Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.52 n.1 Pretoria Apr. 2022
http://dx.doi.org/10.17159/2310-3833/2022/vol52n1a8
RESEARCH ARTICLE
Wheelchair prescription after spinal cord injury: satisfaction and functional mobility
Nadine WolfI; Lebogang MasekoII; Denise FranzsenIII; Patricia Ann de WittIV, *
IBSc OT (Wits), MSc OT (Wits). https://orcid.org/0000-0002-6053-3816; Occupational therapist, Locum at Zenzala Occupational Therapists, Postgraduate student, Department of Occupational Therapy, School of Therapeutic Sciences, Faculty of Health Sciences University of Witwatersrand, Johannesburg, South Africa
IIBSc OT (Wits), MPH (Wits). https://orcid.org/0000-0002-6126-5104; Lecturer, Department of Occupational Therapy, School of Therapeutic Sciences, Faculty of Health Sciences University of Witwatersrand, Johannesburg, South Africa
IIIBSc OT (Wits), MSc OT (Wits), PhD (Wits), DTH(UP). https://orcid.org/0000-0001-8295-6329; Sessional Senior lecturer, Department of Occupational Therapy, School of Therapeutic Sciences, Faculty of Health Sciences University of Witwatersrand, Johannesburg, South Africa
IVDOT (UP), MSc OT (Wits), PhD (Wits). https://orcid.org/0000-0003-3612-0920; Sessional Adjunct Professor, Department of Occupational Therapy, School of Therapeutic Sciences, Faculty of Health Sciences University of Witwatersrand, Johannesburg, South Africa
ABSTRACT
INTRODUCTION: Globally, rehabilitation services aim to address activity limitations and participation restrictions for those with mobility issues. Therefore, the prescription of wheelchairs is integral to the work of rehabilitation professionals, particularly occupational therapists. The dearth of research in South Africa necessitated this study into wheelchair prescription, satisfaction with and the functional mobility in the prescribed wheelchairs for individuals with spinal cord injury
METHOD: A cross sectional, descriptive, non-experimental research design was used to collect data from 40 participants using a demographic questionnaire, the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) 2.0 and Wheelchair Users Functional Assessment (WUFA). The data were analysed descriptively to determine the satisfaction with and the functional mobility in the wheelchair as well as the association between these variables. The influence of involvement in the prescription of the wheelchair, the type of wheelchair prescribed on satisfaction and the functional mobility in the wheelchair were also considered
RESULTS: Of the 40 participants, 34 (85%) were prescribed rigid-frame wheelchairs and only six participants (15%) received folding frame wheelchairs. Over 87.98% of the participants had a high level of satisfaction with their prescribed wheelchair and 84.82% reported being functionally mobile in their wheelchairs. High involvement in the prescription of the wheelchair resulted in higher scores for both satisfaction and functional mobility
CONCLUSION: This study concluded that a rigid-frame wheelchair facilitated functional mobility in individuals with SCI in the South African context. The greater the involvement of participants in the wheelchair prescription process, the higher their satisfaction with their wheelchair and functional mobility, indicating the importance of client-centeredness in wheelchair prescription in occupational therapy
Key words: wheelchair mobility, rigid-frame wheelchair, client-centeredness, involvement in prescription, wheelchair fit, private rehabilitation healthcare
INTRODUCTION AND LITERATURE REVIEW
In 2017, Joseph et al.1 estimated that the incidence for traumatic spinal cord injury (SCI) was 75.6 per million persons in South Africa. It was reported that assault was the main cause of SCI (60%), followed by motor vehicle and pedestrian accidents (26%) and falls (12%)2. There are no reliable reports on the number of individuals living with non-traumatic SCI in this country1.
The South African Integrated Disability Management and Rehabilitation Pathway document indicates that individuals with SCI should receive adequate acute care, followed by 15 to 90 days of high-intensity inpatient rehabilitation as well as appropriate outpatient care3. Assistive technology, most commonly a wheelchair, should be provided3. Post SCI, the prescription of a wheelchair ensures mobility, the fulfilment of individualised goals, facilitation of community integration and social participation4. Individuals with SCI have expressed the need to be seen as equals in society5 and this can be facilitated by an appropriately prescribed wheelchair which enables participation in the range of personally desired activities, roles and responsibilities6,7.
The client-centred occupational therapy wheelchair prescription process with clients with SCI routinely starts with an assessment. Using the International Classification of Functioning, Disability and Health framework (ICF)8, impairments, activity demands, participation, environmental barriers and resources as well as personal factors such as the client's level of motivation and personality need to be considered. This should also be accompanied by a seating assessment9. In this assessment note should be taken of the factors that influence the participation of individuals with SCI in all aspects of everyday life within their specific socio-cultural context5. Amongst these factors are the client's physical abilities, their occupational performance needs, and the available wheelchair technology. A detailed description of the environment within which the wheelchair will be used10 and the attitude of their community towards disability need to be taken into account5.
Funding is one of the constraints faced in the provision of wheelchairs suited to individual clients' needs. This is evident particularly in developing countries but also in developed countries where health insurers and medical funders are demanding high level evidence to support the need for appropriate wheelchairs9. There is an increasing demand for the use of outcome measures to determine the functional requirements of wheelchairs during prescription to motivate for appropriate wheelchairs11. Due to budget cuts, requests for specialised wheelchairs are often rejected, in both the private and public health sectors12. As a result, clients often have to settle for a more 'affordable' wheelchair, with which they are often dissatisfied and that limits their mobility, thus placing them at risk of abandoning the wheelchair when it does not meet their needs13,14.
A cause of abandonment of wheelchairs associated with clients with SCI was reported to be the lack of client involvement in the wheelchair prescription7,15. Equally important to abandonment was the incompatibility of the wheelchair to the environment in which it has to be used16. Studies where wheelchairs have been prescribed without consideration of the environment have found that such wheelchairs are unable to withstand the terrain, resulting in damage and thus abandonment. Individuals with SCI are often faced with environmental barriers such as poor access to public transportation and poor access to buildings or sidewalks as the ramps, if provided, were not suitable for wheelchairs17,18. Faced with these barriers, wheelchair users become frustrated since improving the public environment accessibility may take years to be addressed14,15.
Low self-esteem and poor self-image were also found to be correlated to a poorly fitted wheelchair resulting in poor posture in the wheelchair, making the wheelchair user appear even more disabled, further exacerbating their difference in relation to others4,19. Hence, the wheelchair needs to be aesthetically pleasing to the client as supported by Krantz7. He indicated that wheelchair users felt that the appearance, design and aesthetics of the wheelchair should be emphasized as it enhanced their self-esteem and made them feel more confident in the wheelchair. Over 75% of wheelchair prescribers reportedly do not view the colour and design of the wheelchairs as important factors in the wheelchair prescription process, which may contradict the view of wheelchair users7. This highlights the significance of promoting mental wellbeing in clients with SCI, an aspect which is often overlooked during the wheelchair prescription process6.
Physical complications associated with SCI further highlight the importance of considering a client's physical characteristics - such as spinal deformities, pressure ulcers, pain, discomfort and as well as mental health issues such as depression21 in the wheelchair prescription process20. The wheelchair as an assistive device should reduce the risk of such complications rather than exacerbate them22. It is therefore important that the wheelchair together with the pressure cushion decrease the risk of developing pressure sores and postural deformities19,23. A poor posture in the wheelchair may also result in poor positioning of the head and trunk which reduces effective social interaction as well upper limb functioning, making it more difficult for the wheelchair user to propel themselves effectively in the wheelchair as well as participate in daily life tasks19,23.
If the prescribed wheelchair is found to be inappropriate, community reintegration and quality of life can be compromised10 with limited independence in activities of daily living (ADLs), instrumental activities of daily living (IADLs) and the ability to return to work20. International and local research therefore stress the importance of the prescription of a wheelchair that is not only appropriate to the nature of the disability of the client with SCI but that it also best serves their functional mobility needs and supports their quality of life.
Although checklists for wheelchair-seating guidelines and a wheelchair specification24 are available in South Africa to assist with providing evidence-based wheelchair prescription, there is still limited research to support client involvement in this process, as well as evidence to verify the effectiveness of assistive devices. Therapists are under pressure to provide objective outcomes, which include satisfaction with and the ability to use a wheelchair to mitigate the negative consequences of SCI and ensure appropriate use of the device20. There is a paucity of research regarding the outcomes of assistive device use, thus, the current study aimed to investigate the satisfaction with and the functional mobility in the wheelchair of individuals with SCI rehabilitated in the private healthcare sector in South Africa. Furthermore, the study also examined whether involvement of the individual in their wheelchair prescription process and the type of wheelchair prescribed influenced their satisfaction and functional mobility.
METHODS
Research design
A cross sectional, descriptive, non-experimental research design was used. The research site was a Johannesburg private rehabilitation hospital, for clients needing physical rehabilitation, particularly those with a SCI. Total population purposive sampling was used. All SCI clients over 18 years who were classified within the American Spinal Injury Association (ASIA) Impairment Scale of A (complete impairment), B (incomplete with sensory but not motor impairment), C (incomplete with motor impairment with muscle strength less than Grade 3 below the lesion level) and D (incomplete with motor impairment with muscle strength greater than Grade 3 below the lesion level) and who had been prescribed a manual (non-motorised) wheelchair were invited to participate. All participants had used their wheelchair for three months or more. Ethical clearance from the Human Research Ethics of the University of the Witwatersrand (M 130937) and relevant permissions and informed consent were obtained prior to data collection.
Measurement Tools and procedure
Data were collected using a demographic questionnaire, The Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) 2.0 and the Wheelchair Users Functional Assessment (WUFA)
A demographic questionnaire gathered participant information including age, gender, level of injury, the ASIA Impairment Scale, where the wheelchair was prescribed, the length of time using the wheelchair, the level of client's involvement in the wheelchair prescription process, whether a seating assessment was carried out, supply of a wheelchair cushion, modifications to the wheelchair as well as financing of the wheelchair.
The Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) 2.0
The QUEST 2.0, a self-report measure, was used to investigate the satisfaction of participants with their prescribed wheelchairs25. The QUEST 2.0 was divided in two parts: eight items relate to the assistive device (summed to provide a Device score) and four items relate to the services that were provided (summed to provide a Service score). Each question in the QUEST 2.0 was scored on a five-point satisfaction scale; where one denotes 'not satisfied at all' and five "very satisfied"20. Finally, the participants were required to prioritise the three most important aspects influencing their satisfaction from a list of twelve items20. An international content validation on the QUEST 2.0 found that the test was sufficiently sampled according to the different dimensions of satisfaction with assistive devices25. The content validity was evaluated by experts25. Inter-rater reliability of the QUEST 2.0 was assessed and correlation coefficients were found to be ICC=0.89, 0.76 and 0.91, which showed substantial reliability25.
Wheelchair Users Functional Assessment (WUFA)
The WUFA was used to assess clients' functional mobility in the wheelchair as well as the navigation of potential obstacles in the community26. The tool consisted of thirteen items/tasks, which included: pushing through a tight space, uneven terrain, door management, street crossing, ramp, curb, bed transfer, toilet transfer, floor transfer, bathing, upper and lower dressing, reaching function and picking up objects/sweeping.
For the purpose of this study some sections - bathing, dressing and sweeping - were omitted from the questionnaire, as they were not relevant to the aim and objectives of the study. Validity and reliability have been shown not to be affected through the omission of these three sections26. The scoring of the level of independence that the client achieved on each of the subsections ranged from one (completely dependent), to seven, (completely independent)26. Each of the ten WUFA subsections included were scored and then all subsections were summed to calculate a total score. For this study a maximum score of 70 points could be obtained by the participants.
Content validity was established through a panel of six experienced physiotherapists for the 13-item test. Interrater and intra-rater reliability was determined and found to be adequate for the WUFA26. A high internal consistency (standardized coefficient alpha=0.96) has been established for the WUFA26.
Research procedure
All participants completed the demographic questionnaire and the QUEST 2.0 as a self-report. An occupational therapy technician (OTT) was available to assist with translation of instructions into one of the African languages where required. A pilot study determined the appropriate angles at which the video recording would capture adequate footage to allow for analysis on the WUFA. Each aspect of the data collection was then conducted in an appropriate environment, beginning with the indoor based tasks, followed by the outdoor tasks. In this study, the researcher set up the tasks and each participant was video recorded during data collection for the WUFA. Another experienced occupational therapist, who had not treated any of the participants, rated the participants' performance from the video footage and scored the WUFA to avoid researcher bias.
Data analysis
The demographic data were analysed descriptively. The data obtained from the QUEST 2.0 and the WUFA were analysed using frequency distributions and descriptive statistics, since the data were ordinal. A Spearman's correlation coefficient was used to determine the association between the participants' satisfaction with their wheelchairs and their functional mobility. The difference between the clients' satisfaction with their prescribed wheelchairs and their functional mobility in daily life based on their involvement in the prescription of the wheelchair was investigated using a Kruskal-Wallis test. Differences in satisfaction with the wheelchair and functional mobility were determined according to the type of wheelchair (rigid-frame wheelchair or folding frame wheelchair) prescribed using a Mann Whitney U test and Cohen d effect sizes.
RESULTS
Forty participants were recruited to participate in the study (Table I, above). The participants were mostly males (70%) and below the age of 50 years (90%). The injuries ranged from the level of C7 to L5 and a large proportion of the study sample (65%) had been using their wheelchair for less than a year. Sixty five percent of the participants were highly involved in the prescription of their chairs while just over 12% had had no involvement and 42.5% had their wheelchairs funded by medical aids. Most participants (85%) were prescribed a rigid-frame wheelchair.
The majority of the 40 participants (87.50%; n=35) reported they had a seating assessment along with the prescription of their wheelchair. Three participants stated that they did not receive a cushion with their wheelchair as they already had a cushion bought at a different stage to the purchase of theirwheelchair(7.8%) Of the total study sample, 90% received specific modifications to their wheelchair, among these 85% (n=34) were modifications to the backrest, 22.5% (n=9) to the armrest and 77.5% (n=31) to the footplates. None of the demographic variables showed any significant difference according to satisfaction with the wheelchair or functional mobility.
Satisfaction with wheelchair
The participants' satisfaction levels with the wheelchair assessed using the QUEST 2.0, indicated that most of the participants were very satisfied with the wheelchair that was prescribed for them. All eight aspects of the QUEST 2.0 were scored 'very satisfied' by more than 50% of the participants (Figure 1, above). One participant reported dissatisfaction with the ease of adjusting the wheelchair, the security as well as the comfort in the wheelchair. Between 5% (n=2) and 7.5% (n=3) participants were dissatisfied with the weight and durability of their wheelchair.

Functional mobility in wheelchair
The average WUFA score in this study was 84.82% which indicated that the participants were functionally mobile in their wheelchairs. Figure 2 (page 73) shows that in four out of the ten tasks, participants were completely independent: in navigating tight spaces, uneven terrain and ramps and they were independent in the functional tasks (reaching, lifting, carrying, and pouring) while for the remaining six tasks, the scores varied.

Although some of the participants were completely dependent in these aspects, participants mainly struggled with management of doors, street crossing, curbs, bed transfers, toilet transfers and floor transfers. Although there was no significance in the scores by the level of their lesion or length of time using a wheelchair, participants with higher lesions had less independence in functional mobility.
Association between satisfaction with their wheelchair and functional mobility
Very low correlations, with scores ranging from r = -0.21 to 0.28, indicated no significant association between the participants' satisfaction with their wheelchair and their functional mobility.
Effect of the level of involvement in the wheelchair prescription on satisfaction with the wheelchair and functional mobility
As can be seen from Table II (above) the only significant difference was for total QUEST 2.0 score and the levels of involvement in the prescription process (p=0.05). The participants who were highly involved in the prescription of their wheelchairs had the highest mean total QUEST 2.0 scores indicating they were significantly more satisfied with their wheelchairs.
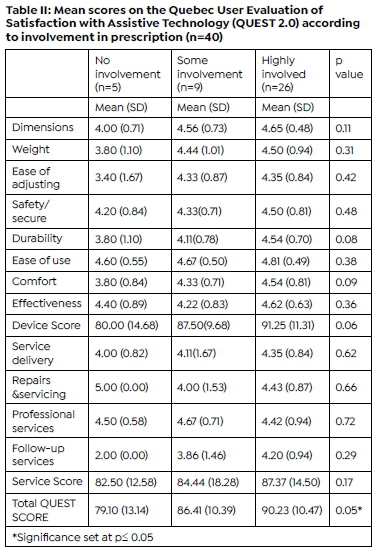
There was no significant difference in the involvement in the prescription of the wheelchair and the participants' functional mobility. However, those who were highly involved in the prescription of their wheelchairs scored higher than those who had some involvement. Those who had no involvement obtained the lowest WUFA scores (Table III, above).

Differences for satisfaction with the wheelchair and functional mobility according to type of wheelchair
All mean scores for the QUEST 2,0 (with the exception of the items 'safe and secure' and 'professional services') were higher for participants who were prescribed a rigid-frame wheelchair. There was a significant difference for all the items and the total WUFA score between the two groups, but the small effect sizes indicated little clinical significance according to the type of wheelchair (rigid-frame wheelchair or folding frame wheelchair) prescribed (Table IV page 73).
DISCUSSION
Literature indicates that males are most at risk of SCI in young adulthood (20-40 years)27, which is consistent with the current study, which included more male to female young adults. Most participants reported SCI between the levels of T10 and T12 which concurs with the study by Joseph et al.1. Participants in this study were conveniently recruited from the rehabilitation records at the research site and as a consequence, the majority had only used their wheelchair for 12 months or less. Rehabilitation for a year post SCI is consistent with other studies28 and commonly includes a seating assessment29. Most participants reported having had a seating assessment prior to the prescription of their wheelchair. Studies have emphasised the promotion of optimal seating postures which should be achieved by a seating assessment, to reduce the risk of pressure ulcers and allow optimal functionality in the wheelchair13,21. The prescription of an ideal cushion and an appropriate wheelchair are key outcomes of the seating assessment30.
The fact that nearly half the wheelchairs of participants were funded by their medical aid and a fifth from other medical funding sources such as Workmen's Compensation (WCA) or Rand Mutual Assurance (RMA) was not unexpected as the research site was a private sector hospital where service delivery is funded by medical insurance. The availability of medical funding may also account for the fact that most participants had more expensive fixed-frame wheelchairs31 although some of participants had to supplement the amount permitted by medical funders to get the wheelchair indicated as best for their needs.
Satisfaction with wheelchair
The results of the Quest 2.0 reported that most of participants were more than 'quite satisfied' with the dimensions and ease of use with their wheelchair. This concurs with the study by Bergstrom and Samuelsson32 who also found that the greatest level of satisfaction with a wheelchair using the QUEST 2.0 was for the ease of use. Most of the participants scored above 'quite satisfied' with their wheelchair attributes (weight, safety and security, durability, comfort and effectiveness). These results suggest that the needs of participants were considered when the wheelchair was prescribed, since most had had a seating assessment prior to the wheelchair prescription, which contributed to their satisfaction level.
Most of the participants in the study also received specific modifications to their wheelchairs, indicating that the therapists who prescribed the wheelchairs in this study regarded adjustments as an integral part of an appropriate wheelchair prescription. Specific modifications to the wheelchair have been shown to be a vital part of wheelchair prescription as evidence has shown that poor seating ergonomics (poor fit) can result in secondary complications post injury, such as back pain, postural deformities, pressure sores and shoulder injuries20. Giesbrecht et al.33 supported the need for modifications but their participants with SCI reported a higher level of satisfaction when the prescribed wheelchair had appropriate modifications to the backrest, footrests and cushion than in the current study. However, more participants were 'quite' to 'very satisfied' with the ease and effectiveness of the wheelchair, once modified, in achieving their daily tasks in this study. These modifications resulted from appropriate wheelchair prescription.
The level of satisfaction with comfort was of concern to participants as many viewed comfort as a critical factor in the prescription of a wheelchair. Ease in adjusting the wheelchair was the only characteristic that scored 'not satisfied at all'. This may be due to the fact that most participants had rigid-frame wheelchairs which are reported to be difficult to take apart and be transported in a car34.
The second part of the QUEST 2.0 measured the clients' satisfaction with the services provided by the rehabilitation team and the suppliers. This part recorded lower satisfaction levels than for the wheelchair, but overall a higher level of satisfaction with the services than the study by Bergstrom and Samuelsson32.They reported that only 55% of their participants were 'fully satisfied' with the follow-up services provided, compared to 74% of participants in this study. This result should be considered in light of the fact that 65% of participants in the current study had used the wheelchair for between 6 and 12 months so had had little opportunity to make use of follow-up services.
Functional mobility in the wheelchair
Overall, the study sample was functionally mobile in their wheelchairs, and regardless of wheelchair type, were able to demonstrate independence in propelling through tight spaces, manoeuvring the wheelchair across uneven terrain, as well as carrying out functional tasks including reaching, carrying, lifting, and pouring. Although not significantly different, the participants that had more experience were better able to demonstrate complete independence in tasks such as opening and closing doors, and transfer on/ off a bed. This was supported by one study that indicated participants' wheelchair skills increased when assessed 12 months post-discharge35.
Association between satisfaction levels and functional mobility in the wheelchair
The lack of association between the satisfaction levels of the participants and their independence in functional tasks was supported by de Groot et al.36 and Rushton et al.37 where no correlation between manual wheelchair users' satisfaction and their participation in their active lifestyle was found. A reason for the poor relationship between satisfaction and function in the wheelchair in the current study may be the fact that all participants were mostly satisfied with their wheelchairs although they were still dependent in four areas of functional mobility. This again may reflect the short duration of wheelchair use since other studies have reported participants generated higher satisfaction levels when they had increased self-efficacy due to their ability to demonstrate a high level of wheelchair skills. These studies however considered wheelchair users one year after injury and many different diagnoses35,38.
Satisfaction and mobility - involvement in prescription
The current study confirmed the findings of previous studies that client participation in wheelchair prescription resulted in higher satisfaction and better functional outcomes and thus a better quality of life4,29. A high total mean score for the WUFA and a high average score for the QUEST 2 was found for the participants who were highly involved in wheelchair prescription in the current study. No participants reported abandoning their wheelchairs as in other studies despite some participants not being fully satisfied because on the whole, the wheelchairs appeared to meet participants' needs, enabled access to the community demands, and met their preferences15,16.
Customisation of a wheelchair for improved satisfaction is supported by the work of Samuelsson, et al.20 which considers the importance of biomechanical properties, as well as the environment in which the wheelchair is used39. This is especially relevant in South Africa where the context and infrastructure are not always wheelchair friendly16. Thus, a wheelchair that is durable and able to handle these contextual challenges is critical. In this study rigid-frame wheelchairs were the most common wheelchairs prescribed which concurs with a report in the literature that fixed-frame wheelchairs are more durable and are better able to withstand rougher terrain40.
Effect of type of wheelchair on satisfaction and mobility
Participants in this study perceived comfort to be the most important factor in choosing a wheelchair followed by safety, ease of use and weight of the wheelchair. This is consistent with the work by Bergstrom and Samuelsson32 who also reported comfort and ease of use as critical factors in the prescription of a wheelchair.
Literature reports that the type of wheelchair frame has implications for the participants' functional mobility34. In this study users of a rigid-frame wheelchairs scored better on mobility than users with a folding frame wheelchair. This was similar to findings of Liu et al.34 where the more compact fixed-frame wheelchairs allowed for better manoeuvrability than the larger folding ones. In the current study there were significant differences between four subtests and the total WUFA score for wheelchair type where the participants in folding frame wheelchairs had greater difficulty in going through the door and opening and closing the door due to the greater turning circle needed for these folding wheelchairs. Street crossings, curbs and transfers were also significantly affected by the type of wheelchair due to issues with tipping the folding wheelchairs and the height difference between wheelchair and transfer surface being greater than for rigid-frame wheelchairs41.
The demographic profile of the participants as suggested by Fliess-Douer et al.35 may also affect the ability to transfer since of the nine participants who were able to execute a floor transfer independently, seven had a low level of injury, i.e., between T10-T12 and L1-L5. Age as well as length of time the participants had used a wheelchair did not play a significant role in the current study.
Implications for clinical practice
The current study showed that almost half of the participants viewed the weight of the wheelchair as an important factor to consider when prescribing a wheelchair. This is in contrast to the findings of Bergstrom and Samuelsson32, who found that the weight of the wheelchair was not considered an important factor. It must therefore be accepted that in the South African context the weight of the wheelchair should also be considered as important when prescribing a wheelchair. Wheelchair weight may have been considered an important factor by the participants of this study due to lack of accessible public transport. Thus, the need to load and unload a wheelchair into a motor vehicle makes wheelchair weight an important factor in wheelchair prescription42.
Safety was the second most important aspect identified in the study when prescribing a wheelchair. This was strongly associated with the participants' level of satisfaction with follow up services and service delivery. There was no other published research that could be found that supports this finding. This relationship may be due to participants feeling safer in a wheelchair that has efficient, effective, and reliable follow-up services. This finding does, however, require further investigation.
The factors that the clients consider important in the wheelchair prescription process will lead to an overall higher satisfaction with the wheelchair as well as the services being provided, as stated in this study. Determining a client's overall satisfaction with the wheelchair prescription needs to be part of general practice as it encompasses the client-centred nature of occupational therapy.
Limitations to the study
While the QUEST 2.0 was simple to administer, the WUFA had prescribed environmental structures, such as the ramp and curb, which needed to conform to standardised measurements. While the outcome measure is valid, the administration proved impractical in a developing country where infrastructure does not meet first world standards. Alternative outcome measures such as the Wheelchair Outcome Measure (WhOM), the Functioning Every Day with a Wheelchair Questionnaire (FEW- Q) and the Wheelchair Skills Test (WST) were excluded as they had even stricter rules of administration than the WUFA11.
The small sample size may have resulted in the lack of significance when demographic factors were analysed in relation to the other study outcomes. Another limitation was that participants of the study were recruited from a single private sector rehabilitation facility and therefore the results cannot be generalised to persons with SCI in other settings.
CONCLUSION
The results of the current study clearly indicate that when prescribing a wheelchair, the individual needs and requirements of wheelchair users should be taken into account. For some, comfort and ease of use will be important while for others, the weight of the wheelchair and the safety in the chair are more important. In addition, the results suggest that involving the clients in wheelchair prescription results in a higher level of satisfaction, supporting importance of client-centred wheelchair prescription.
Assessing a client's functional mobility in the wheelchair is critical to determine whether the client can actively participate in activities and whether the wheelchair is enhancing or limiting their function. This is essential in the occupational therapy context where function and a satisfactory quality of life are the primary goals.
The use of outcome measures in assessing clients' functional mobility in the wheelchair provides an objective means of measuring improvement through intervention. The QUEST 2.0 has shown to be a useful instrument for use during the prescription of a wheelchair as it facilitates a client-centred approach and should be considered as part of general practice when treating patients with SCI.
ACKNOWLEDGEMENTS
Permission to use the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) 2.0 was granted by Louise Demers the developer of this instrument.
DATA AVAILABILITY STATEMENT
Raw data are available on request from Denise Franzsen.
DECLARATION OF CONFLICTING INTERESTS AND FUNDING DECLARATION
The authors declare that there are no conflicts of interest or funding received for this study.
AUTHOR CONTRIBUTIONS
Nadine Wolf, was a postgraduate student who conceptualised the study and completed data collection and analysis and interpretation of data. Lebogang Maseko and Denise Franzsen supervised the study, provided guidance for analysis and interpretation of data. Denise Franzsen analysed the data and with Lebogang Maseko and Patricia de Witt conceptualised, updated and wrote the article.
REFERENCES
1. Joseph C, Scriba E, Wilson V, Mothabeng J, Theron F. People with Spinal Cord Injury in Republic of South Africa. American Journal of Physical Medicine and Rehabilitation. 2017;96(2):S109-S111. doi:https://doi.org/10.1097/PHM.0000000000000594. [ Links ]
2. Joseph C, Delcarme A, Vlok I, Wahman K, Phillips J, Nilsson Wikmar L. Incidence and aetiology of traumatic spinal cord injury in Cape Town, South Africa: A prospective, population-based study. Spinal Cord. 2015;53(9):692-696. doi:https://doi.org/10.1038/sc.2015.51. [ Links ]
3. Department of Health. Integrated Disability Management and Rehabilitation Pathway of Care: A Life Course Perspective. Pretoria; 2015. [ Links ]
4. Cooper RA, Ferretti E, Oyster M, Kelleher A, Cooper R. The relationship between wheelchair mobility patterns and community participation among individuals with spinal cord injury. Assistive Technology. 2011;23(3):177-183. https://doi.org/10.1080/10400435.2011.588991. [ Links ]
5. Joseph C, Wahman K, Phillips J, Wikmar LN. Client perspectives on reclaiming participation after a traumatic spinal cord injury in South Africa. Physical Therapy. 2016;96(9):1372-1380. doi:https://doi.org/10.2522/ptj.20150258 [ Links ]
6. Gowran RJ, Clifford A, Gallagher A, McKee J, O'Regan B, McKay EA. Wheelchair and seating assistive technology provision: a gateway to freedom. Disability and Rehabilitation. 2020. doi:https://doi.org/10.1080/09638288.2020.1768303 [ Links ]
7. Krantz O, Provision of Active Wheelchairs in Relation to Person-Centered Care and Health Literacy in: Henderson KR (ed) Wheelchairs: Perceptions, Technology Advances and Barriers, Nova Science Publishers, Inc., 2016 [ Links ]
8. World Health Organisation. The International Classification of Functioning, Disability and Health. 2001. doi:https://doi.org/10.1097/01.pep.0000245823.21888.71 [ Links ]
9. Lukersmith S, Radbron L, Hopman K. Development of clinical guidelines for the prescription of a seated wheelchair or mobility scooter for people with traumatic brain injury or spinal cord injury. Australian Occupational Therapy Journal. 2013;60(6):378-386. doi:https://doi.org/10.1111/1440-1630.12077 [ Links ]
10. World Health Organisation. Guidelines on the provision of manual wheelchairs in less resourced settings. WHO, Geneva. 2008 [accessed 2021 May 14]. doi:https://www.who.int/publications/i/item/9789241547482 [ Links ]
11. Kenny S, Gowran RJ. Outcome measures for wheelchair and seating provision: a critical appraisal. British Journal of Occupational Therapy. 2014;77(2):67-77. doi:https://doi.org/10.4276/030802214X13916969447119 [ Links ]
12. McIntyre J. Wheelchairs-A human rights issue or a mere mobility device? Personal reflections of an occupational therapist. South African Journal of Occupational Therapy. 2010;40(1):27-31. [ Links ]
13. Shore S, Juillerat S. The impact of a low cost wheelchair on the quality of life of the disabled in the developing world. Medical Science Monitor. 2012;18(9):CR533. doi:https://doi.org/10.12659/MSM.883348. [ Links ]
14. Borg J, Larsson S, Ostergren PO, Rahman AA, Bari N, Khan AN. User involvement in service delivery predicts outcomes of assistive technology use: A cross-sectional study in Bangladesh. BMC Health Services Research. 2012 Dec;12(1):1-0. doi:https://doi.org/10.1186/1472-6963-12-330 [ Links ]
15. Krantz O, Egard H. Use of active wheelchairs in everyday life: experiences among experienced users of active ultra lightweight rigid-frame wheelchairs. Disability and Rehabilitation: Assistive Technology. 2017;12(1):65-72. doi:https://doi.org/10.3109/17483107.2015.1065514 [ Links ]
16. McIntyre J, Cleland KE, Ramklass S. Access to wheelchairs by persons with mobility impairment in a remote rural district of KwaZulu-Natal, South Africa: therapists' perspectives. Rural and Remote Health. 2021;21(1):5855. doi:https://doi.org/10.22605/RRH5855 [ Links ]
17. Unsworth C, So MH, Chua J, Gudimetla P, Naweed A. A systematic review of public transport accessibility for people using mobility devices. Disability and Rehabilitation. 2019 43(16), pp.2253-2267. doi:https://doi.org/10.1080/09638288.2019.1697382 [ Links ]
18. Newman SD. Evidence-based advocacy: Using Photo-voice to identify barriers and facilitators to community participation after spinal cord injury. Rehabilitation Nursing. 2010;35(2):47-59. doi:https://doi.org/10.1002/j.2048-7940.2010.tb00031.x [ Links ]
19. Scheffler E. What is an appropriate wheelchair? Rolling Inspiration. 2009:May-June, 1-20.[accessed 2020.4.12] https://www.wcrc.co.za/docs/34/What%20is%20an%20appropriate%20wheelchair.pdf [ Links ]
20. Samuelsson K, Wressle E. User satisfaction with mobility assistive devices: An important element in the rehabilitation process. Disability and Rehabilitation. 2008;30(7):551-558. doi:https://doi.org/10.1080/09638280701355777 [ Links ]
21. Donnelly B. Code of Practice for Disability Equipment, Wheelchair and Seating Services: A Quality Framework for Procurement and Provision of Services. Troubador Publishing Ltd; 2015. [ Links ]
22. Gallagher A, Cleary G, Clifford A, McKee J, O'Farrell K, Gowran RJ. "Unknown world of wheelchairs" A mixed methods study exploring experiences of wheelchair and seating assistive technology provision for people with spinal cord injury in an Irish context. Disability and Rehabilitation.September 2020 1-3. doi:https://doi.org/10.1080/09638288.2020.1814879 [ Links ]
23. Jones DA, Rader J. Seating and wheeled mobility for older adults living in nursing homes: What has changed clinically in the past 20 years? Topics in Geriatric Rehabilitation. 2015;31(1):10-18. doi:https://doi.org/10.1097/TGR.0000000000000050 [ Links ]
24. Kwa-Zulu Natal Department of Health. Wheelchair Service Delivery Programme. 2010.[accessed 2018.3.24] https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwj83MKrgb30AhXpQkEAHTCWCbwQFnoECB0QAQ&url=http%3A%2F%2Fwww.kznhealth.gov.za%2Fdisability%2Fpolicy%2F2010%2520June%2520KZN%2520Wheelchair%2520policy%2520draft.doc&usg=AOvVaw2BumF_wV7VNZpE0OhFht9k. [ Links ]
25. Demers L, Weiss-Lambrou R, Ska B. The Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0): An overview and recent progress. Technology and Disability. 2002;14(3):101-105. doi:https://doi.org/10.3233/tad-2002-14304 [ Links ]
26. Stanley RK, Stafford DJ, Rasch E, Rodgers MM. Development of a functional assessment measure for manual wheelchair users. Journal of Rehabilitation Research and Development. 2003;40(4):301-307. doi:https://doi.org/10.1682/JRRD.2003.07.0301 [ Links ]
27. Sidon E, Stein M, Ramalingam G, Shemesh S, Benharroch D, Ohana N. Gender Differences in Spinal Injuries: Causes and Location of Injury. Journal of Women's Health. 2018;27(7):946-951. doi:https://doi.org/10.1089/JWH.2017.6687 [ Links ]
28. Whiteneck G, Gassaway J, Dijkers MP, Heinemann AW, Kreider SED. Relationship of patient characteristics and rehabilitation services to outcomes following spinal cord injury: The SCIRehab Project. 2013;35(6):484-502. doi:http://dx.doi.org/10.1179/2045772312Y.0000000057. [ Links ]
29. Digiovine CP, Koontz AM, Berner TF, Kim DJ, Schmeler M, Cooper R, Cooper RA. Wheelchairs and Seating Systems. Braddom's Physical Medicine and Rehabilitation. 2021:261-290.e2. doi:https://doi.org/10.1016/B978-0-323-62539-5.00014-X [ Links ]
30. Lo L, Hebert D, Colquhoun H. Measuring practice gaps in the delivery of evidence-based seating assessments: a retrospective chart review. Disability and Rehabilitation: Assistive Technology. 2019;16(3):255-261. doi:https://doi.org/10.1080/17483107.2019.1672814 [ Links ]
31. Long D. Wheelchair prescription. In: Taktak A, Ganney P, Long D, Axell R, editors. Clinical Engineering : A Handbook for Clinical and Biomedical Engineers Pages. 2nd ed. 2020. p. 411-429. [ Links ]
32. Bergström A, Samuelsson K. Evaluation of manual wheelchairs by individuals with spinal cord injuries. Disability and Rehabilitation. Assistive technology. 2006;1(3):175-182. doi:https://doi.org/10.1080/17483100600573230 [ Links ]
33. Giesbrecht EM, Smith EM, Mortenson W Ben, Miller WC. Needs for mobility devices, home modifications and personal assistance among Canadians with disabilities. Health Reports. 2017;28(8):9-15. [ Links ]
34. Liu HY, Pearlman J, Cooper R, Hong EK, Wang H, Salatin B, Cooper RA. Evaluation of aluminum ultralight rigid wheelchairs versus other ultralight wheelchairs using ANSI/RESNA standards. Journal of Rehabilitation Research and Development. 2010;47(5):441-456. doi:https://doi.org/10.1682/JRRD.2009.08.0137 [ Links ]
35. Fliess-Douer O, van Landewijck Y, Post M, van der Woude L, de Groot S. Wheelchair skills performance between discharge and one year after inpatient rehabilitation in hand-rim wheelchair users with spinal cord injury. Journal of Rehabilitation Medicine. 2013;45(6):553-559. doi:https://doi.org/10.2340/16501977-1152 [ Links ]
36. de Groot S, Post MWM, Bongers-Janssen HMH, Bloemen-Vrencken JH, van der Woude LH V. Is manual wheelchair satisfaction related to active lifestyle and participation in people with a spinal cord injury? Spinal Cord 2011 49:4. 2010;49(4):560-565. doi:https://doi.org/10.1038/sc.2010.150 [ Links ]
37. Rushton PW, Miller WC, Mortenson WB, Garden J. Satisfaction with participation using a manual wheelchair among individuals with spinal cord injury. Spinal Cord. 2010;48(9):691-6. doi:https://doi.org/10.1038/sc.2009.197 [ Links ]
38. Paulisso DC, Schmeler MR, Schein RM, Allegretti ALC, Campos LCB, Costa JD, Fachin-Martins E, Cruz DMC da. Functional mobility assessment is reliable and correlated with satisfaction, independence and skills. Assistive Technology. 2019. doi:https://doi.org/10.1080/10400435.2019.1629125 [ Links ]
39. Visagie S, Scheffler E, Schneider M. Policy implementation in wheelchair service delivery in a rural South African setting. African Journal of Disability. 2013;2(1). doi:https://doi.org/10.4102/ajod.v2i1.63 [ Links ]
40. Visagie S, Duffield S, Unger M. Exploring the impact of wheelchair design on user function in a rural South African setting. African Journal of Disability. 2015;4(1). doi:https://doi.org/10.4102/ajod.v4i1.171. [ Links ]
41. Batavia M. The Wheelchair Evaluation: A Clinician's Guide: A Clinician's Guide The Wheelchair Evaluation: A Clinician's Guide: A Clinician's Guide. 2nd ed. Burlington: Jones & Bartlett Learning; 2010. [ Links ]
42. Kett M, Cole E, TurnerJ. Disability, mobility and transport in low-and middle-income countries: a thematic review. Sustainability. 2020;12(2):589. doi:https://doi.org/10.3390/su12020589. [ Links ]
* Corresponding Author: Patricia Ann de Witt. Email: patricia.dewitt@wits.ac.za














