Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.52 n.3 Pretoria Dec. 2022
http://dx.doi.org/10.17159/2310-3833/2022/vol52n3a7
RESEARCH ARTICLE
Knowledge and perception of occupational therapists and physiotherapists on the use of constraint-induced movement therapy for stroke rehabilitation in South Africa
Velisiwe Zodwa MbuyisaI; Michael O OgunlanaII; Nonjabulo NdabaIII; Pragashnie GovenderIV
ISchool Based Occupational Therapist, Department of Education, Gauteng, South Africa https://orcid.org/0000-0003-1220-4302
IIFederal Medical Centre, Abeokuta, Ogun/ West, Nigeria https://orcid.org/0000-0001-6877-6938
IIISchool of Health Sciences, University of KwaZulu-Natal, South Africa https://orcid.org/0000-0002-8273-028X
IVSchool of Health Sciences, University of KwaZulu-Natal, South Africa https://orcid.org/0000-0003-3155-3743
ABSTRACT
BACKGROUND: Rehabilitation therapists are expected to manage upper extremities difficulties following stroke by using effective treatment approaches. Constraint-induced movement therapy (CIMT) facilitates upper extremity functional recovery in patients after stroke; however, in South Africa, its application is not well documented.
AIM: To assess and compare the knowledge and perception of occupational therapists and physiotherapists on the use of CIMT for stroke rehabilitation in South Africa.
METHODS: A descriptive cross-sectional design using a self-administered online questionnaire was distributed via the two national professional societies. Data were analysed descriptively and the Mann-Whitney U and Kruskal Wallis tests were used to make inferences
RESULTS: Of 108 respondents, 49.1% (n=53) were occupational therapists, and 50.9% (n=55) physiotherapists. A higher level of education (p=0.037) and working specifically with stroke patients (p=0.050) are significantly associated with better CIMT knowledge and perception. The profession of the participants was not significantly associated with their knowledge and perception of CIMT.
CONCLUSION: This study demonstrates gaps in the knowledge of CIMT as a treatment technique for upper extremity impairment following stroke. Although most respondents knew about CIMT, improved guidance and knowledge of CIMT are required to remediate knowledge gaps. This may assist in improving the feasibility of CIMT and thus promote its clinical application, given the prevalence of UE impairment in stroke patients managed by therapists.
Keywords: upper extremity rehabilitation, motor cortical laterality, ipsilateral hemisphere, motor function, continuing professional education.
INTRODUCTION
Most stroke survivors have upper extremity (UE) impairment early after stroke1. The prevalence of upper extremity impairment is approximately 50-80% in the acute phase and 40-50% in the chronic phase2. Impairment of the UE can cause significant difficulties for patients recovering from stroke as it affects all areas of occupation. In clinical practice, occupational therapists and physiotherapists are expected to manage UE impairment after stroke and carry out treatment approaches that will effectively rehabilitate the UE. Yet, the treatment approaches for managing these difficulties in South Africa have not been widely reviewed.
After a stroke, several approaches exist for UE motor function rehabilitation. Constraint-induced movement therapy (CIMT) is a commonly used rehabilitation approach to improve upper extremity function (e.g., hemiparesis) after a stroke. In CIMT, the less affected UE is restrained while the affected UE receives intensive training in unimanual skills and the fine motor skills of the affected UE improve significantly after intervention3. CIMT has been shown to improve motor function in chronic hemiparesis of stroke patients4. In chronic patients with mild to moderate hemiparesis, the CIMT rehabilitation approach has been used for improving the motor recovery of the affected UE4,5. Following a stroke, the patient starts to compensate due to difficulty using the affected limb, relying increasingly on the unaffected limb, and this compensation will result in learned non-use6. Although CIMT is regarded as the most effective approach to facilitating UE recovery following stroke, it has also not been used frequently for neurological rehabilitation by therapists5.
In South Africa, the absolute number of persons affected by stroke has increased yearly since 1990, along with the number of disabled stroke survivors7. The use of the CIMT treatment approach could be valuable in treating UE impairment; however, its application within the South African context is not well documented. Knowledge and perception of the use of CIMT for stroke rehabilitation are reported to directly affect the therapist-patient interaction, competence in carrying out the necessary intervention, and preferred therapy approach when providing treatment6. The study investigated the knowledge and perceptions of South African occupational therapists and physiotherapists on the utilisation of CIMT for UE rehabilitation in stroke patients. The main hypothesis examined in this study was that there would be no significant difference in the knowledge and perception of South African occupational therapists and physiotherapists in the utilisation of CIMT for UE stroke rehabilitation. The outcome of this enquiry may be useful for knowledge translation by South African health professional associations to influence clinical practice, and in informing curricula inclusions at an undergraduate level at institutions.
LITERATURE REVIEW
CIMT is suitable for stroke patients with mild to moderate arm and hand function impairment. It encourages increased use of the affected arm in daily life8. CIMT indicate improvements in the patient's ability to complete daily activities with their affected extremity following CIMT treatment9. Therefore, in patients with residual arm function but still with severe functional impairments (i.e., moderate paresis), therapy with CIMT should be strongly consideredlO. The process of gain in motor function of the affected UE after the introduction of the CIMT during rehabilitation is said to be linked with the increase in activation of motor cortices of the undamaged hemisphere during affected hand movement; patients show a shift in motor cortical laterality toward the ipsilateral hemisphere in association with improved motor function of the affected limb resulting in improved motor function of the affected UE in patients with chronic stroke4, 5.
Practice of constraint-induced movement therapy
The principal foundation of CIMT practice is the (a) use of restraint, (b) repetitive, structured, practice intensive therapy in the more affected arm, and (c) application of a package of behavioural techniques that transfers gains from the clinical setting to the real world11. A restraint is worn over the unaffected arm to prevent movement, to ensure that the stroke survivor uses the affected limb to carry out functional tasks. Mass practice is the intensive repetition of motor activity11. Methods and duration of CIMT delivery vary in the type of constraint worn, and in time frames ranging from 30 minutes to six hours a day, or more12. Prominent ranges in dosage variability found in the literature included: durations from five days13, to 70 days14, and one hour a day13 to six hours a day15. This variation in dosage depends on the availability of the caregiver, level of tolerance and active participation of the patient. Shaping is a method in which motor tasks are gradually made more difficult. It is the progression of tasks given to a patient according to the patient's motor ability11. The tasks are usually functional and can include picking up a cup from the table, taking it to the mouth, drinking from it, writing letters, transferring objects from left to right on a table, brushing the teeth, and removing shoes, amongst others. Transfer package is the use of the hand in life situations, and problem-solving to overcome perceived barriers to using the other body extremities16.
Barriers to constraint-induced movement therapy use
Factors that hinder the usage of CIMT are categorised into three broad groups as described by Fleet et al5. These barriers are therapist-related, institutional mediated, and patient-related barriers (including physical or cognitive challenges). Regarding institutional and patient barriers, findings have shown that a lack of resources can hinder CIMT use. Patient non-compliance and cognitive and physical characteristics may be the main barriers to implementing CIMT. Restraint and repetitive intensive training may affect the participant's motivation to use CIMT17,18 and the high labour demand in the clinical setting may hinder the use of CIMT18. Therefore, increasing participants' motivation and decreasing the CIMT's human resources demand are required to successfully implement CIMT. The duration required for each CIMT session differs widely between studies, ranging from 30 minutes to six hours per day12-15, 17. This can pose a considerable hindrance to the utilization of the CIMT treatment approach.
METHODS
Study Design
The study used a descriptive cross-sectional study design with a self-administered online questionnaire that sought to assess and compare the knowledge and perception of CIMT by South African occupational therapists and physiotherapists.
Study Setting
The study used an online platform to access occupational therapists and physiotherapists working in the public and private health care sectors of SA.
Recruitment, Selection and Sampling
Participants were recruited through a convenience sample after satisfying the selection criteria. Inclusion criteria required participants to be currently registered with the Health Professions Council of South Africa (HPCSA), participants holding recognised undergraduate qualifications in occupational therapy or physiotherapy, employed in South Africa, and currently practising occupational therapy or physiotherapy. Lastly, participants had to be engaged in providing interventions for patients with neurological impairments in clinical practice at the time of the study. Participants employed outside of South Africa and practising in other health professions were excluded.
Participants were sampled based on their field of practice in adult neurology. The sample size was determined using the Cohen effect size formula to compare the knowledge and perception of occupational therapists and physiotherapists about the use of CIMT as described by Sullivan19. Using an a-priori effect size of 0.6, at a power of 80% and a 95% confidence interval, each group needed to have a minimum sample size of 44 participants making a total of N=88 participants for the two groups. Assuming a 10% non-response rate, the desired sample size was 96 participants (48 subjects per group).
A series of initial qualifying questions were asked in the survey. Those who did not meet the eligibility for participation were immediately redirected to submit without being permitted to complete/progress on the survey. The qualifying questions included undergraduate qualification, and registration status with the HPCSA and if their experience in the field of stroke rehabilitation had been obtained in South Africa or internationally. Only participants who met all the predetermined criteria could continue to the next section of the survey.
Research Instrument
The research instrument was a questionnaire that was developed using Google Forms which is a survey administration application. The three-part questionnaire had section A that sought to elicit demographic data, presented in closed multiple-choice format. Section B consisted of twelve dichotomous questions on knowledge about CIMT and Section C had thirteen Likert scale questions on perception of CIMT use in clinical practice.
Intra-rater test-retest reliability involving 20 therapists was done for the developed questionnaire. This had an item-by-item kappa value of 1 for all 25 items correlated implying an excellent item by item internal consistency. The initial intraclass coefficient (ICC) for the research instrument was 0.619 with a 95% confidence interval of 0.426-0.771. The item-by-item Cronbach Alphas were used in improving the ICC by removing some redundant questions. This resulted in a new ICC of 0.768 with a 95% confidence interval of 0.65-0.86. An expert panel of occupational therapists and physiotherapists conducted a face validity check on the questionnaire. This reduced threats of validity by improving the data collection tool and ensuring that it measured what it purports to measure.
Data Collection
An online survey format was used for data collection, and this was appropriate as it limited human to human contact as it is prescribed in this COVID era. It also allowed the researcher to collect data from therapists across a larger geographical area. This online survey was sent out via the Occupational Therapy Association of South Africa (OTASA) and the South African Society of Physiotherapy (SASP). Data collection aimed to gain insight into the knowledge and perceptions of participants.
Data Analysis
Since Google Survey was used as an online platform for data collection, responses were automatically uploaded into a secure Google spreadsheet. The data were transferred onto a spreadsheet using Microsoft Excel and were later analysed using SPSS 21 software (IBM, 2017). Data were collated, cleaned, and coded for descriptive analysis. Scoring of sections B and C of the questionnaire was done to generate knowledge and perception scores, respectively. In the knowledge section, every correct answer was scored one and any incorrect answer was scored zero. For the perception section, all the negative answers (strongly disagree/agreed, disagree/agreed and neutral) were scored zero while all positive answers were scored one; agree/disagree was scored one and strongly agree/ strongly disagreed was scored two. A test of normality was performed on the knowledge and perception scores using the Shapiro Wilk test with a p-value of 0.002 for perception score and <0.0001 for knowledge score, showing that the data were not normally distributed. MannWhitney U and Kruskal Wallis tests were used in making inferences on the association between components of knowledge, perception and demographic characteristics. The level of statistical significance was set at p ^ 0.05.
Ethical Considerations
Ethical approval for the study was obtained from the Human and Social Science Research Ethics Committee (HSSREC) of the University of KwaZulu-Natal (HSS-REC/00002860/2021). Gatekeeper's permission was obtained from OTASA and SASP. Informed consent was obtained from individuals participating in the study. The participants were required to declare that they understood the research process, their rights as participants and voluntarily consent to participate.
RESULTS
A total of n=108 therapists responded to the study and provided consent. Of these 91.7%, (n=99) of respondents completed all three sections of the online questionnaire. Of these, 49.1% (n=53) practised as occupational therapists, and 50.9% (n=55) practised as physiotherapists. Respondents comprised of 30.6% (n=33) males and 69.4% (n=75) females who represented all provinces. A total of 79.6% (n=86) respondents reported a bachelor's degree as their highest level of education, 17.6% (n=19) had a master's degree, and 2.8% (n=3) reported they had a PhD. While all respondents had experience practising in stroke rehabilitation, 38.9% (n=42) reported having less than five years of experience. Most respondents (68.5%; n=74) reported working primarily with both in-patient and out-patients. Other demographic characteristics of the respondents are detailed in Table I, above.
Therapists' Knowledge of Constraint-Induced Movement Therapy
The knowledge score ranged from 5 to 12, with a median knowledge score and its interquartile range being 9.0 (8-10). Statistical hypothesis testing was conducted (Table II, above) between the knowledge components to determine the statistical difference (p <0.05) and the association between selected variables elicited in section A of the questionnaire. The knowledge of occupational therapists and physiotherapists of CIMT was not significantly different as presented in Table II, above (p-value = 0.164).
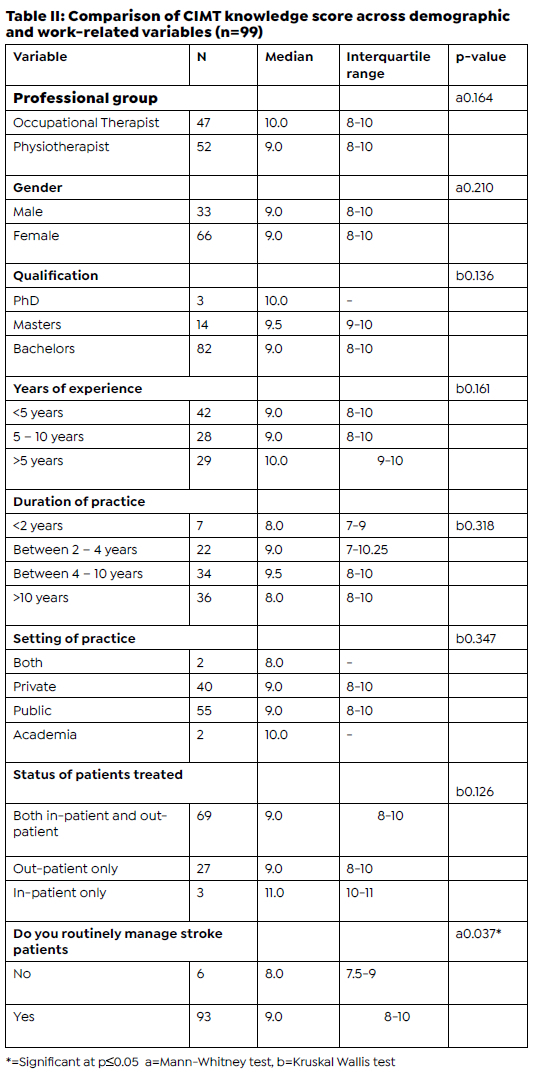
Therapists involved in managing stroke patients in clinical practice had a significantly higher CIMT knowledge score when compared to therapists that do not routinely manage stroke patients with CIMT (p = 0.037).
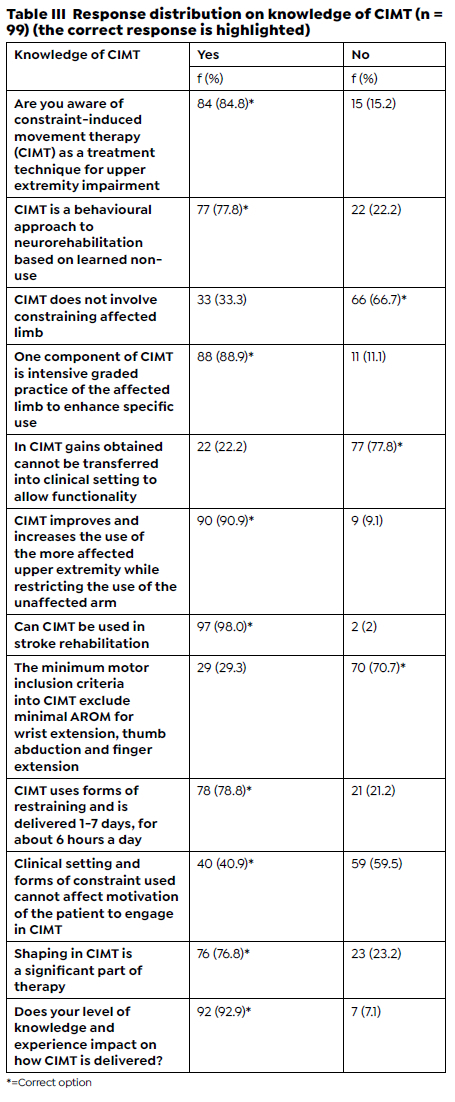
A total of 84.8% (n = 84) respondents were aware of the CIMT as a treatment technique for UE impairment and 98% (n=97) respondents agreed that it can be used in stroke rehabilitation. Furthermore, 15.2% (n=15) of respondents reported being unaware of CIMT as a treatment technique for UE impairment. A total of 66.7% (n=66) respondents reported that CIMT does not involve constraining the affected arm, and 78.8% (n=78) respondents reported that CIMT is delivered one to seven days for about six hours a day. The majority of respondents (88.9%; n=88) reported intensive graded practice of the affected UE to enhance specific use as one of the components of CIMT. The majority (77.8%; n=77) of respondents indicated that CIMT gains could not be transferred from the clinical setting to allow for functions and 90.9% (n=90) described the aim of CIMT as to improve and increase the use of the more affected UE while restricting the use of the unaffected UE hence improving the functioning of the affected UE. Most respondents (98.0%, n=97) believed CIMT to be an efficacious treatment technique in stroke rehabilitation (see Tables III and IV on pages 56 and 57).
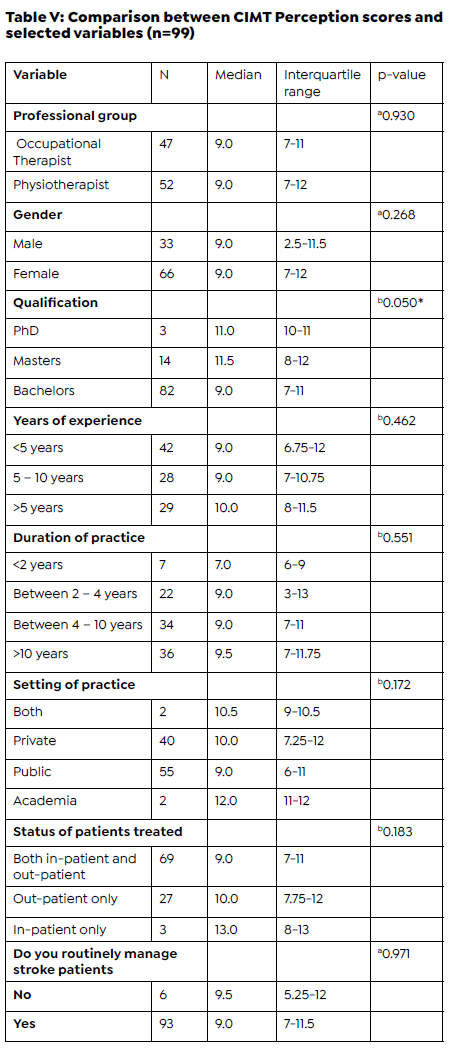
The CIMT perception scores ranged from 0 to 19, with a median and interquartile range of 9.0 (7-12). Statistical hypothesis testing was conducted (Table V page 59) between perception components to determine the statistical difference (p < 0.05) and the association between selected variables elicited in section A of the questionnaire. Therapists with higher qualifications had higher CIMT perception scores (p = 0.050) on the use of CIMT in the management of UE impairment during stroke rehabilitation thus implying that therapists with higher qualifications perceive CIMT as a valuable treatment modality. There was no significant difference between the perception of occupational therapists and physiotherapist on the use of CIMT (p=0.930 see Table V, page 59).
DISCUSSION
This study was designed to assess and compare the knowledge and perception of occupational therapists and physiotherapists on the use of CIMT for managing UE impairment after stroke in South Africa. Occupational therapists and physiotherapists have a fundamental role in treating UE impairment in stroke rehabilitation. Occupational therapists use CIMT to improve the performance of occupations, such as activities of daily living and increased spontaneous use of the affected arm during dressing, bathing, and feeding20. In occupational therapy, CIMT has been shown to elicit changes in UE function through improvements in components of performance skills practised repetitively21 including improved hand function of the affected arm in reach, grasp, release, push, pull, sustained grasp, and bilateral use during play22. Physiotherapists use CIMT to improve gait and mobility-related functions. The outcome of this study reveals that the knowledge and perception of occupational therapists and physiotherapists in SA about CIMT were not significantly different. Though no published study known to the authors had examined the difference in knowledge and perception about CIMT among these two-rehabilitation professionals, it is expected that occupational therapists should be more knowledgeable and practically oriented about the use of CIMT in UE impairments of stroke survivors. This assumption is premised on the fact that the model of the practice of occupational therapists focuses more on the restoration of precision activities function than physiotherapists that focus more on gross movement restoration. Hence, occupational therapists may be more attentive to implementing a transfer treatment package alongside shaping activities as it is entrenched in the CIMT protocol.
Knowledge is a crucial requirement for using CIMT in stroke patients. Knowledge is a modifying factor in perception and practical behaviours23. The level of knowledge about CIMT demonstrated by occupational therapists and physiotherapists will reveal the competency of therapists to use the treatment technique in treating UE impairment successfully. More than half of the respondents reported being knowledgeable about CIMT as a treatment technique used in stroke rehabilitation. They indicated that CIMT improves the potential motor capability of patients following stroke. it appears that some therapists were not well informed on the utility of CIMT while some do not use it at all despite the benefits associated with its use. The non-usage of CIMT by these therapists may be related to their lack of knowledge and other factors that influence their practice.
Most respondents stated that CIMT requires additional specialised training to ensure that therapists are competent and effective when delivering stroke intervention using this treatment technique for UE impairment. There are specific components of CIMT that are necessary for efficacious intervention16,24. These regimens are better learnt with specific training for clinicians interested in delivering CIMT for stroke survivors. The modified protocol of CIMT appears to be much more accepted in clinical practice and therapists are expected to receive further training to enable the standardised usage of the revised protocol. Most respondents reported having clinical experience of more than ten years, this may explain the reason why most of them had good knowledge of CIMT and its components as they may have come across this intervention during their years of training and clinical practice. Therapists who have only some knowledge of CIMT (i.e., minimal or moderate knowledge) would need further training to allow them to implement CIMT in clinical practice competently.
While CIMT is identified as an effective technique, 92.9% of respondents agreed that the level of knowledge and experience impacts the therapist's competency to successfully use CIMT as a treatment technique in a clinical setting. To assess respondents' knowledge about CIMT, they were asked if shaping is a significant component of CIMT. The majority were able to identify shaping as substantial in CIMT. Shaping is considered one of the core components of treatment, and, consequently, a critical part of any CIMT protocol202425. This ability to identify CIMT fundamental components reveals a positive knowledge of the CIMT protocol among respondents24. The results obtained from our sample of therapists reinforce prior observations that increasing therapists' knowledge of CIMT can contribute to more frequent use in clinical practice. This is aligned with Christie and colleagues20, who reported that a range of strategies are needed for improving therapists' knowledge and skills to increase the frequency of CIMT delivery in clinical practice. Inferential analysis reveals that therapists practising stroke rehabilitation had significantly better knowledge than those not routinely involved in stroke rehabilitation. This is a plausible outcome as it is clear that the concept of CIMT stemmed from neurological rehabilitation2526.
A similar analysis reveals that therapists with higher educational qualifications had a significantly better perception of CIMT. Therefore, the level of qualification and duration of working with stroke patients impact the knowledge and perception of occupational therapists and physiotherapists on CIMT as a treatment technique for UE impairment. Fleet et al5 reported similar findings among a population of Canadian occupational therapists and physiotherapists, hence the most accessible means of promoting the effective application of CIMT is through improved education.
The CIMT technique encourages the use of the affected UE therefore, it allows patients to be meaningfully engaged in basic activities of daily living and improve their occupational performance. CIMT has beneficial effects on motor function, arm-hand activities, and self-reported daily arm-hand functioning. Findings from the study showed that less than half of the respondents had a negative perception about using CIMT for UE management hence these respondents would not be eager to use CIMT in stroke rehabilitation. It was noted that restrictions and barriers to using CIMT mainly were a result of the negative perception of some therapists. They suggested that CIMT should not be considered a primary treatment technique for UE impairment in stroke patients. Still, in practical terms, stroke rehabilitation is usually composed of different intervention models. Based on our findings, the divergence between the knowledge and perception of the therapist about CIMT suggests that there are also several barriers to implementation and use of CIMT in clinical practice such as lack of specific knowledge, time duration6 required to implement CIMT, number of therapists working with stroke patients, type of setting and lack of resources in clinical practice5,20,24,25. Therapists also reported type of restraints used to be a barrier preventing CIMT use clinically24.
Limitations
Information gathered from the survey was restricted to closed-ended multiple-choice questions which may have been ambiguous to the respondent. Participants were not provided with an opportunity to share their experiences using CIMT. As a result, only knowledge and perceptions were assessed with no in-depth information regarding CIMT. A mixed-method research design may be more appropriate for comparing the knowledge and perception of the two professionals regarding their usage of CIMT.
CONCLUSION
The importance of occupational therapists and physiotherapists providing intervention for UE impairment using CIMT in stroke rehabilitation within the South African context was assessed and compared in this study. The outcomes from the study suggest that therapist's knowledge and perception on the use of CIMT was not different and a higher level of education / working specifically with stroke patients have better knowledge and perception of CIMT. Our findings regarding knowledge and perception about CIMT among practising therapists in our sample highlight the need for continuing professional education since most respondents indicated that additional training is required for therapists to successfully use CIMT intervention in stroke patients. Therapists' perceptions of CIMT can inform recommendations for UE intervention following stroke. Furthermore, these results can guide future research, which should focus on balancing the clinical feasibility of CIMT and its effectiveness in treating UE impairment in stroke patients.
Author Contributions
Velisiwe Zodwa Mbuyisa completed the study towards a postgraduate degree and was responsible for drafting the manuscript. Michael Opeoluwa Ogunlana, Nonjabulo Ndaba and Pragashnie Govender supervised the study and assisted in the critical revision of the manuscript. All authors approved the final version.
Conflict of Interest (COI) Statement
The authors declare no conflict of interest.
Acknowledgement
The first author is acknowledged posthumously as the primary researcher of this study, which was completed as part of her postgraduate studies. Due acknowledgement is also given to the Occupational Therapy Association of South Africa and the South African Society of Physiotherapy for gatekeepers' approval to access therapists in South Africa through their platforms.
REFERENCES
1. Hayward KS, Kramer SF, Thijs V, Ratcliffe J, Ward NS, Churilov L, Jolliffe L, Corbett D, Cloud G, Kaffenberger T, Brodtmann A, Bernhardt J, Lannin NA. A systematic review protocol of timing, efficacy and cost effectiveness of upper limb therapy for motor recovery post-stroke. Syst Rev. 2019;8(1):187. https://doi.org/10.1186/s13643-019-1093-6 [ Links ]
2. Hussain N, Alt Murphy M, Sunnerhagen KS. Upper Limb Kinematics in Stroke and Healthy Controls Using Targetto-Target Task in Virtual Reality. Front Neurol. 2018;9:300. https://doi.org/10.3389/fneur.2018.00300 [ Links ]
3. Wu WC, Hung JW, Tseng CY, Huang YC. Group Constraint-Induced Movement Therapy for Children With Hemiple-gic Cerebral Palsy: A Pilot Study. The American Journal of Occupational Therapy. 2013;67(2):201-208. https://doi.org/10.5014/ajot.2013.004374 [ Links ]
4. Schaechter JD, Kraft E, Hilliard TS, Dijkhuizen RM, Benner T, Finklestein SP, Rosen BR, Cramer SC. Motor recovery and cortical reorganization after constraint-induced movement therapy in stroke patients: a preliminary study. Neurorehabil Neural Repair. 2002;16(4):326-338. https://doi.org/10.1177/154596830201600403 [ Links ]
5. Fleet A, Che M, Mackay-Lyons M, Mackenzie D, Page S, Eskes G, McDonald A, Boyce J, Boe S. Examining the use of constraint-induced movement therapy in canadian neurological occupational and physical therapy. Physio-ther Can. 2014;66(1):60-71. doi:10.3138/ptc.2012-61 [ Links ]
6. Singh P, Pradhan B. Study to assess the effectiveness of modified constraint-induced movement therapy in stroke subjects: A randomized controlled trial. Ann Indian Acad Neurol. 2013;16(2):180-184. https://doi.org/10.4103/0972-2327.112461 [ Links ]
7. Maredza M, Bertram MY, Tollman SM. Disease burden of stroke in rural South Africa: an estimate of incidence, mortality and disability adjusted life years. BMC Neurol. 2015;15:54. https://doi.org/10.1186/s12883-015-0311-7 [ Links ]
8. Barzel A, Ketels G, Tetzlaff B, Krüger H, Haevernick K, Daubmann A, Wegscheider K, Scherer M. Enhancing activities of daily living of chronic stroke patients in primary health care by modified constraint-induced movement therapy (HOMECIMT): study protocol for a cluster randomized controlled trial. Trials. 2013;14:334. https://doi.org/10.1186/1745-6215-14-334 [ Links ]
9. Charles JR, Wolf SL, Schneider JA, Gordon AM. Efficacy of a child-friendly form of constraint-induced movement therapy in hemiplegic cerebral palsy: a randomized control trial. Dev Med Child Neurol. 2006;48(8):635-642. https://doi.org/10.1017/S0012162206001356 [ Links ]
10. Boyd R, Sakzewski L, Ziviani J, Abbott DF, Badawy R, Gilmore R, Provan K, Tournier JD, Macdonell RAL, Jackson GD. INCITE: A randomised trial comparing constraint induced movement therapy and bimanual training in children with congenital hemiplegia. BMC Neurol. 2010;10:4. https://doi.org/10.1186/1471-2377-10-4 [ Links ]
11. Morris DM, Taub E, Mark VW. Constraint-induced movement therapy: characterizing the intervention protocol. Eura Medicophys. 2006;42(3):257-268. [ Links ]
12. Brady K, Garcia T. Constraint-induced movement therapy (CIMT): pediatric applications. Dev Disabil Res Rev. 2009;15(2):102-111. https://doi.org/10.1002/ddrr.59 [ Links ]
13. Coker P, Lebkicher C, Harris L, Snape J. The effects of constraint-induced movement therapy for a child less than one year of age. NeuroRehabilitation. 2009;24(3):199-208. https://doi.org/10.3233/NRE-2009-0469 [ Links ]
14. Facchin P, Rosa-Rizzotto M, Visonà Dalla Pozza L, Turconi AC, Pagliano E, Signorini S, Tornetta L, Trabacca A, Fe-drizzi E, GIPCI Study Group. Multisite trial comparing the efficacy of constraint-induced movement therapy with that of bimanual intensive training in children with hemi-plegic cerebral palsy: postintervention results. Am J Phys Med Rehabil. 2011;90(7):539-553. https://doi.org/10.1097/PHM.0b013e3182247076 [ Links ]
15. Sakzewski L, Ziviani J, Abbott DF, Macdonell RAL, Jackson GD, Boyd RN. Randomized trial of constraint-induced movement therapy and bimanual training on activity outcomes for children with congenital hemiplegia. Dev Med Child Neurol. 2011;53(4):313-320. https://doi.org/10.1111/j.1469-8749.2010.03859.x [ Links ]
16. Kasehagen B. Constraint Induced Movement Therapy. Physiopedia. Accessed April 28, 2022. https://www.physio-pedia.com/Constraint_Induced_Movement_Therapy [ Links ]
17. Page SJ, Levine P, Sisto S, Bond Q, Johnston MV. Stroke patients' and therapists' opinions of constraint-induced movement therapy. Clin Rehabil. 2002;16(1):55-60. https://doi.org/10.1191/0269215502cr473oa [ Links ]
18. Aarts PB, Jongerius PH, Geerdink YA, van Limbeek J, Geurts AC. Effectiveness of modified constraint-induced movement therapy in children with unilateral spastic cerebral palsy: a randomized controlled trial. Neurorehabil Neural Repair. 2010;24(6):509-518. https://doi.org/10.1177/1545968309359767 [ Links ]
19. Sullivan L. Power and sample size determination. In: Essentials of Biostatistics in Public Health. Jones & Bartlett Learning; 2012:169-188. Accessed June 30, 2020. https://publish.jblearning.com/index.php?mod=jbbrow-se&act=book_details&id=1054 [ Links ]
20. Christie LJ, McCluskey A, Lovarini M. Constraint-induced movement therapy for upper limb recovery in adult neurorehabilitation: An international survey of current knowledge and experience. Aust Occup Ther J. 2019;66(3):401-412. https://doi.org/10.1111/1440-1630.12567 [ Links ]
21. Fritz SL, George SZ, Wolf SL, Light KE. Participant perception of recovery as criterion to establish importance of improvement for constraint-induced movement therapy outcome measures: a preliminary study. Phys Ther. 2007;87(2):170-178. https://doi.org/10.2522/ptj.20060101 [ Links ]
22. Dickerson AE, Brown LE. Pediatric constraint-induced movement therapy in a young child with minimal active arm movement. Am J Occup Ther? 2007;61(5):563-573. https://doi.org/10.5014/ajot.61.5.563 [ Links ]
23. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun. 2015;30(6):566-576. https://doi.org/10.1080/10410236.2013.873363 [ Links ]
24. Kwakkel G, Veerbeek JM, van Wegen EEH, Wolf SL. Constraint-induced movement therapy after stroke. Lancet Neurol. 2015;14(2):224-234. https://doi.org/10.1016/S1474-4422(14)70160-7 [ Links ]
25. Uswatte G, Taub E, Morris D, Barman J, Crago J. Contribution of the shaping and restraint components of Constraint-Induced Movement therapy to treatment outcome. NeuroRehabilitation. 2006;21(2):147-156. [ Links ]
26. Taub E, Miller NE, Novack TA, Cook EW, Fleming WC, Nepomuceno CS, Connell JS, Crago JE. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil. 1993;74(4):347-354. [ Links ]
Submitted: 4 May 2022
1st Review: 24 June 2022
Revised: 1 July 2022
Accepted: 5 July 2022
Corresponding author: Pragashnie Govender naidoopg@ukzn.ac.za
EDTOR: Blanche Pretorius
DATA AVAILABILITY: Upon reasonable request from corresponding author.
FUNDING: Velisiwe Zodwa Mbuyisa received tuition remission from the University of KwaZulu-Natal towards completion of this study.















