Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.51 n.3 Pretoria Dec. 2021
http://dx.doi.org/10.17159/2310-3833/2021/vol51n3a6
RESEARCH ARTICLE
Examining Wound Management in Hand Therapy within the South African Context
Lezane EsterhuizenI, *; Deshini NaidooII; Pragashnie GovenderIII
IBSc Occ Ther (UCT); PGDip Hand Therapy (UP); M Occ Ther (UKZN). Occupational Therapist, Bertha Gxowa Hospital, Germiston, South Africa. https://orcid.org/0000-0001-8237-5890
IIB Occ Ther (UKZN), M Occ Ther (UKZN), PhD (UKZN); Senior Lecturer, Discipline of Occupational Therapy, College of Health Sciences, University of KwaZulu -Natal. https://orcid.org/0000-0001-6276-221X
IIIB. Occ T her (UKZN), M Occ Ther (UKZN), PhD (UKZN); Associate Professor, Discipline of Occupational Therapy, College of Health Sciences, University of KwaZulu-Natal, South Africa. https://orcid.org/0000-0003-3155-3743
ABSTRACT
BACKGROUND: Internationally, it is within occupational therapists' scope of practice to provide interventions for the prevention of wounds, amelioration of wounds and to address occupational dysfunction resulting from wounds. In South Africa, however, the role of occupational therapy in wound management in hand therapy is unclear
AIM: This study aimed to describe current wound management practices and views of occupational therapists on their perceived role and preparedness for providing wound management to hand injured patients in South Africa
METHOD: A cross-sectional survey was administered with a sample of 106 participants via non-probability convenience sampling. Frequencies and percentages are presented for quantitative data analysed with descriptive statistics. Open-ended responses were analysed via inductive thematic analysis
RESULTS: Findings indicated a high prevalence of wounds in patients with hand injuries. Occupational therapists in South Africa have reported experiencing a high demand for involvement in wound management interventions. The identified role of occupational therapists includes providing interventions for the amelioration of wounds and addressing occupational dysfunction resulting from wounds, amongst others
CONCLUSION: Improved guidance on the role and scope of occupational therapy in wound management is required. This is a need within the South African context due to the high prevalence of wounds in populations of hand injured patients that occupational therapists serve
Keywords: wound management, hand therapy, occupational therapy, International Classification of Functioning, Disability and Health.
INTRODUCTION
Individuals with upper limb injuries are at risk of and frequently present with wounds1. The skill of occupational therapists is their ability to analyse and understand the impact that an acute or chronic wound has on an individuals' functioning as well as their participation in meaningful occupations and the fulfilment of meaningful roles1. The complex interaction between client factors, including body structures and functions, an individuals' environment, and occupational participation, is well understood by occupational therapists 1. From this perspective, occupational therapists can address client factors through the prevention and amelioration of wounds, as well as address occupational dysfunction resulting from wounds through compensatory methods and environmental adaptations1.
Internationally, wound management is recognised to be within the scope of practice of hand therapists24. In South Africa, there is an expectation for occupational therapists to provide hand therapy services to individuals with complex upper limb injuries5, including interventions related to wound management. However, occupational therapists may not have received adequate undergraduate education and training to cope with such demands, notwithstanding that the role of occupational therapists is not clearly articulated within the South African scope of practice. This study aimed to address an identified gap in the available literature by describing i) current practices of occupational therapists in providing wound management interventions to hand injured patients in South Africa, ii) the views of practising occupational therapists of their role in wound management within hand therapy and iii) their level of preparedness to manage hand wounds.
LITERATURE REVIEW
Current international wound management practices
Within the context of this study, 'wound management' refers to activities undertaken by an occupational therapist for the prevention of wounds, amelioration of wounds or addressing occupational dysfunction resulting from wounds1. Several authors refer to wound management as part of treatment plans for various upper limb injuries and conditions, implying that this area of practice is viewed as part of holistic care6,7,813. A practice analysis survey conducted in 2014 investigated contemporary upper limb rehabilitation practices of hand therapists, with a particular interest in wound management2. The results showed that wound management activities are deemed highly essential but are infrequently used2.
Prevalence of wounds in hand injuries in South Africa
In South Africa, high rates of interpersonal violence and road accidents (when compared to global statistics14), are reported to contribute to a higher incidence of hand injuries15. Moreover, the high rates of work-related hand injuries amongst workers who engage in manual labour, the traumatic injuries seen within South African state hospitals16,17 together with patients presenting to occupational therapy with firework injuries6 and tendon injuries5,7,18 imply a high prevalence of hand injuries with wounds. Wounds may include, amongst others, abrasions, bites, surgical wounds and traumatic wounds1.
Preparedness of therapists to carry out wound management
Expertise in wound management is reportedly acquired through working with experienced therapists and other knowledgeable professionals2. Therapists develop skills related to wound management during formal education, prior to further training in upper limb rehabilitation or within the first two years practising in hand therapy2. Several authors in the available literature confirm that the occupational therapist can address aspects of health and well-being affected by wounds1-4 and have a role to play in the amelioration of wounds, the prevention of wounds in hand injuries that involve peripheral nerve damage and thus, sensory loss, and in facilitating independent management of wounds1 Moreover, contemporary practices and readiness of therapists in managing wounds have been reported in the international literature2. There is, however, a need to examine the role of occupational therapy in South Africa, including the practices and preparedness of therapists, in managing wounds of patients that they encounter in their practice.
METHODOLOGY
Study design and Instrument development
This study followed a cross-sectional survey design using a self-administered online questionnaire. The content of the questionnaire was informed via a perusal of available literature and thematic analysis of qualitative data from semi-structured interviews with seven purposively recruited occupational therapists who were experienced in the field of hand therapy in South Africa. The framework of the International Classification of Functioning, Disability and Health (ICF)19 was used to structure two of the sections within the semi-structured interview guide. These sections pertained to factors occupational therapists consider when assessing patients with hand wounds, as well as the interventions that occupational therapists provide when treating patients with hand wounds. This study uses the ICF framework to conceptualise a wound as an impairment of the skin (body function and structure), that is precipitated by a hand injury.
Section A of the questionnaire obtained informed consent. Section B contained 11 questions covering relevant demographic and work history to determine a profile of participants and eligibility for participation. Respondents not meeting the criteria were automatically redirected exit the survey. Section C contained 19 questions capturing information relevant to i) current practices, ii) perceived role of occupational therapists and iii) their perceived level of preparedness in providing wound management interventions. The ICF framework was also used to structure three questions within section C of the questionnaire. These pertained to the factors that occupational therapists consider in assessment, the interventions they provide, and the perceived role of occu pational therapy. Response types included closed multiple-choice questions allowing only one response, checkbox answers with participants being allowed to choose multiple relevant options, scaled items and open-ended answers, allowing for justification, specification or elaboration20. To determine content validity, a panel of 11 occupational therapists who were knowledgeable in hand therapy reviewed the questionnaire. A content validity index was calculated per item (I-CVI)21, which was used with qualitative feedback to guide the questionnaire revision. Section C in the initial questionnaire that was presented for review consisted of 27 questions containing 214 items. Reviewers rated 171 items (69%) relevant with an I-CVI of 0.90-1.00. A further 32 items (13%) were rated relevant with an I-CVI of >0.80 <0.90. A total of 45 items (18%) were irrelevant with I-CVIs <0.80. The qualitative review identified ambiguity and a lack of clarity on some items. The final questionnaire consisted of 19 questions containing 139 items in section C.
Population and sampling
The target population were occupational therapists who were responsible for the management of patients with hand injuries in South Africa. There were no data available on the number of occupational therapists working in this field. Thus, databases of the South African Society of Hand Therapists (SASHT) and the Occupational Therapy Association of South Africa (OTASA) were accessed to attain membership figures. In May 2020, 110 occupational therapists were registered with SASHT, excluding international members22. OTASA had 233 registered, practising occupational therapists who had indicated 'hands' as their field of practice in South Africa23. Membership of these associations is not mutually exclusive; thus, an overlap was assumed. As it is not compulsory, it was expected that several occupational therapists working in hand therapy were not registered with either association; therefore, the total number of potential participants in the target population was unknown. Non-probability convenience sampling24 was utilised. Predetermined criteria were applied to select qualified occupational therapists who, at the time of data collection, (i) were registered with the Health Professions Council of South Africa (HPCSA), (ii) were practising or who have practised within the field of hand therapy between 2015-2020, and (iii) obtained most of their experience in hand therapy in South Africa.
Procedure
Data collection occurred between May and July 2020. SASHT and OTASA were approached to send out an invite for participation to their members via an email containing the link to the online questionnaire. An email invitation was also sent to the authors' networks, who were, via snowball sampling, encouraged to extend the invitation to others practising in the field of hand therapy. An information sheet was embedded within the online survey. Contact details of the first author were provided, allowing an opportunity for respondents to ask questions and seek clarification if required.
Data management and analysis
Since Google Survey was used as an online platform for data collection, responses were automatically uploaded into a secure Google spreadsheet. Qualitative responses where participants elaborated on their views were extracted verbatim and analysed via thematic analysis using an inductive approach. A statistician was consulted for quantitative data analysis (descriptive statistics). Frequencies and percentages were calculated and verified for demographic data in section A and for all variables obtained through closed responses in section C. Responses to open short answers where participants specified or provided justification for responses were post-coded, categorised and analysed using descriptive statistics.
Ethical considerations
Ethical approval for the study was obtained from the Biomed-ical Research Ethics Committee (BREC) of the University of KwaZulu-Natal (reference number: BREC/00001029/2020). Participants provided informed consent. The respondents were de-identified during data analysis and reporting to maintain confidentiality.
RESULTS
The number of therapists invited to participate in the study was not known thus, a response rate was not calculable. The total number of responses received was 113. Seven respondents were excluded. One was a physiotherapist, three had not worked in hand therapy between 2015-2020, and three had obtained most of their experience in hand therapy in a country other than South Africa. A total of 106 surveys were eligible for analysis. Frequencies were determined for all variables and descriptors, irrespective of missing data. Where n<106, the number of responses per item is indicated. Findings of open-ended questions (qualitative data) are reported with quantitative results in the relevant sections.
Demographic and practice profile
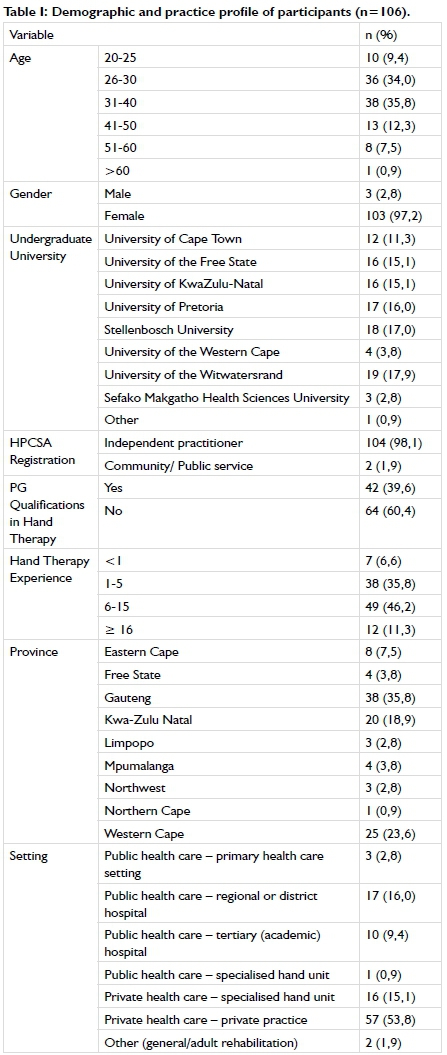
The demographic profile of the study participants is highlighted in Table I (alongside). Most respondents were female (97,2%; n=103) and between 26-40 years old (69,8%; n=74). A fair number of respondents held postgraduate qualifications in hand therapy (39,6%; n=42). Most respondents had 6-15 years of experience practising in hand therapy (46,2%; n=49), with a large percentage (68,9%; n=73) working in private settings.
Current practices of Occupational Therapists: Occupational therapists' current practices related to wound management in hand therapy are reported under the following sub-sections:
The prevalence of hand wounds: Between 50%-100% of patients with hand injuries treated, on a monthly basis, were reported to present with wounds by 7l.7% (n=76) of participants. Nearly a quarter (24,5%; n=26) reported that wounds were seen in > 80% of cases. (Figure 1. p45)
The demand experienced by therapists to manage hand wounds
Most participants experienced a demand for involvement in managing wounds of patients with hand injuries (94,3%; n=100). Reasons for demands experienced are displayed in Table II (above). Two participants indicated that wound management needs to be done by a qualified professional (1,9%; n=2).
Analysis of the open-ended responses highlighted that the demand experienced was related to frequently receiving referrals for diagnoses requiring wound management. Participants also expressed concern for preserving the patients' time and finances by providing wound management as part of the holistic intervention. It was further reported that wound management was frequently needed prior to splinting and mobilisation. The functional implications of wound healing and the impact of scar tissue were discussed. Participants also expressed that wound care professionals are not available in all settings between specialist consultations and that patients do not always follow up with the surgeon.
"Patients often require intervention between consults with specialist and not necessarily referred to wound care sisters". (Participant 33)
Factors considered in assessment and interventions used
Table III (p47) delineates the frequency of factors considered in assessment and the frequency of use of interventions for patients with hand wounds. The item 'application of topical medications' under the use of wound management interventions had 50 responses due to erroneous removal from the online survey before the completion of data collection. It was never/rarely used by 28% (n=14), occasionally used by 30% (n=15), and often/always used by 42% (n=21).
Additional factors considered in the assessment, as reported by some respondents, included how a wound may impact treatment planning (0,9%; n=1), the patient's language and ability to communicate effectively (0,9%; n=1), and financial status (0,9%; n=1), family support for the performance of wound management (0,9%; n=1), as well as unspecified factors relevant to paediatric patients (0,9%; n=1). In the provision of patient education, written wound management instructions were infrequently provided due to low levels of literacy amongst patients (0,9%; n=1) and a preference for videos or photos taken on the patients' phone was indicated (0,9%; n=1). In facilitating participation in meaningful occupations, communication with patients' employers was infrequent due to unemployment levels (0,9%; n=1), and patients were not advised to return to work before wounds were healed (0,9%; n=1).
Occupational Therapists and the MDT in wound management
The frequency of actions/activities undertaken whilst working with the MDT for the provision of wound management to patients with hand injuries is also delineated in Table III (p46). Another reason for referring was a lack of confidence in treating a wound (1,9%; n=2). The team member/s primarily responsible for managing basic wounds of patients with hand injuries was the occupational therapist only (17,0%; n=18), the occupational therapist and other team member/s (49,1%; n=52) and other team member/s excluding the occupational therapist (34,0%; n = 36). For complex wounds, the team member/s primarily responsible were the occupational therapist only (4,7%; n = 5), occupational therapist and other team member/s (37,7%; n=40) and other team member/s excluding the occupational therapist (57,5%; n=61).
Perceived barriers and enablers to using interventions related to wound management
The extent to which various factors were perceived as barriers or enablers to providing wound management interventions to hand injured patients is shown in Figure 2 (above).
Identified role and perceived confidence of the Occupational Therapist
The views of participants of their role in providing interventions related to wound management in hand therapy are reported under to following sub-sections: occupational therapists perception of their role in wound management and the confidence of occupational therapists in providing wound management interventions.
Occupational Therapists perceptions of their role in wound management
All participants responded to all descriptors related to the role of occupational therapy (n=106). The majority agreed that, when treating patients with hand wounds, occupational therapists have a role to play in 'treating hand wounds as part of holistic intervention' (91,5%; n=97), 'providing a supportive role in the management of wounds' (87,7%; n=93), 'providing sensory education to prevent wounds' (98,1%; n=104), 'educating patients on wound management' (90,6%; n=96), 'monitoring and referring for issues of concern' (98,1%; n=104), 'monitoring the progression of wound healing' (89,6%; n=95), 'providing environmental adaptations to address occupational dysfunction' (95,3%; n=101), 'providing adapted techniques to address occupational dysfunction' (98,1%; n=104), 'facilitating ongoing employment' (96,2%; n=102), 'enabling participation in meaningful occupations' (98,1%; n=104) and 'understanding the impact of a wound on function and participation' (99,1%; n=105). One participant disagreed with all descriptors listed (0,9%; n=1), and the remainder were neutral. One participant specified that their primary role in wound management within their work setting was scar management (0,9%; n=1).
The analysis of open-ended responses revealed that occupational therapists have a role to play in applying dressings that avoid poor positioning and allow for splinting as well as functional mobility of the hand. Occupational therapists also have a role to play in monitoring the wound for early detection and prevention of possible complications, given that they have the most frequent contact with the patient. Another identified role included an understanding of how a wound may impact treatment planning.
"Occupational therapists can dress the wounds appropriately which does not cause secondary complications such as poor positioning and immobility from thick dressings." (Participant 58)
Participants further expressed concerns around the scope of practice. One participant stated that, due to the demand that may be experienced by occupational therapists to be involved in wound management, the scope of practice of occupational therapists should be carefully considered when considering wound management training. Another participant stated that
"...there is a high demand for occupational therapists working in hand therapy to be able to deal with all the wound care needs. The problem I fear is regarding HPCSA and the role of the occupational therapist and the litigation regarding scope of practice." (Participant 23)
They also stated that wound management training at an undergraduate level "could improve the scope of practice" of occupational therapists.
Confidence of Occupational Therapists in providing wound management interventions.
Participants' level of confidence in using wound management interventions is presented in Figure 3 (above).
Perceived level of preparedness
The perceived level of preparedness of participants to provide wound management interventions are reported under to following sub-sections:
Acquisition of wound management knowledge and skill
When the knowledge and skill to use wound management interventions were obtained is demonstrated in Figure 4 (p50). The acquisition of knowledge and skill can inclusively occur at various stages of professional development thus, participants were permitted to select all appropriate options. Therefore, percentages may total >100%.
Influence of previous training and experience on preparedness for wound management practice
Advanced wound management training (0,9%; n=1) and experience with wound management for patients with burns (0,9%; n=1) were reported as further contributing to preparedness for practice (Figure 5 p51). One participant felt that they had not received sufficient training (0,9%; n=1):
"Not enough done to prepare for treatment requirements." (Participant 56)
Wound management training needs of Occupational Therapists
Ninety-eight participants (92,5%; n=98) agreed that including basic wound management in undergraduate training is required. Ninety participants (84,9%; n=90) disagreed feeling that wound management does not need to be included in undergraduate training as not all new graduates treat patients with hand injuries. Most participants (98,l%; n=104) concurred that wound management courses aimed at occupational therapists treating patients with hand injuries would be beneficial. Forty-seven participants agreed that 'in-service training in settings where there is a demand for therapists to do wound management is sufficient' (44,3%; n=47), with the other participants either remaining neutral (25,5%; n=27) or disagreeing (30,2%; n = 32). Further training needs specified included wound assessment (2,8%; n=3), basic wound management (3,8%; n=4), complex wound management (0,9%; n=1), an understanding of wound management products (0,9%; n=1), wound cleaning methods (0,9%; n=1), selection and/or application of appropriate dressings (3,8%; n=4), tissue healing phases/ stages of healing (1,9%; n=2), sterilisation of instruments (0,9%; n=1), clean procedures for infection control (0,9%; n=1), removal of stitches/staples (0,9%; n=1), videos (0,9%; n=1), theoretical training (0,9%; n=1) and practical experience (2,8%; n=3).
From an analysis of the open-ended responses, participants felt that more in-depth wound management training is needed at an undergraduate level, specifically relating to hand injuries and that specific detail should be mentioned when covering 'hands'; that therapist should be prepared for their first year of work during which they may be exposed to wounds without access to mentorship, especially in rural placements. Participants also felt that wound management knowledge and skill would be transferable to other conditions/injuries such as burns.
"I think it should be done a bit more thoroughly at an undergraduate level too as you see wounds in other fields of occupational therapy too not just hands..." (Participant 39)
Participants felt that postgraduate education should thoroughly cover wound management at an advanced level. A need for continuing professional development courses and in-service trainings for updates on products and orientation to procurement procedures and availability of stock in work settings was brought forward. Several participants felt that a wound management specialist should do the relevant training. Furthermore, participants expressed the need for formalised courses and qualifications targeted at occupational therapists with a concern that attending courses not explicitly aimed at occupational therapists may encourage practitioners to work outside of their scope of practice.
"Should be included thoroughly in postgraduate training and more CPD courses required". (Participant I6)
"Receiving in-service training on products available in your institution is vital...knowing the procedure on how to procure these products is important and can be addressed with in-service." (Participant 45)
DISCUSSION AND IMPLICATIONS
The role of occupational therapy in wound management in hand therapy within the South African context has not been previously reported. The first aim was to describe the current practices of occupational therapists in providing interventions related to wound management to hand injured patients in South Africa.
The study sample (n=I06) was found to be demographically representative of the South African occupational therapy population with regards to gender, geographical distribution, and the sector in which they worked25. Most participants in this study were female (97,2%), which is reflective of the gender discrepancy seen in South African occupational therapists as reported by Ned and colleaugues25. Occupational therapists registered with the HPCSA in 20I8 were 95% female25. The three major provinces from which participants in this study hailed were Gauteng Province (35,8%), the Western Cape (23,6%), and KwaZulu-Natal (18,9%). As reflected in the HPCSA records of 201825, the distributions were Gauteng Province (35,5%), Western Cape (26,6%), and KwaZulu-Natal (I2%). This studies' skewed distribution of participants working in private settings (68,9%) was reflective of the distribution of South African occupational therapists (74,8%)25.
In this study, a high prevalence of wounds in patients with hand injuries was noted, with most participants reporting 50-I00% of these patients encountered having wounds. A relatively large proportion of participants indicated encountering wounds on a daily basis. This therefore supports inferences about the significance of upper limb injuries featuring wounds, within the country. These results are aligned with international literature2, reporting that wounds were within the top ten diagnoses treated by hand therapists. The traumatic nature of injuries for which patients receive occupational therapy in South Africa, as discussed by other authors5-7,16-18 may account for this high prevalence of wounds. Additionally, occupational therapy frequently commences within the first few days of surgery or injury, as highlighted in local studies6,7, which may contribute to the frequency of encountering wounds.
One of the reasons cited to drive the demand experienced by most participants to be involved in wound management was the frequency with which wounds were encountered. Participants reported that patients often follow up more frequently with occupational therapy, and it was more convenient for patients if the occupational therapist includes wound management as part of their holistic treatment. This also allowed the preservation of the patients' finance and time. South African studies717,26 discuss financial constraints of patients as a concern for the continuation of care, corroborating this finding. South African health care users may prioritise earning an income over attending multiple appointments as the financial strain associated with having an upper limb injury is significant15. Routine and frequent care is substantiated by the intensive nature of hand rehabilitation required for functional recovery7. Lack of access to services for wound care, including specialist consultation, contributed to the need for the occupational therapists' involvement with wounds. These findings are supported by previous research emphasising shortages of orthopaedic surgeons as a source of frustration for therapists treating hand injured patients in the public health sector5. Wound and wound healing impacts intervention planning and therapeutic outcomes, which created a need for occupational therapists to be involved. Other studies reiterate that wound healing is a concern for optimal outcomes in hand injuries6,7.
The participants' approach to intervention planning was explored to determine the frequency of considering factors within the components of the ICF. These components are health condition, body function and structure, activities, participation, environmental factors and personal factorsl9. Various factors were specified within the questionnaire. One example is the presence of stitches or staples, a factor within the body function and structure component of the framework. Participants were also asked how frequently they consider the impact of a wound on hand function. Findings demonstrated that various factors within each component, and the impact of a wound on hand function were readily considered when planning intervention. Within the South African context, conditions such as access to running water are essential to note. It is of concern that social and physical environmental aspects were considered less readily than personal and body function and structure elements, similar findings by De Klerkl8 reinforce this point.
Intervention practices were also investigated. A similarity between the frequency of encountering and providing interventions for wounds emerged, with a significant subgroup of the sample intervening daily or several times a day. Keller et al.2found wound management was carried out more frequently in Australia (weekly/ almost weekly) than in the United States and Canada (monthly). The difference in the regularity of providing intervention for wounds in South Africa versus abroad could be attributed to the higher rates of trauma.
Participant feedback highlighted scar management, followed by wound assessment, applying dressings, and cleaning wounds as the most frequent intervention provided. Internationally, these were used in the same order of frequency2. It is worth noting that South African intervention practices closely mirrored international practice.
Patients were often educated on caring for wounds at home, ensuring functional hand use and mobility, and preventing wounds. Both internationally and locally, therapists have been found to provide education regularly2,27. Written wound management instructions were not provided by a large number of participants, citing low levels of literacy and a preference for videos or photographs. Internationally, identifying or producing resources to facilitate education is viewed as routine in hand therapy practice2.
Interventions for the prevention and amelioration of wounds were more frequently provided than interventions facilitating participation in meaningful occupations. This reiterates findings by other authorsl8,26, implying a lack of focus on occupation in hand therapy intervention. However, participants reported providing interventions such as recommending appropriate work-related activities, though it was less frequent than interventions facilitating healing. This indicates some consideration of the work-related engagement and participation needs of patients while other authors7 similarly found that the choice of splint design is guided by consideration for the patients' quicker commencement of work. Although the results of this study imply that activity and participation aspects of the ICF are being addressed, the means of evaluating activity limitations and participation restrictions remains undetermined, warranting further investigation.
Exploring engagement with other members of the MDT indicated that occupational therapists were infrequently the only team member responsible for wound management. Interactions with the MDT were often directed at ensuring positive surgical and rehabilitative outcomes. The AOTA supports a team approach to the provision of wound management1. Therefore, occupational therapists should foster good relationships with the MDT for collaborative efforts towards optimal patient outcomes.
Financial constraints, poor availability of wound management supplies/consumables, and other team members' perceptions of occupational therapists' role were experienced, by most participants, as barriers to wound management. Similar findings in the area of hand therapy were reported in the country5,7,17,26. Communication, knowledge and skills in the MDT were amongst factors experienced as enablers. This further enhances the argument for occupational therapists to build favourable relationships with other team members.
The second aim of this study was to explore the views of occupational therapists of their role and preparedness in managing hand wounds. The findings revealed that occupational therapists identified their role in the provision of interventions within the ICF as addressing body functions and structures elements, as well as activity limitations and participation restrictions components. However, the results revealed that interventions were more frequently geared towards addressing body function and structure impairment. The confidence of occupational therapists in wound management was also explored. Participants were mostly confident, but findings indicated a lack of confidence in mechanical and sharp debridement and staple removal. Notably, these interventions were also infrequently used.
Preparedness was explored by determining when wound management knowledge and skill was acquired, and previous training and experience. There was a trend towards this knowledge and skill being developed within the first two years of practice in hand therapy, reiterating international findings2. However, it emerged that wound assessment, scar management, use of pressure garments and identifying signs of infection, phase of healing and delayed healing was to some extent covered at an undergraduate level. This is in line with the minimum standards for the education of occupational therapists28.
Results demonstrated that theoretical training in undergraduate education somewhat prepared just over half of the participants. However, it was noted that the undergraduate practical fieldwork experience could be reviewed to provide more opportunities for hand therapy and wound management practice. Van Stormbroek and Buchanan5 similarly found a lack of undergraduate fieldwork experience in 'hands' challenging for transitioning into practice. Factors contributing to increased preparedness were clinical experience, observing and working alongside more knowledgeable professionals, and mentorship. International2and local5,7,17,29 studies support these findings.
Finally, the findings of the study illustrated a need for basic wound management to be included in undergraduate training and a concern for the preparedness of new graduates to meet practice demands also emerged. The unpreparedness of newly qualified occupational therapists for hand therapy practice has previously been documented by other South African authors5,29 and the results of this study reiterate those findings. Furthermore, wound management courses and advanced wound management at a postgraduate level were also identified as training needs.
LIMITATIONS OF THE STUDY
The sample was skewed towards occupational therapists working in private practice settings. This is, however, not surprising considering the recruitment processes and potential for sample bias. Examining wound management practices with a sample more representative of public health management may, therefore, be required. Self-selection bias may have skewed the results of the study as individuals who more regularly encounter wounds in practice may have been more likely to respond. The results of this study should be interpreted with caution and are not generalisable to the entire population of occupational therapists treating hand injured patients in South Africa.
CONCLUSION
The frequency of encountering wounds and the demand that occupational therapists experience to be involved in wound management has highlighted the need for improved education and guidance on the role of occupational therapy. The demand for South African occupational therapists to be involved in wound management may be more significant when compared to other countries, as wounds may be more frequently encountered in hand therapy practice within the South African context. The apparent lack of preparedness for wound management in undergraduate education is compounded by the poor articulation of the occupational therapists' role within the South African scope of practice. Occupational therapists also do not readily have access to CPD courses addressing wound management. Subsequently, this element of holistic upper limb rehabilitation may be omitted in practice. Limited supervision and mentorship to newly qualified occupational therapists may further contribute to a lack of confidence in providing wound management. Even though it is not feasible to equip undergraduate students with all the skills they may need for practice, occupational therapists need to be provided with clear guidance on their role and scope with regards to wound care in hand therapy in the country. This may assist in improving the confidence of occupational therapists to seek opportunities for professional growth and development and to advocate for the unique contribution of the profession within an MDT approach to the treatment of patients with hand wounds.
ACKNOWLEDGEMENTS
The authors extend acknowledgement and gratitude to the therapists who participated in this research.
AUTHOR CONTRIBUTIONS
Lezane Esterhuizen was the primary researcher as a Master of Occupational Therapy candidate and was involved in the conceptualisation of the study, instrument development, data collection and analysis and drafting of the manuscript. Pragashnie Govender and Deshini Naidoo served as supervisors of the study and provided critical input into research design, concept development, design of the instrument and review and critique of the article and in writing assistance.
CONFLICTS OF INTEREST DECLARATIONS AND FUNDING
The authors declare no conflicts of interests. The study was not funded by any funding agency. The first author (LE) received tuition remission from the University of KwaZulu-Natal College of Health Sciences towards completion of her Master's degree, from which this paper emanated.
DATA AVAILABILITY STATEMENT
All data curated from this study is pooled and presented in this paper. Reasonable requests for access to the data can be addressed to the corresponding author.
REFERENCES
1. American Occupational Therapy Association. Role of occupational therapy in wound management. American Journal of Occupational Therapy. 2018; 72(Supplement_2): 7212410057pl. http://dx.doi.org/10.5014/ajot.2018.72S212 [ Links ]
2. Keller J, Caro C, Dimick M, Landrieu K, Fullenwider L, Walsh J. Thirty years of hand therapy: the 20l4 practice analysis. Journal of Hand Therapy. 20l6; 29(3): 222-234. http://dx.doi.org/10.1016/j.jht.2016.02.011 [ Links ]
3. International Federation of Societies for Hand Therapy. IFSHT Hand Therapy Practice Profile. International Federation of Societies for Hand Therapy website. http://ifsht.org/sites/default/files/IFSHT_Hand_Therapy_Profile_FI-NALJUNe%202010.pdf Accessed September 10, 2020. [ Links ]
4. American Society of Hand Therapists. Position Paper on Hand Therapists' Scope of Practice 11/08/2011. American Society of Hand Therapists website. http://www.asht.org/sites/default/files/images/Practice/ASHT%20Scope%20of%20Practice.pdf Accessed September 10, 2020. [ Links ]
5. van Stormbroek K, Buchanan H. Novice therapists in a developing context: extending the reach of hand rehabilitation. Hand Therapy. 2017; 22(4): 141-152. http://dx.doi.org/10.1177/1758998317720951 [ Links ]
6. Pilling T, Govender P Profile and management of the firework-injured hand. South African Family Practice. 2016; 58(2): 48-53. http://dx.doi.org/10.1080/20786190.2015.1125167 [ Links ]
7. Mottay N, Govender P Mpanza D. The use of the ICAM splint programme in zone IV to VII extensor tendon repairs: patient outcomes and clinician experiences in a specialised hand unit in SA. South African Journal of Occupational Therapy. 2020;50(2):23-34. http://dx.doi.org/10.17159/2310-3833/2020/vol50no2a4 [ Links ]
8. Erlandsson G. Article Commentary: Cultural differences in hand rehabilitation. Hong Kong Journal of Occupational Therapy. 2011; 21(2): 88-91. http://dx.doi.org/10.1016/j.hkjot.2011.12.001 [ Links ]
9. Hundozi H, Murtezani A, Hysenaj V Hysenaj V Mustafa A. Rehabilitation after surgery repair of flexor tendon injuries of the hand with Kleinert early passive mobilisation protocol. Medical Archives. 2013; 67(2): 115. http://dx.doi.org/10.5455/medarh.2013.67.115-119 [ Links ]
10. O'Brien V Skye J. developing hand therapy interventions based on icf framework for epidermolysis bullosa, the "worst skin disease you have never heard of*": an observational case series. Journal of Hand Therapy. 2018; 31(1): 166-170. https://doi.org/10.1016/j.jht.2017.11.037 [ Links ]
11. Rrecaj S, Martinaj M, Murtezani A, IbrahimiKacuri D, Haxhiu B, Zatriqi V Physical therapy and splinting after flexor tendon repair in Zone ll. Medical Archives. 2014; 68(2): 128. http://dx.doi.org/10.5455/medarh.2014.68.128-131 [ Links ]
12. Sposato L, Yancosek K, Cancio J. Psychosocial reactions to upper extremity limb salvage: A case series. Journal of Hand Therapy. 2019; 32(1): 48-56. http://dx.doi.org/10.1016/j.jht.2017.09.003 [ Links ]
13. Young W, Daya M, Govender P. Functional outcome using early controlled active motion in rehabilitation of a replanted hand: a case report. Journal of Hand Therapy. 2020; 33(3): 426-434. http://dx.doi.org/10.1016/j.jht.2018.10.004 [ Links ]
14. Norman R. The high burden of injuries in South Africa. Bulletin of the World Health Organization. 2007; 85(09): 695-702. http://dx.doi.org/10.2471/blt.06.037184 [ Links ]
15. Makobore P, Galukande M, Kalanzi E, Kijjambu S. The burden of hand injuries at a tertiary hospital in ub-Saharan Africa. Emergency Medicine International. 2015; 2015:1-5. http://dx.doi.org/10.1155/2015/838572 [ Links ]
16. Stewart A, Biddulph G, Firth G. The aetiology of acute traumatic occupational hand injuries seen at a South African state hospital. South African Orthopaedic Journal. 2017; 16(4): 49-53. http://dx.doi.org/10.17159/2309-8309/2017/v16n4a8 [ Links ]
17. Naidoo J, Naidoo D, Govender P. Taking a hold of hand trauma in KwaZulu-Natal, South Africa. African Health Sciences. 2021; 21(4). [ Links ]
18. de Klerk S, Buchanan H, Pretorius B. Occupational therapy hand assessment practices: cause for concern? South African Journal of Occupational Therapy. 2015; 45(2): 43-50. http://dx.doi.org/10.17159/2310-3833/2015/v45n2a7 [ Links ]
19. International classification of functioning, disability and health: ICF World Health Organization. http://apps.who.int/iris/handle/10665/42407 Accessed July 12, 2020. [ Links ]
20. Wilkinson D, Birmingham P. Using research instruments - a guide for researchers. London: Routledge Falmer; 2003. [ Links ]
21. Polit DF Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Research in Nursing & Health. 2006; 29(5): 489-497. http://dx.doi.org/10.1002/nur.20147 [ Links ]
22. SASHT 2020 Members Booklet, version 5 as of 22 June 2021. South African Society of Hand Therapists. Accessed May 23, 2020. https://www.sasht.org.za/MEMBERS%20BOOKLET%2007%20JUNE%202021.pdf [ Links ]
23. Leathicia Venter. Email communication. August 04 2020; OTASA administrator. [ Links ]
24. Onwuegbuzie A, Collins K. A typology of mixed methods sampling designs in social science research. The Qualitative Report. 2007; 12(2): 281-316. [ Links ]
25. Ned L, Tiwari R, Buchanan H, Van Niekerk L, Sherry K, Chikte U. Changing demographic trends among South African occupational therapists: 2002 to 20l8. Human Resources for Health. 2020; 18(1). http://dx.doi.org/10.1186/s12960-020-0464-3 [ Links ]
26. de Klerk S, Badenhorst E, Buttle A, Mohammed F Oberem J. Occupation-based hand therapy in South Africa: challenges and opportunities. South African Journal of Occupational Therapy. 2016; 46(3): 10-15.http://dx.doi.org/10.17159/2310-3833/2016/v46n3a3 [ Links ]
27. van Stormbroek K. The extent which community service occupational therapists are equipped to treat patients with upper limb injuries and conditions [Internet]. The University of Cape Town; 2015. Available from: https://open.uct.ac.za/handle/11427/13807 [ Links ]
28. HPCSA. The minimum standards for the education of occupational therapists. 2009. Accessed October l9 2020. https://www.hpcsa.co.za/Uploads/OCP/Policy%20and%20Guidelines/Minimum_Standards_of_OT_Training_Final_22_May_2020.pdf [ Links ]
29. Naidoo D, van Wyk J, Joubert R. Are final year occupational therapy students adequately prepared for clinical practice? A case study in KwaZulu-Natal. South African Journal of Occupational Therapy. 2014; 44(3): 24-28. [ Links ]
* Lezane Esterhuizen. Email: Lezane.esterhuizen@gmail.com














