Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Occupational Therapy
versão On-line ISSN 2310-3833
versão impressa ISSN 0038-2337
S. Afr. j. occup. ther. vol.53 no.3 Pretoria Dez. 2023
http://dx.doi.org/10.17159/2310-3833/2023/vol53n3a2
RESEARCH ARTICLE
Content validity of the modified Barthel Index for stroke patients in an African country
Fiona C. Breytenbach; Juliana D. Freeme; Patricia A. de Witt; Denise Franzsen
Department of Occupational Therapy, University of the Witwatersrand, Gauteng, South Africa. Fiona C. Breytenbach: http://orcid.org/0000-0002-7986-0737; Juliana D. Freeme: http://orcid.org/0000-0002-3630-1695; Patricia A. de Witt: http://orcid.org/0000-0003-3612-0920; Denise Franzsen: http://orcid.org/0000-0001-8295-6329
ABSTRACT
BACKGROUND: The Barthel Index is considered the global gold standard for assessing performance in activities of daily living (ADL) tasks, but there has been little research undertaken on this outcome measure for a stroke population in a low to middle income country. The study aimed to determine the content validity of the modified Barthel Index (MBI) for assessing the ADL of stroke patients in an African country.
METHOD: A mixed methods design using the nominal group technique was utilised. The study sample consisted of occupational therapists (n=11) and physiotherapists (n=4) with four or more years' experience working in the field of adult neurorehabilitation in South Africa. Each of the four focus groups analysed the content validity of the MBI using five questions based on the Table of Specifications methodology. Data analysis followed van Breda's steps to analysing multi-group nominal group technique to establish themes arising from each question and were presented according to final rank scores.
RESULTS: The findings highlighted aspects of content validity of the MBI related to language, clarity, content completeness and appropriateness that require revision.
CONCLUSION: This study provides recommendations for the revision of the MBI to improve its content validity for the South African stroke population.
IMPLICATIONS FOR PRACTICE:
• Methodology can be replicated in other multi-cultural and language countries
• Training on administration of the MBI can overcome barriers related to language and item clarity where English is a healthcare worker's second language
• The MBI is currently most suited to environments with water and sanitation infrastructure
• A future study implementing recommendations for revision of the MBI for the African stroke populations is suggested
Keywords: nominal group technique, Occupational Therapy Practice Framework (OTPFIII), Functional Independence Measure (FIM), neurorehabilitation, activities of daily living
INTRODUCTION
Stroke is a leading cause of disability in South Africa, resulting in a high population of people dependent on caregivers to assist them with their activities of daily living (ADL)1. The Barthel Index (BI) is considered the international gold standard for asessing one's independence in ADL namely feeding, chair/bed tranfers, grooming, toileting, bathing, ambulation (walking or wheelchair mobility), stair-climbing, dressing and bowel and bladder management2. One version of the BI - the modified Barthel Index (MBI) - has been studied in various developing countries providing insight into the contextual and cultural factors that affect validity 3-5. Despite being developed and adapted in a Western country, the fact that the MBI is an easy-to-administer, cost-free, accessible, and a brief outcome measure, made it a potentially fitting tool for the African context3. This study aimed to determine whether the MB I accurately reflects the current ADL domain and its appropriateness for the South African stroke population.
Literature review
Stroke rehabilitation aims to promote the recovery and functional indepen dence of survivors to reduce caregiver burden and restore quality of life. One of the primary areas of focus in acute stroke rehabilitation6 is independence in ADL as this is needed for basic independent survival and is often the greatest need of the client. To gain a full picture of a patient's ADL performance, therapists need valid and reliable outcome measures to generate objective results to set realistic rehabilitation goals. Furthermore, these outcome measures can be re-administered throughout the rehabilitation process to monitor a patient's gradual improvement and evaluate the efficacy of treatment rendered.
The BI, developed in the United States of America, was first published in 1965 as an outcome measure scoring a patient's functional improvement during rehabilitation7. The original BI is a 10 item ADL index, which scored a patient as either 'independent' or 'dependent' in the following tasks: feeding, wheelchair transfers, grooming, toilet transfers, bathing, walking , stair climbing, dressing, and bowel and bladder continence. The problem with the BI is that "it fails to quantify the quality and quantity of assistance"8:704 needed in the listed tasks. That is, the amount of assistance required in a task can vary, from total physical assistance to just needing supervision. It would therefore be important for a tool to be sensitive to a patient's gradual improvement in such tasks to measure the efficacy of their rehabilitation. In response to this need. In 1989, Shah et al. published a modified BI (MBI) to improve the sensitivity of the BI by introducing three categories of assistance and descriptions for each item8. Through the adoption and translation of the MBI worldwide, research has identified some items of the instrument to be problematic or culturally loaded3,4, The studies highlighted that the MBI descriptions only considered western tools in the ADL tasks (e.g., knife and fork to feed, western bath, etc.) which may not be appropriate in another nation due to varying people groups, cultures, environments, and languages. Although the most widely recognized and used versions of the BI were published in English7,8, the South African National Department of Health adopted 3 of the 11 South African languages for the national language policy, namely isiZulu, Sesotho and English9. This emphasizes the importance of determining whether the MBI is a valid ADL assessment tool for stroke patients in South Africa.
Validity of the BI
An outcome measure's instrument validity determines whether the tool accurately measures what it is supposed to measure10. The strength of the tool's validity can be determined in several ways; most commonly through analysis of its face validity, criterion-related validity (predictive and concurrent validity), construct validity and content validity10. The construct validity for the BI is well-established11,12 and it has also been shown to have adequate to good criterion-related validity11,13,14. There is also evidence indicating an excellent correlation between the MBI and Functional Independence Measure (FIM); a widely used ADL measure15. Despite themultiple validity studies on the BI and its versions, a rarely reported type of validity is content validity. Content validity is seen as the basis for determining other types of validity, since it compares the representativeness of the items to the framework which you are assessing16. It is essential to regularly revise test content to ensure it accurately reflects current theory and frameworks. That said, there is no record or description of the framework on which the MBI is based.
One framework by which the ADL construct is defined is the Occupational Therapy Practice Framework 3rd edition (OTPFlll)17. The OTPFIII has been used as a framework to outline all aspects of ADL functioning worldwide. The International Classification of Functioning, Disability and Health (ICF) is used as benchmark for the terminology and criteria in the OTPFIII so that a universal language by which occupational therapists assess and treat clients ean be established. Furthermore, the OTPFIII forms a framework which outlines all elements within each domain or 'area of occupation' which overlap the ICF's 'Activity' and Participation' fields. A therapist's chosen outcome measure for assessment of a stroke patient's ADL functioning should reflect this current ADL framework to ensure it remains relevant and assesses all aspects of the ADL domain. Each ADL item listed in the OTPFIII is described below and compared to the content in the MBI and the context of the South African population:
(i)Bathing, showering
According to the OTPFIII, 'bathing and showering' is an ADL activity which encompasses "obtaining and using supplies; soaping, rinsing, and drying body parts; maintaining bathing position; and transferring to and from bathing positions"17:S19. The MBI includes 'bathing self' as an item and requires the person to be able to "use a bathtub, a shower, or take a complete sponge (bed bath) bath. The patient must be able to do all the steps of whichever method is employed without another person being present" 8:708. In a Japanese and Chinese study, the MBI bathing item was criticized for being a culturally loaded item as it does not include various methods of bath i ng3. Th is is true for many other countries, as many rural dwellers bathe themselves by using plastic basins or zinc bathtubs. According to the 2021 General Household survey, only 45.2% of South African households have plumbing inside their homes, with the remaining 54.8% of households sourcing water from outside, neighbour, or communal taps18. Zinc bathtubs and basins are used as a substitute for baths in households without bathrooms or indoor plumbing and 20-liter water containers are corn monly used to carry water from a main water source (communal/ yard tap) into homes to fill these tubs and basins19. Therefore, the MBI does not account for obtaining supplies (water) as described in the OTPFIII.
(ii)Toileting (Bowel and bladder management)
Toileting is grouped with toilet hygiene in the OTPFIII and is described as the "intentional control of bowel movements and urinary bladder and, if necessary, use of equipment or agents for bladder control"17:S,19. The highest score demands the patient's intentional control of the bowels, as having no accidents, and can use a suppository or take an enema when necessary. One study suggested that the bowel control item is a likely measurement of another construct (i.e., not measuring AD L, but physiological body functions)2. This finding is supported by two other studies that found the continence items to misfit the single dimension model4,20. A South African study found that in stroke survivors, the bowel and bladder continence items scored higher than any other items on discharge and at more than six weeks post-discharge21. Th is concurs with two other studies23. These studies suggest content misfit and disproportionate ease of bowel and bladder continence as compared to other items. Although it has been suggested that the continence items should be removed from the MBl2 in some African cultures, bowel and bladder cleansing is an important activity. Gastrointestinal cleansing rituals are performed to rid the person of spiritual possessions to restore health and spiritual harmony through ingesting herbal laxatives, emetics, or administering enemas. Despite the lack of literature in these bowel and bladder cleansing rituals, 80% of the South African black population use the services of traditional healers22, and therefore the everyday practice of this must not be overlooked.
(iii) Toilet hygiene
The OTPFIII details toilet hygiene as "obtaining and using supplies, clothing management, maintaining toileting position, transferring to and from toileting position, cleaning the body, and caring for menstrual and continence needs"17:S;19. The OTPFIII states that toilet hygiene includes using assistive devices such as catheters, colostomies, etc. Toilet hygiene is an ADL item under 'on and off the toilet' in the MBI; the patient must be able to get on and off the toilet, undress, and dress, prevent soiling of clothes and use toilet paper independently8. It also includes that if the patient requires a bed pan, commode, or urinal, they must be able to empty it and clean it8. This item does not include obtaining supplies as described in the OTPFIII, which is a crucial aspect of toileting in many developing nations (e.g., fetching bucket). Authors have suggested this item is culturally loaded since it assumes a western toilet is used3,23. Although the majority of South Africans (64.8%) have access to flushing toilets18, the remainder of the population uses government subsidized pit latrines which are non-flushing toilets within a small, sheltered cu bide situated within 200 meters from the house. Others rely on using buckets which are emptied by municipal sanitary personnel or poured into a dug out hole19,24. Some areas have no sanitary infrastructure and individuals use the bush18. Additionally, not only does the structure of toileting in many African countries differ, but also the position and custom required to toilet. For example, traditional Indian people use flushing squatting toilets and clean by washing themselves, whereas Africans and Caucasians sit on a western toilet or bench and clean themselves by wiping with paper.
It is a concern that menstrual care has never been included in any version of the BI, this is especially import ant since Africa has a younger stroke population25. Additionally, neither the MBI nor one of the professional frameworks consider whether the patient can get rid of the toilet waste or access the toilet - a crucial aspect of toileting in countries without sanitation infrastructure.
(iv)Dressing
Dressing encompasses "selecting clothing appropriately, obtaining clothing from storage area; dressing and undressing in a sequential fashion; fastening and adjusting clothing and shoes; and applying and removing personal devices, prostheses, or orthoses"17 S19. The MBI awards full score for the 'Dressing' item to a patient who can put on, remove, and fasten clothing, tie shoelaces, or put on, fasten, remove corsets and braces, as prescribed8. Notably, the MBI excludes the task of selecting appropriate clothing and obtaining it from a storage area, as described in the OTPFIII. One study comparing the inter-rater reliability of the 100-point BI and MBI to the Functional Independence Measure (FIM), found the 'dressing' item received the lowest verage kappa scores for inter-rater reliability in both versions of the BI and this was attributed to possible ambiguity in the definition s15. The authors therefore recommended revision of the definitions and that dressing be separately scored for upper and lower body15.
(v)Swallowing/Eating
Succeeding in the act of feed ing, eating is "the process of keeping and manipulating food/fluid in the mouth and safely swallowing it" as described by the OTPFlll17 S,19. Eating is not listed as an item in any versions of the BI, probably because it is considered a body function, not an ADL item. This is debatable since bowel and bladder continence are included items; however, no literature has argued this.
(vi)Feeding
Feeding is an ADL described as "the process of setting up, arranging, and bringing food or fluids from the plate or cup to the mouth"17s,19 . In the MBI, the patient should be able to feed them selves if the food is set-up and the patient must put on an assistive device if needed, cut food, and if desired, use salt and pepper, spread butter, etc8. In the literature, the feeding item consistently shows moderate to very good agreement for inter-rater reliability across all versions of the Bl15,26,27 One study criticized the MBI for being culturally loaded since it implies Western utensils are used, as opposed to other utensils such as chopsticks for Chinese populations3 Similarly, African, and Indian ethnic groups do not necessarily use Western utensils and often eat from communal plates using one or both hands.
(vii) Functional mobility
Functional mobility is a broad ADL encompassing one's ability "to move from one position or place to another" as described in the OTPFIH17:S,19. Although this activity is integrated into other ADL, it is comprised of the following activities: in-bed mobility, wheelchair mobility, transfers (wheelchair, bed, car, shower, tub, toilet, chair, and floor), walking, and carrying objects17. Four items of the MBI relate to mobility: namely On and off the toilet (toilet transfers), Stairs, Ambulation (or Wheelchair management), and Chair/bed transfers. The MBI excludes some functional mobility items listed in the OTPFIII such as in-bed mobility which is a common early rehabilitation goal in acute stroke rehabilitation. That said, the chair/bed transfers and ambulation items in the 20-point BI were considered two of the three main predictors of total BI score, indicating that priority mobility areas are included28. Africa's unforgiving terrain, space limitations (overcrowding) and informal dwellings in both urban and rural areas act as additional environmental barriers to the mobility impaired. One author commented that the physical environment can pose a threat to the validity of MBI since differing natural and built environments may not mirror that of developed nations3.
(viii)Personal device care
Personal device care is listed as an ADL under the OTPFIII and involves "cleaning and maintaining personal care items"17 S,19 such as hearing aids, orthotics, glucometers, etc. Although 'personal device care' is not listed as an ADL item in the MBI, device use is integrated into each item's description. In most parts of South Africa, long waiting lists and delayed provision of assistive devices are common due to frequent budget constraints and the lack of therapists29. Furthermore, care and maintenance services are scarce, particularly in rural areas29, leaving patients responsible for the care and maintenance of their devices, emphasizing the needed independence in this area. However, the ability to perform this task is not applicable to all patients as some may not use assistive devices, or the caregiver assumes the role of caring for the device. Therefore, whether the item should be included in the MBI is debatable.
(ix) Personal hygiene and grooming
'Personal hygiene and grooming' as described by the OTPFIII, involves 'Obtaining and using supplies; use of cosmetics; hair, nail, skin, ear, eye, and nose care, applying deodorant; oral hygiene; and the cleaning, and inserting of orthotics and prosthetics"17S,19. In the MBI, the patient should be able to wash their hands and face, comb hair, clean teeth, and shave. The MBI most noticeably excludes nail care, skin care and the use of dental orthotics. The MBI includes obtaining and using the supplies, and states that a female patient must apply her own make-up, if used, but need not braid or style her hair. Interestingly, hair styling is explicitly excluded from the MBI although it is included in the OTPFIII.Initial hair styling in African women is done by another person/professional, but daily maintenance, such as clipping in weaves, is an important daily task to preserve the style. Certain practices in personal hygiene and grooming in African cultures and religions extend beyond what is understood in a western context. For example, 'applying cosmetics' would include traditional mud, clay and natural dyes which are used to ceremoniously deco rate the faces and bodies of men and women.
(x) Sexual activity
Sexual activity is included as an ADL in the OTPFIII and is described as "any activity that results in sexual satisfaction"17;S,19. Compared to the OTPFIII, not all versions of the BI include sexual activity. The need for its inclusion for the African context is debatable. One South African study excluded sexual functioning from both urban and rural versions in the development of an ADL outcome measure because participants from both cohorts felt shocked and uncomfortable if asked about their sexual functioning as it was not considered culturally appropriate30. One of the effects of this attitude results in sex being a frequently forgotten area in ADL assessments.
Two global ADL frameworks, namely the ICF and OTPFIII, form the foundation of current ADL theory, outlining the tasks that constitute this domain. The BI is considered the benchmark ADL outcome measure; how ever, it is essential that this outcome measure reflects current theory. Furthermore, ADL outcome measures should also be appropriate and contextually relevant for the population it is testing. In this literature review, each ADL task listed in the OTPFIII was defined, analyzed for the stroke population, and then compared to the content of the MBI. The literature review highlighted the strengths and weaknesses of the MBI and its appropriateness for the African population. This emphasized the need to determine the content validity of the MBI for stroke patients in South Africa.
METHODOLOGY
Study design
Content validity is established by gaining a consensus among experts whether an assessment tool is an accurate representation of the framework that it is measuring. This study investigated whether the MBI ADL items mirrored the OTPFIII framework ADL items. Although content validity can be established through quantitative or qualitative research designs, a mixed methods approach is preferred as it allows for quantification of the group consensus as well as providing qualitative insights from experts regarding the population and context in which the tool will be used31. A nominal group technique (NGT) using a consensus-generating participatory methodology was chosen for simultaneously collecting of qualitative (test contents) and quantitative (ranking of test items) data from experienced clinicians in focus groups32. The Table of Specifications (TOS) was used as a universal methodological structure as it uses a two-way chart to align all the topics of the MBI, as well as the number of items associated with each topic, to with all concepts that need to be assessed with a particular ADL topic31. Thus, qualitative data were collected from the participants in small groups while the more quantitative data were collected through a consensus seeking process.
Ethical considerations
Ethical clearance was obtained through the University of the Witwatersrand Human Ethics Committee to undertake this study (Certificate no. M130810). Permission to undertake the study was also given by the publishers of the MBI. Participants who met the inclusion criteria were recruited using a written invitation in an information sheet that detailed the research's nature, scope, and anticipated data collection time. The voluntary nature of participation was stressed as were the processes that were followed to maintain confidentiality throughout the research process. Participants who agreed to participate gave written consent and consent for the focus groups to be audio-recorded.
Study population and sample
The population was defined as experienced rehabilitation healthcare workers (HCWs) including occupational therapists and physiotherapists working in the field of neurological rehabilitation in Gauteng, South Africa. A snowball sampling method was chosen due to the poorly defined population parameters of occupational therapists and physiotherapists working in neurorehabilitation with four or more years working experience33.
Data collection
A demographic questionnaire developed for occupational therapists from the same population was used34. To ensure this questionnaire was unbiased between professions, it was completed by two physiotherapists to ensure the questions were clear and easy to understand. Suggested changes made by the participants were implemented. This was completed by all participants at the beginning of the NGT groups.
Four NGT groups, of three to six participants each, were held over 10 months. Each group had a mix of both professions. The discussions were approximately 90 minutes in duration. Before the group, participants who consented to participating were given a chance to peruse the MBI. The first author facilitated the groups. Group participants were posed 5 questions: i) Who should administer the MBI? ii) What language should the MBI be in? iii) How can we rephrase the MBI to make it clearer and more understandable? iv) Compare the OTPFIII to the MBI. Are there any items of the MBI you would include/exclude? v) How do South African ADL differ from western ADL?
The NGT followed four steps of the TOS for each question asked:
Generating ideas: The facilitator presented the question to the group in written form and read it to the group. All participants were directed to silently generate ideas in brief statements on their notepads.
Recording ideas: Participants engaged in a round-robin feedback session (without debate); each statement was typed by the facilitator and projected onto a screen.
Discussing ideas: Discussion regarding each statement was then facilitated to determine clarity, importance, and consensus. Participants discussed each item in-depth (if found to be important) and compared it to current theory (OTPFIII) and clinical experience.
Voting on ideas: Participants each choose five statements from the list of statements generated that they found the most important regarding that question. Each participant voted privately on their voting cards by prioritizing the statements from one to five (one being the 'most important'). Each voting card was collected, and the votes were tallied to identify the ideas rated highest by the group. At the end of the session all group statements and voting cards were collected
Data analysis
All data from the demographic questionnaires were entered into Microsoft Excel. Univariate analysis was done to describe the central tendency (mean, median), range and present frequency distributions of demographic data. Van Breda's seven steps to analysing multi-group NGT data was used for the current study32. This data analysis process is recommended for analysis of combined qualitative and quantitative data required for the current study35.
i). Each statement generated over the four NGT groups was listed on a Microsoft Excel spreadsheet with its accompanying group number, summed scores received from votes (highest vote = 5 points, lowest vote = 1 point), the average score (sum of scores/number of persons in the group) and then arranged according to importance (highest averages for scores for each group listed first). ii) All statements were thoroughly perused, and similar statements were grouped together into themes whilst ensuring that all themes were mutually exclusive and collectively exhaustive. This process was repeated several times until the researcher was satisfied that all statements were allocated a theme, and all necessary themes were generated and distinct from one another. Each theme was named, defined, numbered, and typed next to each. No new themes arose in the fourth NGT group and therefore, data saturation was reached.
iii). Four volunteers not involved in the data analysis were asked to peer-review the previous step. The themes and their descriptions were provided, and each volunteer worked independently to allocate a theme to each statement. Once all completed lists were returned to the researcher, the group of volunteers convened to discuss any discrepancies. Themes were added, divided, combined, and re-defined by the group until consensus on each theme-statement pairing was reached.
iv)The researcher summed the scores of ranked importance, ranked frequency, ranked average producing a final rank score. Final rank scores were arranged in descending order from most to least significant.
RESULTS
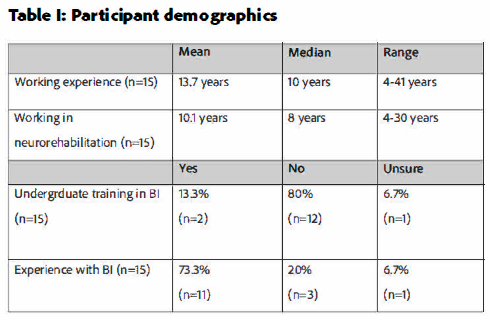
The sample consisted of 15 participants, 11 (73.3%) registered occupational therapists and four (26,7%) physiotherapists working in the city of Pretoria or Johannesburg, South Africa. All participants (n=15) were working in the neuro-rehabilitation field in government, private or academic facilities at the time of data collection. As can be seen from Table I (below), the mean number of years that the participants had worked was 13.7 years and the mean number of years in work in the neurorehabilitation field was 10.1 years. Participants reported that only 13% (n=2) had had training in the BI during their undergraduate training but 73% (n=11) had had experience with the BI while working.
Administrators and language of the test
Participants considered therapists (occupational therapists and physiotherapists) and nurses to be the persons who should administer the MBI.The theme 1B - 'Therapists and nurses' was ranked highest of the five themes in terms of importance and frequency of statements with a final rank score of 14/15. For the question "What language should the MBI be in?" theme 2B -'English for HCWs' was ranked highest overall with a final rank score of 14/15 indicating that participants agreed that the MBI should remain in English since HCWs typically administer the MBI. The second highest final ranked theme was 'Translate MBI into all SA languages'(score 10.5/15}
Instrument clarity
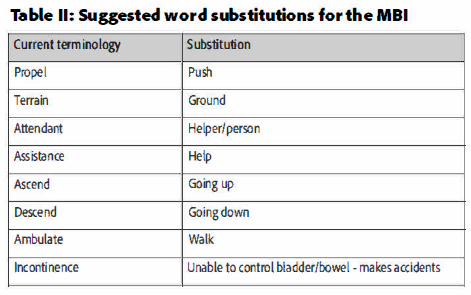
Six themes arose from the list of 22 statements generated by the four NGT groups in response to the third question, "How can we rephrase the MBI to make it clearer and more understandable?". The overall highest ranked theme was theme 3A - 'Quantify amount or type of assistance' with a final rank score of 16/18. The statements contributing to this theme emphasized the importance of quantifying the amount of assistance given to the patient using percentages. One statement suggested including a key on the document to improve the reliability of what is understood by words such as 'minimum', 'moderate' and 'maximum' assistance, which was frequently raised in the groups and often compared to what is used in the FIM. Theme 3B - 'Use simple contextually relevant words or explanations'- obtained the highest rankings in importance (ranked 6/6) and frequency of statements (ranked 6/6) with a final rank score of 15/18. Table II (adjacent) lists substitutions for diffi cult words as suggested by participants.
Content areas: Completeness
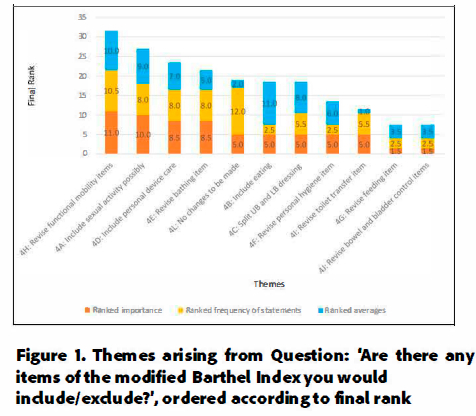
Twelve themes arose from the list of 34 statements generated by the four NGT groups in response to the question "Compare the OTPFIII to the MBI. Are there any items of the MBI you would include/exclude?". As shown in Figure 1 (avove), the highest ranked themes were 'functional mobility' (final rank 31.5/36), 'sexual activity' (final rank 27 /36), and 'personal device care' (final rank 23.5/36) respectively. The theme with the highest ranked frequency of statements is theme 4L which grouped statements that referred to aspects of the MBI that should not be changed.
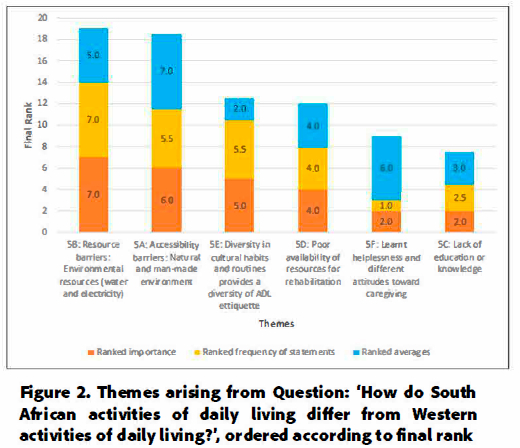
Content areas: Appropriateness
Seven themes arose from a list of 32 statements generated by the four NGT groups in response to the question "How do South African ADL differ from Western ADL?". As reflected in Figure 2 (page 9), two themes were awarded a considerably higher final ranking compared to other themes; theme 5B - 'Resource barriers' - and theme 5A - 'Accessibility barriers' - scored 19/21 and 18.5/21 respectively, with the 'Resource barriers' theme having the highest ranked importance and frequency of statements, and the 'Accessibility barriers' theme having the highest ranked average.
DISCUSSION
The participants in this study (n=15) comprised of occupational therapists and physiotherapists working in the field of neurorehabilitation in various settings with an average of 13.7 years working experience. While a nominal group technique typically requires a single group with between 4-7 participants, 15 participants were recruited into this study to hear the voices of clinicians in different contexts. Eleven participants were occupational therapists (73.3%) which may have created a bias toward occupational-therapy focused themes, while only four physiotherapists were included, possibly placing less emphasis on mobility items. While majority (73.3%) of participants had used the BI in practice, most (80%) participants had not received undergraduate training of the tool. This finding highlights the need for a valid ADL measure that can be understood on first impress ion and the need for formal training in university curricula.
Language and administrators
The first question regarding who should administer the MBI aimed to orientate the participants and reach a consensus on who should administer the tool - since the language of a tool is dependent on who will be administering it. In this study, participants voted that occupational therapists, physiotherapists and nurses should be the persons who should administer the MBI to stroke patients. Similarly, nurses, therapists and physicians are the primary administrators of the BI globally27. Although the BI can be self-administered or completed by patient caregivers, participants were of the view that experienced clinicians would score items most reliably based on direct observation. This finding is supported by Waeherens et al.36 who found self-report scores to be higher than those completed by observation. This finding lent itself to the researcher's second question to the group, "What language should the MBI be in?" since South Africa is a multilingual nation. Participants reported English to be the most common language in their work setting and therefore voted for the MBI to remain in English. However, all participants were working in Gauteng which may not be representative of all South African healthcare settings. The participants decision for the tool to remain in English was also practical as translation into all official languages will be costly and time-consuming. Further research is needed to determine the effect of training on the inter-rater reliability of the MBI in South Africa as English not everyone's primary language. If training is found to improve the inter-rater reliability of the tool, it is recommended that standardized directions or training options that are feasible for the African population be developed. It is important to note that although the BI is an observation-based tool and doesn't require translation into a patient's home language, the stroke survivor should still have a clear grasp of what the HCW is using the tool for to provide informed consent37. Translation of the tool description or the use of a translator would be of help to address this concern.
Instrument clarity
To determine a tool's content validity; clarity, statement fit (item appropriateness), redundancy and consistency must be inspected38. Clear and simple wording ensures that the items are easy to understand and make sense38. The third question posed to the group, "How can we rephrase the MBI to make it clearer and more understandable?" resulted in theme 'Quantify amount or type of assistance' being ranked highest overall. Th e MBI uses a variety of methods in describing assistance, such as using descriptors for instance "minimum /moderate/ maximum", or of the number of people required, e.g., "two attendants" or "one person". This varying phrasing was perceived as vague and inconsistent by participants.
Participants suggested that, to improve understanding and clarity in the MBI, the amount of assistance required in each item must consistently be quantified either through percentages or the number of persons required to assist in the task. However, this method of quantifying the degree of assistance can still be subjective.
In terms of clarity participants suggested that the MBl's language may not be clear and appropriate for the South African population since English is many people's second language. This finding is supported by several studies in countries where English was not the primary spoken language3,4,5,39. Participants suggested that difficult terminology in the MBI be substituted with more common/simple words, and/or providing definitions of words as shown in Table I (page 8) This theme was the most discussed and most voted theme across the four NGT groups, emphasizing the urgency participants placed on the need to improve the clarity of the MBI.
Content areas: Completeness
As summarized in the literature review, four of the nine ADL tasks in the OTPFIII are not included in the MBI. Throughout the four NGT groups, all these items were suggested to be included in the MBI; functional mobility was ranked highest, followed by sexual activity, personal device care and lastly, eating.
The first suggesting revision of functional mobility items highlighted that the MBI should encompass all aspects of functi onal mobility. The statements receiving the highest ranked votes for this theme were statements pertaining to the inclusion of 'in-bed mobility' as an item, confirming in-bed mobility as an important and common rehabilitation goal. The current study highlighted that when the accessibility barriers in the community are considered, mobilizing becomes more challenging and time-consuming compared to Western environments. Specifically, rough terrain, space limitations, poor accessibility, far distances to toilets and a lack of housing fixtures makes this ADL more physically demanding. Therefore, the content description of the items should accommodate for aspects of the African environment that affects mobility to improve the validity and sensitivity of the tool.
Secondly, statements contributing to the sexual activity item was ranked third highest in the fourth question posed to the groups - suggesting that it should be considered for inclusion in the MBI. All statements contributing to this theme identified that sexual activity may not be applicable to some patients and would be difficult to gain information regarding functioning in this area. However, the literature recognizes sexual activity as . an important, but frequently overlooked aspect in neurorehabilitation40 Therefore, one must be aware that results may be biased by therapists in this study's NGT groups since the literature indicates that therapists a re reluctant to approach this subject and therefore neglect it in therapy40. This item remains a controversial topic and it is recommended that future studies investigate the opinions of South African stroke survivors to determine whether this is a need in their rehabilitation.
Thirdly, 'Include personal device care' was ranked the fourth highest theme in the fourth question posed to the groups. As was the case with sexual activity, personal device care is a debatable item to be included in the MBI as it may not be applicable to all patients. Furthermore, there is a multitude of varying types and models of assistive devices and therefore scoring for this item would be difficult and possibly unreliable. It is recommended that future studies investigate the opinions of stroke survivors in South Africa and other diverse countries to determine whether this is a need in their rehabilitation.
Lastly, 'Include eating (swallowing)' was ranked the least important theme amongst the four 'missing' ADLs from the MBI. 'Include eating (swallowing)' was ranked lower than theme 4L 'No changes to be made to the MBI'. Therefore collectively, participants felt it was more important for the MBI to remain as is than to include 'eating (swallowing)' as an item. Participants voiced concern that speech and language therapists typically perform swallow assessments, and an unsafe assessment could result in aspiration since many stroke patients are prone to dysphagia. Therefore, it is not recommended to include eating as an ADL item in the MBI.
Content areas: Appro priateness
Two themes that strongly emerged from the question "How do South African ADL differ from Western ADL? - were 'Resource barriers' and 'Accessibility barriers', with respective final rank scores of 19/21 and 18.5/21. Participants discussed how a lack of resources (access to water and electricity) acts a barrier to some South African's performance in their ADL making tasks more difficult and time-consuming. For example, one may pour bathwater from an indoor tap, drain it once complete, and have materials readily available at the bath/shower. However, this is not the case for 54.8% of the South African population who need to fetch water from a yard or communal tap, carry the water in a bucket or container, and fill a basin or zinc tub/basin to bath1S. Thereafter, the tub or basin must be carried outdoors to be emptied. The MBI does not include 'obtaining supplies' as part of the bathing as escribed in the OTPFIII, indicating incompleteness of the content of the tool. Additionally, South African ADL are more difficult due to accessibility barriers, that is differences in the natural environment and man-made environment. Rough terrain in rural areas, limited and crowded space in homes, toilets built outside, and a lack of indoor fixtures make tasks more difficult to complete due to the physical demands needed to overcome barriers such as one requiring better balance when walking over an uneven surface, or increased strength and endurance to walk or push a wheelchair to access an outside toilet. With such a large portion of the population relying on these environments, it emphasizes the stark environmental differences between developed and developing countries and the need for the MBI to not assume a contextual bias. It is recommended that each item description of the MBI consider all environments needed to complete ADL.
Limitations of the study
The demographic profile of the group consisted of almost three quarters of participants being occupational therapists due to the sampling method which may create a bias toward occupational-therapy focused themes. Future studies should ideally include an equal number of occupational therapists, physiotherapists, and nurses, as these HCWs most commonly administer the MBI.
In the NGT groups, the researcher undertook the role of the group facilitator as well as being the scribe which caused frequent breaks which interrupted the flow of thought and debate - in future it is recommended that a research assistant is used. Demographic data should have been checked for normality. The fourth and fifth question posed to jurors could have been phrased around the content of the MBI and how ADL tasks are performed rather than as a comparison to generate more statements and insight from the groups.
CONCLUSION AND RECOMMENDATIONS
The Barthel Index has endured a lot of criticism for not being culturally sensitive enough, however it remains the most feasible ADL outcome measure for the South African population since it is cost-free, brief, accessible, and does not require formal training.The findings of the current study highlighted aspects of the MBl's content related to language, clarity, completeness, and appropriateness that require revision.
The following recommendations list summarized the findings from this study and serve as a guideline to future studies that aim to standardize the MBI for the South African stroke population.
Administrators: The MBI should be designed for use by nurses, occupational therapists, and physiotherapists.
Language: The MBI should remain in English, however item description revision was recommended.
Items: Each item description in the MBI referring to assistance must quantify the amount of assistance required (e.g., extent of task completed by therapist in percentage). Complex or contextually unfamiliar terminology should be substituted by simpler words as suggested in the results. Where terminology cannot be substituted by simpler words are given a longer explanation or a 'definition sheet' be provided as an appendix to the tool.
Revision: Bathing and dressing items to be revised. The item name should be changed from 'bathing self' to 'washing' and should include obtaining supplies (fetching and emptying bathwater) as this is relevant to rural areas. The bathing item should include zinc tub and basin as options. The dressing item should be split into two sections, namely, 'Upper-body dressing' and 'Lower-body dressing'.
Training: South African universities training occupational therapists, physiotherapists and nurses should include the MBI in their curriculum.
Content: Each item of the MBI should consider all environments and fixtures needed to complete ADL and score the difficulty accordingly.
Additional items: Although no items were suggested for deletion, additional items to be added to the MBI relating to functional mobility were suggested for inclusion: All aspects of functional mobility should be included in the MBI, such as in-bed mobility, and the content description of the functional mobility items should accommodate aspects of the South African environment that affects mobility (e.g. ability to walk over rough terrain).
It is suggested that a future study implementing the abovementioned recommendations be conducted and a new version be developed for the African stroke population.
Author Contributions
Fiona Breytenbach devised the main conceptual idea, collected, and analysed the data and wrote the initial draft of the manuscript. Juliana Freeme supervised the research, assisted with conceptualisation, methodology and provided key literature and critical feedback on draft manuscript. Patricia de Witt and Denise Franzsen consulted during data collection and analysis, and critically reviewed the manuscript.
Competing Interests
The authors have no competing interests to declare.
Acknowledgements
We want to thank all participants for your contribution to this study and the following hospitals for the use of their premises; Steve Biko Academic Hospital and Mediclinic Muelmed Hospital. Thank you to co-author Juliana Freeme for your guidance throughout the research process and the OT teams at Kalafong Provincial Tertiary Hospital and Chris Hani Baragwanath Academic Hospital for your continued assistance and support.
REFERENCES
1. Connor MD, Walker R, Modi G, Warlow CP. Burden of stroke in black populations in sub-Saharan Africa. The Lancet Neurology 2007; 6(3): 269-278. https://doi.org/10.1016/S1474-4422(07)70002-9 [ Links ]
2. de Morton NA, KeatingJL, Davidson M. Rasch analysis the Barthel Index in the assessment of hospitalized older patients after admission for an acute medical condition. Archives of Physical Medicine and Rehabilitation. 2008; 89(4): 641-647. https://doi.org/10.1016/j.apmr.2007.10.021 [ Links ]
3. Leung SOC, Chan CCH, Shah S. Development of a Chinese version of the Modified Barthel Index - Validity and reliability. Clinical Rehabilitation. 2007; 21(10): 912-922. https://doi.org/10.1177/0269215507077286 [ Links ]
4. Küçükdeveci A, Yavuzer G, Tennant A, Süldür N, Sonel B, Arasil T. Adaptation of the Modified Barthel Index for use in physical medicine and rehabilitation in Turkey. Scandinavian Journal of Rehabilitation Medicine. 2000; 32(2): 87-92. https://doi.org/10.1080/003655000750045604 [ Links ]
5. Oveisgharan S, Shirani S, Ghorbani A, Soltanzade A, Baghaei A, Hosseini S, et al. Barthel Index in a Middle-East country: Translation, validity and reliability Cerebrovascular Diseases. 2006; 22(5-6): 350-354. https://doi.org/10.1159/000094850 [ Links ]
6. De Wit L, Putman K, Lincoln N, Baert I, Berman P, Beyens H et al. Stroke rehabilitation in Europe: What do physiotherapists and occupational therapists actually do? Stroke. 2006; 37(6): 1483-1489. https://doi.org/10.1161/01.str.0000221709.23293.c2 [ Links ]
7. Mahoney FI, Barthel DW. Functional evaluation: The Barthel Index. Maryland State MedicalJournal. 1965; 14(1): 56-61. [ Links ]
8. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. Journal of Clinical Epidemiology. 1989; 42(8): 703-709. https://doi.org/10.1016/0895-4356(89)90065-6 [ Links ]
9. National Deptartment of Health. National Department of Health: Language Policy [Government Gazette]. No. 442 2015. Retrieved from: https://static.pmg.org.za/150527healthlanguagepolicy.pdf [ Links ]
10. Brink H. Fundamentals of Research Methodology for Health Care Professionals. 2nd Edition. Cape Town: Juta & Co.; 1996. [ Links ]
11. Hsueh I, Lee M, Hsieh C. Psychometric characteristics of the Barthel Activities of Daily Living Index in stroke patients. Journal of Formosan Medical Association. 2001; 100(8): 526-532. https://doi.org/10.1136/jnnp.73.2.188 [ Links ]
12. Hobart J, Thompson A. The five item Barthel Index. Journal of Neurology, Neurosurgery and Psychiatry. 2001; 71(2): 225-230. https://doi.org/10.1136/jnnp.71.2.225 [ Links ]
13. Liu C, McNeil JE, Greenwood R. Rehabilitation outcomes after brain injury: Disability measures or goal achievement? Clinical Rehabilitation. 2004; 18(4): 398-404. https://doi.org/10.1191/0269215504cr741oa [ Links ]
14. Wade DT, Hewer RL. Functional abilities after stroke: Measurement, natural history and prognosis. Journal of Neurology, Neurosurgery and Psychiatry. 1987; 50(2): 177-182. https://doi.org/10.1136/jnnp-2011-301689 [ Links ]
15. Fricke J, Unsworth CA. Inter-rater reliability of the original and modified Barthel Index, and a comparison with the Functional Independence Measure. Australian Occupational Therapy Journal. 1996; 43(1): 22-29. https://doi.org/10.1111/j.1440-1630.1997tb00750.x [ Links ]
16. Haynes SN, Richard DCS, Kubany ES. Content validity in psychological assessments: A functional approach to concepts and methods introduction to content validity. Psychological Assessment. 1995; 7(3): 238-247. https://doi.org/10.1037/1040-3590.7.3.238 [ Links ]
17. American Occupational Therapy Association. Occupational therapy practice framework: Domain & process 3rd Edition. American Journal of Occupational Therapy. 2014; 68(Suppl. 1): S1-48. https://doi.org/10.5014/ajot.2014.682006 [ Links ]
18. Statistics South Africa. General Household Survey [Internet]. 2021. Retrieved from: https://www.statssa.gov.za/publications/P0318/P03182021.pdf [ Links ]
19. Thomas EP, Seager JR, Viljoen E, Potgieter F, Rossouw A, Tokota B, et al. Household Environment and Health in Port Elizabeth, South Africa. Cape Town: Medical Research Council; 1999. [ Links ]
20. Van Hartingsveld F, Lucas C, Kwakkel G, Lindeboom R. Improved interpretation of stroke trial results using empirical Barthel Item weights. Stroke. 2006; 37(1): 162-166. https://doi.org/10.1161/01.STR.0000195176.50830.b6 [ Links ]
21. Mamabolo M, Mudzi W, Stewart A, Olorunju S, Singh A. A study to determine post discharge functional improvements in patients with stroke. South African Journal of Occupational Therapy. 2009; 39(1): 15-18. [ Links ]
22. Abdool Karim SS, Ziqubu-Page T, Arendse R. Bridging the gap. Durban: South African Medical Research Council; 1992. [ Links ]
23. Murdock C. A critical evaluation of the Barthel Index, part 1. British Journal of Occupational Therapy. 1992; 55(3): 109-111. https://doi.org/10.1177/030802269205500310 [ Links ]
24. Statistics South Africa. Statistical release: Mid-year population estimates [Internet]. 2015. Retrieved from: http://www.statssa.gov.za/publications/P0302/P03022015.pdf (3 Dec 2020) [ Links ]
25. Connor M, Tipping B, de Villiers L, Wainwright H, Candy S, Bryer A. Stroke in patients with human immunodeficiency virus infection. Journal of Neurology, Neurosurgery and Psychiatry. 2007;v78(12):v1320-324. https://doi.org/10.1136/jnnp.2007.122416 [ Links ]
26. Sainsbury A, Seebass G, Bansal A, Young JB. Reliability of the Barthel Index when used with older people. Age and Ageing. 2005; 34(3): 228-232. https://doi.org/10.1093/ageing/afi063 [ Links ]
27 Duffy L, Gajree S, Langhorne P, Stott DJ, Quinn TJ. Reliability (inter-rater agreement) of the Barthel Index for assessment of stroke survivors: Systematic review and meta-analysis. Stroke. 2013; 44(2): 462-468. https://doi.org/10.1161/strokeaha.112.678615 [ Links ]
28.Ellul J, Watkins C, Barer D. Estimating total Barthel scores from just three items: The European Stroke Database "minimum dataset" for assessing functional status at discharge from hospital. Age and Ageing. 1998; 27(2): 115-122. https://doi.org/10.1093/ageing/27.2.115 [ Links ]
29. Visagie S, Scheffler E, Schneider M. Policy implementation in wheelchair service delivery in a rural South African setting. African Journal of Disability. 2013; 2(1): 1-9. https://doi.org/10.4102/ajod.v2i1.63 [ Links ]
30. Visagie S, Scheffler E, Schneider M. Policy implementation in wheelchair service delivery in a rural South African setting. African Journal of Disability. 2013; 2(1): 1-9. [ Links ]
31. Maleka MED. The development of an outcome measure to assess community reintegration after stroke for patients living in poor socioeconomic urban and rural areas of South Africa (Dissertation). Johannesburg: University of Witwatersrand; 2010. https://doi.org/10.1177/1558689813476922 [ Links ]
32. Newman I, Lim J, Pineda F. Content validity using mixed methods approach: Its application and development through the use of a Table of Specifications methodology. Journal of Mixed Methods Research. 2013; 7(3): 243-260. https://www.researchgate.net/publication/292746636_Steps_to_analysing_multiple-group_NGT_data (1 Feb 2016) [ Links ]
33. van Breda A. Steps to analysing multiple-group NGT data. The Socia-Work Practitioner-Researcher. 2005; 17(1): 1-14. Retrieved from: https://www.researchgate.net/publication/292746636_Steps_to_analysing_multiplegroup_NGT_data (1 Feb 2016) [ Links ]
34. Parker C, Scott S, Geddes A. Snowball sampling. SAGE research methods foundations. 2019.Freeme JD. The training and practice in neurological rehabilitation theories in the occupational therapy management of stroke patients in South Africa (Dissertation). Johannesburg : University of Witwatersrand; 2011. [ Links ]
35. McMillan S, Kelly F, Sav A, Kendall E, King M, Whitty J, et al. Using the nominal group technique: How to analyse across multiple groups. Health Services and Outcomes Research Methodology. 2014; 14(3): 92-108. https://doi.org/10.1007/s10742-014-0121-1 [ Links ]
36. Wæhrens EE, Bliddal H, Danneskiold-Samsøe B, Lund H, Fisher AG.Differences between questionnaire- and interview-based measures of activities of daily living (ADL) ability and their association with observed ADL ability in women with rheumatoid arthritis, knee osteoarthritis, and fibromyalgia. Scandinavian Journal of Rheumatology. 2012; 41(2): 95-102. https://doi.org/10.3109/03009742.2011.632380 [ Links ]
37. Sobane K, van der Merwe C, Shandu B. The silence of South African health policies on the language barrier between healthcare providers and patients language matters. 2020; 51(3): 87-107. https://doi.org/10.1080/10228195.2020.1794017 [ Links ]
38. Mastaglia B, Toye C, Kristjanson U. Ensuring content validity in instrument development: Challenges and innovative approaches. Contemporary Nurse. 2003; 14(3): 281-291. https://doi.org/10.5172/conu.14.3.281 [ Links ]
39. Lorica J, Rosdewi S, Solon M. Construct validity Indonesian version of Barthel index for post stroke. Indian Journal of Public Health. 2020; 11(3): 1996-2000. [ Links ]
40. Mellor RM, Greenfield SM, Dowswell G, Sheppard JP, Quinn T, McManus RJ. Health care professionals' views on discussing sexual wellbeing with patients who have had a stroke: a qualitative study. PLoS One. 2013; 8(10): 1-9. https://doi.org/10.1371/journal.pone.0078802 [ Links ]
 Correspondence:
Correspondence:
Fiona Breytenbach
fiona.breytenbach@wits.ac.za
Submitted: 16 February 2021
Reviewed: 25 November 2021
Revised: 21 June 2023
Accepted: 6 July 2023
Editor: Blanche Pretorius: https://orcid.org/0000-0002-3543-0743
Data availability: From The Corresponding Author
Funding: None To Declare














