Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.52 n.1 Pretoria Apr. 2022
http://dx.doi.org/10.17159/2310-3833/2022/vol52n1a2
RESEARCH ARTICLE
Current practice used by therapists to screen and assess cerebral visual impairment in children with cerebral palsy in the South African setting
Nikita Ann SweetI, *; Denise FranzsenII
IB OT. (UKZN), MSc. OT (Wits). http://orcid.org/0000-0002-5185-2030; Occupational Therapist, Department of Occupational Therapy, Royal Hospital for Neuro-disability, London, UK
IIBSc. OT (Wits), MSc. OT (Wits), PhD (Wits), DHT(UP). http://orcid.org/0000-0001-8295-6329; Sessional Senior Lecturer, Occupational Therapy Lecturer, Department of Occupational therapy, School of Therapeutic Sciences, Faculty of Health Sciences, University of Witwatersrand , South Africa
ABSTRACT
BACKGROUND AND PURPOSE: Cerebral visual impairment (CVI) is a common comorbidity in children with cerebral palsy and has a significant impact on their functional capabilities. The lack of obvious deficits related to the eyes means awareness of CVI is poor. However, early diagnosis of CVI in children with cerebral palsy supports intervention which may improve the child's functioning in everyday activities. Occupational therapists and physiotherapists are able to identify children at risk for CVI, but there is a lack of research on the screening procedures they use to identify this deficit. This study therefore aimed at determining the current awareness of and clinical screening procedures used by occupational therapists and physiotherapists to detect CVI in children with cerebral palsy in South Africa
METHOD: A quantitative descriptive survey was distributed nationally to occupational therapists and physiotherapists treating children with cerebral palsy
RESULTS: The majority (81%) of the participants could define and explain CVI but a formal diagnosis of CVI is not commonly seen in practice (15.3%). The difficulty in getting a formal diagnosis of CVI was reported as being due to a lack of testing for functional vision by medical professionals. Less than half of the participants (45.7%) reported that they would always screen for a CVI in children with cerebral palsy and 42.9% of participants reported that they used informal screening procedures. Most of the participants reported that they would alter their intervention if they were aware that a child with cerebral palsy presented with CVI
CONCLUSION: This study shows that although therapists are aware of CVI, there is limited screening for this deficit and little or no formal screening of CVI in children with cerebral palsy in the South African context
Key words: cerebral palsy, cerebral visual impairment, screening, assessment, CVI-MQ
INTRODUCTION
Cerebral palsy (CP) is defined as a motor disorder, but is also associated with non-motor dysfunctions such as disorders of communication, behaviour, cognition and sensation1. Since the assessment and treatment of the physical, cognitive and communicative deficits take priority, particularly in children with marked functional limitations, thorough assessment of comorbidities associated with CP is often neglected or lacking because of the child's already numerous difficulties2. These deficits in children with CP also make the assessment of these various comorbidities - including visual impairments - difficult3,4. Fairhurst5 however, emphasised the importance of efficient assessment and intervention in comorbidities associated with children with CP, such as the presence of visual disorders including visual impairment. Visual disorders in children with CP include peripheral deficits within the eye structure as well as deficits in the central nervous system or cerebral visual impairment (CVI)6. Cerebral visual impairment is described as heterogeneous in nature, and there are controversies with regards to its classification7 but it is agreed that it is caused by damage to the retro-geniculate visual pathways (optic radiations, occipital cortex, visual associative areas)8. These deficits cover a wide range of visual sensory and visual perceptive dysfunction which result from a known neurological cause, but exclude visual deficits due to abnormalities of the eye9.
The lack of obvious deficits related to the eyes and healthcare providers' poor awareness of CVI means the condition often goes undiagnosed10,11. An early diagnosis of CVI in children with CP is important because there is evidence that intervention from a young age may improve the outcome for a child in terms of quality of life and occupational performance12. Although there is extensive research on assessment of children with CP there has been little focus on CVI and how this can be identified or assessed. Formal assessment procedures for CVI by professionals such as ophthalmologists, require extensive training or experience. The lack of research on assessment of CVI in children with CP, has been ascribed to the reported difficulty in adapting assessment for CVI in the presence of other deficits9,13.
Occupational therapists and physiotherapists, however, are positioned to screen and identify children with CP at risk for CVI because these professionals are often the first to complete a screening and in-depth assessment of the child's physical, cognitive and communicative deficits and comorbidities affecting everyday function. The screening for CVI should consider the effect of markedly fluctuating visual performances on motor and functional ability9. Most rehabilitation professionals rely on the child's medical history and informal clinical observations to screen for CVI9 even though literature indicates that there are some standardised screening tools that therapists can use. However, these standardised screening tools have not been validated for use in South Africa and it is also not currently known what screening and assessment procedures are used by therapists to screen for CVI in children with CP, in South Africa.
LITERATURE REVIEW
Cerebral visual impairment
Literature states that CVI is the most common cause of visual impairment in children with CP14 and according to four research studies, the incidence of CVI in children with CP ranges from 16% - 84%. Very little research on CP and associated visual comorbidities has been reported for the African context. A systematic review of African studies, indicated that the comorbidities in countries like Tanzania and Nigeria were much like those reported in research in developed countries. Lagunju & Oluleye15 found vision abnormalities in 58% and reported an incidence of 47.7% of CVI in children with CP in Nigeria .
Cerebral visual impairment includes a variety of visual sensory and perceptive disorders that are of a neurological origin that do not include optical visual impairments9. Due to the lack of an obvious ocular deficit diagnosing CVI can be a challenge due to its cortical nature10. The condition has a variety of presentations, therefore CVI has been described as an umbrella term for a number of visual deficits16 which can be present in children with normal visual acuity. According to Salavati17, CVI can be categorised by visual processing deficits including those of any likely cerebral cause with individual differences in presentation which have functional implications. The deficits can include severely reduced light perception, visual latency, visual field preference, difficulty with distance viewing and atypical visual reflexes. Behaviour observed in children with CVI may be a preference for a specific colour and familiar or rapidly moving objects. They often present with a non-purposeful gaze, an absence of visually guided reach and distress in complex sensory environments. They may bump into things regularly and their eye movements may be dependent on their head movement6.
Given that the visual manifestations of CVI are broad and depend on the location and severity of the underlying pathology3, a variety of screening assessments and assessments for CVI are needed. Currently assessment tools for identifying children at-risk for CVI are limited and the formal assessment of CVI is not time and cost-efficient9. This is particularly true in developing countries with a lack of access to specialists and health care facilities means that CVI in children with CP is often not recognised and it is difficult to have the diagnosis confirmed18.
Assessing cerebral visual impairment
The suggested formal assessments of CVI include three avenues19. The assessment of body structure for CVI is routinely done using neuro-ophthalmological and neuro-radiologic techniques such as computerised tomography (CT) or magnetic resonance imaging (MRI) scans as well as functional MRIs20. The second type of assessment for body function include the use of neurophysiological and ophthalmological investigations such as Visual Evoked Potentials (VEP) and electroencephalogram (EEG). Ophthalmological testing using VEP requires the child to have some level of communication and cognitive ability and therefore is not always appropriate for children with CP21. However, there is limited availability of these procedures in developing countries such as South Africa and this has resulted in little to no information on the prevalence and management of CVI in Africa18. The third type of assessment used to identify the presence of CVI is more accessible. These behavioural assessments include non-standardised tests for children with CP who are able to cooperate with the assessment process. Optokinetic nystagmus, visual fields, oculomotor function and visual acuity are assessed by introducing objects in the periphery, using light gazing for fixation and tracking, as well as preferential looking at cards with patterns. A concern about the use of the behavioural assessments is that these cannot be used for all children with CP, especially those with other severe deficits8,10.
None of these assessments focus on the constructs of activity and participation in line with the International Classification of Functioning, Disability and Health (ICF)22. Dera-more Denver et al.23 review the assessment of vision in terms of visual ability and participation in everyday activities for the unique visual characteristics of children with CVI, where "visual ability" is considered a measurable construct23. The review emphasises the importance of assessment tools for visual ability and describes four assessment tools for measuring the use of daily visual performance or functioning, some of which have proven validity and reliability. However, one of these comprehensive assessments, the CVI-range4 may not be suited to children with CP. Two of the assessments: Functional Visual Questionnaire13 and the Visual Skills Inventory24 have been designed to be used in conjunction with ophthalmological or VEP assessments for children with CP and motor deficits. The last assessment, The Preverbal Visual Assessment Questionnaire25 was designed to use a comprehensive history taking with parents of infants, but not infants with neurological deficits, which excludes its use with children with CP. None of the assessment tools have been validated for use in clinical setting by therapists in developing countries such as South Africa2.
It is suggested that occupational therapists and physiotherapists therefore use "visual ability" screening assessments to identify possible CVI in children with CP. These therapists are well placed to observe the effect of CVI on the children's functioning in their everyday environments9. Screening of a CVI would allow a therapist to make a better decision as to whether a child should be investigated further for assessment and diagnosis of CVI by the multidisciplinary team6. Two tools specifically for screening CVI have been described25 by one of the screening assessments. The CVI-questionnaire12 may not be suitable for use with children with CP as it does not accommodate motor deficits. The Cerebral Visual Impairment Motor Questionnaire (CVI-MQ)9 developed and validated in the Netherlands does, however, take the motor ability of a child with CP (using the Gross Motor Function Classification System (GMFCS), and the impact of potential visual difficulties to perform motor tasks, into account. This assessment uses everyday items and equipment and may be useful in contexts with limited resources.
This study aimed to determine the current awareness of CVI and current practice of occupational therapists and physiotherapists in screening for CVI in children with CP, in various settings in South Africa.
METHODS
Research design
A quantitative descriptive survey design was used for this study26.
Population and sampling
The survey was distributed to occupational therapists and physiotherapists who were members of the South African Neurodevelopmental Therapy Association (SANDTA). This association focuses on neurodevelopmental disorders in children and adults, and their members may be trained in Neurodevelopmental Therapy (NDT), and therefore some therapists treating children with CP would be members of this association. These therapists work in various settings with children with CP, including the private sector (private practices), non-profit organisations, schools for learners with special educational needs (LSEN) and government hospitals and clinics27.
The survey questionnaire was also distributed through Rural Rehab South Africa (RuReSA), an association for rehabilitation therapists and physiotherapists working in rural areas of South Africa, and Occupational Therapy Association of South Africa (OTASA), a professional association for occupational therapists, to increase the sample size. Total population sampling was used and all the therapists on the databases for SANDTA, RuReSA and OTASA, with contact details for more than 3000 therapists, were used. Emails were sent to all members on the databases, some of whom may have been duplicated as therapists belong to more than one association, some who do not treat children with CP and some of whom may have been speech therapists. There appear to be a limited number of therapists working with children with CP who are members of these associations and only occupational therapists and physiotherapists working with children with CP were requested to complete the questionnaire. Based on a previous study, which surveyed occupational therapists and physiotherapists working with children with CP in South Africa using a similar sampling method, a sample of 48 therapists was achieved27. The exact number of therapists working with children with CP registered with RuReSA and OTASA is unknown, although a sample of 62 therapists was recruited though OTASA in a previous study on visual problems in children with CP in South Africa28. Thus, a target sample of 40-50 participants was set for this study.
Research tools
Questionnaire on CVI and current practice
The first part of the questionnaire focused on demographic information including work-related information, qualifications, and experience of the participants. The profession of the participant, whether an occupational therapist or physiotherapist, the number of years they had been working and working with children with CP, what province and sector they were working in, and whether they had a qualification in neurodevelopmental therapy were also considered.
Questions on current practice determined the understanding of CVI, diagnosis of CVI and current screening procedures used to identify CVI in children with CP were included in this part of the questionnaire. Closed-ended questions with space for open-ended comments were used. Questions were formulated with guidance from the literature based on CP, CVI and CVI screening procedures. The questionnaire consisted of information regarding the number of years' experience the participants had in treating children with CP, how many children were treated within the space of a month, the main age group of children treated and what the most common GMFCS levels of the children with CP treated were, The questionnaire was piloted for content validity by three subject matter experts.
Data collection
Data collection was done by means of the REDCap electronic platform29 and was distributed through SANDTA, RuReSA and OTASA. Participants who were working with children with CP at the time of the study were invited to fill out the questionnaire. A reminder was sent out a month after the first distribution.
Data analysis
The questionnaire was formulated such that the data to be analysed were ordinal or nominal. All responses were downloaded from the REDCap programme into an Excel spreadsheet. The researcher checked all the data and completed descriptive analyses using frequencies and percentages for the closed-ended questions using Statistica v13.2. Comments and open-ended questions were analysed using summative content analysis and the number of participants making each comment was noted and the frequency of each comment was represented in the results.
Ethical considerations
Ethical clearance was obtained from the HREC of the University of the Witwatersrand (M180953). An information sheet was emailed with the questionnaires to all members of the three organisations. Completion of the questionnaire was considered informed consent. Anonymity was ensured by use of the REDCap platform.
RESULTS
There were 47 participants who responded to the questionnaires. Nine of the participants (19%) were not currently working with children with cerebral palsy (CP) so only the data for the remaining 38 participants was analysed. Although all questions of the questionnaire were not completed by all the participants, all questionnaires were included in the analysis. Not all participants answered all questions and this is indicated in the results.
Demographics
Most of the participants were occupational therapists (84.2%). More than half of the 38 participants had an undergraduate degree as their highest level of education. Slightly more than one quarter of the participants had master's degrees in occupational therapy. Two participants each had a master's degree either in early childhood education or public health (Table I, adjacent).

Of the 38 participants working with children with CP, more than a quarter had 5-7 years' experience while 39.3% of the participants had over 8 years' experience. The majority of the participants worked in KwaZulu-Natal followed by Gauteng, and the Southern and Western Cape. In terms of the work sectors, some of the participants were working in two or more sectors (42%), such as in a school for LSEN and a private practice. Just over a quarter of participants in the public health sector worked in rural, urban, district, regional and tertiary public hospitals and community clinics. The other participants worked in non-profit organisations, private practices and schools for learners with special needs as well as university clinics.
Postgraduate training for treating children with cerebral palsy
Thirty-two of the 38 participants had further training in assessing and treating children with CP (Table II, adjacent) and 12 of the 38 participants had further training in assessing and treating children presenting with CP and CVI. This training included workshops held by Malamulele Onward and SANDTA including the Bobath 8-week basic paediatric course, advanced NDT courses such as the advanced baby course and hemiplegia course, Movement Analysis and Education Strategies (MAES) course. Some had also attended workshops specifically on vision such as a low vision tutorial from EyeTek, CVI-range training (three-day workshop) by an occupational therapist, Christa Scholtz, or a cortical visual impairment course called From Theory to Practice presented by Lindsay Hillier.

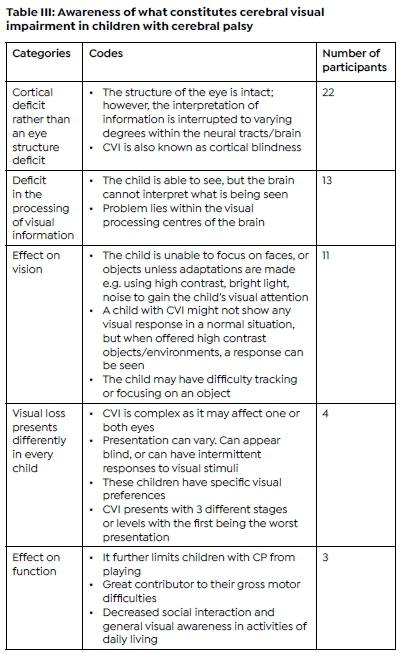
Awareness of what constitutes cerebral visual impairment
The participants responses were analysed based on the definition of CVI according to Salavati17 Most of the participants were aware that CVI was a cortical deficit rather than an eye structure deficit (62%) while two of the participants reported they were not aware of CVI. Participants agreed that although CVI is common in children with CP it is often not identified. Other difficulties reported to be associated with CVI included poor visual skills, visual field deficits, spasticity of the eye muscles, poor eye contact, not looking and reaching at the same time, visual latency, difficulty with distance viewing, visual perceptual difficulties, inconsistent visual responses, and fatiguing in visual tasks (Table III, above).
Diagnosing cerebral visual impairment
Of the 35 participants who responded, approximately half were not always aware of whether a child with CP presented with CVI. Only 11.4% of participants reported that they knew when a child with CP was diagnosed with CVI and 37.1% said that it depended on whether a caregiver indicated a possible CVI when describing the child's visual ability.
The majority of the participants (85.7%) did not know whether a formal diagnosis of CVI was confirmed, and a quarter of the participants (25.7%) reported they depended on the caregivers to inform them of the diagnosis of CVI. Just less than 30% reported that a CVI diagnosis was reported in the child's file despite the child not having been formally diagnosed. Only one participant, who works in a school for LSEN, indicated that the information about CVI diagnosis was given by the child's teacher.
Participants reported that they often observed the signs of CVI before the child had been given a diagnosis and referred the child for further assessment.
It was indicated that a formal diagnosis of CVI was often not made due to the carer's lack of knowledge, the age of the child (although it was not stipulated if this was because the child was too young or too old), or because there are often more pressing issues for the caregiver to deal with such as feeding and seizures. Obtaining a formal diagnosis for CVI is difficult as agreed to by 70.8% of the participants. This was noted especially in children being treated in the public health sector. The main reason expressed for the difficulty in getting a formal diagnosis of CVI was that medical professionals do not know how to test for functional vision. The child is assessed using tests that test the eye structures but not necessarily for CVI and the participants reported that, in their experience, doctors, optometrists and ophthalmologists are reluctant to assess CVI in children with CP. These professions either are unaware of assessments for CVI; or do not have the knowledge of the functional implications of CVI in CP. Some health professionals do not know when to refer a child for a CVI assessment and doctors are not always prepared to commit to a diagnosis without other formal assessments.
The fact that a child with CP can have communication difficulties makes it more difficult for a formal assessment to be conducted. Two participants mentioned that decreased cognitive level of functioning as well as physical motor deficits in children with CP, exacerbated this difficulty. One participant who worked in a non-profit organisation school for special needs reported that it was difficult to arrange for children with CP to go for a formal assessment as there was only one CVI clinic in Johannesburg, with a limited number of eye clinics in other catchment areas. This caused long waiting times for appointments and ultimately, delayed diagnosis. Logistically, if a child has not been formally diagnosed while in the health system, it is difficult then to confirm the diagnosis when in the education system. If the parents or caregivers have funds to do a formal assessment, the therapists report that they will do a screening at school and suggest a formal assessment.
Three participants were neutral in their response to the difficulty of obtaining a CVI diagnosis. One participant reported that s/he had only seen one child with CP who was high functioning, another participant reported that CVI was not one of the diagnoses considered in children with CP. Of the participants who reported CVI was assessed, three participants used an international CVI screening assessment. Four other participants did not find it difficult to obtain a CVI diagnosis since most of the children get referred to the eye clinic to be assessed, but one of these participants reported it was difficult to evaluate the effectiveness of this service.
Screening for cerebral visual impairment
Less than half of the participants (45.7%) reported that they always screened for a CVI in children with CP that they were treating. Nine participants said they would sometimes screen for CVI, while three participants said that they would never screen for CVI (8.6%). The remaining participants (20%) reported that it depended on whether a visual impairment was suspected.
When identifying the need for screening for CVI, participants reported that concerns were usually verbalised by the caregivers, or they would observe inconsistencies in the child's visual function when interacting with their environment. Most participants (88.6%) indicated that they used observations in assessment and therapy sessions during functional tasks to identify the need to screen for CVI. Fifteen of the participants (42.9%) reported that they used informal screening procedures including tracking of an object as an informal screening procedure. Other screening procedures are listed in Table IV (alongside). Most participants indicated they used more than one method of informal screening procedure.
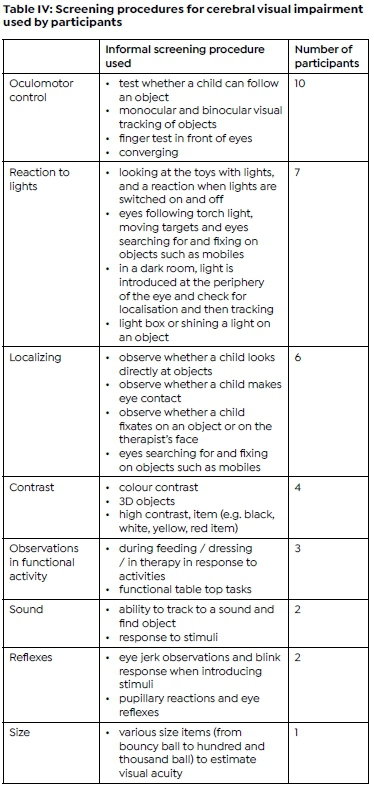
Only five participants (20%) were aware of validated screening and assessment tools/procedures and named the CVI-Range by Christine Roman-Lantsky. Two other participants mentioned using the GMFCS and the HAR assessment, neither of which assesses for CVI. One participant, who worked in a school for special needs and private practice, reported creating their own CVI kit to evaluate the children. However, this CVI kit is not standardised and is rather practice-based. It cannot be assumed that this kit effectively screens or assesses for CVI as it is not a formal screening or assessment tool.
Procedure followed when a cerebral visual impairment is suspected
Participants reported that they would use their own informal screening procedures and observations (57.1%). The majority of the participants reported that they would refer to a specialist if they suspected CVI in a child with CP because they had access to specialists in their settings (65.7%). These specialists included ophthalmologists, optometrists, paediatric neurologists, behavioural optometrists, neurologists, medical officers, developmental doctors and experienced occupational therapists. Thirteen of the participants (37.1%) reported that they would assume a child had CVI and alter their intervention accordingly, but continue with treatment since they did not have access to assessments and specialists to diagnose CVI. Only 11.4% of participants reported that they would carry on with treatment without considering CVI because they did not have access to assessments and specialists to diagnose CVI.
DISCUSSION
Most of the participants in the study were occupational therapists and this could be because the survey was not only administered through SANDTA, but also through OTASA, which targeted only occupational therapists. It was not possible, due to the anonymity of the survey, to identify from which organisations therapists responded. Most sectors and provinces were represented in the sample.
The participants in the study had work experience ranging from 1-32 years, although they had fewer years' experience in working with children with CP. Results therefore indicate that therapists with different levels of experience are currently working in the field of CP. However, nearly two thirds of therapists working with children with CP can be considered as experienced (more than four years of work experience) or experts (more than 10 years of work experience)30. The participants in this study appeared to have a particular interest in the treatment of CP. A large majority of the participants had postgraduate training in the assessment and treatment of children with CP in line with another South African study where 72.2% of the participants had completed postgraduate courses in the field of CP28. The most common postgraduate course attended was the Bobath NDT 8-week paediatric course and, since it is hosted by SANDTA, it is likely that participants were members of SANDTA because they had completed courses with this association. A third of participants had further training in assessing and treating children with CP presenting with a CVI completed through SANDTA or the CVI-Range training workshops held by Christa Scholtz. Christa Scholtz was listed as an important source of CVI knowledge in a previous study on visual deficits in children with CP in South Africa28.
Participants worked in the most populated provinces, which is congruent with another recent study which surveyed therapists working with children with CP in South Africa and, as with this study, the majority of the participants were working in the private sector and schools for LSEN27. It is possible that this is where other services which deal with CVI are available, making therapists more aware of the condition. It should also be considered that the results indicate a possible paucity of services in more rural provinces and public hospitals, where the prevalence of children with CP and the severity of the condition may be greater31. The current study did, however, provide data from participants in a diversity of settings.
According to Salavati et al.9, it is often therapists who first identify the possibility of CVI in children with CP and therefore it is important that therapists in the South African setting are aware of CVI. The awareness of what a CVI is among the other participants was accurate, although it is a concern that some participants had not heard of CVI. The awareness amongst other participants could be due to the fact that a third of them had postgraduate training in the assessment and treatment of children with CP, so they would have been more likely to have been exposed to information about CVI after their undergraduate training. This supports a study done in South Africa on visual deficits in CP where the participants reported that they felt their undergraduate training was insufficient in managing visual deficits in children with CP 28.
Nearly a third of participants were also aware of varying presentations of CVI, including tracking and localization difficulties; unique visual and behavioural characteristics, such as being attracted to high contrast objects; visual latency; and visual perception difficulties. This heterogeneity of what different participants reported is congruent with other CVI studies9. However, only 8% of participants noted that CVI would limit function in daily life, despite other studies reporting that children with CP and CVI have greater limitation and slower development in terms of mobility, self-care and socialization32-34. It seems that the participants in the current study focused on impairments and symptoms related to CVI rather than participation in occupations32, even though it is recommended that CVI in children with CP be assessed on how children use their vision to perform daily living activities32,34.
Half of the participants were not always aware if a child with CP had CVI since identifying CVI can be a challenge as there is often no obvious ocular deficit due to its cortical nature10. There are also a wide range of visual deficits included under the umbrella of CVI, of which therapists, teachers and caregivers may not always be aware. It appears that a diagnosis of CVI, even if it is not formal, is reported for nearly a third of children with CP seen by the participants in the study. More than two thirds of participants agreed that it is difficult to obtain a formal diagnosis of a CVI, especially in the public sector where limited resources and expertise mean children are often not assessed or diagnosed35,36. The main reason expressed for the difficulty in establishing a formal diagnosis of CVI was a lack of services from other health professionals who are reluctant, or do not know how, to test for functional vision. In the current study, none of the participants mentioned the use of formalised assessments reportedly used globally for CVI, such as CT, MRI and functional MRIs20, Visual Evoked Potentials and EEGs6. This may indicate that use of these assessments for CVI is limited in South Africa. Donald et al.18 support this and indicate that in developing countries, diagnosing CVI in children with CP is limited by lack of resources18. This confirms the difficulties experienced by the participants in the current study in receiving a formal confirmed diagnosis of CVI, where they also reported accessibility and logistics as a major concern.
The participants reported (as indicated by the limited literature and a lack of research internationally32), that other health professionals lack knowledge about, and do not acknowledge the functional implications of CVI in a child with CP3,4. This has been ascribed to the fact that in children with CP, CVI is often outweighed by the importance of other comorbid deficits3,4. There is often an assumption that a child with CP has a poor prognosis and there are more pressing medical concerns, so a comorbidity such as CVI and the resultant functional implications are not always considered2. However, although participants felt that other health professionals lacked knowledge and expertise to diagnose CVI, 65.7% reported that they would still refer to a specialist commonly involved in functional vision assessment, including for CVI10 if they suspected CVI in a child with CP. These participants reflect those who work in the private sector and LSEN schools where access to more experienced and specialist health care for children with CP is available37.
Occupational therapists and physiotherapists appear more aware of CVI and the functional implications of the condition because they assess and treat function in terms of client factors and participation in children with CP9. However, participants did mention that they were more likely to screen a child with CP for a CVI when they were on a higher GMFCS level. The difficulty in screening or assessing children on a lower GMFCS level is hampered by the greater number of comorbidities experienced by these children, which are often a barrier to the effective screening and assessment of CVI. Cognitive, motor and speech and language difficulties have to be considered when assessing for CVI and as suggested by Salavati et al.9, occupational therapists and physiotherapists should be trained to screen and manage possible CVI in children with lower GMFCS.
Of concern, however, are the more than 50% of participants who were aware of CVI only 'sometimes' or 'never' screen for CVI. Literature indicates the importance of screening for CVI in view of the impact of CVI on functional mobility and quality of life, as well as the high occurrence of CVI in children with CP in developing countries, such as Kenya38. As reported in the literature, participants indicated that their screening for CVI in children with CP was mostly based on their own observations, reports from caregivers and on history taking, and less on reports from doctors and medical files. This is because caregivers are usually most able to give clear descriptions of the effect of visual functioning39.
The use of observational and behavioural assessments are described by Chorna, Guzzetta and Maitre as a "battery of behavioural assessments" which consist of the non-standardised assessments of optokinetic nystagmus, visual fields, oculomotor function, visual acuity and visual-perceptual difficulties19. It must be noted, however, that this form of assessment is recommended for children with less severe forms of CP19. Only 20% of participants were aware of and possibly used formalised screening assessments and this is supported by other studies where formal screening for CVI is rarely used unless research is being conducted9. Thus, the current practice of the participants in this study is in line with global practice for screening for CVI in children with CP34.
More than two thirds of the participants did acknowledge that the presence of CVI would alter their intervention and it seems that they were aware of the importance of acknowledging CVI but not the functional implications thereof in their treatment of children with CP2. This is supported by another South African study where participants reported they would alter their intervention if they discovered that a child with CP had a visual impairment28.
Limitations
The biggest limitation of this study was the low response rate. Cerebral visual impairment is considered a specialised field and has only been introduced as a topic in the SANDTA eight-week paediatric NDT course curriculum in recent years13. Thus, the smaller than expected sample may have been due to therapists, who are aware of and screen for CVI, responding since email surveys are highly related to the research interests of the participants. Trespalacios & Perkins40 found that 90% of participants would be more likely to complete a survey if they were interested in the topic. Although the emails were sent from a reliable source, the response rate may have been affected by a lack of personalisation as well as participants' email checking behaviour and the accuracy of the contact details on the organisation databases41.
The low response rate means that the results must be interpreted with caution and are not generalisable for other therapists working with children with CP in South Africa. However, data analysis did provide information that can be used in considering the use of the CVI-MQ in screening for CVI in children with CP.
CONCLUSION
There is a lack of research on the screening and assessment procedures that therapists can use to determine the presence of CVI in children with CP, both locally and internationally. Screening for CVI is not always a common practice. Less than half of the participants reported that they would screen for CVI; the remaining participants would only sometimes screen if a visual impairment was suspected and the others would not screen for CVI. Participants reported screening for CVI in children with CP through observation and screening procedures used in therapy sessions. This is congruent with research which found that occupational therapists and physiotherapists use observations to make a diagnosis due to the lack of available screening and assessment tools for CVI9. The CVI-Range by Christine Roman-Lantsky was the only validated screening tool/assessment tool used by a limited number of participants; however, this tool is not validated in the South African setting, requires training, and is not specific to children with CP.
There are many challenges that face occupational therapists and physiotherapists in screening and assessing for CVI in children with CP. These challenges include a lack of knowledge of CVI by health professionals, a lack of access to specialists and formal CVI screening tools and assessments, and diagnostic difficulties due to multiple comorbidities in children with CP. Research suggests that therapists will often assume the presence or absence of a CVI9 and the majority of the participants reported that they would alter intervention if they were aware of CVI, but not having access to formal screening and assessment tools means that CVI often go undiagnosed.
RECOMMENDATIONS
It is clear from the study that there is a great need for validated screening and assessment tools for CVI in the South African setting. This warrants further research of other internationally-validated screening tools and whether they would be valid and usable in the South African setting.
Investigating and improving knowledge of CVI for all health care professionals in South Africa through adding this knowledge in undergraduate training.
CONFLICTS OF INTEREST
No funding for the project was received.
DATA AVAILABILITY STATEMENT
Upon reasonable request the data is available from Nikita Sweet.
AUTHOR CONTRIBUTIONS
Nikita Sweet, a postgraduate student who conceptualized, contributed to and completed the article. Denise Frnzsen, supervisor of the projec - data analysis and conceptualisation of results and discussion - conceptualisation and contribution to the article.
REFERENCES
1. Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M. A report: The definition and classification of cerebral palsy April 2006. Developmental Medicine and Child Neurology. 2007;49(SUPPL. 2):8-14. doi:https://doi.org/10.1111/j.1469-8749.2007.tb12610.x [ Links ]
2. Alimovic S. Visual impairments in children with cerebral palsy. Hrvatska revija za rehabilitacijska istrazivanja. 2012;48(1):96-103. [ Links ]
3. Dutton GN, Jacobson LK. Cerebral visual impairment in children. Seminars in Neonatology. 2001;6(6):477-485. doi:https://doi.org/10.1053/siny.2001.0078 [ Links ]
4. Newcomb S. The reliability of the CVI range: A functional vision assessment for children with cortical visual impairment. Journal of Visual Impairment and Blindness. 2010;104(10):637-647. doi:https://doi.org/10.1177/0145482x1010401009 [ Links ]
5. Fairhurst C. Cerebral palsy: The whys and hows. Archives of Disease in Childhood: Education and Practice Edition. 2012;97(4):122-131. doi:https://doi.org/10.1136/edpract-2011-300593 [ Links ]
6. Edmond JC, Foroozan R. Cortical visual impairment in children. Current Opinion in Ophthalmology. 2006;17(6):509-512. doi:https://doi.org/10.1097/ICU.0b013e3280107bc5 [ Links ]
7. Salavati M, Rameckers EAA, Steenbergen B, Van Der Schans C. Gross motor function, functional skills and caregiver assistance in children with spastic cerebral palsy (CP) with and without cerebral visual impairment (CVI). European Journal of Physiotherapy. 2014;16(3):159-167. doi:https://doi.org/10.3109/21679169.2014.899392 [ Links ]
8. Fazzi E, Signorini SG, La Piana R, Bertone C, Misefari W, Galli J, Balottin U, Bianchi PE. Neuro-ophthalmological disorders in cerebral palsy: Ophthalmological, oculomotor, and visual aspects. Developmental Medicine and Child Neurology. 2012;54(8):730-736. doi:https://doi.org/10.1111/j.1469-8749.2012.04324.x [ Links ]
9. Salavati M, Waninge A, Rameckers EAA, van der Steen J, Krijnen WP, van der Schans CP, Steenbergen B. Development and face validity of a cerebral visual impairment motor questionnaire for children with cerebral palsy. Child: Care, Health and Development. 2016. doi: https://doi.org/10.1111/cch.12377 [ Links ]
10. Ospina LH. Cortical visual impairment. Pediatrics in Review. 2009;30(11):81-90. doi:https://doi.org/10.1542/pir.30-11-e81 [ Links ]
11. Gorrie F, Goodall K, Rush R, Ravenscroft J. Towards population screening for Cerebral Visual Impairment: Validity of the five questions and the CVI questionnaire Kueh YC, editor. PLoS ONE. 2019;14(3):e0214290. doi:https://doi.org/10.1371/journal.pone.0214290 [ Links ]
12. Ortibus E, Laenen A, Verhoeven J, De Cock P, Casteels I, Schoolmeesters B, Buyck A, Lagae L. Screening for cerebral visual impairment: Value of a CVI questionnaire. Neuropediatrics. 2011;42(4):138-147. doi:https://doi.org/10.1055/s-0031-1285908 [ Links ]
13. Ferziger NB, Nemet P, Brezner A, Feldman R, Galili G, Zivotofsky AZ. Visual assessment in children with cerebral palsy: Implementation of a functional questionnaire. Developmental Medicine and Child Neurology. 2011;53(5):422-428. doi:https://doi.org/10.1111/j.1469-8749.2010.03905.x [ Links ]
14. Dutton GN, Calvert J, Cockburn D, Ibrahim H, Macintyre-Beon C. Visual disorders in children with cerebral palsy: The implications for rehabilitation programs and school work. Eastern Journal of Medicine. 2012;17(4):178-187. [ Links ]
15. Lagunju IA, Oluleye TS. Ocular abnormalities in children with cerebral palsy. African journal of medicine and medical sciences. 2007;36(1):71-75. [ Links ]
16. Martín MBC, Santos-Lozano A, Martín-Hernández J, López-Miguel A, Maldonado M, Baladrón C, Bauer CM, Merabet LB. Cerebral versus ocular visual impairment: The impact on developmental neuroplasticity. Frontiers in Psychology. 2016;7(DEC):1-9. doi:https://doi.org/10.3389/fpsyg.2016.01958 [ Links ]
17. Salavati A. Assessing gross motor function, functional skills, and caregiver assistance in children with cerebral palsy (CP) and cerebral visual impairment (CVI) (Doctoral dissertation, Rijksuniversiteit Groningen). Rijksuniversiteit Groningen; 2016. [ Links ]
18. Donald KA, Samia P, Kakooza-Mwesige A, Bearden D. Pediatric cerebral palsy in Africa: A systematic review. Seminars in Pediatric Neurology. 2014;21(1):30-35. doi:https://doi.org/10.1016/j.spen.2014.01.001 [ Links ]
19. Chorna OD, Guzzetta A, Maitre NL. Vision Assessments and Interventions for Infants 0-2 Years at High Risk for Cerebral Palsy: A Systematic Review. Pediatric Neurology. 2017;76:3-13. doi:https://doi.org/10.1016/j.pediatrneurol.2017.07.011 [ Links ]
20. Fazzi E, Signorini SG, Bova SM, La Piana R, Ondei P, Bertone C, Misefari W, Bianchi PE. Spectrum of visual disorders in children with cerebral visual impairment. Journal of Child Neurology. 2007;22(3):294-301. doi:https://doi.org/10.1177/08830738070220030801 [ Links ]
21. Watson T, Orel-Bixler D, Haegerstrom-Portnoy G. Early visual-evoked potential acuity and future behavioral acuity in cortical visual impairment. Optometry and Vision Science. 2010;87(2):80-86. doi:https://doi.org/10.1097/OPX.0b013e3181c75184 [ Links ]
22. World Health Organisation. Overview of ICF Components. Geneva: World Health Organisation; 2001. doi:https://doi.org/10.1055/s-0033-1338283 [ Links ]
23. Deramore Denver B, Froude E, Rosenbaum P, Wilkes-Gillan S, Imms C. Measurement of visual ability in children with cerebral palsy: a systematic review. Developmental Medicine and Child Neurology. 2016;58(10):1016-1029. doi:https://doi.org/10.1111/dmcn.13139 [ Links ]
24. McCulloch DL, Mackie RT, Dutton GN, Bradnam MS, Day RE, McDaid GJ, Phillips S, Napier A, Herbert AM, Saunders KJ, et al. A visual skills inventory for children with neurological impairments. Developmental Medicine and Child Neurology. 2007;49(10):757-763. doi:https://doi.org/10.1111/j.1469-8749.2007.00757.x [ Links ]
25. García-Ormaechea I, González I, Duplá M, Andres E, Pueyo V. Validation of the Preverbal Visual Assessment (PreViAs) questionnaire. Early Human Development. 2014;90(10):635-638. doi:https://doi.org/10.1016/j.earlhumdev.2014.08.002 [ Links ]
26. Creswell JW. Research design: qualitative, quantitative and mixed method approaches. Second. Sage Publications; 2003. [ Links ]
27. Davies L. Current occupational therapy and physiotherapy practice in implementing home programmes for young children with cerebral palys in South Africa. University of the Witwatersrand; 2016. http://wiredspace.wits.ac.za/handle/10539/21369 [ Links ]
28. Janse van Rensburg Z. Occupational Therapy practice used for children diagnosed with a dual diagnosis of cerebral palsy and visual impairment in South Africa. 2016:1-123. https://core.ac.uk/download/pdf/188775518.pdf [ Links ]
29. Vanderbilt University. REDCap. 2006. https://projectredcap.org/about/ [ Links ]
30. Owen A. Clinical and Professional Reasoning in Occupational Therapy. New York: Lippincott Williams & Wilkins; 2011. [ Links ]
31. Coombe H. The clinical presentation of Cerebral Palsy in children in rural Kwazulu Natal, South Africa. University of the Western Cape; 2017. [ Links ]
32. Anaby D, Korner-Bitensky N, Steven E, Tremblay S, Snider L, Avery L, Law M. Current Rehabilitation Practices for Children with Cerebral Palsy: Focus and Gaps. Physical and Occupational Therapy in Pediatrics. 2017;37(1):1-15. doi:https://doi.org/10.3109/01942638.2015.1126880 [ Links ]
33. Ghasia F, Brunstrom J, Gordon M, Tychsen L. Frequency and severity of visual sensory and motor Deficits in children with cerebral palsy: Gross motor function classification scale. Investigative Ophthalmology and Visual Science. 2008. doi: https://doi.org/10.1167/iovs.07-0525 [ Links ]
34. Deramore Denver B, Adolfsson M, Froude E, Rosenbaum P, Imms C. Methods for conceptualising 'visual ability' as a measurable construct in children with cerebral palsy. BMC Medical Research Methodology. 2017;17(1):1-13. doi:https://doi.org/10.1186/s12874-017-0316-6 [ Links ]
35. Maphumulo WT, Bhengu BR. Challenges of quality improvement in the healthcare of South Africa post-apartheid: A critical review. Curationis. 2019;42(1):1-9. doi:https://doi.org/10.4102/curationis.v42i1.1901 [ Links ]
36. Reid S. 20 Years of community service in South Africa: what have we learnt? 2018. [ Links ]
37. Barratt J, Penn C. Listening to the voices of disability: Experiences of caring for children with cerebral palsy in a rural south African setting. In: Disability and International Development: Towards Inclusive Global Health. 2009. p. 191-212. doi:https://doi.org/10.1007/978-0-387-93840-0_13 [ Links ]
38. Njambi L, Kariuki M, Masinde S. Ocular findings in children attending occupational therapy clinic at Kenyatta National Hospital, Nairobi, Kenya. Joecsa. 2009;15(1). [ Links ]
39. Philip SS, Dutton GN. Identifying and characterising cerebral visual impairment in children: A review. Clinical and Experimental Optometry. 2014;97(3):196-208. doi:https://doi.org/10.1111/cxo.12155 [ Links ]
40. Trespalacios JH, Perkins RA. Effects of Personalization and Invitation Email Length on Web-Based Survey Response Rates. TechTrends. 2016;60(4):330-335. doi:https://doi.org/10.1007/s11528-016-0058-z [ Links ]
41. Saleh A, Bista K. Examining Factors Impacting Online Survey Response Rates in Educational Research: Perceptions of Graduate Students. Online Submission. 2017;13(2):63-74. [ Links ]
* Corresponding Author: Nikita Sweet. Email: nikitaannsweet@gmail.com














