Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.53 n.1 Pretoria Apr. 2023
http://dx.doi.org/10.17159/2310-3833/2023/vol53n1a10
RESEARCH ARTICLE
Barriers experienced by stroke survivors when participating in meaningful occupations in a rural and semirural community
Refilwe MohotlhoaneI, II; Mashudu Norman NemakangaI, II
IDepartment of Occupational Therapy, University of Pretoria, South Africa. Refilwe Mohotlhoane: https://orcid.org/0000-0003-4521-5374; Mashudu Norman Nemakanga: https://orcid.org/0000-00001-6027-5477;
IIOccupational Therapy Department, Sefako Makgatho Health Sciences University, Ga-Rankuwa, South Africa
ABSTRACT
INTRODUCTION: There are various personal and environmental factors that hinder the stroke survivors' participation in meaningful occupations within a rural and semi-rural community context. Thus, occupational therapists need to consider such barriers in order to provide holistic treatment
AIM: This study intended to explore the barriers experienced by stroke survivors on their participation in meaningful occupations in a rural and semi-rural community
METHOD: An explorative qualitative study was conducted, using a purposive sampling method to recruit participants at a public healthcare district hospital. Data were collected at the participants' homes using individual semi-structured interviews. The researcher made use of open-ended questions guided by the Occupational Therapy Practice Framework 3rd edition and the Person Environment Occupation Performance model
FINDINGS: Four themes related to the barriers experienced by stroke survivors on their participation in meaningful occupations emerged: (i) physical barriers, (i) psychological barriers, (iii) financial and (iv) environmental barriers
CONCLUSION: The barriers explored in this study compelled the stroke survivors to accept varying degrees of assistance from their caregivers. The findings of this study could assist occupational therapists to consider the factors that hinder the stroke survivors' participation in meaningful occupations in rural and semi-rural South African communities, and inform treatment aims that are relevant to the respective communities. If occupational therapists consider these barriers when planning treatment, this could assist with maximizing independence in all areas of stroke survivors' lives, lessening the burden of care on their caregivers and decreasing the patient load on clinical and community occupational therapists
Implications for practice
Stroke survivors dwelling in the semi-rural and rural community contexts experience barriers which are unique to such settings. Thus, occupational therapist should be aware of the differences of barriers experienced not only in the hospital setting, but in the community context that stroke survivors are reintegrated to. Such consideration could contribute to intervention focussed on the individual's specific needs with regard to participation in meaningful occupations within the semi-rural and rural contexts they reside in.
Keywords: Occupational Therapy Practice Framework, Person Environment Occupation Performance model, burden of care, patient load, informed intervention
INTRODUCTION
Stroke is considered to be second leading cause of death and disability globally1. Whitehead & Baalbergen2 estimated that the global number of stroke survivors will continue to increase to approximately 70 million by the year 2030. In South Africa (SA), a total of 564 000 people are living with a certain degree of disability as a result of a stroke2.
Occupational therapists are most concerned with the result of participation in meaningful occupations after stroke. Amongst other roles, occupational therapists provide holistic treatment by exploring personal and environmental factors that hinder participation in meaningful occupations, and make necessary adaptations according to the stroke survivors needs in order to enhance participation in occupations. This study explored the barriers experienced by stroke survivors on their participation in meaningful occupations in a rural and semi-rural community in South Africa.
LITERATURE REVIEW
The study focused on the personal and environmental factors that hindered the stroke survivors' participation in meaningful occupations. These factors were investigated using the Person Environment Occupation Performance (PEOP) model3. The PEOP model emphasises the challenges related to residual symptoms of stroke that may be caused by the relationship between the community-based stroke survivor and their environment, rather than by the condition itself3. The model takes into consideration the person (intrinsic factors) and environment (extrinsic factors) which may interfere with or hinder the stroke survivors' participation in meaningful occupations.
Person factors associated with barriers of stroke survivors when participating in meaningful occupations in the community
Physiological and Neurobehavioral factors
A study conducted in rural China4 highlighted that muscle tone and muscular endurance were reported as physiological barriers for stroke survivors when participating in meaningful occupations. The findings of the study revealed that physiological factors appeared to have significant impact on their participation. Subsequently, the stroke survivors had to take frequent rest breaks as a result of experiencing fatigue and as such, needed more assistance from their caregivers. These physiological factors are as a result of the impaired neuro-behavioral factors such as decreased active movement on the affected side, pain, poor balance, and incoordination3,5. However, findings from research performed in Rwanda and Johannesburg6-11 identified restricted mobility and pain as the main neurobehavioral barriers that affect aspects of the stroke survivors' lives and their ability to participate in meaningful occupations. Additionally, Braaten et al.12 revealed that fatigue was more prevalent in the subacute phase of stroke recovery.
Psychological factors
Walsh8 highlighted the concerns of stroke survivors about being a burden on their family members as they required assistance in order to participate in meaningful occupations. He reported that a sense of satisfaction arose from being given tasks to do for their families, as this increased their sense of personal causation. The participants from the study also expressed concerns about their families offering too much support and feelings of a decreased sense of capacity, or too little support which resulted in feelings of loneliness, neglect and stigma. Common emotions that have been identified by literature as barriers to participation in meaningful occupations, include feelings of loneliness, sadness, fear, anxiety, frustration, decreased self-esteem and feeling useless7-8,13. All of these emotional factors impaired the stroke survivors' participation regardless of the level of disability resulting from the stroke. This has been linked with episodes of depression as they felt like they had lost valuable roles within their families as well as autonomy7,13-14.
Environmental factors associated with barriers of stroke survivors when participating in meaningful occupations in the community
Social support
Previous studies8,15-17 revealed that participants interpreted too much support from their immediate family as a barrier as it reinforced dependency behaviour for instance, when families provide assistance to stroke survivor capable of engaging in activities independently. Additionally, too much support did not afford the stroke survivors an opportunity to become independent when participating in meaningful occupations.
Restricted mobility was also identified as a primary factor that caused secondary barriers in receiving social support 6. This came with being either confined to a wheelchair or not being able to walk independently. As a result, it became difficult for the stroke survivors to visit friends and family. It also became challenging for them to attend social gatherings such as wedding and birthday celebrations, where participation in such social activities enabled them to receive social support. However, due to restrictions in mobility, the stroke survivors reported that they had to wait and see if friends or family members would visit them, which led to them feeling isolated and confined to their homes18.
Participants in studies conducted in South Africa and China identified a lack of support from friends as a barrier, since they no longer visited to check on them, nor went out with them11,18. The results of another study discovered that the stroke survivors' friends considered going out with them to be physically taxing as they had to provide physical assistance particularly if they had restricted mobility19 .Furthermore, the stroke survivors' friends revealed that they had adjust their physical abilities to those of the stroke survivors19. These identified barriers contributed to the stroke survivors feeling like they were a burden to their friends, and that put a strain on the friendships. This resulted in further isolation from their friends which compromised the social support offered to the stroke survivors and their participation in social activities.
Transport
Participants of a study conducted in South Africa identified using a wheelchair as a barrier to participation in meaningful occupations, particularly whereby the stroke survivor had limited or no motor function11. Moreover, the barrier of depending on the caregiver to be pushed in the wheelchair restricted participation such as community mobility and social participation Transferring the stroke survivor from the wheelchair into a bus or a minibus taxi to access health care facilities was also seen as a burden on family members. Mudzi et al11 further reported that stroke survivors had to pay an extra taxi fare for putting the wheelchair in a taxi and for the caregiver, which made the use of public transport more costly.
Participants of another study conducted in China revealed that they made use of buses as a common mode of transport. However, they were not able to get on and off the bus, as the buses were not adapted to accommodate people with physical disabilities4. Other studies conducted in China, indicated there was also limited access to assistive devices for personal care devices such as wash mitts, long handled sponges, button hooks, etc418. The participants had to pay for these personal care devices and financial constraints made the devices inaccessible to some. The study reported that the only accessible assistive devices were canes which were limited to those who had regained movement in the lower limbs18.
Accessibility
A systematic review study conducted by Jellema et al.20 identified inaccessible buildings and public spaces such as health care facilities that were not reasonably accommodated for wheelchair use, to be barriers to participation. This included: having limited space in public buildings for the stroke survivor, using a mobility assistive device such as a walker or a wheelchair, to move around. Stroke survivors also identified having steps inside their house, uneven terrain and soil in the yards as a barrier, as this made it difficult for them to move around freely in their homes, particularly, if they used a wheelchair or a walker20. As a result, the participants needed to be pushed in the wheelchair or assisted by their caregivers, which further increased the burden of care.
METHOD
Setting
The study was conducted in the rural and semi-rural parts of Hammanskraal situated in the northern region of Gauteng. The common housing structures include houses built as part of the Reconstruction and Development Project (RDP) and those built with corrugated iron (shacks). There is access to a shopping mall, shopping centres, clinics and one public healthcare district hospital. Most of the population is unemployed and cannot afford to own private transport. As such, the community relies on public transport such as taxis (microbuses) and buses as a means of getting from one place to another. The transport is only accessible at the main tar road, which could be within a 2km-5km radius from the stroke survivors' homes. Gravel roads surround the stroke survivors' homes. This research setting was conveniently sampled because the researcher worked as a clinical occupational therapist in this region at the time of the study.
Design
An explorative, qualitative research study was conducted using a phenomenological approach21.
Population
The population included all the stroke survivors admitted to the district hospital 6-12 months prior to the commencement of the study. The stroke survivors had to be attending occupational therapy rehabilitation at the hospital.
Sampling
A purposive sampling method21 was used to select the participants with subjective experience about the phenomenon of the barriers experienced when participating in meaning occupations in the community context after suffering stroke. Stroke survivors were included if they were: (i) able to speak Setswana and or English, (ii) above the age of 21, (iii) diagnosed with a stroke six to 12 months prior to the commencement of the study and (iv) attending occupational therapy at the monthly stroke clinic at the district hospital. The participants were excluded from the study if they had global aphasia.
Sample size
The participants were recruited at the occupational therapy department of a public healthcare district Hospital in Ham-manskraal, where they attended a multi-disciplinary stroke clinic once per month. The aim and objective of the study were explained in the information leaflet to the stroke survivors. Ten Setswana speaking stroke survivors between the ages of 42 and 77 years consented to participate in the study and for data to be collected at their homes. However, data saturation was reached at seven participants.
Data collection tools
A demographic form and an interview guide were used to collect data. The interview guide consisted of seven open-ended questions that were guided by the Occupational Therapy Practice Framework 3rd edition(OTPF-3)22. The interview guide was translated into Setswana, the language commonly spoken by the participants.
Data collection
Data were collected by the researcher using individual semi-structured interviews which were conducted in Setswana. Furthermore, the researcher took notes to record additional information such as observations made that could not be captured by the audio recorder. For instance, participants' non-verbal expressions, emotional expressions, the side affected by the stroke and the terrain around their house was noted. The collected data were stored electronically on dedicated file that was password protected, as well as on a cloud account.
Data analysis
All interviews were recorded in Setswana and then transcribed verbatim in English. To ensure the accuracy of the translations, these were completed by both the researcher and independent checker who was also fluent in speaking, writing and reading Setswana as a first language and English as a second language. Clarke's deductive thematic analysis method was used to analyse the collected data23. The PEOP model3 was used to guide the emerging themes.
Methodological rigour
The credibility of the study was ensured by the use of more than one person to analyse the data which strengthened the rigour and trustworthiness of the results of the study23. An occupational therapist with experience in qualitative research served as an independent reviewer after the researcher had analysed all the data. Peer checking24 was performed by an additional occupational therapist and no discrepancies arose. Transferability was achieved by providing a thorough and accurate description of the participants' profiles and the methodology employed at each step during the study.
Ethical considerations
The study obtained ethical clearance from the University of Pretoria's Faculty of Health Science Research Ethics Committee (REC) and the National Health Research Committee (NHRC). The project number assigned for this study was 06/2020 with the reference number GP_202001_019. The principles of autonomy, justice and confidentiality were applied throughout the study by: explaining the contents of the information sheet in a language the participants understood (Setswana); having signed consent to participate and be audio recorded; making use of a fair inclusion and exclusion criteria which did not discriminate the participants based on factors such as their race, gender, religious beliefs and by using alphanumeric codes in data analysis to ensure confidentiality.
RESULTS
Demographics of the participants
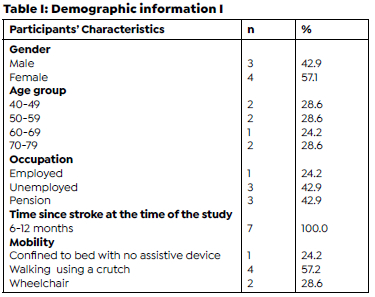
Most of the participants were female, unemployed or on pension and walked with a crutch (Table 1, below).
Themes and sub-themes related to the objective of the research
Overall, four themes and nine sub-themes emerged from the findings. The themes included: physiological, psychological, financial and environmental factors.
Theme 1: Physiological barriers
The physiological factors included fatigue, pain and restricted/limited movement.
Sub-theme: Fatigue
The participants reported that they experienced fatigue, and this has limited their participation in meaningful occupations such as basic activities of daily living (BADL), instrumental activities of daily living (IADL) and social participation. They either performed tasks at a slower rate or had completely stopped participating in meaningful occupations. For the stroke survivors, participating in a simple activity such as bathing, preparing a meal or walking is physically draining.
"I become easily tired. I just do a bit, and I rest when I feel tired." P03
"I am not able to sit in the taxi because I become easily tired." P06
Sub-theme: Pain
The participants who identified localized pain on the affected upper (shoulder and or wrist) or lower limb (hip and or knee) joints as a barrier to participating in occupations, reported that they refrained from using the affected side to avoid experiencing further pain. They reported that the pain was exacerbated by active participation in occupations.
"Sometimes, I feel pain in my leg. So I don't walk that much." P02
"I have severe pain in my shoulder and hand. I am not able to bend it. I am unable to do most of the things because of the pain in this arm." P05
Sub-theme: Restricted/no movement in the affected limbs
The participants reported that they had challenges with mobilizing the affected body structures either due to having no movement or having limited movement.
"My legs become stiff and it becomes difficult for me to move." P02
"The problem is the shoulder. It is heavy and does not move." P04
Theme 2: Psychological barriers
Sub-theme: Fear
Two participants reported that they experienced the fear of something bad happening to them. For example, a fear of suffering another stroke, regressing on the recovery process, falling, or leaving the house on their own.
" I was scared that I might regress." P02
"Sometimes I fear going out on my own because I think I will be stuck, and I am not able to get back home." P03
Sub-theme: Feelings of being a burden
The participants reported to feel like they were being a burden to their caregivers as they needed moderate to maximum assistance in order to participate in meaningful occupations.
"My husband has to wake up in the morning and do everything. I had asked him to stop washing me because it was too much for him, and he had focus on other things such as cleaning and maintaining the yard and other things." P02
"My daughter would be watching TV, and I have to call her to come help with stabilizing the pot. I sometimes feel for her, and I let her be." P03
Theme 3: Environmental barriers
The participants identified the following environmental factors as barriers: access to water and sanitation, physical environment, assistive devices, financial constraints, and access to transport.
Sub-theme: Access to water supply systems
The participants identified not having easy access to water and sanitation as a barrier. They reported that having to fetch water from an outside tap by using a bucket limited their independence in BADLs and lADLs as they had to rely on family members to fetch water for them.
"My child brings me water to wash myself, as I am unable to lift up things using both hands." P04
"My wife prepares water for me to bath. She boils water in a kettle and pours it into a bucket." P05
Sub-theme: Toilet and bath facilities
The participants also reported that using an outside pit toilet was a challenge, as the toilets were located at a distance ranging between 10-30 metres from the house. As a result, the participants were not able to reach the toilet on time to avoid bowel and bladder accidents. This restricted the participants' independence in functional mobility (transferring from the wheelchair to the toilet seat) and toilet hygiene Furthermore, the toilet was not wide enough to accommodate a wheelchair and two people inside (participant and caregiver), and the participants therefore resorted to wearing adult diapers (nappies).
"I wear a nappy. They (referring to his mother and sister) cannot carry me to the toilet because I am heavy." P06
"I wear a nappy because the toilet is outside, and I cannot walk." P07
Most of the participants reported that having to use a plastic bowl for bathing which was a barrier due to the instability of the bowl, as it could easily tip over while attempting to get in and out.
"I would struggle if I try to get inside the plastic dish because it is not stable." P02
Sub-theme: Access to public transport
The participants also identified access to transport as the main barrier to their participation in meaningful occupations. They reported that they had to walk a long distance on gravel roads and uneven terrain in order to reach the main road to access a taxi, and this was a challenge due to restricted mobility and fatigue. They indicated that getting in and out of a taxi was a challenge because they need assistance since the taxi was too high for them to climb in and out, and that the taxis do not allow, or are not built to accommodate, a wheelchair. The participants resort to hiring private cars to transport them to and from their destination, usually the hospital for follow ups.
"We have to walk to the main road to catch a taxi, did you see how far it is." P02
"The leg needs someone to bend it for me to be able to get inside a taxi. You see that a Quantum (a minibus taxi the participants use for transport), it is a bit high." P03
Theme 4: Financial barriers
Sub-theme: Financial constraints
A unique theme emerged from this study. Most of the participants reported that they receive social grants (pension and disability grants) from the government which assist with their day to day living. However, they reported that the funds from the grant are not sufficient to meet their daily requirements; they acknowledged the financial support as a barrier to participation in meaningful occupations.
"We have to hire a car for R50 to take us to church. We are both not working." P01
"We live on pension grants. We take care of our grandchild. We have to hire a car for R400 to take me to the hospital for check-ups. Money does not last." P02
DISCUSSION
Physiological barriers
The participants identified fatigue, pain and restricted or no active movement in the affected limbs as the main contributing factors that hinder their participation in meaningful occupations. The participants of this study revealed that pain was the main contributing factor to hindering participation in meaningful occupations. The finding is supported by the results whereby pain affected the stroke survivors ability to participate in occupations they considered to be meaningful6,11. This resulted in the participants either needing moderate to maximal assistance from their caregivers or ending up experiencing discontinuity with regards to participating in occupations that provide meaning to them, irrespective of the level of disability or severity of the stroke3,5. This increased the burden of care on caregivers and decreased the quality of life of the stroke survivors.
Other participants also refrained from actively moving the affected limbs to avoid experiencing pain. As a result, the participants were confined to one space in their house because the less they moved the less pain they experienced. Active movement was restricted by pain, which is expected after suffering a stroke25. These factors contributed to the participants' poor participation in meaningful occupations. Even though the stroke survivors were educated about the benefits of including the affected limbs in functional activities, their fear of experiencing pain outweighed the benefits of relieving the spasticity through actively mobilizing the affected limbs.
In addition to pain and restricted or no active movement, the participants in this study identified fatigue as a barrier. Although fatigue was identified as a barrier, the participants continued to participate in meaningful occupations but with a decreased rate of performance. Braaten et al12 supported the finding of this study by revealing that fatigue in stroke survivors remained prevalent 3-12 months post stroke. The participants often had to wake up more than two hours earlier to ensure that tasks are completed timeously. Such a challenge caused the participants to become frustrated, as they did not have the energy due to lack of sleep to still manage to participate in their meaningful activity. Previous studies only focused on fatigue impacting negatively on the stroke survivors' BADL and IADL4,26-27, and not occupations such as social participation (going to church) which the participants of this current study identified as meaningful.
Psychological barriers
The findings of this study revealed that the participants experienced the fear of falling and suffering a second stroke, particularly when in a public place. This resulted in them refraining from participating in activities that required them to leave their home regardless of if they were accompanied by a family member or were alone. Walsh et al28. presented related findings showing that it is common for stroke survivors to experience the fear of falling, and that the fear was a barrier that restricted their participation in their lived world. The identified feelings of fear were heightened when the participants had to leave home alone. A study conducted in Malysia by Ainuddin et al.29 further highlighted that the impairments in the stroke survivors' physical, cognitive and sensory systems contribute to the recurrent falls. Furthermore, unfamiliar environments also posed a risk to increased fall. For example, falls may occur when stroke survivors are exposed to uneven surfaces in public places such health care facilities, shopping malls, and other environments they may not be familiar with.
The participants often experienced feelings of being a burden to others as they needed assistance that ranged from moderate to maximum in order to participate in meaningful occupations. The altered level of independence could lead to role loss in occupations they consider to be meaningful as they have to rely on others in order for them to actively participate. The possible role loss has a negative impact on the stroke survivors' self-esteem and mood which could lead to experiencing feelings of depression. A study conducted in Western Cape relates to the findings of this study as it was discovered that gaining independence could improve the stroke survivors' confidence in actively participating in the community and reduce the risk of depression26.
Financial barriers
Most of the participants were dependent on R1780 received from the government's pension and disability grants as a source of income in the year 2020. However, the funds were not adequate to meet all their day-to-day needs. Most of the participants spent a portion of their grant money towards hiring a private car to take them to and from the hospital as well as church. The money spent on hiring a private car ranged from R250-R450 depending on how far the participants live from the hospital or church. This resulted in few participants missing their monthly appointments at the occupational therapy department stroke clinic. Participants in a study by Mudzi et al.11 experienced similar financial challenges whereby they had to spend more money on taxi fare. They had to pay for themselves, the wheelchair and the person helping them to get in a taxi.
The findings of the current study highlighted an important factor whereby the stroke survivors had to compromise their health needs to provide for their family's basic needs such as buying groceries. Such a compromise put them at a significant risk of experiencing secondary complications such a contractures and possible readmission to hospital. Similarly, to the participants in study by Mudzi et al.11, they had to prioritize other needs over spending more money on transport, which compromised their compliance with attending outpatient rehabilitation due to financial constraints.
Environmental barriers
The lack of access to water supply systems, poor toilet and bath facilities and access to public transport were identified as the main barriers in this study. All these factors contributed to the stroke survivors' restricted participation in meaningful occupations such as bathing, toileting, home management, health management and social participation. Findings of previous studies concur that having easy access to resources such as water, electricity and proper sanitation made it easy for participants to be independent in occupations such as BADLs living and lADLs such washing, cleaning, toilet hygiene, cooking and doing laundry4,18.
There is limited research conducted regarding stroke survivors' ability to participate in the activity of bathing using a plastic bowl, particularly in a semi-rural or rural area. The act of bathing from a bowl is different to that of bathing in a bathtub or a shower as it requires a lot of preparation and physical effort when compared to bathing in a bathtub This method of bathing using a plastic bowl is distinctive in non-urban communities as the participants must warm bathing water by boiling it in a kettle and pouring it into a bucket. They then still have to carry the warm water to the bedroom where they transfer it into the plastic bowl, they will be using to wash themselves. The participants raised a concern of the plastic bowl not being stable and safe for them to transfer into and stand in. This is mainly due to the fact that the bowl has to be placed on a chair or on the bed when bathing the upper body to allow the stroke survivors to stand on the floor in an upright position. Subsequently, the bowl must be lifted and positioned on the floor to allow them to bath the lower body. Therefore, stroke survivors will have to get inside the bowl to wash the lower body. This could possibly pose a challenge to the stroke survivor due restricted active movement in the affected side Furthermore; the plastic bowl could easily tip over when it is being transferred from the chair/bed to the floor, or when the stroke survivors climb in it. These actions could cause the water to spill on the floor and result in the participants slipping on the water and suffering fall injuries leading to multiple re-admissions to hospital.
Additionally, the participants of the current study made use of an outside pit toilet that was located far from their houses and required them to walk a distance. Moreover, even if they did reach the toilet on time, there was not enough space inside the toilet to accommodate both the participant on a wheelchair and their caregiver. This challenge contributed to the participants' decreased independence in toileting and toilet hygiene with the added expense of using adult diapers for some.
The stroke survivors also identified having challenges with accessing and using public transport as an environmental barrier. The stroke survivors had to walk a distance to access taxis which are only available at the main road due to the poor or lack of tar road infrastructure near their houses. Subsequent to the challenge of accessing transport, the stroke survivors often had to make use of two or more taxis for the purpose of accessing the nearest health care facilities, church or shopping malls which is time consuming and adds further discomfort to the participants as they have transfer more than once into the taxi and maintain a sitting position for longer. This is because unlike private transport, taxis do not use direct routes to reach the desired destinations. As cited in Jellema et al.20 that living in a rural area presented greater barriers to participation in meaningful occupations due to challenges such as uneven terrain, long distances and poor geographical coverage of public transport thus, supporting the findings of this current study.
Limitations of the study
The study only focused on the experiences of a small sample of older adults with ages ranging from 42 to 77 years. Younger stroke survivors did not participate in the study and thus the existing literature requires further research which will include a wider age range and a larger sample size. Another limitation was that the type of stroke the participants suffered was not classified in their medical history as the hospital did not have resources to identify this, at the time of the study.
Recommendations
A more extensive and larger study is recommended for the purpose of developing a practice framework that will be relevant to the South African context in a community setting. The framework will assist in guiding the assessment and treatment processes, as they will be relevant and specific to the South African context within a community setting. Furthermore, a case study method on this specific topic can be considered for close observation of stroke survivors throughout the process of rehabilitation. This will provide a more in-depth insight into the experiences of stroke survivors when participating in meaningful occupations in the community.
The researcher recommends that occupational therapists should assist stroke survivors identify the factors that they perceive as barriers to their participation within their home and community contexts. This should take place during the initial assessment process, so that intervention may address specific factors in order to enhance participation in occupations the stroke survivors perceive as meaningful.
Moreover, the clinicians could advocate for better resources that will facilitate higher levels of participation in meaningful occupations among communities. They may do this by influencing local municipalities (Ward councillors), policy makers and local taxi associations to consider building and maintaining roads that will enable taxis to be available at various places within the stroke survivors' communities and not only at the main road. In addition, they should also advocate for user-friendly taxi minibuses with easily accessible entrances and adequate space to accommodate wheelchairs. Lastly, the researcher recommends for the clinicians to advocate for community-based projects that will afford the stroke survivors opportunities to generate income, as the financial support they receive from grants, is not adequate sustain them.
CONCLUSION
The findings of this study highlighted a significant difference between the barriers experienced by stroke survivors residing in the rural/semi-rural and urban community contexts. These barriers contributed to the stroke survivors experiencing greater discontinuity and or challenges concerning participating in meaningful occupations than has been reported for urban areas. Thus, a screening tool that is relevant to the South African community context is needed for the purpose of making occupational therapy more meaningful to the lives of the stroke survivors residing in the rural and semi-rural communities.
Author contributions
Refilwe Mohotlhoane was involved in designing the study, data collection, formal analysis, writing of the original draft and wrote the manuscript. Refilwe Mohotlhoane and Mashudu Norman Nemakanga reviewed and revised the manuscript. Both authors read and approved the final manuscript. The study was conducted by the first author for higher degree purposes, supervised by the second author.
Acknowledgements
Mrs Jodie de Bryun for her postgraduate supervision during the time of study.
Conflicts of interest
The authors have no conflicts of interest to declare.
REFERENCES
1. Murphy SJ, Werring DJ. Stroke: causes and clinical features. Medicine. 2020 Sep 1;48(9):561-6. https://doi.org/10.1016/j.mpmed.2020.06.002 [ Links ]
2. Whitehead S, Baalbergen E. Post-stroke rehabilitation. South African Medical Journal. South African Medical Association NPC; 2019 Jan 31;109(2):81. https://dx.doi.org/10.7196/samj.2019.v109i2.00011 [ Links ]
3. Baum CM, Christiansen CH & Bass J. The Person-Environment-Occupation-Performance (PEOP) model. In C,H Christiansen, C.M. Baum,& J.D. Bass(Eds), Occupational therapy: Performance, participation, and well-being.(4th ed.,pp.49-56).Thorofare. NJ:SLACK Incorporated. 2015; 4:49-56. [ Links ]
4. Zhang LMSN, Yan TMDP, You LP, Li KMSNP. Barriers to activity and participation for stroke survivors in rural China. Archives of Physical Medicine and Rehabilitation. 2015; 96(7):1222-8. https://doi.org/10.1016/j.apmr.2015.01.024 [ Links ]
5. Law M, Cooper B, Strong S,Steward D, Rigby P, Letts L. The person-environment-occupation model: A transactive approach to occupational performance. Canadian Journal of Occupational Therapy. 1996; 63(1):9-23. https://doi.org/10.1177/000841749606300103 [ Links ]
6. Urimubenshi G. Activity limitations and participation restrictions experienced by people with stroke in Musanze district in Rwanda. African Health Sciences. African Journals Online (AJOL); 2015 Sep10;15(3):917.https://doi.org/10.4314/ahs.v15i3.28 [ Links ]
7. Fallahpour M, Jonsson H, Joghataei M, Nasrabadi A, Tham K. I am not living my life: Lived experience of participation in everyday occupations after stroke in Tehran. Journal of Rehabilitation Medicine. Acta Dermato-Venereologica; 2013; 45(6):528-34. https://doi.org/10.2340/16501977-1143 [ Links ]
8. Walsh ME, Galvin R, Loughnane C, Macey C, Horgan NF. Factors associated with community reintegration in the first year after stroke: a qualitative meta-synthesis. Disability and Rehabilitation. Informa UK Limited; 2014 Nov 10;37(18):1599-608. https://doi.org/10.3109/09638288.2014.974834 [ Links ]
9. Akosile C, Nworah C, Okoye E, Adegoke B, Umunnah J, Fabunmi A. Community reintegration and related factors in a Nigerian stroke sample. African Health Sciences. African Journals Online (AJOL); 2016 Oct 17;16(3):772. https://doi.org/10.4314/ahs.v16i3.18 [ Links ]
10. Fryer K, Baxter S, Brumfitt S. The meaning of participation to stroke survivors: a qualitative study. International Journal of Therapy and Rehabilitation. Mark Allen Group; 2016 Aug 2;23(8):356-62. https://doi.org/10.12968/ijtr.2016.23.8.356 [ Links ]
11. Mudzi W, Stewart A, Musenge E. Community participation of patients 12 months post-stroke in Johannesburg, South Africa. African Journal of Primary Health Care & Family Medicine. AOSIS; 2013 Jan 24;5(1). https://doi.org/10.4102/phcfm.v5i1.426 [ Links ]
12. Braaten RS, Askim T, Gunnes M, Indredavik B. Fatigue and activity after stroke. Secondary results from the life after stroke study. Physiotherapy Research International. 2020; 25(4):e1851. https://doi.org/10.1002/pri.1851 [ Links ]
13. White JH, MacKenzie L, Magin P, Pollack MRP. The Occupational Experience of Stroke Survivors in a Community Setting. Occupational Therapy Journal of Research: Occupation, Participation and Health. SAGE Publications; 2008 Sep 1;28(4):160-7. https://doi.org/10.3928/15394492-20080901-05 [ Links ]
14. Obembe A, Mapayi B, Johnson O, Agunbiade T, Emechete A. Community reintegration in stroke survivors: Relationship with motor function and depression. Hong Kong Physiotherapy Journal; 2013 Dec;31(2):69-74. https://doi.org/10.15405/epsbs.2019.11.50 [ Links ]
15. Torregosa MB, Sada R, Perez I. Dealing with stroke: Perspectives from stroke survivors and stroke caregivers from an un-derserved Hispanic community. Nursing & Health Sciences. Wiley; 2018 Mar 7;20(3):361-9. https://doi.org/10.1111/nhs.12414 [ Links ]
16. Qiu X, Sit JWH, Koo FK. The influence of Chinese culture on family caregivers of stroke survivors: A qualitative study. Journal of Clinical Nursing. Wiley; 2017 Sep 6;27(1-2):e309-e319. https://doi.org/10.1111/jocn.13947 [ Links ]
17. Suttiwong J, Vongsirinavarat M, Hiengkaew V. Predictors of Community Participation Among Individuals with First Stroke: A Thailand Study. Annals of Rehabilitation Medicine. Korean Academy of Rehabilitation Medicine; 2018 Oct 31;42(5):660-9. https://doi.org/10.5535/arm.2018.42.5.660 [ Links ]
18. Zhang L, Yan T, You L, Gao Y, Li K, Zhang C. Functional activities and social participation after stroke in rural China: a qualitative study of barriers and facilitators. Clinical Rehabilitation. SAGE Publications; 2017 Aug 4; 32(2):273-83. https://doi.org/10.1177/0269215517719486 [ Links ]
19. Erler KS, Sullivan V, McKinnon S, Inzana R. Social support as a predictor of community participation after stroke. Frontiers in Neurology. 2019 Sep 20; 10:1013. doi:10.3389/fneur.2019.01013 [ Links ]
20. Jellema S, van Hees S, Zajec J, van der Sande R, Nijhuis- van der Sanden MW, Steultjens EM. What environmental factors influence resumption of valued activities post stroke: a systematic review of qualitative and quantitative findings. Clinical Rehabilitation. SAGE Publications; 2016 Sep 28;31(7):936-47. https://doi.org/10.1177/0269215516671013 [ Links ]
21. Creswell JW, Poth CN. Qualitative inquiry & research design : Choosing among five approaches. Fifth edition. Thousand Oaks, CA : SAGE; 2018. [ Links ]
22. Occupational Therapy Practice Framework: Domain and Process (3rd Edition). American Journal of Occupational Therapy. AOTA Press; 2017 Sep11;68(Supplement_1):S1. https://dx.doi.org/10.5014/ajot.2014.682006 [ Links ]
23. Clarke V, Braun V. Teaching thematic analysis: Over-coming challenges and developing strategies for effective learning. The Psychologist. 2013; 26:120-1-3. [ Links ]
24. Leech NL, Onwuegbuzie AJ. An array of qualitative data analysis tools: A call for data analysis triangulation. School Psychology Quarterly. American Psychological Association (APA); 2007 Dec; 22(4):557-84. https://doi.org/10.1037/1045-3830.22.4.557 [ Links ]
25. Li S. Spasticity, Motor Recovery, and Neural Plasticity after Stroke. Frontiers in Neurology. Frontiers Media SA; 2017 Apr 3; 8. https://doi.org/10.3389/fneur.2017.00120 [ Links ]
26. Elloker T, Rhoda A, Arowoiya A, Lawal IU. Factors predicting community participation in patients living with stroke, in the Western Cape, South Africa. Disability and Rehabilitation. Informa UK Limited; 2018 May 29; 41(22):2640-7. https://doi.org/10.1080/09638288.2018.1473509 [ Links ]
27. Meijering L, Nanninga CS, Lettinga AT. Home-making after stroke. A qualitative study among Dutch stroke survivors. Health & Place. Elsevier BV; 2016 Jan; 37:35-42. https://doi.org/10.1016/j.healthplace.2015.11.006 [ Links ]
28. Walsh M, Galvin R, Horgan NF. Fall-related experiences of stroke survivors: a meta-ethnography. Disability and Rehabilitation. Informa UK Limited; 2016 Mar 23;39(7):631-40. https://doi.org/10.3109/09638288.2016.1160445 [ Links ]
29. Ahmad-Ainuddin H, Romli MH, Hamid TA, SF Salim M, Mackenzie L. An exploratory qualitative study with older malaysian stroke survivors, caregivers, and healthcare practitioners about falls and rehabilitation for falls after stroke. Frontiers in Public Health. 2021 Apr 27. https://doi.org/10.3389/fpubh.2021.611814 [ Links ]
 Correspondence:
Correspondence:
Mashudu Nemakanga
mashudu.nemakanga@smu.ac.za
Received: August 2022
Peer review: September 2022
Revised: December 2022
Accepted: January 2023
Published: April 2023
Editor: Blanche Pretorius: https://orcid.org/0000-0002-3543-0743;
Funding: No funding was received for this research.














