARTICLE
Paediatric hand function assessment practices of occupational therapists in South Africa
Marieta VisserI; Mariette NelII; Chanelle BornmanIII, V; Tessa KellermanIII, V; Zoe MullerIV; Carien OosthuizenIII, V
IOccupational Therapy Department, University of the Free State, Bloemfontein, South Africa. https://orcid.org/0000-0002-8825-4683
IIDepartment of Biostatistics, University of the Free State, Bloemfontein, South Africa; https://orcid.org/0000-0002-3889-0438
IIIPrivate occupational therapy practice, South Africa; Chanelle Bornman: https://orcid.org/0000-0001-8074-5683; Tessa Kellerman: https://orcid.org/0000-0002-7381-5783; Carien Oosthuizen: https://orcid.org/0000-0003-4895-8907
IVOccupational therapist in a senior educator post at Khanyisa Developmental Centre, South Africa; https://orcid.org/0000-0001-8320-5033
VUndergraduate student at the University of the Free State, Bloemfontein, South Africa, at the time of the study
ABSTRACT
INTRODUCTION: South African occupational therapists' assessment practices of children's hand function are unknown, although the treatment thereof is an integral part of the paediatric scope of practice and clientele. Hand function assessment frameworks and instruments are available, but a lack of contextually relevant, comprehensive standardised instruments was identified. The study aimed to investigate occupational therapists' current paediatric hand function assessment practices and their preferences towards future practice.
METHODS: A quantitative, cross-sectional study design using convenient and snowball sampling was employed. An EvaSys© survey system, custom-developed online questionnaire, was used to collect information.
RESULTS: In total, 194 HPCSA-registered occupational therapists participated. All the participants currently rely on informal observations. Although not exclusively designed for hand function, standardised developmental tests were often used. Limited familiarity with and use of the available published hand function assessment instrument was reported. Future assessment preferences supported a standardised, comprehensive hand function assessment instrument for different age groups and paediatric conditions.
CONCLUSION: This study provides baseline evidence of current and preferred paediatric hand funct ion assessment practices used by occupational therapists. The need for training to use the available published instruments was highlighted. Recommendations towards the refinement of existing or the development of a standardised, contextually relevant instrument for paediatric practice in South Africa are offered.
IMPLICATIONS FOR PRACTICE:
This article offers a deeper understanding of available paediatric hand function assessment frameworks, assessment instruments, and practices of occupational therapists. It provides an outline of existing methods therapist use and offers clear directives for how the South African OT would prefer to assess hand function in children. Emphasis is placed on the need for a contextually relevant instrument and future research in refining existing instruments or developing a new instrument is proposed. Additionally, practitioners provided practical suggestions to guide the development of a contextually relevant instrument for potential use in future instrument development research.
Keywords: paediatric practice, hand function assessment frameworks, psychometric properties, assessment methods, contextually relevant instrument, fine-motor skills
INTRODUCTION
Children use their hands as instruments to experience life, express themselves and explore their world1. The term hand skills is used interchangeably with terms such as dexterity, fine-motor skills and hand function2. Hand skills can be defined as "skills of the hand that are needed to attain and manipulate objects" to interact with the environment and people2,230. Hand function is crucial for engagement in early childhood occupations of learning, doing and thinking1. Limitations in hand function may cause children to experience difficulties in fine-motor activities, for example, grasping small objects, writing, fastening buttons and using an electronic device2. Without hand function skills, children are unable to meet the demands of daily life2. Children with several different health conditions can present with various hand function difficulties, causing restriction in activity participation and impairment in quality of life. Thus, children are often referred to occupational therapy, where precise assessment and effective intervention are crucial to address these impairments3
In South Africa, research indicates that only 30.4 % of South African pre-schoolers' fine motor are on par for age4. Fine motor skills have been identified as one of the predictive components of children's performance in the preschool years4. With South African occupational therapists frequently treating young children, it may be important to look at their paediatric hand function assessment practices to ultimately address these difficulties in South Africa children5. Assessment practices refer to the methods of assessment, type of assessments used, the preference, reasons for use/non-use, the frequency of use, the particular context of practice used in and the population being evaluated6-7.
It is widely acknowledged that assessment is a core professional skill considered an essential first step in the occupational therapy process8. Assessment involves determining the factors that support or hinder "health, well-being and participation" through determining the client's current and potential problems8:24. Sound assessment instruments are valuable in the decision-making process, guiding intervention planning and augmenting evidence-based practice8-10. The use of valid and reliable assessment instruments may assist the occupational therapist to obtain trustworthy information to justify and guide intervention, can be used to evaluate the effectiveness of occupational therapy service and guide clinicians to discover ways of advancing knowledge and practices9-13.
Moreover, another aspect to consider in the field of assessment practice is the rapidly growing fields of instrument development across disciplines14. This has led to the availability of a wide range of emerging assessment instruments, approaches, and methods of great value to the profession, considering the broad scope of services provided by occupational therapists14-21. At the same time, occupational therapists need to be thoughtful in their choice of instruments to obtain relevant, valid and reliable information to ensure the best assessment practices13,15.
The type of instruments used to assess children's hand function has been described in the literature1-3,10,22,23. Moreover, the method of assessment seems to be dependent on the availability of instruments. Therefore, it seems that hand function assessments often occur in combination with other more general developmental assessments or are administered as part of informal observations. Nevertheless, despite all the available paediatric hand function instruments described in the literature, it appears that there is no one assessment that (i) includes assessment items to cover all hand function aspects20; (ii) displays the characteristics of a systematic and comprehensive instrument development process as previously described12,13,15; (iii) provide evidence of the essential psychometric properties10,24; and (iv) have been standardised as norm-referenced instruments for a wide age range of children in South Africa25.
However, little is known about the assessment practices of South African occupational therapists pertaining to paediatric hand function26,27. In 2021, South African occupational therapists in-hand manipulation (IHM) assessment practices have been described with regard to current and preferred assessment methodsS Only one international study and no national studies could be located regarding the paediatric hand function assessment instruments selected and used by occupational therapists28. Therefore, several questions arose regarding South African occupational therapists' current paediatric hand function assessment practices and their preferences towards future assessment practices.
LITERATURE REVIEW
Considerations when selecting an assessment instrument
The wide range of assessment instruments available, occupational therapists need to be thoughtful when choosing an assessment instrument. From the literature, cognisance of specific considerations is pivotal during any critical evaluation process of potential assessment instruments (to be purchased and used in clinical practice or for research). Foundational to these considerations are (i) instrument evaluation framework/s; (ii) instrument development theory and process; (iii) evidence of the psychometric properties; and (iv) contextual relevance of assessment instruments. Each consideration is briefly described below.
Firstly, occupational therapists should critically review available instruments for appropriateness and performance against an evaluation framework, such as those described by Law12 or Rudman and Hannah13.These frameworks describe five broad categories: clinical utility, standardisation, purpose, psychometric properties and patient's perspective12,13.
Secondly, instruments should be reviewed to determine whether a systematic theory-based process for instrument development was followed and recorded to substantiate the instrument's scientific soundness11,14,29,30. These include the classic test, item response, and multidimensional scaling theories. Many currently available instruments used in occupational therapy have been developed with the classic test theory16,35.
A third consideration is the evidence of evaluated psychometric properties of the instrument11,29. The nature of the psychometric evaluations depends on the type of assessment instrument but generally include reliability (i.e., inter-rater, intra-rater, test-retest and internal consistency), validity (i.e., face, content, construct, criterion, concurrent and predictive validity), and responsiveness (i.e., longitudinal validity)10,11,13,15,16,29-32 .
Lastly, a critical continuous consideration is whether the instrument has evidence of social, cultural, religious, gender and contextual relevance2,33,
Components of a comprehensive paediatric hand function assessment
Concerning all the different aspects of hand function that can be assessed, three models/frameworks that can serve as conceptual guides toward comprehensive assessment of paediatric hand function have been proposed.
They include the following:(i) the Hand Function Evaluation Model which proposes three levels of assessment: sensorimotor components, developmental progress and function of the hand34; (ii) the Functional Repertoire of The Hand Model is based on four key components, namely personal constraints, task parameters, hand roles and hand actions3; and (iii) the Children's Hand Skills Framework recommends a comprehensive hand repertoire that can be divided into six distinct categories applicable to the assessment process22. The first two categories do not include contact with objects, namely manual gesture and body contact hand skills. The object-related categories include hand skills involving arm-hand use, hand function involving adaptive skills of hand use (such as grasping and in-hand manipulation), hand skills involving bimanual use, and general quality of hand function (dexterity, coordination speed)22.
The available paediatric hand function assessment instruments
Although this article does not aim to provide a literature review on available hand function assessment instruments, a comprehensive selection and charting of instruments were needed to inform the development of the questionnaire for this study. Therefore, a literature search was conducted in May 2020 to identify all the paediatric hand function assessment instruments that are currently available.
The following databases were searched: Academic Search Ultimate, Africa-Wide Information, Cl NAHL with full text, eBook collection (EBSCOhost), Health Source: Nursing/Academic Edition, Kovsiecat, KovsieScholar, MEDLINE with full text, Open Dissertations and MEDLINE.
The search was limited to articles written in English that were published from 2010-2022. The search terms used were [instrument] and child*. From these sources, a broad overview of published paediatric hand function assessment instruments was identified, arranged and tabulated according to categories of observational assessment, pathology-specific assessments, pegboard tests and questionnaires in Table I (page 24-25). The study did not include the psychometric properties of each instrument. The following types of instruments were excluded from the table: (i) in-hand manipulation instruments (assessing a small part of hand function); as a recently published scoping review on existing in-hand manipulation instruments is already available35; (ii) instruments that assess single occupational performance components (i.e., muscle strength and coordination), for example, the Two-Arm Coordination Tests (TACT)36 and the Cup-Task and Box-Task test, which is a functional hand and upper extremity muscle-strength test37; (iii) paediatric developmental tests such as the Bayley scales of infant and toddler development38 designed to measure more comprehensive aspects such as motor, cognitive, sensory and socio-emotional and language; (iv) instruments that can be used to assess children's participation, specifically in life situations requiring hand use, such as the Children's Assessment of Participation and Enjoyment/Preferences for Activities of Children (CAPE/PAC)39; (v) instruments currently under development (but not referred to in any publications) such as the GRAB40 and the Pizza Putty Test47; and (vi) questionnaires that assess hand function developed for adult hand injuries but not adapted for children, for example, the DASH (disabilities of the arm, shoulder and hand) questionnaire42 and the Michigan Hand Outcomes Questionnaire43.
Ostensibly, a wide variety of children's hand function assessment instruments is available, but when charting these instruments in different categories and according to specific criteria, the opposite becomes evident. After certain instruments were excluded (as motivated above), Table I (page 24-25) was compiled and demonstrated that only two observational assessment instruments, seven pathology-specific, three pegboards and four questionnaires, were considered. Only one published clinical instrument covers several (although not all) hand function components, with a broad age range that is not pathology-specific. However, not one instrument standardised for the South African population is available. Therefore, a need for a contextually relevant paediatric hand function assessment instrument for occupational therapists is evident. However, before refining available instruments or developing a new instrument for children in South Africa, it is important to understand therapists' paediatric hand function assessment practices. Therefore, this study aimed to investigate occupational therapists' current paediatric hand function assessment practices and their preferences towards future practice.
METHODS
Study design
A quantitative, cross-sectional research approach was employed for this study60.
Population and sampling
In this study, the population represented registered South African paediatric occupational therapists. During the study, 5 682 occupational therapists were registered with the Health Professions Council of South Africa (HPCSA). However, it was not evident who was retired, not practicing, or living in other countries. The HPCSA could also not disclose the exact number of occupational therapists practicing within the paediatric field. Therefore, convenience sampling was used to reach the population via email, social media (i.e., Facebook, lnstagram and WhatsApp) and the Occupational Therapy Association of South Africa (OTASA) platform61. To reach even more occupational therapists, snowball sampling was also used62,63.
The inclusion was regulated based on the following criteria: (i) participants should be occupational therapists registered with the HPCSA; (ii) participants should have worked with children between the ages of 1 to 12 years directly or indirectly (through training of students or research in this field); (iii) participants should have practiced within the last five years; (iv) participants should have practiced in South Africa for more than two months; (v) participants should have assessed hand function in children; and (vi) participants should have access to the internet and email.
Measuring instruments
An online questionnaire developed from the literature and expert consultation was developed and posted on the EvaSys© survey system. Literature considered throughout the questionnaire development covered (i) available standardised and non-standardised paediatric hand function assessment instruments (c.f. Table I, page 24-25); (ii) instrument development theory; (iii) instrument evaluation theory; (iv) literature on psychometric properties, and (v) assessment approaches. The questionnaire consisted of closed and open-ended questions to allow participants to raise their opinions.
The first section of the questionnaire was directed at the demographic information of the participants and the second section at the paediatric client profile of the participants. The third section related to the current methods that participants used to assess hand function in children. The final section focused on the preferred assessment practices of participants and their preferences towards a potentially suitable hand function assessment tool to assess children in South Africa.
Pilot study
The questionnaire was piloted to determine face- and content validity. Aspects also considered were whether the EvaSys© survey link was accessible on different devices and overall technical efficiency64,65. Four occupational therapists from different practice sectors participated. Feedback was used to refine the questionnaire's format, wording and content. The results of the pilot study were not included in the final study since only a few small changes to some assessment instruments' names in the questionnaire were required.
Data collection procedure
The researchers used the EvaSys© survey system to distribute the questionnaire and collect data. Participants were able to access and complete the questionnaire online. The study advertisement and the specific EvaSys© survey link to the questionnaire were distributed via the OTASA electronic database and social media platforms. The link was available for three weeks and two reminder emails were distributed. To promote a higher response rate, an optional continuing professional development (CPD) activity was available for completion at the end of the questionnaire. The researchers scored the accredited CPD activity, and an electronic certificate providing three CPD units was distributed.
Validity was maintained by excluding ineligible participants, preventing selection bias and using consistent scoring procedures during data analysis. Reliability was ensured by maintaining the same questions throughout data collection; using an electronic survey to guarantee internal consistency; and maintaining confidentiality to ensure objectivity during data analysis.
Data analysis
The EvaSys© survey system automatically captured the responses and extracted the data to compile a Microsoft Excel spreadsheet. Descriptive statistics, namely frequencies and percentages for categorical data and medians and percentiles for numerical data, were calculated.
Ethical consideration
Approval for this study was obtained from the Health Sciences Research Ethics Committee (HSREC) of the University of the Free State in Bloemfontein, South Africa (reference number: UFS-HSD2020/0127/2104). OTASA granted written permission to use their platform. All the participants were provided with an information letter explaining the purpose of the study and were informed that completing the questionnaire implied voluntary agreement to participate. Participants could withdraw at any given time without being disadvantaged. Participation was not anonymous, but information of a personal nature was kept confidential.
RESULTS
A total of 203 questionnaires were completed, with 194 participants eligible for inclusion in this study. The calculated response rate for the 3 860 OTASA members was 3.8%, although a response rate of 5% was achieved, similar to other South African online survey studies66.
Demographic profile
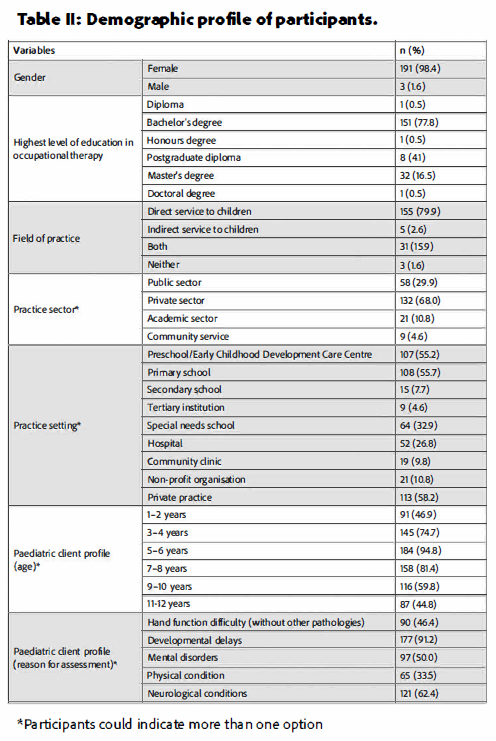
The participants' age ranged from 23 to 63 years, with a median of 29 years, of which most were female (n=191; 98.5%). Years of practice ranged from 0.25 to 40 years, with a median of 6 years. As shown in Table II (below), the highest level of education was a Bachelor's degree (n=151; 77.8%), while 32 (16.5%) participants had a Master's degree. Most participants provided direct occupational therapy services to children (n=155; 79.9%), and the majority worked in the private sector (n=132; 68.0%), followed by 58 (29.9%) participants who worked in the public sector. Regarding the client profile, most participants (n=184; 94.8%) assessed the age group 5-6 years with developmental delays (n=177; 91.2%) and neurological conditions (n=121; 62.4%). Additionally, children who suffered a head injury, brachial plexus injury, congenital condition/syndrome, or any post-injury condition (e.g., fractures and burns) were assessed.
Current informal assessment methods used by participants to assess children's hand function
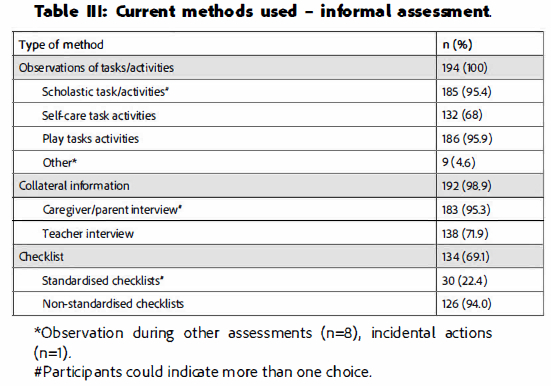
Regarding informal assessment methods used, all (n=194; 100%) participants used observation of tasks and/or activities, followed by collateral information (n=192; 99.0%) and checklists (n=134; 69.1%). The main source of collecting collateral information was via parent/caregiver consultations (n=183; 95.3%), as shown in Table III (below).
Current assessment instruments used by participants to assess children's hand function
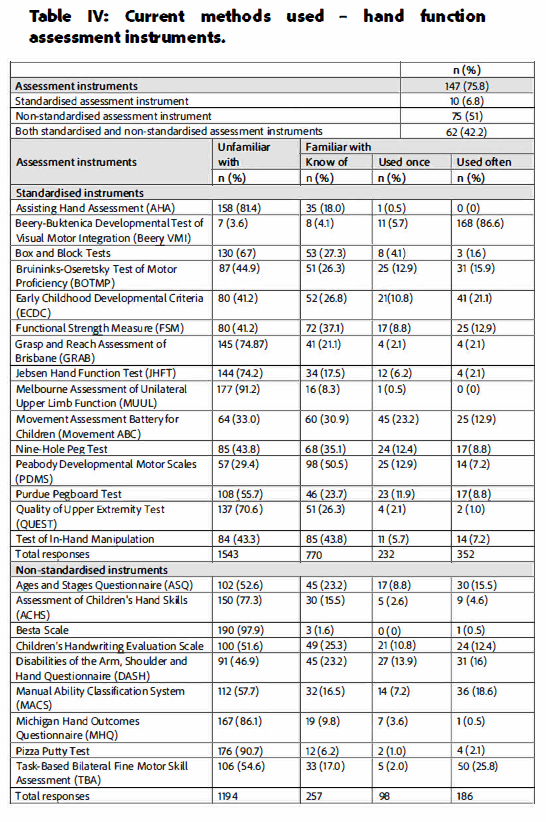
Table IV (page 28) illustrates that most participants used assessment instruments (n=147; 75.8%). The standardised test most often used was the Beery-Buktenica Developmental Test of Visual Motor Integration (Beery VMl)67 (n=168; 86.6%), followed by the Early Childhood Developmental Criteria (ECDC)68 (n=41; 21,1%), Bruininks-Oseretsky Test of Motor Proficiency (BOTMP) 69 (n=31;16%) and Movement Assessment Battery for Children (Movement ABC) 69 (n=25; 12.9%). Thus, participants were more familiar with developmental tests than any other hand function specific instruments Participants were least familiar with the Melbourne Assessment of Unilateral Upper Limb Function (MUUL)47 (177; 91.2%), followed by the Assisting Hand Assessment (AHA)46 (158; 81.4%) and the Grasp and Reach Assessment of Brisbane (GRAB)40 (n=145; 74.8%).
It was noted that participants reported that they know of instruments, for example, the Peabody Developmental Motor Scales (PDM S)71 (n=98;50.5%), the test of in-hand manipulation (n=85; 43.8%), and the Functional Strength Measure (FSM)18 (n=72; 37.1%), but did not often use it. Regarding the non-standardised tests, participants mostly used the Task-Based Bilateral Fine Motor Skill Assessment (TBA)45 (n=50; 25.77%) followed by the Manual Ability Classification System (MACS)49 (n=36; 18.6%). They were least familiar with the Besta Scale 50(n=190; 97.9%), Pizza Putty Tests41 (n=176; 90.7%) and Michigan Hand Outcomes Questionnaire (MHQ)43 (n=167; 86.1%).
Participants indicated that they knew of the Children's Handwriting Evaluation Scale (n=49; 25.3%), the Ages and Stages Questionnaire (ASQ)72 (n=45; 23.2%) and (Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH)73 (n=45; 23.2%).
Qualities of assessment instruments frequently used by participants to assess hand function of children
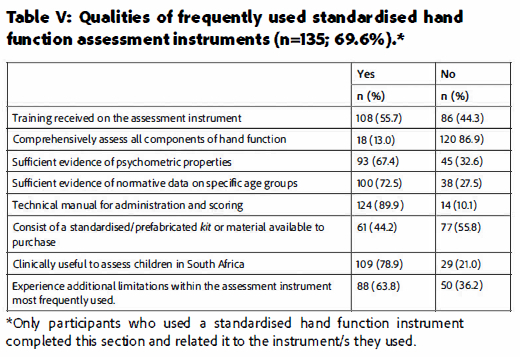
Most participants (69.6%) indicated that they frequently used standardised assessment instruments to assess the hand function of children. The tests frequently used are as follows. The majority (n=100; 72.5%) of participants based their answers on the Beery VMI test (n=81; 60.0%), followed by BOTMP (n=16; 11.9%), the Movement ABC (n=12; 6.7%) and the DASH (n=8; 5.9%). Other tests used by the remaining 38 (275%) participants included the Nine-Hole Peg Test (n=4 (2.9%), Purdue Pegboard test (n=5; 13.2%), MACS (n=6; 13.2%), Jebsen Hand Function Test (n=2; 5.3%), and the ECDC (n=3; 7.9%).
Table V (page 28) shows that most participants (86.9%) did not consider the assessment instrument they used to comprehensively assess all components of hand function. Overall, participants considered the hand function assessment instruments that they used at the time of the study to have sufficient evidence of psychometric properties (n=93; 67.4%) and normative data on specific age groups (n=100; 72.5%), and also noted the availability of technical manuals for administration and scoring (n=124; 89.9%).
However, comments indicated that certain instruments were not regarded as valid and reliable for hand function specifically but more in terms of developmental tests (e.g., Beery VMI). Some instruments (n=77; 55.8%) did not include a standardised or prefabricated kit or material available to purchase. Additionally, some participants reported on the expensiveness of test material that often has to be procured from overseas. Other limitations experienced included the lack of in-depth hand function results, too lengthy administration times, difficult portability, and lack of cultural, age and language relevance.
Most participants (n=109; 78.9%) considered the instrument they used to be clinically useful to assess children in South Africa. However, they were aware that these assessment instruments had not been standardised on South African children and were thus not ideal to use.
Practical aspects of current and preferred hand function assessments
The median time participants spent on the administration of assessments was 30 minutes, whereas the preferred median was21 minutes, as shown in Table VI (page 29). Both the current and preferred median scoring time was 15 minutes. Regarding the materials used by participants, most used toys, objects, and/or activities within their clinical setting (n=175; 902%), while 81 (41.8%) also used the assessment instruments' specified materials. One participant preferred to use tasks within the context of functional activities, such as buttoning a shirt or handling utensils. Another participant preferred using materials that would not have to be replaced or run out.
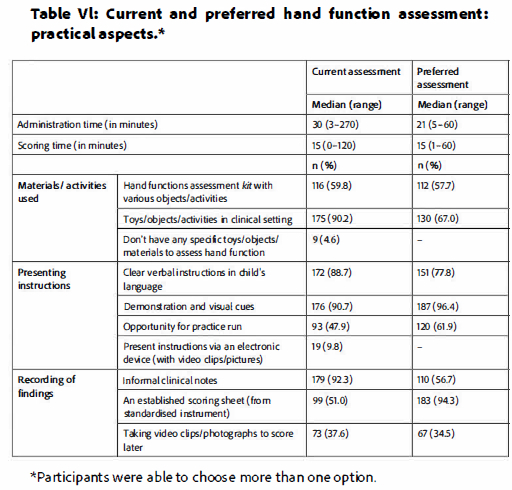
When presenting instructions to the child, most participants indicated using dear verbal instructions in the child's language (n=172; 88.7%) and demonstration and visual cues (n=176; 90.7%). However, less than half (n=93; 47.9%) indicated providing an opportunity for a practice run. Only 19 participants (9.8%) indicated using electronic devices (e.g., tablets) with video clips and/or pictures to present instructions.
Most participants (n=179; 92.3%) indicated recording their findings on informal clinical notes at the time of the study. Nevertheless, 110 participants (56.7%) preferred informal clinical notes. While only 99 (51.0%) used an established scoring sheet at the time of the study. 183 (94.3%) indicated they prefer established scoring sheets to record their assessment findings. Overall, approximately one third of the participants (n=67; 34.5%) preferred video recording the assessment to be scored afterwards.
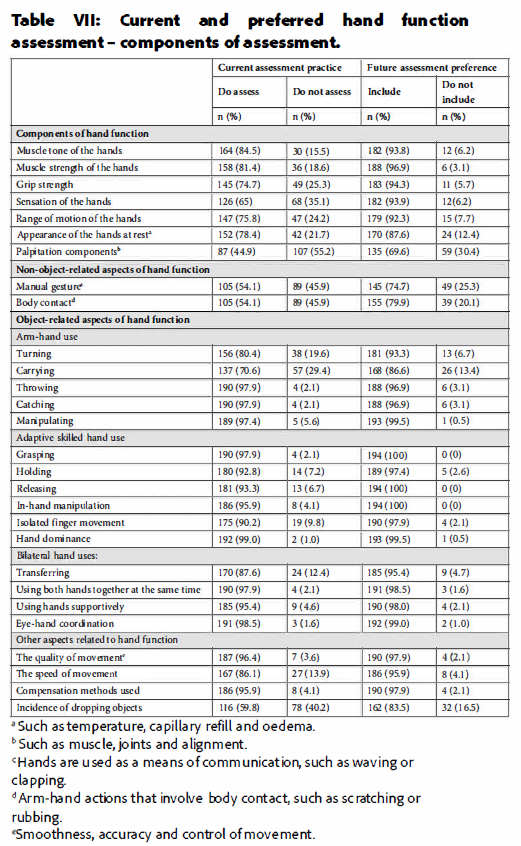
Current assessment practice and future assessment preference of different components of hand function assessment
As shown in Table VII (adjacent), over 80% of the participants indicated a strong preference for incorporating most aspects listed in Table VI (above) into any future assessment instrument. Least preferred but still of importance were components of palpitation (n=135; 69.6%), manual gesture (n=145; 74.7%) and body contact (n=155; 79.9%). All participants (n=194; 100%) indicated that a future instrument should include grasping, releasing and in-hand manipulation. Almost all the participants indicated that they currently assessed object-related aspects of hand function and would prefer these aspects to be included in a future assessment instrument. A small number of participants indicated that although they did not currently assess specific components of hand function (e.g., grip strength and muscle tone of the hands), they would prefer its inclusion in a future assessment instrument.
Contextual aspects of an assessment
Overall, participants considered the instruments that they used to be relevant for children's age (n=182; 93.8%), gender (n=182; 93.8%), cultural (n=148; 76.3%) and socio-economic background (n=137; 70.6%), and also acknowledged its importance in future instruments.
Preferences for a future hand function assessment instrument
Table VIII (page 30) summarises that most participants (n=134; 69.1%) preferred an instrument to be available in the public domain (open access) with specifications of the equipment/materials required for self-assembly, over a standardised format. A very small number of participants (n=3; 1.5%) commented that they would like a combination of both formats to make it affordable in all clinical settings.
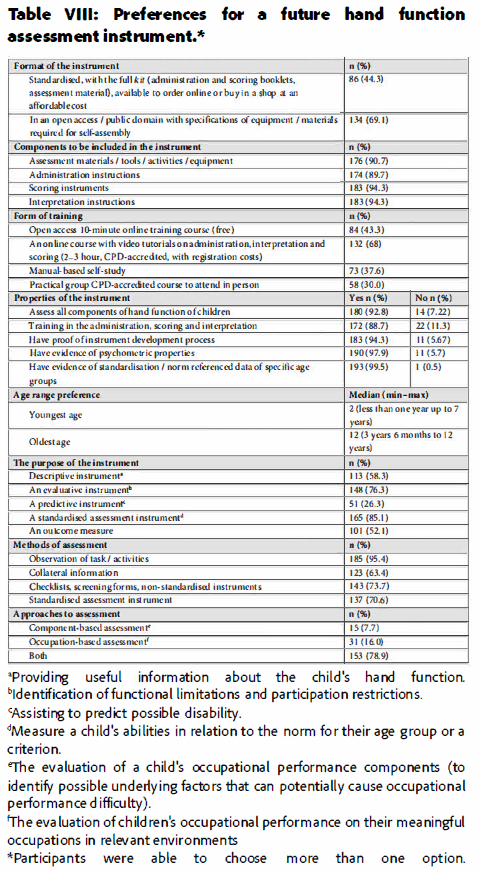
The most preferred form of training was indicated to be online courses with video tutorials. Participants considered it important for future instruments to display evidence of all the properties listed in Table VIII (page 30). Participants preferred a future hand function assessment instrument to accommodate an age range of 2-12 years. A standardised assessment instrument with age-related norms was the most preferred characteristic of a future instrument (n=165; 85.1%).
Observation of tasks and activities was the recommended assessment method (n=185; 95.4%). Both component- and occupational-based assessment approaches were preferred by most participants (n=153; 78.9%).
A total of 163 participants (84.0%) stated they did not know of any standardised hand function assessment instrument for South African children. The few who indicated otherwise (n=10; 9.8%), proposed the ECDC as a hand function assessment instrument standardised on South African children. Almost all the participants (n=189; 97.4%) agreed that there is a need for a paediatric hand function assessment instrument designed for and standardised on South African children.
DISCUSSION
Current hand function assessment practices
The study revealed that in current practice, most participants used developmental or visual perception assessment instruments rather than hand function-specific instruments. The limited use of hand function-specific instruments might be attributed to a lack of knowledge, diminished satisfaction with and appreciation of available instruments and limited time27,74. Although some standardised developmental instruments used are not hand function-specific and those that are, do not comprehensively assess all components of hand function. However, developmental assessments such as the Beery VMI or ECDC do provide the opportunity to observe hand function components.
According to our findings, the standardised test most often used was the Beery VMI. Previous studies also reported the Beery VMI as one of the most popular tests used in paediatric practice in South Africa75 and internationally6,7. Although the Beery VMI is not standardised for our population, evidence has revealed that South African children's performance on the Beery VMI compared well to the American normative sample76. But, the VMI can only be used to observe a child's hand function (i.e., pencil grip) of the VMI, and was not developed as a comprehensive hand function assessment.
All participants indicated using observation of tasks/activities as part of their assessments, which could be expected since it is considered one of occupational therapists' core skills77, developed from their unique assessment outlook and subjective experience6. However, observation alone creates the risk of subjectivity8,75. Therefore, using it in conjunction with a standardised hand function assessment, if available, is preferable to obtain objective and evidence-based results8,78.
Most participants agreed that the currently used instruments fail to comprehensively assess all components of hand function. Consequently, participants frequently found it necessary to supplement their assessment with informal observations. No single comprehensive assessment standardised on South African children that also provides psychometric evidence has been described before. Comprehensive evaluation is crucial to determine the child's ability to participate in daily occupations and to understand participation limitations that ensure evidence-based practice2,9,10.
More participants reported that they were unfamiliar with most of the standardised and non-standardised tests than those familiar with them. This could be due to clinicians not routinely using standardised tests due to time constraints, difficulties in assessing young children and the complexity of the tests66. Similar findings have been reported by Visser et al.25, who described that the measuring instruments currently used by occupational therapists in South Africa, were often either standardised on foreign populations, not affordable or unavailable for the specific outcome. These tests lack clinical utility, which could be described as the usefulness (appropriateness, accessibility, practicability and acceptability) of an assessment in clinical practice12,79.
Participants mostly assessed the 5-6 year age group and developmental delays or neurological conditions were the most common reasons for assessment (Table I, page 24-25), aligning with findings by Brown et al.6 and Feder et al7.
Although the prevalence of developmental delays in South African children has not been well documented, the worldwide prevalence is 2-5%80. The prescribed assessment materials to be used for the developmental age of the children create a discrepancy for children with physical and neurological disorders, and profound intellectual barriers (functional versus chronological age).This could indicate the need for a standardised test appropriate for the age group of 5-6 years, accommodating developmental delays and neurological conditions.
It became evident in this study that many of the participants want to use inclusive instruments but most instruments either do not contain a standardised or prefabricated kit or materials, are not available for purchase, are often too expensive, and are limited by therapists' practice setting and financial resources. Hence, these tests do not meet the requirements of clinical utility in terms of accessibility79. Moreover, according to instrument evaluation literature by Rudman and Hannah13 and Law12, assessment materials need to meet standardised specifications. In contrast with paper-based visual perception instruments (e.g., Beery VMI), hand function is a construct that implies the use of material/objects (in a prefabricated kit) to observe certain components of hand function.
When designing an assessment instrument, it is important to consider the child's context, which influences their activity choices8,13. Some participants in the private sector indicated that tests were usually culturally and socio-economically compatible with the population of children they assessed. However, participants commented that although some materials were neutral, e.g., crayons, they often adapted the materials and toys according to the child's age, gender, cultural and socio-economic background. It is important to incorporate terms that are compatible across different cultural groups33.
Preferred hand function assessment practices
More than 80% of the participants demonstrated a high preference for most aspects presented in Table VII (page 29), namely object-related and non-object-related components, to be included in a future assessment instrument. Components of palpitation, manual gesture and body contact were least preferred but are still important to include in developing a future assessment instrument, as proposed in the literature19. Participants strongly preferred grasping, releasing and in-hand manipulation to be part of the components assessed in a future instrument. Bieber et al. recommended developing a new comprehensive tool that includes the different aspects of manual function19.
Most participants preferred an affordable instrument, available in the public domain, with a standard format for equipment and materials. Availability of an assessment instrument can be limited by cost, language or format13,27,74,79. Participants preferred a standardised assessment instrument designed to measure or describe a child's abilities at one moment in time in relation to norms or criteria, corroborating the findings reported by Diamantis74 and Janse van Rensburg et al.75
Most hand therapists agree that occupation-based assessment and intervention are ideal, although it is not always the most commonly used form of therapy due to time constraints74,81. A clinically applicable instrument is one that assesses both underlying components of hand function as well as the use of hands in activities13,81.
Participants reported currently spending more time administering a test than they would prefer. Scoring times remained consistent for both current and preferred practices. According to the literature, administration time and training are crucial factors that may affect occupational therapists' choice of assessment6,74-75. Occupational therapists in South Africa often face high caseloads, quick referral turnover and medical aid-related time limits. Consequently, time constraints are a common reason for therapists not to use an occupation-based approach to assessment81.
Age appropriateness, relevance to all genders, cultures and socio-economic backgrounds were important, as supported by Rudman and Hannah13, who recommended that therapists should select instruments appropriate for their clients' population and settings. These are therefore important factors to consider within the diverse South African population.
Consequently, there is a need for a test that provides in-depth hand function assessment results, has a short administration time, is easily transportable and is culture, age and language relevant and clinically useful.
Strengths and limitations of the study
In terms of strengths, this study made use of a comprehensively developed questionnaire through (i) performance of an in-depth literature search of all relevant assessment instruments (c.f. Table I, page 24-25); (ii) researchers attending an EvaSys© training session to ensure accuracy and user-friendliness of the questionnaire; and (iii) confirming face validity of the questionnaire by means of the pilot study.
Another strength of this study was the use of an online questionnaire accessible on different social media platforms through snowball sampling, which allowed more participants across South Africa to be reached. An optional CPD activity increased the response rate of the questionnaire. Although it was a quantitative study, the participants had the opportunity to add comments that enriched the data.
A limitation of this study was, firstly, the sample size, preventing the generalisability of the findings to all South African occupational therapists. Secondly, completing the questionnaire was time-consuming, which could have influenced the response rate negatively. Finally, the test-retest reliability of the questionnaire was not determined in a second-round questionnaire.
Recommendations
Based on the results and conclusions drawn from this study, the authors made the following recommendations with regard to future research: (i) a scoping review of the literature to provide a broad overview and critical evaluation of available paediatric hand function assessment instruments with evidence on the validity/reliability; and (ii) developing a new, or refining an existing, hand function assessment instrument according to a systematic instrument development process.
Recommendations for clinical practice include the following: (i) training in the use of the available instruments; (ii) critical evaluation of assessment instruments; and (iii) using standardised instruments to ensure objective results and evidence-based practice.
We recommend that more attention should be paid to under- and postgraduate training in the assessment and treatment of hand function.
CONCLUSION
This study was the first of its kind, documenting the unique voice of South African occupational therapists on their current and preferred assessment practices to evaluate children's hand function. Results highlighted that although a variety of instruments may be available when mapped out and compared, the lack of a standardised, comprehensive hand function assessment instrument with evidence of established psychometric properties is evident.
Hence, the preference for an assessment instrument standardised on South African children is irrefutable. Furthermore, practical direction for developing a future instrument or refinement of a potential assessment instrument is proposed. Recommendations for the continuation of research towards the development of a standardised assessment instrument are supported to guide intervention planning and in due time, improve children's engagement in all their daily activities.
Author contributions
Marieta Visser identified the research topic and supervised the study. Marieta Visser, Zoe Muller, Tessa Kellerman, Carien Oosthuizen, Chanelle Bornman and Mariette Nel formulated the research aims and objectives, and contributed to the conception and design of the study. Zoe Muller, Tessa Kellerman, Carien Oosthuizen and Chanelle Bornman collected the data. Mariette Visser analysed the data. Marieta Visser, Zoe Muller, Tessa Kellerman, Carien Oosthuizen. and Chanelle Bornman interpreted the data, and prepared the first draft of the manuscript. The authors finalised and approved the final version of the manuscript.
Conflicts of interest
The authors have no conflict of interest to declare
Acknowledgements
All the occupational therapists who participated in the study, and Dr. Daleen Struwig, medical writer/editor, Faculty of Health Sciences, University of the Free State, for technical and editorial editing of the manuscript
REFERENCES
1. Fowler N, Nicol A. Functional and biomechanical assessment of the normal and rheumatoid hand. Clinical Biomechanics. 2001;16(8):660-666. http://dx.doi.org/10.1016/s0268-0033(01)00057-2 [ Links ]
2. Case-Smith J, O'Brien JC. Occupational Therapy for Children and Adolescents 7th Ed. St. Louis, MO: Elsevier Mosby; 2015. [ Links ]
3. Kimmerle M, Mainwaring L, Borenstein M. The functional repertoire of the hand and its application to assessment. American Journal of Occupational Therapy. 2003;57(5):489-498. https://doi.org/10.5014/ajot575.489 [ Links ]
4. Giese S, Dawes A, Tredoux C, Mattes F, Bridgman G, van der Berg S, SchenkJ, Kotze J. Thrive by Five Index Report Revised August 2022, Innovation Edge, Cape Town. 2022. ww.thrivebyfive.co.za. [ Links ]
5. Kruger A, Strauss M, Visser M. Assessment of in-hand manipulation by occupational therapists in paediatric practices in South Africa. South African Journal of Occupational Therapy. 2021;51(2):11-20. http://dx.doi.org/10.17159/2310-3833/2021/vol52n2a3 [ Links ]
6. Brown GT, Rodger S, Brown A, Roever C. A profile of Canadian pediatric occupational therapy practice. Occupational Therapy In Health Care. 2007;21(4):39-69. https://doi.org/10.1080/J003v21n04_03 [ Links ]
7. Feder K, Majnemer A, Synnes A. Handwriting: current trends in occupational therapy practice. Canadian Journal Of Occupational Therapy. 2000;67(3):197-204. https://doi.org/10.1177/000841740006700313 [ Links ]
8. American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and Process. 4th Ed. American Journal of Occupational Therapy. 2020;74 (Suppl_2) :7412410010p1-7412410010p87. https://doi.org/10.5014/ajot.2020.74S2001 [ Links ]
9. Law M, Baum CM, Dunn W. Measuring Occupational Performance: Supporting Best Practices in Occupational Therapy. Thorofare, NJ: Slack Incorporated; 2017. [ Links ]
10. van de Ven-Stevens LA, Munneke M, Turwee CB, Spauwen PH, van der Linde H. Clinimetric properties of instruments to assess activities in patients with hand injury: a systematic review of the literature. Archives of Physical Medicine and Rehabilitation. 2009;90(1):151-169. http://dx.doi.org/10.1016/j.apmr.2008.06.024 [ Links ]
11. Kielhofner G. Research in Occupational Therapy: Methods of Inquiry for Enhancing Practice. Philadelphia, PA: FA Davis Company; 2006. [ Links ]
12. Law M. Measurement in occupational therapy: scientific criteria for evaluation. Canadian Journal of Occupational Therapy. 1987;54(3):133-138. http://dx.doi.org/10.1177/000841748705400308 [ Links ]
13. Rudman D, Hannah S. An instrument evaluation framework: description and application to assessments of hand function. Journal of Hand Therapy. 1998;11(4): 266-277. http://dx.doi.org/10.1016/S0894-1130(98)80023-9 [ Links ]
14. DeVellis RF. Scale Development: Theory and Applications. 4th Ed. Los Angeles, CA: Sage Publications, Inc.; 2017. [ Links ]
15. Grove SK. Burns N, Gray JR. The Practice of Nursing Research: Appraisal, Synthesis and Generation of Evidence. 7th Ed. St Louis, MO: Elsevier; 2012. [ Links ]
16. Pett MA, Lackey NR, Sullivan JJ. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Research. Thousand Oaks, CA: Sage Publications, Inc.; 2003. [ Links ]
17. Chien CW, Brown T, McDonald R. Examining content validity and reliability of the Assessment of Children's Hand Skills (ACHS): a preliminary study. American Journal of Occupational Therapy. 2010;64(5):756-767. http://doi.org/10.5014/ajot.2010.08158 [ Links ]
18. Artssen WFM, Ferguson GD, Smits-Engelsman BCM. Reliability and structural and construct validity of the functional strength measurement in children aged 4to 10 years. Physical Therapy. 2016;96(6):888-897. http://dx.doi.org/10.2522/ptj.20140018 [ Links ]
19. Bieber E, Smits-Engelsman, BCM, Sgandurra G, Cioni G, Feys H, Guzzetta A, Klingels K. Manual function outcome measures in children with developmental coordination disorder (DCD): systematic review. Research in Developmental Disabilities. 2016;55:114-131. https://doi.org/10.1016/j.ridd.2016.03.009 [ Links ]
20. Law M, Cooper BA., Strong S, Stewart D, Rigby P, Letts L. The person-environment-occupation model: a transactive approach to occupational performance. Canadian Journal of Occupational Therapy. 1996;63(1):9-23. https://doi.org/10.1177/000841749606300103 [ Links ]
21. Polatajko HJ, Davis JA, Hobson SJG, Landry JE, Mandich A, Street SL, Whippey E, Yee S. Meeting the responsibility that comes with the privilege: introducing a taxonomic code for understanding occupation. Canadian Journal of Occupational Therapy. 2004;71(5):261-264. http://dx.doi.org/10.1177/000841740407100503 [ Links ]
22. Chien CW, Brown T, McDonald R. A framework of children's hand skills for assessment and intervention. Child: Care, Health and Development. 2009;35(6):873-884. https://doi.org/10.1111/j.1365-2214.2009.01002.x [ Links ]
23. Backman C, Gibson SCD, Parsons J. Assessment of hand function: the relationship between pegboard dexterity and applied dexterity. Canadian Journal of Occupational Therapy. 1992;59(4):208-213. https://doi.org/10.1177/000841749205900406 [ Links ]
24. Schoneveld K, Wittink H, Takken T. Clinimetric evaluation of measurement tools used in hand therapy to assess activity and participation. Journal of Hand Therapy. 2009;22(3):221-236. https://doi.org/10.1016/j.jht.2008.11.005 [ Links ]
25. Visser M, Du Plessis C, Jacobs S, Joubert A., Muller M, Smith B, Van Soest R. In-hand manipulation in children 6 and 7 years of age: a follow-up study. South African Journal of Occupational Therapy. 2016;46(2):52-58. http://dx.doi.org/10.17159/2310-3833/2016/v46n2a9 [ Links ]
26. Van der Merwe J, Smit N, Vlok B. A survey to investigate how South African occupational therapists in private practice are assessing and treating poor handwriting in foundation phase learners: Part I - Demographics and assessment practices. South African Journal of Occupational Therapy. 2011;41(3):3-11. Available from: http://www.scielo.org.za/scielo.php?script=sci_rttext&pid=S2310-38332011000300003 (accessed 25 January 2023). [ Links ]
27. De Klerk S, Buchanan H, Pretorius B. Occupational therapy hand assessment practices: cause for concern? South African Journal of Occupational Therapy. 2015;45(2):43-50. https://doi.org/10.17159/2310-3833/2015/v45n2a7 [ Links ]
28. Grice KO. The use of occupation-based assessments and intervention in the hand therapy setting: a survey. Journal of Hand Therapy. 2015;28(3),300-306. http://dx.doi.org/10.1016/j.jht.2015.01.005 [ Links ]
29. Benson J, Clark F. A guide for instrument development and validation. American Journal of Occupational Therapy.1982;36(12):789-800. http://dx.doi.org/10.5014/ajot.36.12.789 [ Links ]
30. Hambleton RK, Jones RW. Comparison of classical test theory and item response theory and their applications to test development. Educational Measurement: Issues and Practice. 1993;12(3):38- 47. https://doi.org/10.1097/01.mlr.0000245426.10853.30 [ Links ]
31. Gray J, Grove S, Sutherland S. Burns and Grove's The Practice of Nursing Research: Appraisal, Synthesis, and Generation of Evidence. St. Louis, MO: Saunders, 2016. [ Links ]
32. Jerosch-Herold C. An evidence-based approach to choosing outcome measures: a checklist for the critical appraisal of validity, reliability and responsiveness studies. British Journal of Occupational Therapy. 2005;68(8):347-353. https://doi.org/10.1177/030802260506800803 [ Links ]
33. Chien CW, Brown T, McDonald R. Cross-cultural validity of a naturalistic observational assessment of children's hand skills: a study using Rasch analysis. Journal of Rehabilitation Medicine. 2011;43(7):631-637. https://dx.doi.or/10.2340/16501977-0827 [ Links ]
34. Tsang WPC. Hand Function Evaluation for Preschool Children With and Without Physical Dysfunction. Doctoral Thesis. Hong Kong: The Chinese University of Hong Kong; 1999. Available at: https://www.proquest.com/docview/304574525/fulltextPDF/6B9989B6D0D54DFDPQ/1?accountid=17207 (accessed 25 January 2023). [ Links ]
35. Kruger A, Strauss M, Visser M. In-hand manipulation assessment instruments for children: a scoping review. British Journal of Occupational Therapy. 2022;85(2):83-98. http://dx.doi.org/10.1177/03080226211037859 [ Links ]
36. Riquelme I, Arnould C, Hatem SM, Bleyenheuft Y. The two-arm coordination test: maturation of bimanual coordination in typically developing children and deficits in children with unilateral cerebral palsy. Developmental Neurorehabilitation, 2019;22(5):312-320. http://dx.doi.org/10.1080/17518423.2018.1498552 [ Links ]
37. Dekkers KJFM, Smeets RJEM, Janssen-Potten YJM, Gordon AM, Speth L AWM, Rameckers EAA. Psychometric evaluation of 2 new upper extremity functional strength tests in children with cerebral palsy. Physical Therapy. 2019;99(8):1107-1115. http://dx.doi.org/10.1093/ptj/pzz019 [ Links ]
38. Nguyen KVH. Adaptation of the Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-Ill) for Vietnam: A Preliminary Study. Doctoral thesis. New York, NY: St. John's University ProQuest Dissertations Publishing; 2017, ProQuest Number 10609746. Available at: https://www.proquest.com/docview/1904873381?pq-origsite=gscholar&fromopenview=true (accessed 15 February 2023). [ Links ]
39. Ullenhag A, Almqvist L, Granlund M, Krumlinde-Sundholm L. Cultural validity of the Children's Assessment of Participation and Enjoyment/Preferences for Activities of Children (CAPE/PAC). Scandinavian Journal of Occupational Therapy. 2012;19(5):428-438. http://dx.doi.org/10.3109/11038128.2011.631218 [ Links ]
40. Krumlinde-Sundholm L., Ek L, Eliasson AC. What assessments evaluate use of hands in infants? A literature review. Developmental Medicine and Child Neurology. 2015;57(2):37-41. https://doi.org/10.1111/dmcn.12684 [ Links ]
41. Leese S, Hackett J, Aslam R, Mills L, Jester A, Southwood TR. A91: The development and initial evaluation of a standardised play based hand assessment tool for use in children and adolescents: the PizzaPutty Test. Arthritis and Rheumatology. 2014;66(S3):S126. https://doi.org/10.1002/art.38508 [ Links ]
42. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). American Journal of Industrial Medicine. 1996;29(6):602-608. http://dx.doi.org/10.1002/(SICl)1097-0274(199606)29:6%3C602::AlD-AJIM4%3E3.0.CO;2-L [ Links ]
43. Chung K.C., Pillsbury MS., Walters MR., Hayward RA., Arbor A. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. Journal of Hand Surgery. 1998;23(4):575-587. http://dx.doi.org/10.1016/S0363-5023(98)80042-7 [ Links ]
44. Chien CW, Brown T, McDonald, R. Examining construct validity of a new naturalistic observational assessment of hand skills for preschool- and school-age children. 2012;59(2):108-120, https://doi.org/10.1111/j.1440-1630.2012.00997.x [ Links ]
45. Ratcliffe I, Franzsen D, Bischof F. Development of a task-based bilateral fine motor skill assessment for grade 0 children in South Africa. South African Journal of Occupational Therapy, 2013;43(1):9-15. Available at: https://sajot.org.za/index.php/sajot/issue/view/13 (accessed 25 January 2023). [ Links ]
46. Krumlinde-Sundholm L, Holmefur M, Kottorp A, Eliasson A. The Assisting Hand Assessment: current evidence of validity, reliability, and responsiveness to change. Developmental Medicine and Child Neurology. 2007;49(4):259-264. https://doi.org/10.1111/j.1469-8749.2007.00259.x [ Links ]
47. Randall M, Imms C, Carey L M, PallantJ F. Rasch analysis of The Melbourne Assessment of Unilateral Upper Limb Function. Developmental Medicine and Child Neurology. 2014;56(7):665-672. https://doi.org/10.1111/dmcn.12391 [ Links ]
48. DeMatteo C, Law M, Russell D, Pollock N, Rosenbaum P, Walter S. QUEST Manual: Quality of Upper Extremity Skills Test Manual. Hamilton, Ontario: McMaster University; 1992. Available at https://slpemad.files.wordpress.com/2015/06/1992_quest_manual.pdf (accessed 25 January 2023). [ Links ]
49. Eliasson A, Ullenhag A, Wahlström U, Krumlinde-Sundholm SL. Mini-MACS: development of the Manual Ability Classification System for children younger than 4 years of age with signs of cerebral palsy. Developmental Medicine and Child Neurology. 2017;59(1):72-78. https://doi.org/10.1111/dmcn.13162 [ Links ]
50. Rosa-Rizzotto M, Visonà Dalla Pozza L, Corlatti A, Luparia A, Marchi A, Molteni F, Fedrizzi E. A new scale for the assessment of performance and capacity of hand function in children with hemiplegic cerebral palsy: reliability and validity studies. European Journal Of Physical And Rehabilitation Medicine. 2014;50(5): 543-556. Available at: https://moh-it.pure.elsevier.com/en/publications/a-new-scale-for-the-assessment-of-performance-and -capacity-of-han (accessed 25 January 2023). [ Links ]
51. Jongbloed-Pereboom M, Nijhuis-van der Sanden M, Steenbergen B. Norm scores of the box and block test for children ages 3-10years. AmericanJournal of Occupational Therapy. 2013;67(3):312-318. https://doi.org/10.5014/ajot.2013.00664352. [ Links ]
52. Elvrum AG, Zethræus B, Vik T, Krumlinde-Sundholm L. Development and validation of the both hands assessment for children with bilateral cerebral palsy. Physical and Occupational Therapy In Pediatrics. 2017;38(2):113-126. http://dx.doi.org/10.1080/01942638.2017.1318431 [ Links ]
53. Lindstrom-Hazel D, VanderVlies Veenstra N. Examining the Purdue Pegboard Test for occupational therapy practice. Open Journal Of Occupational Therapy. 2015;3(3):1-15. https://doi.org/10.15453/2168-6408.1178 [ Links ]
54. Smith Y, Hong E, Presson C. Normative and validation studies of the nine-hole peg test with children. Perceptual And Motor Skills. 2000;90(3 Pt 1):823-843. https://doi.org/10.2466/pms.2000.90.3.823 [ Links ]
55. Tissue C, Velleman P, Stegink-Jansen C, Aaron D, Winthrop B, Gogola G. Validity and reliability of the Functional Dexterity Test in children. Journal Of Hand Therapy. 2017;30(4):500-506. https://doi.org/10.1016/j.jht.2016.08.002 [ Links ]
56. Ryll UC, Eliasson A, Bastiaenen CHG, Green D. To explore the validity of change scores of the Children's Hand-use Experience Questionnaire (CHEQ) in children with unilateral cerebral palsy. Physical and Occupational Therapy in Pediatrics. 2019;39(2):168-180. https://doi.org/10.1080/01942638.2018.1438554 [ Links ]
57. Arnould C, Penta M, Renders A, Thonnard J. ABILHAND-Kids: a measure of manual ability in children with cerebral palsy. Neurology. 2004;63(6):1045-1052.https://doi.org/10.1212/01.wnl.0000138423.77640.37 [ Links ]
58. van der Holst M, Geerdink Y, Aarts P, Steenbeek D, Pondaag W, Nelissen RH, Geurts AC, Vliet Vlieland TP. Hand-Use-at-Home Questionnaire: validity andreliability in children with neonatal brachial plexus palsy or unilateral cerebral palsy. Clinical Rehabilitation. 2018;32(10):1363-1373. https://doi.org/10.1177/0269215518775156 [ Links ]
59. Uswatte G, Taub E, Griffin A, Vogtle L, Rowe J, Barman J. The pediatric motor activity log - revised: assessing real-world arm use in children with cerebral palsy. Rehabilitation Psychology. 2012;57(2):149-158. https://doi.org/10.1037/a0028516 [ Links ]
60. Taylor R, Kielhofner G. Kielhofner's Research in Occupational Therapy: Methods of Inquiry for Enhancing Practice. 2nd ed. Philadelphia, PA: F.A Davis Company; 2017. [ Links ]
61. McMillanJ, Schumacher S. Research in Education: Evidence-Based Inquiry. 7th ed. London: Pearson Education Limited; 2014. [ Links ]
62. Gee BM, Devine N, Werth A, Phan V. Paediatric occupational therapists' use of sound-based interventions: a survey study. Occupational Therapy International. 2013;20(3):155-162. https://doi.org/10.1002/oti.1354. [ Links ]
63. Maree K. First Steps in Research. 2nd ed. Pretoria: Van Schaik publishers, 2016. [ Links ]
64. Rice S, Winter SR, Doherty S, Milner M. Advantages and disadvantages of using internet-based survey methods in aviation-related research.Journal of Aviation Technology And Engineering. 2017;7(1):58-65. https://doi.org/10.7771/2159-6670.1160 [ Links ]
65. Wright KB. Researching internet-based populations: advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. Journal Of Computer-Mediated Communication. 2005;10(3). https://doi.org/10.1111/j.1083-6101.2005.tb00259.x [ Links ]
66. Minnaar L, HeystekJ. Online surveys as data collection instruments in education research: a feasible option? South AfricanJournal Of Higher Education. 2016;27(1). https://doi.org/10.20853/27-1-233 [ Links ]
67. Beery K, Buktenica N. Beery-Buktenica Developmental Test of Visual Motor Integration. 6th Edition. Bloomington: Pearson Assessments. 2010 [ Links ]
68. Herbst J. Early Childhood Developmental Criteria (ECDC). Austin: Pro-Ed. 1990. [ Links ]
69.Bruininks R, Bruininks B.Bruininks-Oseretsky Test of Motor Proficiency, 2d Edition. Minneapolis: Pearson Assessments. 2005. [ Links ]
70. Henderson S, Sugden D, Barnett A. Movement Assessment Battery for Children, 2d Edition. London: Harcourt Assessment. 2007. [ Links ]
71. Folio M. R, Fewell R. Peabody Developmental Motor Scales: Examiners Manual. 2d Edition. Austin: Pro-Ed. 2000. [ Links ]
72. SquiresJ, Twombly E, Bricker D, Potter L, Ages and Stages Questionnaires, 3rd Edition. Baltimore: Paul H. Brookes Publishing Co. 2009. [ Links ]
73. Hudak P, Amadio P, Bombardier, C. Development of an upper extremity outcome measure: the DASH. American Journal Industrial Medicine, 29(6):602-608. https://doi.org/10.1002/(SICI)1097-0274(199606)291996 [ Links ]
74. Diamantis A. Use of standardised tests in paediatrics: the practice of private occupational therapists working in the United Kingdom. British Journal of Occupational Therapy. 2006;69(6):281-287. https://doi.org/10.1177/030802260606900606. [ Links ]
75. Janse van Rensburg E, Johnson C, Rawlins C, Smit CT, Janse van Rensburg E, Van Greunen I. Describing the use of assessments by occupational therapists in paediatric practice in South Africa. Unpublished undergraduate study. Bloemfontein: University of the Free State; 2017. [ Links ]
76. Visser M, Nel M. Visual perception of five-year-old Afrikaans-speaking children in Bloemfontein using the Beery VMl-6, DTVP-3 and TVPS-3: a follow up study of their English-speaking counterparts in Bloemfontein. South African Journal of Occupational Therapy. 2018;48(3):31-43. https://dx.doi.org/10.17159/2310-3833/2017/vol48n3a6 [ Links ]
77. Nielsen KT, Warhrnes EE. Occupational therapy evaluation: use of self-report and/or observation? Scandinavian Journal of Occupational Therapy. 2015;22(1):13-23. https://doi.org/10.3109/11038128.2014.961547. [ Links ]
78. Sirkka M, Zingmark K, Larsson-Lund M. A process for developing sustainable evidence-based occupational therapy practice. Scandinavian Journal of Occupational Therapy. 2014;21(6):429-437. https://doi.org/10.3109/11038128.2014.952333 [ Links ]
79. Smart A. A multidimensional model of clinical utility. International Journal for Quality In Health Care. 2006;18(5):377-382. https://doi.org/10.1093/intqhc/mzl034 [ Links ]
80. Fieggen K, Lambie L, Donald K. Investigating developmental delay in South Africa: a pragmatic approach. South African Medical Journal. 2019;109(4):210-213. https://doi.org/10.7196/samj.2019.v109i4.13991 [ Links ]
81. De Klerk S, Badenhorst E, Buttle A, Mohammed F, Oberem J. Occupation-based hand therapy in South Africa: challenges and opportunities. South African Journal of Occupational Therapy. 2016;46(3):10-15. http://dx.doi.org/10.17159/2310-3833/2016/v46n3a3 [ Links ]
 Correspondence:
Correspondence:
Marieta Visser
vissermm@ufs.ac.za
Submitted: 15 February 2023
Reviewed: 8 May 2023
Revised: 11 July 2023
Accepted: 12 July 2023
Editor: Blanche Pretorius: https://orcid.org/0000-0002-3543-0743
Data availability: From the corresponding author
Funding: The authors did not receive funding for this study.














