Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.53 n.2 Pretoria Aug. 2023
http://dx.doi.org/10.17159/2310-3833/2023/vol53n2a8
RESEARCH ARTICLE
Integrated knowledge-translation in occupational therapists working with high-risk infants in South Africa: An explorative qualitative inquiry
Ayesha DawoodI; Pragashnie GovenderII; Samantha J YorkIII; Gina RenckenII; Michael O OgunlanaII, IV
IOccupational Therapy, King Dinizulu Hospital Complex, Department of Health, KwaZulu-Natal, South Africa. Ayesha Dawood: https://orcid.org/0000-0002-3316-5907
IIDiscipline of Occupational Therapy, School of Health Sciences, University of KwaZulu Natal, South Africa. Pragashnie Govender: https://orcid.org/0000-0003-3155-3743; Gina Rencken: https://orcid.org/0000-0002-3658-4453
IIIOccupational Therapy Private Practice, KwaZulu-Natal, South Africa. Samantha J York: https://orcid.org/0000-0002-6535-3662
IVAssistant Director: Physiotherapy Services, Federal Medical Centre Abeokuta, Nigeria. Michael O Ogunlana: https://orcid.org/0000-0001-6877-6938
ABSTRACT
BACKGROUND: This qualitative study explored the knowledge to practice gaps of occupational therapists who have a vital role in neurodevelopmental supportive care for high-risk infants
METHODS: Via purposive sampling, 17 therapists working in public health in South Africa were recruited to participate in virtual focus groups. Data were thematically analysed using a hybrid approach
FINDINGS: Five themes emerged, which included (i) occupational therapy and neonatal care in the public health sector, (ii) knowledge acquisition and knowledge synthesis, (iii) knowledge translation and utilisation, (iv) contextual barriers and adaptation and (v) the ideal occupational therapist in the ideal neonatal setting. Facilitators, inhibitors, referrals, and interest in occupational therapy neonatal care were also highlighted
CONCLUSIONS: Knowledge to practice gaps in occupational therapy include insufficient training, a decreased interest in neonatal care, staff shortages, multi-disciplinary team rotations and a reduced understanding of the professional role and scope of occupational therapy. Resources, training, and policy development appear to be necessary to inform a standard of care
Implication for practice
The role of the occupational therapist in supporting high risk infants is generally limited and remains somewhat unknown in current South African contexts. It is essential to identify knowledge-to-practice gaps for occupational therapists supporting high-risk infants in the public health sector for successful implementation of neurodevelopmental supportive care.
By the exploration of practitioner opinions and insight through appreciating the role of the occupational therapist in managing high risk infants, contextually specific and relevant knowledge translation interventions may be developed and implemented which have implications for evidence-based practice and more successful outcomes in the high-risk infant.
Keywords: neonatal care, evidence-based practice, knowledge utilisation, early intervention, neurodevelopmental supportive care
INTRODUCTION
Goal three of the Sustainable Development Goals (SDG) aims to decrease neonatal mortality rates by 1.2% in 1000 births and reduce mortality in children below five years before and until 20301. Whereas child mortality rates have shown a decline over the past 20 years, there is a need to emphasise child morbidity. The results of preterm birth complications and other neonatal risk factors at birth may lead to a neurological injury resulting in long-term cognitive, sensory, and motor impairments in infants2. There is a paucity of literature on morbidity rates, and the resultant impairment following neurological insults post preterm and at full-term births in low and middle-income countries (LMICs). However, 98% of neonatal morbidity occurs in underprivileged countries3. Morbidity forms part of the occupational therapy scope of practice. Early recognition of neurodevelopmental disorders and the care of the developing brain through neurodevelopmental supportive care (NDSC) should thus be implemented in neonatal intensive care units (NICU) to reduce the severity of morbidity.
There has been a surge of evidence relating to knowledge translation (KT) in the past ten years, with stakeholders concurring that knowledge requires translation into action. A scoping review highlighted limited studies indicating the benefits and results of KT strategies and decreased practical research on integrating KT4. Notwithstanding this, a recent study in South Africa (SA) utilised implementation research to investigate the current practices of NDSC amongst the multi-disciplinary team (MDT) who service the NICU in two public hospitals in the province of Gauteng5. Hardy and colleagues investigated community service occupational therapists experiences working in the NICU in KwaZulu-Natal (KZN), South Africa6. Anecdotal evidence has identified a gap within the South African context in determining how permanently employed occupational therapists working in the NICU/high care units integrate their clinical experiences with evidence-based practice (EBP) in the care of the high-risk infant. There is evidence to suggest a lack of research utilisation by occupational therapists who work in the NICU in the South African public health sector, with many therapists utilising various sources that may not be evidence-based or are outdated6. The exploration and use of KT in developing and determining occupational therapists' skills in utilising EBP have been identified in previous studies in developed countries7. However, to the authors' best knowledge, it has not been explored with occupational therapists who support high-risk infants in the public health sector of KZN8.
The occupational therapist working in the NICU must have expert training in NDSC to plan inclusive intervention, evaluation, and discharge planning of the neonate, provide education to staff and families, and make fast, efficient, and effective decisions8-11. A recent study has discovered that occupational therapists found it challenging to establish their roles within the NICU; therapists felt that they did not have the adequate skills and knowledge to work in the stressful NICU environment. The hardships experienced in the public health sector, especially with the high infant and child mortality and morbidity rates, indicate the need to translate EBP into practice12-13. Therefore, the current clinical standards of care must be determined before EBP can be applied14. This study aims to discover the existing knowledge to practice gaps and visualise the ideal knowledge to practice interventions for occupational therapists. They support high-risk infants by exploring occupational therapists' perceptions of working in neonatal care in the public health sector of KZN.
Literature Review
There is a limited understanding of the NDSC approach for high-risk infants15. Sensory development during the perinatal period is a susceptible phase that occurs in a particular order, with each system maturing in its course16. Implementation of NDSC in NICU's and high care settings during this period will have lasting consequences on a neonate's perceptual and behavioural development. One of the cited reasons for high neonatal mortality rates were attributed to a poorly skilled MDT17. Other studies have deduced that the clinical outcomes of implementing NDSC during an infant's stay in the NICU result in; reduced morbidity in the initial four weeks of being admitted, a decreased amount of time in the NICU, and a significant improvement in neurobehavioral functioning on discharge18. Over the last decade, there has been a shift from prioritising survival to reducing the consequences of morbidity to ensure an enhanced quality of life19. Presently there is a paucity in the SA literature investigating the quality of care and the interventions sourced and utilised by the MDT with high-risk infants in the NICU20. In the public health sector of KZN, the number of occupational therapists has decreased to 45%, with many institutions managed by junior occupational therapists21. For new therapists, the NICU, is an intimidating environment to be working in without supervision6,22. Hardy et al.8, in their study, discovered that occupational therapists found it challenging to establish their roles within the NICU; therapists also felt that they did not have the adequate skills and knowledge to work in the stressful NICU environment.
As EBP expands, studies indicate that results from research are not implemented into the occupational therapy scope of practice22-23. The use of standardised assessments inpatient care by therapists is scarce24, with many occupational therapy interventions not being evidence-based. Therapists display decreased skills, knowledge, and confidence to apply scientific evidence into their daily practice. Therapists generally have a negative perception of research and receive inadequate administration assistance in their work areas, thus less time to engage with scientific evidence23,25.
Studies have shown that EBP allowed for minimum exploration in clinical practice whilst others viewed EBP as a positive when utilised simultaneously with current occupational therapy clinical practices26. Therapist recognised years of experience in clinical practice as a critical part of their knowledge, decision-making abilities, skills and evidence in everyday practice25-26. Many therapists engaged with senior therapists or colleagues who have more experience in the field, attended journal clubs and referred to textbooks27. Therapists who have had postgraduate training display confidence in clinical practice and utilise research findings inpatient interventions. These outcomes are aligned with research in the field of KT. It is suggested that KT interventions include cognitive learning theories to allow therapists to develop their knowledge in EBP and detect gaps in their clinical knowledge28. Studies investigating the effectiveness of KT interventions in occupational therapy have found that focusing on inhibitors that prevent EBP may show positive results in increasing knowledge, self-worth and changing clinical practice behaviours7. A crucial step suggested in studies producing KT interventions for occupational therapists is to be aware of the inhibitors and enablers of the clinician and the clinical context. Four concepts have been identified to evaluate the success of KT interventions in influencing changes in clinical practice namely; the elements that the intervention consists of, the personal attributes of the therapist, aspects of the conduct that the KT intervention is attempting to modify, and features of the health context in which the therapist practices29. KT interventions need to correspond with a therapists clinical context, preferred learning methods and personality traits30. Generally, occupational therapists believe that EBP includes research and clinical experience and designing patient-specific interventions26. The results and continuous evaluation of KT in occupational therapy need exploration to enhance knowledge and skills in using EBP in clinical settings.
MATERIAL AND METHODS
This study is reported according to the Consolidated Criteria for Reporting Qualitative Research (COREQ)31.
Methodological Orientation and Theory
This research formed part of a larger study aiming to identify and bridge the knowledge-to-practice gaps with rehabilitation therapists who work with high-risk infants in the public health sector of South Africa32. This particular study was a qualitative exploration of occupational therapists' experiences in the public health sector of KZN who share similar ethnography or characteristics, guided by an appreciative inquiry (AI) approach33 and KT process28.
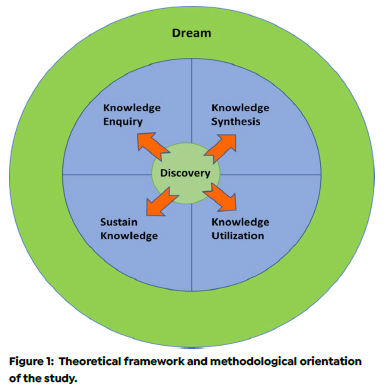
AI encompasses four phases: discovery, dream, design, and destiny33. The first two phases of the AI approach were used and aligned with KT principles, such as knowledge inquiry, knowledge synthesis, sustaining knowledge, and knowledge utilisation in the care of the high-risk infant31. This promoted a discussion amongst occupational therapists about how they acquire knowledge to intervene in the NICU/high care units, support the high-risk infant, and synthesise and sustain the information they source, utilise, and adapt to their contextual needs (Figure 1 page 77).
Recruitment and Sampling
Using purposive non-probability sampling33, 17 participants were recruited into the study. Informed consent and demographic information forms were sent to potential participants who were informed on voluntary participation and confidentiality. Therapists had to meet criteria that included permanent employment for more than two years and having worked with neonates and high-risk infants in various levels of care in public health institutions across the province of KZN SA.
Sample Demographics
Of the 17 participants, 70.6% (n=12) completed their undergraduate training at the same institution. The majority were female (94%; n=16) and had up to ten years of experience (70,6%; n=12). The practice setting involved therapists mainly from the district level (59%; n=10), with a large percentage having had prior neonatal training (65%; n=11) (Table I page 76 refers).
Setting
Upon the South African government's decision to initiate a nationwide lockdown due to the Coronavirus (COVID 19) pandemic globally, alternate methods for qualitative data collection due to social distancing guidelines were sought33. Two focus groups via the online platform ZOOM were used to collect data in this study. Each focus group spanned 90 minutes. Participants represented six of the ten districts in the province of KZN, SA. There was no other presence involved in data collection besides the research team (three of the authors) as facilitator/co-facilitator/moderator of the discussion, and the participants.
Focus Group Schedule
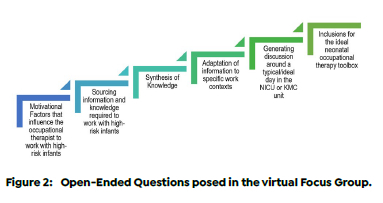
The initial questions for the discussion schedule were reviewed and refined with the research team with knowledge and experience in knowledge translation and or neonatal care. The questions were refined within a theoretical framework to focus on occupational therapists that worked with high-risk infants supported by evidence found in literature and from the team's clinical experiences. (Figure 2 above).
Pilot Study
A pilot study with two community service occupational therapists was conducted. Refinement in the presentation style of the questions and how the discussions would be facilitated were acknowledged by the team. The primary issue identified was internet connectivity and the background noise from the participant's video calls.
Main Study
The sessions were conducted in English. Discussions were recorded via the audio recorder available on ZOOM. The facilitators made memos during the session. This assisted with a preliminary analysis of possible themes that could emerge from the data. Each focus group spanned 90 minutes. Data saturation were reached once no new themes could emerge from the data; therefore, further coding was not feasible34. Transcripts were returned to participants for comment. Two authors listened to the audio recordings prior to the transcripts being available. Transcripts were also checked and rechecked against the audio recordings to ensure credibility35.
Data Analysis
The transcribed data were imported into NVivo (version 12 Pro), for the organisation. The data were analysed separately and repeatedly to identify initial coding using thematic analysis36. Word trees and thematic maps were generated on NVivo. A hybrid approach that included a shared data-driven inductive deductive method was utilised to demonstrate rigour in the thematic analysis37. This approach to analysing the data complemented the instrument questions by allowing the principle of KT and occupational therapy in the care of the high-risk infant to be fundamental in deductive reasoning whilst still letting themes emerge from the data using inductive reasoning37. Documenting of evidence through this approach displayed credibility, validity and trustworthiness in the research method38. The coding process involved the reduction of data into initial themes. These were later categorised into themes and sub-themes (16 codes and seven subcodes), and the relevant verbatim responses were highlighted to support the findings. The final stages of the data analysis included grouping the possible themes and sub-themes identified from the initial coding36. Emergent themes were reduced to five core themes based on the objectives of the study.
Ethical Considerations
TheBiomedical Research Ethics Committee (BREC/00001886/2020) and the DOH Research and Knowledge Management Directorate (NHRD Ref. KZ_202008_066) issued ethical approval for the study.
Trustworthiness, reliability, credibility, and dependability
Triangulation can be described as using numerous data sources, models, and methodology to provide valuable information to a study35. Triangulation occurred by peer debriefing the coded data from the transcripts and, eventually, the emergent themes to ensure dependability, reliability, trustworthiness, and counter researcher insider bias. This also allowed for the data to be validated. Credibility was assured by the participants' views being accurately interpreted from the audio recordings. Dependability was confirmed by keeping thorough data collection and analysis records (audit trail).
RESULTS
Five core themes with relevant sub-themes, shown in Figure 3 (above) emerged from the data and are augmented by verbatim responses.

THEME 1: Occupational therapy and neonatal care in the public health sector
Facilitators in working with high-risk infants
Participants believe that the doctors who work in paediatrics at their facilities acknowledge the role and benefit of occupational therapy intervention, Early Childhood Intervention (ECI), and neonatal care. They perceive some facilities' management as a facilitator in supporting the occupational therapy role in providing intervention to high-risk infants. The facility management also supports follow-up programmes once the infant and mother are discharged. This allows management to identify the implementation of occupational therapy programmes and increases recognition of the occupational therapy role in ECI.
"An enabler is definitely your management where you show how well your program can run and if you feed from one programme into the next programme and you're getting early childhood disability on top of it then that's an enabling factor." (OT1, 10-15 years clinical experience, training in paediatric NDT)
Inhibitors in working with high-risk infants
It is perceived that health facilities in KZN are a common inhibitor in providing quality interventions to high-risk infants. They do not fund training for therapists to improve and expand their knowledge and skills. Paying for training on a personal capacity is not always affordable, as courses and workshops are costly.
"Money is the big disabler, the fact that they don't fund training." (OT1, 10-15 years clinical experience, training in paediatric NDT)
Once an infant is discharged, the parent does not always comply with their follow-up appointment dates with the facility's high-risk baby clinic programmes. Follow-up appointments usually monitor the infant's medical, feeding, and overall development up to two to three years of age - this varies at different facilities. Participants identified that locating patients who default when the programme is extensive; there are time limitations and insufficient occupational therapy staffing at most public health facilities in KZN. Staffing numbers in rehabilitation have decreased since the moratorium was placed on posts in the KZN public health sector in 2016. This has led to many smaller departments being managed solely by junior therapists. Other departments in more resourced facilities struggle to provide full-time occupational therapy services in wards that consistently require assistance. An inhibitor described included not having adequate staffing to have an occupational therapist providing full-time services in the NICU.
"Some of our disablers is that we don't have enough staff to be able to work in neonatal ICU and ideally, we'd have an occupational therapist working full time there." (OT4, >15 years clinical experience, no additional training).
Furthermore, participants believe they were not provided with enough knowledge and skills to work with high-risk infants during their undergraduate training. Therapists' self-learnt skills and appropriate interventions to support high-risk infants through their daily clinical experiences.
"I think one of the barriers we have as new therapists, we weren't really trained in neonatal care on campus, and you go into this new hospital, and you have to learn as you go along." (OT2, >15 years clinical experience and training in Little Steps)
Interest in paediatrics and neonatal occupational therapy practice
Once therapists are placed at various facilities to complete their community service, they are likely required to provide intervention to paediatrics in all spheres. Occupational therapists who work in paediatrics generally have an interest and passion for working with infants and children.
"Initially it was that I never had any exposure to working with neonates as a student or during varsity but once I did comm serve and started working in the department of health, obviously we got referrals for babies from the nursery and neonatal ICU, and I'm really interested in it." (OT5, 5-10 years clinical experience, training in Little Steps and NDT advanced baby course).
Further training, courses, and workshops focusing on ECI and neonatal care increases interest in the field, as occupational therapists feel more confident and equipped to provide therapy to high-risk infants or children. The therapist's interest in neonatal care is sustained by clinical experience, monitoring infant development if ECI is initiated, compared to an infant who had not received any intervention and therefore had poor functional outcomes.
"It's been a combination of seeing the outcomes later in life and just knowing if you worked backwards, they could've introduced access care a lot earlier in the system and then through experience having worked with them early on and seeing the impact that an intervention can make reinforced for me why it is so essential to get into that field and the importance of early intervention." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
Referral system to occupational therapy as part of protocol and policy
Most health facilities in KZN develop independent standard operating procedures (SOP) regarding paediatric referral protocols and policies to other disciplines. Occupational therapists at some facilities only assess and provide intervention to patients when the MDT refers them. Participants do not blanket cover wards due to inadequate staffing and compliance with the SOP of the facility. Some participants indicated that working with high-risk infants is not a choice of interest. They provide assessment and intervention in the NICU only upon referrals received from the doctors.
"I don't think we're drawn to do it; I think it's a matter of the referrals that we get from the doctors and then we just do the treatment as per requirements or as we see necessary." (OT8, 5-10 years clinical experience, training in Little Steps, WHO Infant and Young Child Feeding, Infant Sensory Integration Training).
THEME 2: Knowledge Acquisition and Knowledge Synthesis
Acquiring knowledge from the multi-disciplinary team Therapists acquire knowledge to support the high-risk infant through doctors, specialist paediatricians, neonatologists and nurses to develop integrated intervention strategies to help the high-risk infant and parent. Healthy relationships are formed between clinicians with knowledge brokerage being implemented as they learn and share the expertise of their roles in support of the infant and the family. Participants view the nursing staff in the NICU as an essential role player in understanding the occupational therapy scope of practice in the care of the high-risk infant. Therapists generally rely on nursing staff in reminding doctors to refer to occupational therapy. MDT ward rounds in the NICU, also promote knowledge brokerage amongst the various disciplines. The MDT have internal communication channels, where they share information or refer patients to each other.
"The other source comes to think of it is colleagues, we have had the most amazing paediatricians and neonatologists that we got to work with, both South African and international and having that shared sort of think tank where you're working with a dietician, in combination with a paediatrician, with a neonatologist and an OT, and you're getting all together and you're starting to think about intervention strategies and everyone starts sharing expertise from their fields, we developed a strong multi-disciplinary team and we got to learn from each other which was great." (OT7, 10-15 years clinical experience, training in introductory workshop on high risk babies).
Sourcing information to support occupational therapy neonatal practice
Participants use the infant's clinic book (Road to Health booklet) to educate parents on the developmental milestones that the infant should achieve. The book contains simple illustrations. This makes it user friendly for mothers that are literate or illiterate.
"The patient road to health card, road to health booklet gives us a lot on the developmental milestones." (OT11, 2-5 years clinical experience, no further training).
Therapist's use the information provided in the paediatric assessment forms during the infant's admission. This helps understand the infant from a medical and rehabilitation perspective as information is sourced from an MDT perspective. Besides sourcing information from the infant's admission records and booklets, data is sourced through interviews with the family. Comprehensive referral forms that occupational therapy departments in various facilities have individually created also help gather information about the infant from the treating doctor.
"We source our info from just being able to work in the NICU, from the patient record, so the patient file, the interview with the mom or dad or the parents, from the referral letter, we have a request for consult that the doctor has to fill." (OT11, 2-5 years clinical experience, no further training).
Acquiring information, knowledge and skills from multiple sources
Participants acquire information, knowledge and skills from textbooks available in their departments on neonates. Colleagues with experience was the main point that participants identified in developing knowledge and skills in the care of the high-risk infant and to guide them in making use of the correct information, advising on complex cases and treatment modalities.
"It's just having access to speak to colleagues that have more experience, so when I first started out obviously being able to speak to people that that had more experience in the NICU." (OT5, 5-10 years' experience, training in Little Steps and NDT advanced baby course)
Therapist's also acquired information from policies implemented by the KZN Department of Health (DOH). This comprehensive policy is a checklist that the nurses who work in the NICU complete. This assists in identifying and providing information on an infant that is or has the potential of being classified as high risk.
"With the new policy that's come into neonatal to try lower litigation against the department of health, there's that checklist that the nurses have to fill in and if you go through the checklist, a lot of the factors that we have had on our form are now also on that checklist. It is in our policy now and when I started there was no such thing as a neonatal check list, so there definitely are those guidelines to say if the baby isn't checking these boxes-that's a red baby, orange baby or a green baby." (OT1, 10-15 years clinical experience, training in paediatric NDT)
The Little Steps course, which focuses on NDSC for premature infants, is one of the most popular SA courses, which caters for the MDT who work with high-risk infants in the NICU. Participants identified this course to increase their confidence, knowledge, and skills working with high-risk infants and their families. The Little Steps course is not affordable to all therapists. Therefore, those who have attended the course provide in-service training to others to translate the knowledge to staff in their facilities on NDSC strategies to implement in the NICU.
"The Little Steps course which we haven't attended personally but have gotten in-service training from therapists that did it and the suggestions made for how you can work in the neonatal ICU were brilliant and we just took it back and in serviced it in our hospital and just said how can we ask the nursery to intervene." (OT9, 2-5 years' experience, training in infant massage and breastfeeding).
Academic supervisors from the University of KZN provide knowledge brokerage through offering workshops on working with high-risk infants to clinicians. Academic supervisors also educate students whilst they are at their clinical sites. This allows clinicians also to observe and learn concurrently. Therapist's keep updated neonatology by acquiring and improving knowledge by engaging with scientific evidence from published articles in journals. They use online searching to enhance their experience and understanding in classifying specific terminology used in the NICU and what factors would influence an infant's medical and functional prognosis once they are discharged.
"There's lots of really superb cutting-edge research coming out so accessing journal articles in the latest neonatal journals, there's also a lot of OT research coming out which is very exciting." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
Synthesising knowledge to work in occupational therapy neonatal practice
Participants who have two to five years of experience synthesise information that they have accessed from various sources and use it through trial and error in intervention with patients to observe what is useful and what is not. They believe that most of the knowledge and skills they develop or acquire are through their own clinical experiences and reasoning.
"I think it comes down to your clinical reasoning at the end of it, there's so much information out there, you want to use your clinical reasoning in addition to the information you gather to provide the best possible treatment." (OT9, 2-5 years' experience, training in infant massage and breastfeeding).
THEME 3: Knowledge Translation/Utilisation
The inhibitors and facilitators in sustaining knowledge
Therapists attribute doctors in smaller facilities as inhibitors in maintaining knowledge in neonatal care. This is due to them rotating frequently and not prioritising rehabilitation with high-risk infants. Therefore, they do not refer infants for therapy.
"From my experiences in district hospitals I find it more difficult to get buy in from medical staff. You know doctors are rotating the whole time and you're trying to play catch up and their doctor meetings are not- the focus on rehab and intervention is not as strong." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
Participants believe that scheduling occupational therapy in in-service medical rosters and providing consistent in-service training to educate doctors and nurses on the occupational therapist's role in the care of the high-risk infant, on the occupational therapy referral process and what programmes are offered at the facility and on discharge, act as a facilitator in sustaining knowledge in facilities. In-service training may help build a trusting relationship with the occupational therapy department and accept occupational therapy as a valuable member of the MDT. They also believe that getting the medical manager on board may help sustain knowledge transfer of the occupational therapist's role in the care of the high-risk infant amongst the paediatric medical team.
"We did in-service training with our nurses on how to implement some of the care practices, we also did in-service training with every single intern-medical-intern that was coming through, so that everyone in the team is aware of how to implement your therapeutic approaches so it's not just therapy and it becomes the base standard the entire system runs on." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
Therapists believe that another facilitator in sustaining knowledge of the occupational therapist's role in neonatal intervention uses scientific evidence to prove to hospital management that occupational therapy interventions may assist the facility in decreasing expenses. They perceive the parent role in the NICU as essential in sustaining knowledge in the high-risk infant's care. Participants educate the parent individually or in groups and adapt the intervention to the infant and parent dyad's specific needs.
"So, another thing that was done was a lot of work with the parents one-on-one as well as in groups and then seeing how you can adapt your care approach specifically to the parents' needs and how is that best going to achieve a dyadic approach in that moment, how best you're going to get the child and parent to work together." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
THEME 4: Contextual barriers and adaptation
Adapting to the contextual needs of the facility and community
Participants engage with their past and present knowledge and experiences and combine them with scientific evidence to develop and adjust intervention strategies to their specific contexts. They indicated that most research in neonatology comes from first world countries and may not suit the SA context.
"You also need to consider the resources at your institution because a lot of the research that comes out is from first world countries, and we don't always have those kinds of resources. So, it's always nice to see what they are using and try to think out the box and how we can use a similar sort of idea to get the same result." (OT9, 2-5 years' experience, training in infant massage and breastfeeding).
They have developed language-appropriate education pamphlets for parents and caregivers at their facilities. Participants employed at tertiary institutions prioritise what information should be given to a parent or caregiver as they are not admitted for long periods. They believe that selecting the most applicable information to the parent comes with experience.
"Because we're tertiary and we not retaining these kids for a long period, kind of being able to prioritise what you hand over to the caregiver and that comes with a bit of practice as well because you want to help the mom as much as you can and give them as much but sometimes, I find that less is more." (OT6, 5-10 years clinical experience, introductory workshop to at risk infants).
Poor Referrals from the MDT
Therapists indicate that although doctors rotate at the smaller hospitals every few months, some do not acknowledge or understand the occupational therapy role in neonatal care even if there is a continuous in-service training programme.
"I think the doctors that we work with do rotate, but most of the time they are there for like 2/3 months, so depending on the doctors...some of the doctors don't really work close with rehab at all. You trying to inform them maybe that this is what OT does and this is how we can actually play a role they still for whatever reason generally don't refer." (OT13, 5-10 years clinical experience and introductory workshop on high risk infants)
Typical day in the NICU, high care and Kangaroo Mothercare units
Participants describe an average day in the NICU as busy, short and chaotic due to working around the infant's sleep and wake states or the parent not always being present. Participants feel that the NICU and Kangaroo Mother Care (KMC) environments are supportive. There is continuous training amongst staff and parents daily, in classes, groups and individual education.
"I think short and chaotic summarises it for me, you go in there and this baby is sleeping and the other one is deep quiet sleep, and you can't interact with that one and you move to the next one but mom is showering and then you're here and then you're there, so it often felt quite chaotic." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
"It is usually quite busy in the morning, but it is a nice environment for me to work in because the team is very supportive and there's a lot of training that goes on and it's constant." (OT1, 10-15 years clinical experience, training in paediatric NDT)
THEME 5: The ideal occupational therapist and neonatal setting
The ideal occupational therapist in neonatal practice
Therapists believe that the ideal occupational therapist must be a confident person knowledgeable in neonatal care. She must also have an assertive personality to engage with the MDT to facilitate change. They also indicate that if the undergraduate training for working with high-risk infants was comprehensive, occupational therapists may feel more equipped to work in the NICU.
"I think if we had a richer training system that would contribute more into having decent therapists. I think the other thing is passionate therapist, someone who is interested in it; you don't want someone who is halfhearted in the NICU, it's very emotionally intense work, it's very draining work so I think you need someone with gentleness with an equal thick skin. I think someone who can work as well with your neonates as well as your parents, a lot of communication skills with your staff." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
Participants also describe the ideal occupational therapy as being patient, compassionate and educated in the field of neonatal care. They do not believe that a junior therapist should work in the NICU. Participants view work in the NICU as a 'specialised" field of practice in occupational therapy, and the therapist working there should have adequate training and experience to make them feel confident.
"I think a very patient, compassionate and an educated person in that field. I don't think your comm serve is the person that should be in that space. The person must be trained, neonatal ICU in my view is a specialised field and I don't think that comm serves can actually work there because if you are starting, you need first to understand the environment you are working in." (OT4, >15 years clinical experience, no additional training)
The ideal day in occupational therapy practice in the NICU
The ideal day for an occupational therapist working in the NICU was described as: having a good working relationship amongst the MDT and having the time and flexibility to structure your workday.
"I think the ideal day would include proper team connection, as well as just the time to be flexible and fluid in who you see and when." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
The ideal toolbox for the occupational therapist in neonatal practice
Therapists envision the ideal toolbox to include protocols for occupational therapists working in the NICU based on scientific evidence for various diagnoses. Participants think it should consist of standardised SA assessment tools applicable to the country's context and population group. They believe that this assessment's data can be utilised to develop research within the South African context in occupational therapy and neonatal care. They would like the ideal toolbox to have a room allocated solely for family and parent counselling.
"I think what I would really like in the toolbox is a South African assessment that is sensitive to our population, and we can really start using that to generate our own data and to stand our ground on an international level in terms of research." (OT7, 10-15 years clinical experience and introductory workshop on high risk babies).
Participants indicate that it is difficult for them and other occupational therapists who have not had further training in working with high-risk infants to identify what the ideal toolbox should consist of, compared to therapists who have received additional training.
"I think it's quite hard for us who haven't had further training in high-risk babies, it's hard for us to say what would be ideal whereas a person who has had that training may have a lot of things they would think would be most beneficial to kids." (OT9, 2-5 years' experience, training in infant massage and breastfeeding).
DISCUSSION
This study's findings have outlined the knowledge to practice gaps for occupational therapists supporting high-risk infants in the KZN public health sector. Doctors working in paediatrics recognise the value of occupational therapy in ECI and neonatal care in some hospitals. Hospital management acknowledges occupational therapy services once they see the benefits of early developmental care, especially with morbidity cases. Receiving support from management contributes to the successful implementation of NDSC, and may decrease the facility's expenses through shorter admissions and fewer health complications15,20. Research has identified that the early implementation of NDSC encourages high-risk infants' overall development39-40.
In several studies, it has also been recommended that high-risk infants be referred to occupational therapy to provide early intervention programmes to promote neurocognition, performance in areas of occupation, maternal mental health, and family-centred care to sustain knowledge supporting the infant and parent dyad 15,20. Inhibitors in working with neonates, including a lack of funding for training in neonatal care for occupational therapists, with training being unaffordable for many therapists correlate to a previous study, in which junior therapists stated attending neonatal courses was difficult as they were costly. In the occupational therapy profession, permanent staff shortages in the KZN DOH inhibit consistent care of high-risk infants in the NICU and strain therapists 6,41.
It was found that participants who work in paediatrics at their hospitals generally are interested in working with children and neonates. Further training in neonatal care increases a therapist's confidence and interest in the field. Studies have found that therapists with little clinical experience feel incompetent, have decreased self-confidence, engage in interventions with flawed clinical reasoning and face challenges with their skill level and what is expected of them in the work environment42-43. Participants outlined that seeing positive developmental outcomes with early intervention encouraged an interest in neonatal care. Other participants had no interest in working with neonates but followed the referral process, SOP of their facilities and the occupational therapy scope of practice to intervene only as required. This is aligned with findings from a study in which occupational therapists did not work in the NICU due to a lack of interest in neonatal care6.
Participants acquire information and knowledge from a range of professionals in the MDT. Working relationships are formed between disciplines to implement knowledge brokerage to learn and share individual roles in supporting the high-risk infant. Information is shared during in-service training, ward rounds, and internal communication channels. This is consistent with studies in which working in an MDT has been highlighted as beneficial to ensure consistency in the neonate's care 15,44-46. Information to support the infant and parent was acquired through working in the NICU and from other sources such as referral forms, admission booklets, interviews with the parent and the South African DOH Road to Health booklet, which consists of an immunisation schedule, developmental and growth monitoring as well as other health information for infants and young children. Participants' clinical knowledge and skills were acquired through textbooks, online searching, consulting with experienced colleagues, DOH nursing policies, journal articles, courses and support from the University of KZN lecturers. A lack of DOH policies for the occupational therapy role and specific practice in neonatal care could be an area for future research; this may help provide a standard of care across the KZN province.
A scoping study outlined that experienced occupational therapists used evidence-based practice (EBP) in clinical decision making, using online research, reading relevant literature, and increasing knowledge and skills by attending courses and workshops for professional development in fields of interest 7:26,47-48. The 'Little Steps' course focusing on NDSC for preterm infants was identified as the most common course attended by occupational therapists. This correlates to two other studies that have recognised the course to be helpful in the operationalisation of NDSC amongst the MDT working in the NICU6,15. The synchronisation of acquired information, knowledge and skills was considered from a therapist's own clinical experiences and practice. Experience plays a vital role in increasing the self-confidence of an occupational therapist and integrating research into practice7.
Frequent staff rotations and doctors' disinterest to refer infants to occupational therapy make it challenging to sustain neonatal services6. The focus on rehabilitation is not prioritised as medical concerns take precedence. Providing in-service training to the MDT on the occupational therapy role facilitates knowledge sustainment and optimises NDSC practices 15. EBP guidelines for NDSC come from first world countries and are adapted by professionals to the SA context 15,49. Participants adopt and adapt international guidelines according to their resources and the population they service. This may assist in relaying information to caregivers and suggesting contextually appropriate intervention methods. Some participants outlined a typical day in the NICU as a brief, chaotic, but supportive MDT environment. The ideal occupational therapy to service the NICU needs to be trained, confident, compassionate, assertive, and motivated to encourage practice change amongst the MDT. Junior therapists are not recommended to work in the NICU due to their lack of training and experience. This correlates with findings from other studies 20,42-43. An ideal day in the NICU is having positive working relationships with the MDT, time, and flexibility to provide individualised infant and family centred care. Participants envision the ideal neonatal toolbox to consist of standardised South African assessment tools and EBP protocols specific to occupational therapy whilst others felt like they could not imagine what the ideal would be, as they received no further training in neonatal care. The following stage in this study is to determine what is required in KT interventions via a consensus process50.
Limitations
The study was limited to one province in SA and only included occupational therapists in the public health sector; therefore, the findings may not outline occupational therapists' perceptions in the country as a whole or on an international level. The qualitative design and small sample size may not represent the perceptions of all occupational therapists. A response bias may have developed, as occupational therapists who had no interest or little knowledge in supporting high-risk infants did not respond to the invite for participation.
CONCLUSION
The findings demonstrate that the knowledge to practice gaps for occupational therapists employed in the public health sector of KZN are insufficient training in neonatal care due to postgraduate courses being unaffordable and not receiving funding or training from the DOH to improve knowledge and skills. A decreased interest of some occupational therapists to support high-risk infants may indicate a gap in practice. Severe staff shortages place strain on therapists as they are unable to provide consistent care in the NICU. Frequent doctor rotations and a poor understanding of the occupational therapy role in neonatal care result in infants not being referred to occupational therapy. Resources, training of occupational therapists, and SOPs relating specifically to the occupational therapy role in neonatal care in the public health sector appear to be necessary to inform a standard of care across the province of KZN.
Author Contributions
Ayesa Dawood completed this study as part of a masters study and was responsible for drafting the manuscript. Pragashnie Govender was the principal investigator of the larger study and primary supervisor of the study. Samantha York assisted in the data collection and analysis. Gina Rencken and Michael Ogunlana were co-supervisors and collaborators on the larger study. All authors contributed to critical review and revisions of the manuscript.
Acknowledgements
The authors wish to acknowledge Ms NN Khanyile for her assistance in data transcription. The authors also acknowledge author Samantha Jo York, posthumously (19932023) for her contributions to this study.
Declaration of Conflicting Interests
The authors declare that they have no competing interests.
REFERENCES
1. United Nations Children's Fund (UNICEF). Nurturing care for early childhood development: A framework for helping children survive and thrive to transform health and human potential. World Health Organization, Geneva; 2018. Available from: https://apps.who.int/iris/bitstream/handle/10665/272603/9789241514064-eng.pdf [Accessed 21 April 2020] [ Links ]
2. Aylward GP. Neurodevelopmental outcomes of infants born prematurely. Journal of Developmental & Behavioral Pediatrics. 2014; 35(6):394-407. https://doi.org/10.1097/01.dbp.0000452240.39511.d4 [ Links ]
3. Mwaniki MK, Atieno M, Lawn JE, Newton CR. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: A Systematic Review. The Lancet. 2012; 379(9814):445-52. https://doi.org/10.1016/s0140-6736(11)61577-8 [ Links ]
4. Gagliardi AR, Dobrow MJ. Identifying the conditions needed for integrated knowledge translation (ikt) in health care organisations: Qualitative interviews with researchers and research users. BMC Health Services Research. 2016; 16(1):256. https://doi.org/10.1186/s12913-016-1533-0 [ Links ]
5. Jacobs L, Casteleijn D, Lubbe W. Neurodevelopmental supportive care in South African NICUs - An essential change of attitude. World Federation of Occupational Therapists (WFOT), Johannesburg: University of the Witwatersrand; 2018. Available from: https://congress2018.wfot.org/downloads/presentations/SE77/lizelle_jacobs.pdf [Accessed: 21 April 2020] [ Links ]
6. Hardy M, Govender P, Naidoo D. Novice occupational therapist's experience of working in neonatal intensive care units in KwaZulu-Natal. South African Journal of Occupational Therapy. 2021; 51(1):27-35. https://doi.org/10.17159/2310-3833/2021/vol51n1a5 [ Links ]
7. Thomas A, Law M. Research utilisation and evidence-based practice in occupational therapy: A scoping study. American Journal of Occupational Therapy. 2013;67(4):e55-e65. https://doi.org/10.5014/ajot.2013.006395 [ Links ]
8. Hockenberry MJ, Wilson D. Wong's nursing care of infants and children-e-book: Elsevier Health Sciences; 2018. https://doi.org/10.1097/00001163-199110000-00015 [ Links ]
9. Nightlinger K. Developmentally supportive care in the neonatal intensive care unit: An occupational therapist's role. Neonatal Network. 2011; 30(4):243-8. https://doi.org/10.1891/0730-0832.30.4.243 [ Links ]
10. Royal College of Occupational Therapists. Occupational Therapy in Neonatal Services and Early Intervention. Practice Guideline. 2017:1-52. Available from: https://www.rcot.co.uk/practice-resources/rcot-publications/downloads/neonatal-services [Accessed: 25 April 2020]. [ Links ]
11. Craig JW, Smith CR. Risk-adjusted/neuroprotective care services in the NICU The elemental role of the neonatal therapist (OT, PT, SLP). Journal of Perinatology. 2020; 40(4):549-59. https://doi.org/10.1038/s41372-020-0597-1 [ Links ]
12. Sherry K. Disability and Rehabilitation: Essential considerations for equitable, accessible and poverty-reducing health care in South Africa. South African Health Review. 2014; 2014(1):89-99. [ Links ]
13. Hoque M, Haaq S, Islam R. Causes of neonatal admissions and deaths at a rural hospital in KwaZulu-Natal, South Africa. Southern African Journal of Epidemiology and Infection. 2011; 26(1):26-9. https://doi.org/10.1080/10158782.2011.11441416 [ Links ]
14. Robinson JE. Access to employment for people with disabilities: Findings of a consumer-led project. Disability and Rehabilitation. 2000; 22(5):246-53. https://doi.org/10.1080/096382800296818 [ Links ]
15. Lubbe W. Best practice guidelines for neurodevelopmental supportive care of the preterm infant: North-West University; 2010. Available from: http://repository.nwu.ac.za/bitstream/handle/10394/3656/Lubbe_Welma.pdf?sequence=3&isAllowed=y [Accessed: 18 May 2020]. [ Links ]
16. Graven SN. Sound and the developing infant in the NICU: Conclusions and recommendations for care. Journal of Perinatology. 2000; 20(1):S88-S93. https://doi.org/10.1038/sj.jp.7200444 [ Links ]
17. Lloyd LG, De Witt T. Neonatal mortality in South Africa: How are we doing and can we do better? South African Medical Journal. 2013; 103(8):518-9. https://doi.org/10.7196/samj.7200 [ Links ]
18. Lubbe W, Van der Walt CS, Klopper HC. Integrative literature review defining evidence-based neurodevelopmental supportive care of the preterm infant. The Journal of Perinatal & Neonatal Nursing. 2012; 26(3):251-9. https://doi.org/10.1097/jpn.0b013e3182650b7e [ Links ]
19. Hinchliffe SR, Seaton SE, Lambert PC, Draper ES, Field DJ, Manktelow BN. Modelling time to death or discharge in neonatal care: An application of competing risks. Paediatric and Perinatal Epidemiology. 2013; 27(4):426-33. https://doi.org/10.1111/ppe.12053 [ Links ]
20. Butler ML. The self-reported perceptions of the multi-disciplinary team regarding standards of neurodevelopmental supportive care in the neonatal intensive care unit; 2018. Available from: https://wiredspace.wits.ac.za/bitstream/handle/10539/25338/ML%20BUTLER%20(MSC.%20OT)-%20THE%20SELF-REPORTED%20PERCEPTIONS%20OF%20THE%20MULTI-DISCIPLINARY%20TEAM%20REGARDING%20STANDARDS%20OF%20NEURODEVELOPMENTAL%20SUPPORTIVE%20CARE%20IN%20THE%20NEONATAL%20INTENSIVE%20CARE%20UNIT.pdf?sequence=1 [Accessed: 15 February 2022] [ Links ]
21. KwaZulu-Natal OT Forum. Annual provincial report Pietermaritzburg; Greys Hospital. 2019. [ Links ]
22. Cameron KAV, Ballantyne S, Kulbitsky A, Margolis-Gal M, Daugherty T, Ludwig F. Utilization of evidence-based practice by registered occupational therapists. Occupational Therapy International. 2005; 12(3):123-36. https://doi.org/10.1002/oti.1 [ Links ]
23. Korner-Bitensky N, Wood-Dauphinee S, Teasell R, Desrosiers J, Malouin F, Thomas A, et al. Best versus actual practices in stroke rehabilitation: Results of the Canadian National Survey: 57. Stroke. 2006; 37(2) https://doi.org/10.1016/j.apmr.2007.01.005 [ Links ]
24. Chard G. Adopting the assessment of motor and process skills into practice: Therapists' voices. British Journal of Occupational Therapy. 2006; 69(2):50-7. https://doi.org/10.1177/030802260606900202 [ Links ]
25. Bennett S, Tooth L, McKenna K, Rodger S, Strong J, Ziviani J, et al. Perceptions of evidence-based practice: A survey of Australian Occupational Therapists. Australian Occupational Therapy Journal. 2003; 50(1):13-22. https://doi.org/10.1046/j.1440-1630.2003.00341.x [ Links ]
26. Copley JA, Turpin MJ, King TL. Information used by an expert paediatric occupational therapist when making clinical decisions. Canadian Journal of Occupational Therapy. 2010; 77(4):249-56. https://doi.org/10.2182/cjot.2010.77.4.7 [ Links ]
27. Lyons C, Casey J, Brown T, Tseng M, McDonald R. Research knowledge, attitudes, practices and barriers among paediatric occupational therapists in the United Kingdom. British Journal of Occupational Therapy. 2010; 73(5):20 0-9. https://doi.org/10.4276/030802210x12734991664147 [ Links ]
28. Petzold A, Korner-Bitensky N, Salbach NM, Ahmed S, Menon A, Ogourtsova T. Increasing knowledge of best practices for occupational therapists treating post-stroke unilateral spatial neglect: Results of a knowledge-translation intervention study. Journal of Rehabilitation Medicine. 2012; 44(2):118-24. https://doi.org/10.2340/16501977-0910 [ Links ]
29. Menon A, Korner-Bitensky N, Kastner M, McKibbon K, Straus S. Strategies for rehabilitation professionals to move evidence-based knowledge into practice: A systematic review. Journal of Rehabilitation Medicine. 2009; 41(13):1024-32. https://doi.org/10.2340/16501977-0451 [ Links ]
30. Green L, Gorenflo DW, Wyszewianski L. Validating an instrument for selecting interventions to change physician practice patterns. J Fam Pract. 2002; 51(11):938-42. [ Links ]
31. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. 2007; 19(6):349-57. https://doi.org/10.1093/intqhc/mzm042 [ Links ]
32. Govender P. Identifying and bridging the knowledge-to-practice gaps in rehabilitation professionals working with at-risk infants in the public health sector of South Africa: A multimethod study protocol. BMJ Open. 2021; 11(5):e039242. https://doi:10.1136/bmjopen-2020-039242 [ Links ]
33. Ludema JD, Cooperrider DL, Barrett FJ. Appreciative inquiry: The power of the unconditional positive question. Handbook of Action Research. 2006:155-65. [ Links ]
34. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006; 18(1):59-82. https://doi.org/10.1177/1525822x05279903 [ Links ]
35. Creswell JW, Creswell JD. Research design: Qualitative, quantitative, and mixed methods approaches: Sage Publications; 2017. [ Links ]
36. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006; 3(2):77-101. https://doi.org/10.1191/1478088706qp063oa [ Links ]
37. Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods. 2006; 5(1):80-92. https://doi.org/10.1177/160940690600500107 [ Links ]
38. Koch T. Establishing rigour in qualitative research: The decision trail. Journal of Advanced Nursing. 1994; 19(5):976-86. https://doi.org/10.1111/j.1365-2648.1994.tb01177.x [ Links ]
39. Wallin L, Eriksson M. Newborn individual development care and assessment program (NIDCAP): A systematic review of the literature. Worldviews on Evidence-Based Nursing. 2009; 6(2):54-69. https://doi.org/10.1111/j.1741-6787.2009.00150.x [ Links ]
40. Legendre V, Burtner PA, Martinez KL, Crowe TK. The evolving practice of developmental care in the neonatal unit: A systematic review. Physical & Occupational Therapy in Pediatrics. 2011; 31(3):315-38. https://doi.org/10.3109/01942638.2011.556697 [ Links ]
41. Shung-King M, Lake L, Sanders D, Hendricks Me. Child, and adolescent health: Leave no one behind. Cape Town: Children's Institute: University of Cape Town, 2019. https://doi.org/10.7196/sajch.2020.v14i4.01853 [ Links ]
42. Hodgetts S, Hollis V, Triska O, Dennis S, Madill H, Taylor E. Occupational therapy students' and graduates' satisfaction with professional education and preparedness for practice. Canadian Journal of Occupational Therapy. 2007; 74(3):148-60. https://doi.org/10.1177/000841740707400303 [ Links ]
43. Robertson DM. Critical thinking and clinical reasoning in new graduate occupational therapists: A phenomenological study. 2012. [ Links ]
44. Müller M, Myburgh A, Stock R. The training and role of occupational therapists in South African neonatal intensive care units. [Unpublished]. University of the Witwatersrand Faculty of Health Sciences, School of Therapeutic Sciences: Johannesburg; 2016 [ Links ]
45. van Wyk H, de Beer M. Inter-professional education: Healthcare students' experiences. South African Journal of Occupational Therapy. 2017; 47(2):35-40. https://doi.org/10.17159/231-3833/1017/v47n2a6 [ Links ]
46. King G, Strachan D, Tucker M, Duwyn B, Desserud S, Shillington M. The application of a transdisciplinary model for early intervention services. Infants & Young Children. 2009; 22(3):211-23. https://doi.org/10.1097/iyc.0b013e3181abe1c3 [ Links ]
47. Vachon B, Durand MJ, LeBlanc J. Using reflective learning to improve the impact of continuing education in the context of work rehabilitation. Advances in Health Sciences Education. 2010; 15(3):329-48. https://doi.org/10.1007/s10459-009-9200-4 [ Links ]
48. Sharoff L. Integrating Youtube into the Nursing Curriculum. The Online Journal of Issues in Nursing. 2011; 16(3):1-6. [ Links ]
49. Als H, Lester BM, Tronick EZ, Brazelton TB. Toward a research instrument for the assessment of preterm infants' behavior (APIB). Theory and Research in Behavioral Pediatrics: Springer; 1982. p. 35-132. https://doi.org/10.1007/978-1-4899-0442-3_2 [ Links ]
50. York SJ, Rencken G, Ogunlana MO, Dawood A, Govender P. Expert opinions on knowledge-translation interventions for occupational therapists working with neonates in South Africa: A delphi study. Health SA Gesondheid. 2022. 27-10. https://doi:10.4102/hsag.v27i0.1724 [ Links ]
 Correspondence:
Correspondence:
Pragashnie Govender
naidoopg@ukzn.ac.za
Received: September 2021
Peer review: March2022
Revised: May 2022
Accepted: September 2022
Published: August 2023
Editor: Janine van der Linde: https://orcid.org/0000-0003-1067-9494
Funding: The principal investigator, Pragashnie Govender, of the larger study, from which this knowledge claim emanates, received support from the National Research Foundation (NRF) of South Africa via the Research Development Grants for Y-Rated Researchers Funding instrument, Grant Number 120400 (Reference: CSRP190423432325).














