Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Occupational Therapy
versão On-line ISSN 2310-3833
versão impressa ISSN 0038-2337
S. Afr. j. occup. ther. vol.49 no.2 Pretoria Ago. 2019
http://dx.doi.org/10.17159/23103833/2019/vol49n2a8
SCIENTIFIC ARTICLES
Introducing early active mobilisation following flexor tendon repair in the context of care in a developing country: A randomised feasibility study
Amy Buttle NaudéI; Susan de KlerkII
IB Sc OT (UCT), M OT (SU). Senior Occupational Therapist, Department of Occupational Therapy, Tygerberg Hospital, Cape Town. https://orcid.org/0000-0003-2971-347X
IIB OT (SU), DHT (UP), M OT (SU). Senior Lecturer, Division of Occupational Therapy, Department of Health and Rehabilitation Sciences, Stellenbosch University. https://orcid.org/0000-0001-7639-9319
ABSTRACT
INTRODUCTION: Flexor tendon injuries remain one of the most difficult hand injuries to manage post-operatively. Early active mobilisation protocols are considered 'best practice' internationally but have not been well researched in the developing country context. The feasibility of such research, and use of these protocols, need to be determined by considering the potential for improved functional outcomes for patients, together with various contextual and resource challenges
PURPOSE: To explore aspects of feasibility related to the recruitment, consent and retention rates in consideration of a future definitive Randomised Control Trail. In addition, preliminary results of an early active therapy protocol compared to an early passive therapy protocol were reported on, together with patient satisfaction and demographics
METHODS: A parallel randomised pilot trial design was used. Thirty-one participants were recruited into one of two therapy groups (active or passive). Fourteen of these participants completed their therapy and eight-week assessments including: Total Active Motion, grip strength, the Michigan Hand Questionnaire and the Smith Hand Function Evaluation. 95% Confidence intervals examined feasibility data. Non-parametric data analysis was done primarily using medians and ranges
RESULTS: Feasibility results of 37% recruitment rate, 97% consent rate and 45% retention rate, did not meet the criteria for success, deeming a trial in the present design, not feasible
DISCUSSION: Due to the dearth of research from public health clinical settings in developing countries, this study contributes rich contextual data, but the challenges discussed need to be addressed before further research will achieve success
Key words: Feasibility studies, recruitment-, consent-, and retention rates, early active rehabilitation, activity and participation
INTRODUCTION
Flexor tendon injuries to the hand often result in poor outcomes and restricted functional hand use, with negative implications for independence and quality of life1,2. Flexor tendon rehabilitation aims to achieve a balance between optimal range of motion (ROM) and normal tendon excursion while protecting the repair. In addition, therapists prioritise best possible functioning, ensuring return to valued pre-injury occupations.
Post-operative management of patients following flexor tendon repair has evolved over time, sparked by advances in surgical techniques and suture materials. Post-operative rehabilitation protocols can be broadly grouped into: immobilisation, early passive mobilisation, early active mobilisation, and combination protocols, with management in the first three to six weeks being most critical3. Early active mobilisation protocols have been demonstrated to hold potential for reduced adhesion formation, greater grip strength and ROM, fewer complications and the need for subsequent surgical release, fewer proximal interphalangeal joint (PIPJ) contractures, and no difference in rupture rates4,5,6. Despite these findings, a review of comparative studies evaluating the outcomes of passive versus active mobilisation has shown contradictory results, and there is still much controversy around optimal management protocols. Although early active mobilisation for rehabilitation post flexor tendon repair is more prominently supported by current medical evidence7, a recent United States (US) survey, to evaluate current management trends, found that only 50.5% (207 of 410) of surgeons opt for the use of an early active protocol, whilst the remaining 49.5% (203 of 410) still prefer an early passive protoco17. A lack of an established 'gold standard' in rehabilitation of a repaired flexor tendon3, has led many therapists currently in practice to combine existing concepts from multiple sources to create combination protocols, that meet patient and context needs8. With no conclusive evidence around optimal rehabilitation protocols for this complex injury, there is an ongoing need for research to address the poor functional outcomes. The successful repair and rehabilitation of flexor tendon injuries, presents a challenge to any health setting in both developed and developing contexts.
Rupture rates and ROM have been the primary outcomes used to evaluate the success or failure of flexor tendon repair and rehabilitation protocols9. However, rupture rates do not provide information about the functional and occupational outcomes for patients. In addition, regaining ROM does not automatically translate to return to functional hand use. Outcomes are commonly poor and complications plague the post-operative periodl,2,9. Moreover, there is a dearth of evidence from developing country contexts.
Optimising quality of care and effectiveness of interventions in occupational therapy, relies on sufficient accessible evidence10. The requisite for research from developing countries is further necessitated by the unique additional factors at play in such a context (further explored in this article). There also exists a need to expand upon the use of outcome measures in this field beyond only rupture rates and ROM. An early active mobilisation protocol was developed, based on the consideration of best current evidence, the patient population and the context.
Experiential context and feasibility
A variety of challenges are faced throughout the process of flexor tendon rehabilitation of individuals within developing country contexts. Due to issues such as fragmentation of health systems, poor access to health services, poor public transport infrastructure, over-burdened hospital facilities, and over-extended healthcare professionals, individuals who sustain hand injuries do not always have access to optimal management11. Lack of specialised knowledge, and over-run systems may lead to the mis-diagnosis of patients who present with a traumatic hand injury at a clinic or primary health care facility. If patients are referred to specialised hand units in time, the required surgical procedure may be delayed for a number of reasons, including but not limited to bed shortages and lack of theatre time.
Issues of access to health care are a vital consideration in this context. Levesque et al.12 offer a broad definition of access in their conceptual framework, where access is seen as the opportunity to recognise healthcare needs, seek healthcare services, attain those services and to have that need for services met. Their framework describes five dimensions of accessibility, which interact with five corresponding abilities of populations, to generate access12. According to this framework, this study considers the dimensions of availability, appropriateness and af-fordability, in relation to the selected interventions and aspects of feasibility.
Considering the contextual barriers and challenges in routine service delivery, the feasibility of a randomised controlled trial was indicated. In recent years there has been an appeal from practitioners for more studies to be conducted in settings where community constraints take preference over optimum conditions, considering the fit of interventions to real-world settings13. In research literature, feasibility studies assist in bridging this gap and are defined as any study that aids researchers in preparation for a full-scale trial leading to a change in practice13. Of the eight focus areas of feasibility studies described by Bowen et al.13 this study highlighted the aspects of acceptability, practicality, implementation, and limited-efficacy testing. The primary study objectives were to determine the feasibility of the: 1) recruitment rate of patients with flexor tendon injuries to the fingers (in zones I - IV), within the first week post repair at a tertiary academic state hospital in Cape Town, 2) consent rate, and 3) retention rate. The study also described the contextual and demographic factors in relation to the primary outcomes of recruitment, consent and retention rates. The study considered the feasibility of the selection criteria, delivery of an early active therapy protocol in this context, selected outcome measures, and patient satisfaction. In addition, the preliminary results of the pilot are reported, evaluating whether an early active mobilisation flexor tendon repair (FTR) protocol yields better functional outcomes, compared to a passive mobilisation FTR protocol, in a developing context. The rationale for piloting lies in assessing aspects of the processes, resources and management required for such a trial, with a secondary outcome being the consideration of the effect of interventions across the two groups14. The second outcome was considered in order to pilot the methods that would be required in an RCT, and not primarily to report on efficacy.
METHODS
Trial Design
This parallel randomised pilot trial adheres to the CONSORT (Consolidated Standards for Reporting Trials) 2010 guidelines for reporting a pilot or feasibility trial15 (the completed checklist is available from the first author). This provides an appropriate resource for the authors to offer clear, complete and transparent reporting on the pilot trial, particularly in relation to internal and external validity. Participants were recruited into two groups (active or passive), where allocation was by equal randomisation (i.e. 1:1). This allocation provides the greatest power for testing effectiveness for a future randomised control trial (RCT)15. Randomisation allows for comparison between the two groups, and reduces the influence that confounding variables, such as age, gender, ethnicity, and occupation, have on the outcomes16.
Sampling
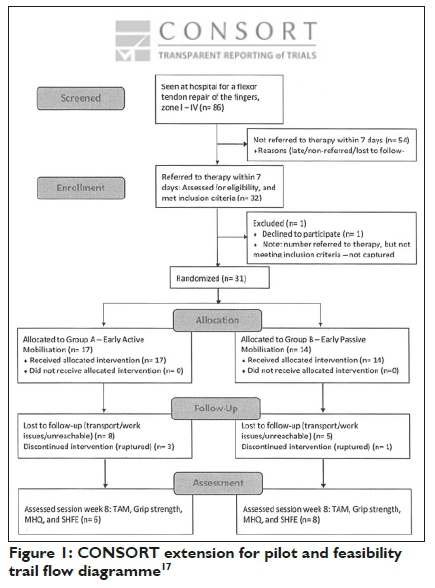
The sample size for a future RCT, was determined through statistical calculation using the selected outcome measures. A sample size of 48 (24 patients in each group) was determined to ensure statistically and clinically significant results that would achieve a power of 81% (to reject the null hypothesis) in such a trial. The CONSORT extension for pilot and feasibility trials flow diagram17(Figure 1 on page 50) demonstrates the randomisation of patients within this trial as well as accounting for those lost to follow-up and the number of patients included in the final measurement and analysis per intervention group. A population sample was used, with the population of interest being all patients with flexor tendon injuries referred to an occupational therapy department hand service, within a tertiary academic state hospital (Tygerberg Hospital, Cape Town, South Africa). Participants had to be recruited within one week of their surgery to meet the inclusion criteria and allow for early mobilisation3.
Feasibility Criteria
Feasibility criteria for success included recruitment rate, consent rate, and retention rate.
The criteria for determining feasibility of a RCT involved recruitment of at least 94% of all eligible patients within the facility, which translates to eight patients per month, thus a total of 60 over an eight-month period, based on an informed estimation of the average number of patients managed at the facility per month (n = 8). Consent rate should be at least 97%, with no more than 2 of 60 patients declining. Retention rate of at least 83% of recruited patients is needed (83% of the remaining 58 participants). This calculation therefore provides for 48 participants for a feasible RCT. This translates to a loss to follow-up rate of 17%. International literature in the field of flexor tendon rehabilitation reports a loss to follow-up rate of between 7.7% and 15% 418,19.
Recruitment measures
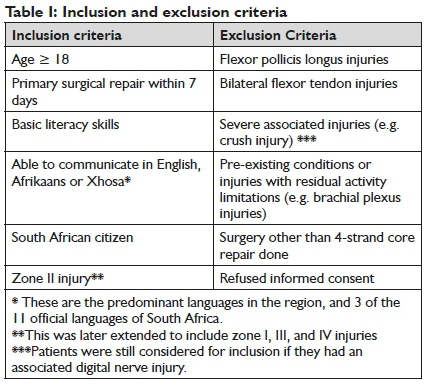
Measures to ensure timely referral of potential participants included: emails to all orthopaedic doctors in the department, announcements and reminders at staff meetings, notices posted in the theatres, liaison with the head of the orthopaedic department, the hand specialist, and relevant nursing staff. Patients were referred, either after their surgery, in which case the first author provided an appointment date, or when they returned for their first outpatient appointment at the hand unit. Patients were selected according to criteria in Table I below.
Informed consent and ethical considerations
Approval from the Stellenbosch University, Health Research Ethics committee was obtained prior to conducting this research (reference number: SI6/07/122). Approval from the facility in accordance with the Provincial Research Policy and Tygerberg Hospital Notice No. 40/2009, was obtained. All participants gave their signed informed consent prior to inclusion, once the study and objectives were explained to them. Consent forms were available in English, Afrikaans and isiXhosa, translators were used if indicated.
Randomisation
Randomisation of patients to intervention groups was performed prior to initiating therapy. An allocated staff member drew a card indiscriminately from an envelope with an equal number of cards labelled 'active' and 'passive' to assign each participant to either group A (active-experimental group) or group B (passive-control group). This staff member informed the first author (therapist) or second therapist of each participant's group allocation. Once a card was removed and a patient recruited into the study, and randomised into one of the two therapy groups, this card was then placed in a separate envelope labelled accordingly. (Figure 1 below)
Intervention
Once the operative dressings were removed, therapy was initiated with the patient, according to their group allocation. Participants in both groups were seen for their first therapy session within the first post-operative week, receiving a total of five to six, 45-min-ute, sessions over eight to ten weeks. Participants in group A, the experimental group, received a dorsal splint (position: wrist in neutral to 20° extension, metacarpal phalangeal joints in 80° flexion and interphalangeal joints in extension), and began with a therapy protocol designed for the purpose of this study. Focus of this protocol was on controlled, graded, active digital flexion and extension from the initial session. Participants in group B, the control group, received a dorsal splint (position: wrist in neutral to 20° flexion, the metacarpal phalangeal joints in 60-80° flexion, and the interphalangeal joints in extension), and began with what is 'treatment as usual' at this hand therapy service. This protocol was a 'modified Duran'20 inspired protocol, the focus of which was on passive digital flexion. Active finger flexion, in this protocol, was only introduced at four and a half to five weeks post repair.
Surgical Technique
The surgical procedure for this repair, consists of a 4 strand core suture using a 3/0 braided material, either Ethibond or Tycron, the repair is then over-sewn with a continuous nylon 6/0 suture2I. According to clinical evidence and biomedical studies, the use of this surgical technique is enough to provide the tensile strength required for the repair to withstand early active motion without tendon rupture4,22,23.
Outcome Measures and Data Collection
The initial patient information form captured demographic and injury information such as age, gender, hand dominance, number of affected fingers, mechanism of injury, and associated injuries. A variety of measures were selected to evaluate aspects of activity and participation24 in addition to predictable use of rupture rate and ROM. Outcome measures were administered once at the eight-week data collection session in both groups. The assessor was an independent therapist, blinded to group allocation. The outcome measures, in administered order, were: I) joint ROM, using goniometry and the Total Active Motion (TAM) system25, 2) grip strength, using the Jamar dynamometer26,3) patient rated assessment of satisfaction and hand function, with the Brief Michigan Hand Questionnaire (MHQ)27, and 4) an objective measure of functional hand use, using the Smith Hand Function Evaluation (SHFE)28. See Table II on page 51 for details.
The importance of follow-up at therapy was emphasised with patients and patients were educated on the need for follow-up therapy in order to obtain the best possible outcomes for their hand. Follow-up instructions included the date, time and place of the follow-up appointment, the therapist's name, the occupational therapy department number, and what to do if they were unable to attend a follow-up appointment. The follow-up instructions were explained to each participant by the therapist and the appointment was clearly written on their hospital appointment card, handed back to them at the end of a visit. Patients who missed their appointment were contacted by phone, by the first author, if she could reach them, to reschedule. These processes were followed in order to minimise loss to follow-up.
Pragmatic deviations from the original protocol
The randomised pilot trial protocol was amended to include zone I, III and IV injuries in addition to zone II injuries over the 16 month period, as it was evident following the first eight months that recruitment of persons with zone II injuries only were low (n = II after first eight months). As a result, the measurement for ROM was changed from Strickland an Glogovac's29 original system, measuring only interphalangeal joint ROM, to the TAM method, including metacarpal phalangeal joint ROM, as per the American Society for Surgery of the Hand25. In addition, one foreign citizen participant was included, as he was in the process of obtaining citizenship and met all other selection criteria.
Statistical analyses
95% Confidence intervals (CIs) were calculated for the primary objectives related to feasibility in order to make inferences to the population. Descriptive statistics were used to categorise demographics and performance for each group. Analyses were performed using IBM SPSS version 25. Due to the small sample size and lack of normal distribution of the data, primarily non-parametric measures were used. Demographic data of participants were descriptively summarised by medians and interquartile ranges.
RESULTS
The recruitment period was November 2016 to March 2018. The facility saw a total of 86 patients with flexor repairs to the hand in this period, 32 of these patients were successfully referred and invited to participate, resulting in a recruitment rate of 37% (95% CI: 27.22% - 48.35%). One patient declined participation, resulting in a 97% consent rate (95% CI: 82% - 99.84%). Fourteen of the 31 patients recruited went on to complete their therapy programme and eight-week assessment session, resulting in a retention rate of 45% (95% CI: 27.78% - 63.70%). Seventeen participants dropped out of the trial, not returning for scheduled appointments, and the first author was unable to reach them. Of the 31 participants who were randomised, the ratio of male to female participants was 23:8, 74% male and 26% female (see Table III on page 51). The mean age of participants was 29 years (range: 18-50 years). The trial was stopped as it became evident that insufficient eligible patients were accessed over a protracted time frame (16 months), despite preparatory research around the average number of these patients treated at the facility. However sufficient feasibility data were obtained. Recruitment rates were low, drop-out rates high and various contextual barriers were experienced. There were four participants that experienced rupture, these were however not related to treatment received, for example one participant removed his splint while showering, slipped in the shower and ruptured the repair. Participant demographics and injury variables are summarised in Table III on page 51. Preliminary results for each outcome measure, at eight weeks, per randomised group are reported in Table IV above. Results of these outcome measures are inconclusive, and should be viewed with caution, in light of the small sample size.
DISCUSSION
This study examined feasibility criteria, recruitment, and consent and retention rates, in a randomised pilot trial comparing two post-operative therapies for patients with flexor tendon injuries to the hand.
Recruitment
Recruitment was slow and unpredictably difficult. There were suitable information pathways and adequate patient numbers, however referrals to therapy services, were often received too late to meet the study's inclusion criteria. The recruitment rate of 37% (32 of 86) points to the barriers in this setting related to recruitment. The referral of the target population was lower than expected.
Despite high health expenditure, the South African public health care system is still considered unequal, racially skewed30, underdeveloped and weak. It continues to struggle to overcome poor administrative management, low morale, lack of funding, and shortages of medical personnel - a high percentage of whom are absorbed into the private sector11,31. These challenges relate to the dimension of availability, by Levesque et al.12, the physical health resources and capacity to produce these resources. The challenges and fragmentation of the health care system translate into barriers at the practice level, which pose a threat to research procedures11. These barriers include ineffective communication systems, difficulties with carry-over of referral information, long patient waiting times32, incomprehensive documentation for surgeries performed, poor information systems, non-uniformity in surgical techniques, high patient turn-over, repairs done without patients being admitted, under-resourced facilities, and limited human resources32. These could have been contributing factors to the unsuccessful recruitment of these patients, and the target of recruitment within allotted and expanded timeframes was not met. According to the criteria for success of feasibility, this randomised pilot trial demonstrated that despite the 'on paper' feasibility of recruitment of patients with flexor tendon injuries in this setting, recruitment in reality was far below the anticipated rate. The eligibility of the referred and screened population was also slightly lower than anticipated, indicating that the inclusion criteria may have been too stringent. Future research should consider including foreign citizens, especially in areas where there is a large population of foreign citizens, as well as children aged twelve to seventeen, as their ability to follow a therapy protocol has been observed in practice33.
Consent
Consent rate was almost 100% with the exception of one patient. Despite clear explanation regarding the trial, patients might have had the sense that participation would somehow lead to 'special treatment', which may have introduced a performance bias. However this was not formally investigated in the trial. The point of recruitment, at the initiation of therapy, was found to be appropriate and feasible. This reflects the dimension of accessibility that Levesque et al.12 refer to as appropriateness. There was a good fit for the point of recruitment, within the context of this feasibility study.
Retention
The retention rate was low, with a dropout rate of more than half the participants (55%). There were no obviously notable differences in demographics between those who dropped out and those who were retained in the trial, pointing to there being no 'loss to follow-up bias'. Those who dropped out, did so randomly however there were some trends that emerged as a result of the high dropout rate. These should be viewed with caution considering the small sample size. Of the mechanisms of injury, those whose injury was sustained through violence were most likely to drop out, 11 of 18 (61%), compared with those who dropped out in the group who were injured accidently, 6 of 11 (55%), and all were retained among those who sustained work-related injuries 0 of 2 (0%). With 59.9% of the injuries in this trial as a result of violent injury, there could be a correlation between 'mechanism of injury' and drop out, not investigated in this study. Considering zone of injury, participants with zone III injuries had the highest dropout rate of all zones (6 of 8, 75%), this may be of interest for future research when developing selection criteria.
Retention was also worst in the group who sustained injury to one finger only (14 of 20, 70%), as opposed to those who sustained injury to two or more fingers. This is possibly due to the fact that participants felt they could manage functionally with restricted use of only one finger, as opposed to multiple. Related to this notion is the high dropout rate in those participants who had an injury to their dominant hand, 11 of 17 (65%) of participants with dominant hand injuries as opposed to a dropout of only 35% (6 of 17) in those that had a non-dominant hand injury. This seems to support an observation in practice, in a largely casual job market, with a no-work, no-pay policy. Patients are often more motivated to return to work when they notice any improvement, often sacrificing potentially better functional outcomes in order to be able to earn again. Across both groups, the majority of participants were employed prior to injury, 11 ofl4, 79% in the passive group and 13 of 17, 77% in the active group. Median duration from surgery to initiation of therapy was similar in both groups, 6 days for those in the passive group and 5 days for those in the active group. A larger proportion of the participants in the active group had an injury to their dominant hand, 12 of 17, 71% (versus 7 of l4, 50% in the passive group whose dominant hand was injured). This might also help to explain the higher dropout rate in the active group.
The participants who dropped out had a longer duration from injury to surgery (median of 6 days in patients who dropped out vs. 3 days where patients were retained), which could point to poor personal health seeking behaviours or poor health service delivery. It became evident that those not employed prior to their injury, were more likely to drop out.
Overall, identifiers for dropout in this trial included mechanism of injury (i.e. sustained due to violence), level of injury (i.e. zone III), nature of injury (i.e. number of involved fingers), hand dominance (i.e. injury to dominant hand), waiting period (i.e. longer duration from injury to surgery), and employment status (i.e. unemployed prior to surgery).
The high rate of dropout, as evident from the limited possible post drop-out telephonic communication, points primarily to the patient circumstances such as poverty, unemployment, inefficient public transport and poor access to public services. Reasons for dropout could not be definitively reported for all participants, as not all of them could be reached. From the participants who could be contacted, the most commonly reported reasons for loss to follow-up were the lack of money for transport to the facility, and issues with being away from work, which were also reasons cited by Wentzel34. Research in trauma and orthopaedic settings from other countries has explored various factors and demographics that are associated with a higher chance of dropout in treatment and research. Common risk factors included: male gender, current smokers, younger than 30 years, high alcohol and substance use, and lack of health insurance35,36. Increased efforts to maintain contact with patients identified as being at higher risk of not following up, may help to decrease the possible complications resulting from unmonitored recovery37.
Factors influencing the follow-up of patients, however is intractably linked to their setting. In a South African Orthopaedic study, Badenhorst et al.38 identified three main factors influencing loss to follow-up, namely distance to travel, BMI and HIV status. The factor of distance can be linked to the finding in this research of 'lack of money for transport' arising as a reason for dropout. The distances in the present research were far less than those reported by Badenhorst et al.38 thus it is likely that poor transport infrastructure and poverty, rather than purely distance, are reasons for the high dropout rates. Affordability as a dimension of accessibility12 is reflected here, with the constrained economic capacity of the population. Considering the demographics of the patients included in this study, it could have been valuable to explore whether a correlation exists between those lost to follow-up and the distance that they reside from the hospital.
Wentzel34 discussed how loss to follow-up was also one of the main factors affecting the results of her research exploring a comparison of rehabilitation protocols post flexor tendon repair. By the first follow-up session, at four weeks post-surgery, she reported a 23.9% loss to follow-up rate, and an overall loss to follow-up rate of 39.l3%. In the discussion she suggests that a relationship between loss to follow-up and socio-economic status could exist, proposing the factors of education level, employment status and access to finances for transport, as possible reasons for this relationship. Further research is indicated in this context to explore and address reasons for loss to follow-up. Spark39 experienced a loss to follow-up rate of 48% in her research on flexor tendon rehabilitation. This loss to follow-up rate was similar to what was experienced in the present trial (55%).
With review of these results, it can be noted that the initially anticipated loss to follow-up rate was perhaps not conservative enough, taking into account the challenges known to government health care settings and citizens in South Africa.
Attempts were made with all patients to ensure maintained follow-up. However with the results of this study, further measures could be put in place to address issues of loss to follow-up, particularly among those patients who possess any of the contributing factors in this setting. Examples here could include sending a message reminder of appointment dates to participants the day prior to their session. Participants could also be reminded of their commitment to the programme at the start of each session, promoting a sense of responsibility in the process. This would also assist in reducing number of complications and poor outcomes.
In accordance with the study design, recruiting adequate numbers of patients with flexor tendon injuries and repairs is not feasible, and retention is inadequate. In addition, the change to early referral of patients with flexor tendon repairs in this setting, was vital to allow for early mobilisation, and consideration for inclusion. However, because early referral, within one week post repair, was not yet common practice at this facility, this too resulted in patients being referred too late and not meeting inclusion criteria (affecting recruitment).
Feasibility and utility of selected outcome measures
Preliminary results of the selected outcome measures for the trial were reported. Assessment of functional hand use, activity and participation, and patient satisfaction are not common practice in reported trials in flexor tendon rehabilitation studies. In a systematic review of flexor tendon rehabilitation protocols in zone II of the hand, only one study was found that reported quality of life using a validated scale9. Chesney et al.9 conclude that future studies should include such outcomes, emphasising the importance of these measures becoming common place in these trials.
The MHQ is a measure of patient satisfaction with one's functional outcome as well as activity and participation. There was almost a 15-point difference in the median of this score between the two groups, in favour of the active group. The minimal clinically importance difference (MCID)40 for this outcome measure related to conditions of the hand and forearm has been determined to fall between 8 and 1340. The authors therefore suggest that the difference of15 in the median scores between the two groups, could point to a clinically important difference in patient satisfaction in the areas of hand function, pain, work performance, and aesthetics in the active group. Instruments such as the MHQ can assist therapists in refocusing their attention on people's personal, social and practical experiences, going beyond reductionist treatment of aspects of body function and structure.
Grip strength was higher overall in the active group. The proportion of participant's fingers that obtained an overall active ROM in either the 'excellent' or 'good' range was 54% (13 of 24) in the active and 47% (15 of 32) in the passive group. There was no statistically significant difference in the time taken between the two groups to complete the items in the SHFE. However, when results were analysed against how many sessions the participants had attended, certain test items held statistical significance, calculated at p = < 0.05. Participants who had had five sessions or more, performed statistically better on the items of: repositioning of nails with the right hand (p = 0.029), fastening the buckle (p = 0.001), tying a bow (p = 0.004), and doing up of laces (p = 0.029).
Although there were statistically significant differences for those who had had more therapy sessions on these items, this holds little clinical significance, in reality taking a few seconds longer to tie one's laces holds little practical relevance41.
Each assessment session took no longer than 30 minutes to administer the four outcome measures. The MHQ could be completed independently by the participant once explained. The SHFE was novel to most participants who appeared to appreciate the experience of completing the various simulated tasks. Overall measures selected were acceptable to participants, time efficient and convenient to administer, while also capturing information about function, activity and participation. The use of this combination of outcomes in future research on the topic would be recommended.
Strengths and Limitations
The methodological strengths of this trial design lay in the high consent rate at the initiation of therapy, after potential trial participation was discussed in detail by the therapist. Another strength that can be carried forward into future research was the careful selection of outcome measures that were appropriate to the patient population and injury, and were time efficient while still maintaining a focus on patients' function and satisfaction. Another strength lies in the insights gained into certain 'areas of focus'13 of feasibility studies, namely acceptability, implementation, practicality, and limited-efficacy testing. Acceptability of the intended intervention, as well as assessing how individual patients reacted to involvement in a study was made evident. The extent to which the study procedure could be implemented as planned was assessed and analysed. Practicality, in terms of time and resource constraints, was considered. Lastly, the intervention was tested in a limited way, as would be done in a future trial, with intermediate rather than final outcomes.
The small sample size in this trial was a major limitation, and participant numbers for statistically significant results could not be obtained. This limits the generalisability to a broader population, although not the primary purpose of the trial. A larger sample size based on the formal power calculation would be needed to determine significant differences in outcomes over time between the two therapy groups. To this end it is suggested that cluster recruitment be considered in future, with more institutions involved to increase access to eligible patients. The fact that this injury is so widely researched internationally suggests that a provincial or national registry could be set up with details of every patient who has sustained this injury and would be interested in participating in a trial. This data-base can be made available to those embarking on future research in this field.
As randomisation was not completed, this may have introduced a randomisation bias, with more participants in the one group than in the other. Stratification in the randomisation process would have been beneficial to achieve a greater balance between the two groups in terms of size and characteristics, as well as account for the extension of the inclusion criteria to zones I-IV. The short time of therapy prior to assessment (eight weeks) was a limitation, and data collection was limited to one assessment session. This was done due to patient circumstances but may have been too short to determine long term effects of the therapy protocols, and the rate of progress between the two groups. Limited human resources to manage the trial's logistical requirements (therapists and blinded assessors) presented a limitation.
The retention rate of 45.5% points to the need for a future trial to recruit and randomise more than double the number required for the end point analysis. The potential correlation between a violent mechanism of injury and retention should be studied further. The inclusion criteria were potentially too narrow. Future research should consider obtaining ethical approval to recruit children aged 12 to 17 years, and foreign citizens, legally and ethically. Further research is required to explore reasons for the high loss to follow-up rates, and how these may be addressed. Correlations between loss to follow-up and factors such as distance from the hospital, employment and socio-economic status should be further considered.
Another limitation was the incomplete data related to whether or not participants smoked. This was not recorded for all participants, and the first author was unable to reach participants retrospectively. This factor could not be considered in analysis of outcomes and retention.
CONCLUSION
This research was able to provide rich feasibility data regarding a randomised pilot trial of this nature in settings in developing country contexts. Various barriers limit the potential to conduct research with aims related to efficacy. The trial demonstrated a failure to meet the criteria for feasibility. Preliminary results related to the outcome measures and demographics across the two groups were reported but need to be viewed with caution. A larger study could address this research question (early active vs. passive mobilisation) with this patient population in future, once contextual barriers that threaten feasibility, have been addressed, and the protocol adjusted according to findings and recommendations reported here. Outcome measure selection in this study proved to be time efficient, whilst still capturing aspects of activity and participation of patients, relating to occupational outcomes.
ACKNOWLEDGEMENTS
The authors thank all the participants for their time in study participation. They also thank the staff at Tygerberg Hospital Orthopaedic, and Occupational Therapy departments. The Ruth Watson Research Grant was awarded to the first author for this study in 2018, and is gratefully acknowledged.
REFERENCES
1. Kaskutas V Powell R. The impact of flexor tendon rehabilitation restrictions on individuals' independence with daily activities: implications for hand therapists. J Hand Ther. 2013;26(1):22-29. https://doi.org/10.1016/j.jht.2012.08.004. [ Links ]
2. Fitzpatrick N, Finlay L. "Frustrating disability": The lived experience of coping with the rehabilitation phase following flexor tendon surgery. Int J Qual Stud Health Well-being. 2008;3(3):143-154. http://doi.org/10.1080/17482620802130407. [ Links ]
3. Pettengill KM. The evolution of early mobilization of the repaired flexor tendon. J Hand Ther. 2005;18(2):157-168. http://doi.org/10.1197/j.jht.2005.011.007. [ Links ]
4. Trumble TE, Vedder NB, 3rd JGS, Hanel DP Diao E, Pettrone S. Zone-II flexor tendon repair: a randomized prospective trial of active place-and-hold therapy compared with passive motion therapy. J bone Jt surgeryAmerican Vol. 2010;92(6):1381-1389. https://doi.org/10.2106/JBJS.H00927 [doi]. [ Links ]
5. Baktir A, Turk CY Kabak S, Sahin V Kardas Y Flexor tendon repair in zone 2 followed by early active mobilization. J Hand Surg Br. l996;2l(5):624-628. https://doi.org/10.1016/s0266-7681(96)80145-8. [ Links ]
6. Starr HM, Snoddy M, Hammond KE, SeilerJG. Flexor tendon repair rehabilitation protocols: A systematic review. J Hand Surg Am. 2013;38(9):1712-1717.el4. https://doi.org/10.1016/j.jhsa.2013.06.025. [ Links ]
7. Gibson PD, Sobol GL, Ahmed IH. Zone II Flexor Tendon Repairs in the United States: Trends in Current Management. J Hand Surg Am. 2017;42(2):e99-e108. https://doi.org/10.1016/j.jhsa.2016.11.022. [ Links ]
8. Sammer DM, Chung KC. Advances in the healing of flexor tendon injuries. Wound Repair Regen. 2014;22:25-29. https://doi.org/10.1111/wrr.12161. [ Links ]
9. Chesney A, Chauhan A, Kattan A, Farrokhyar F Thoma A. Systematic review of flexor tendon rehabilitation protocols in zone II of the hand. Plast Reconstr Surg. 2011;127(4):1583-1592. https://doi.org/10.1097/PRS.0b0l3e318208d28e . [ Links ]
10. Takata SC, Wade ET, Roll SC. Hand therapy interventions, outcomes, and diagnoses evaluated over the last 10 years: A mapping review linking research to practice. J Hand Ther. 2016. https://doi.org/10.1016/j.jht.2017.05.018. [ Links ]
11. Coovadia H, Jewkes R Barron P Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374(9692):817-834. https://doi.org/10.1016/S0l40-6736(09)60951-X. [ Links ]
12. Levesque J-F Harris MF Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12(1):l8. https://doi.org/10.1186/l475-9276-12-18. [ Links ]
13. Bowen DJ, Kreuter M, Spring B, et al. How we design feasible studies. NIH Public Access - Am J Prev Med. 2010;36(5):452-457. https://doi.org/10.1016/j.amepre.2009.02.002. [ Links ]
14. Thabane L, Ma J, Chu R. Commentary. A tutorial on pilot studies: the what, why and how. BMC Medial Res Methodol. 2010;10:1-10. https://doi.org/10.1186/l471-2288-10-l. [ Links ]
15. Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ. 2016;355:l-32. https://doi.org/10.ll36/bmj.15239. [ Links ]
16. Law M, Stewart D, Pollock N, Letts L, Bosch J, Westmorland M. Critical review form-Quantitative studies. McMaster Univ Occup Ther Evidence-Based Pract Res Gr. l998. [ Links ]
17. Moher D, Hopewell S, Schulz KF et al. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. Int J Surg. 2010;10(8):28-55. https://doi.org/10.1016/j.ijsu.2011.10.00l. [ Links ]
18. Kitis PTA, Buker N, Kara IG. Comparison of two methods of controlled mobilisation of repaired flexor tendons in zone 2. Scand J Plast Reconstr Surg Hand Surg. 2009;43(3):160-165. https://doi.org/10.1080/02844310902864122. [ Links ]
19. Bainbridge LC, Robertson C, Gillies D, Elliot D. A comparison of post-operative mobilization of flexor tendon repairs with "passive flexion-active extension" and "controlled active motion" techniques. J Hand Surg Am. 1994;19(4):517-521. https://doi.org/10.1016/0266-7681(94)902l9-4. [ Links ]
20. Duran RJ, Houser RG. Controlled passive motion following flexor tendon repair in zones 2 and 3. In: AAOS Symposium on Tendon Surgery in the Hand. CV Mosby St. Louis; 1975:105-114. [ Links ]
21. Ikram A SK. Flexor Tendon, Research Protocol [Unpublished Research Protocol]. Stellenbosch; 2015. [ Links ]
22. Matthews P, Richards H. The repair potential of digital flexor tendons. An experimental study. J bone Jt surgery British Vol. 1974;56- B(4):618-625. https://doi.org/10.1302/030l-620x.56b4.618. [ Links ]
23. Thurman RT, Trumble TE, Hanel DP, Tencer AF, Kiser PK. Two-, four-, and six-strand zone II flexor tendon repairs: an in situ biome-chanical comparison using a cadaver model. J Hand Surg Am. 1998; 23(2):261-265. https://doi.org/10.1016/S0363-5023(98)80124-x. [ Links ]
24. Stucki G, Kostanjsek N, Ustun B, Cieza A. ICF-based classification and measurement of functioning. Eur J Phys Rehabil Med. 2008;44(3):315-328. [ Links ]
25. Kleinert HE. Report of the Committee on Tendon Injuries. J Hand Surg Am. l983;8(5):794-798. https://doi.org/10.1016/S0363-5023(83)80275-5. [ Links ]
26. JAMAR Hydraulic Hand Dynamometer: User Instructions. In: Indiana, USA: Lafayette Instrument Company Inc.; 2004. [ Links ]
27. Waljee JF Kim HM, Burns PB, Chung KC. Development of a brief, 12-item version of the michigan hand questionnaire. Plast Reconstr Surg. 2011;128(1):208-220. https://doi.org/10.1097/PRS.0b0l3e3182l8fc51. [ Links ]
28. Smith HB. Smith hand function evaluation. Am J Occup Ther Off Publ Am Occup Ther Assoc. 1973;27(5):244-251. http://search.ebscohost.com/login.aspx?direct=true&db=cmedm &AN=4716362&site=ehost-live&scope=site. [ Links ]
29. Strickland JW, Glogovac SV Digital function following flexor tendon repair in zone II: a comparison of immobilization and controlled passive motion techniques. J Hand Surg Am. 1980;5(6):537-543. [ Links ]
30. Mayosi BM, Lawn JE, Van Niekerk A, Bradshaw D, Abdool Karim SS, Coovadia HM. Health in South Africa: Changes and challenges since 2009. Lancet. 2012;380(9858):2029-2043. https://doi.org/10.1016/S0l40-6736(12)61814-5. [ Links ]
31. Chopra M, Lawn JE, Sanders D, et al. Achieving the health Millennium Development Goals for South Africa: challenges and priorities. Lancet. 2009;374(9694):1023-1031. https://doi.org/10.1016/S0l40-6736(09)61122-3. [ Links ]
32. Mayosi BM, Lawn JE, Van Niekerk A, Bradshaw D, Abdool Karim SS, Coovadia HM. Health in South Africa: Changes and challenges since 2009. Lancet. 2012;380(9858):2029-2043. https://doi.org/10.1016/S0140-6736(12)61814-5. [ Links ]
33. Cooper L, Khor W, Burr N, Sivakumar B. Flexor tendon repairs in children: Outcomes from a specialist tertiary centre. J Plast Reconstr Aesthetic Surg. 2015;68(5):717-723. https://doi.org/10.1016/j.bjps.2014.12.024. [ Links ]
34. Wentzel R Dissertation for the Faculty of Health Sciences School of Health Care Sciences: A Comparison of the outcomes of two rehabilitation protocols after flexor tendon repair of the hand at Chris Hani Baragwanath Academic Hospital (Protocol number:314/2014). 2014; (January 2017). https://doi.org/10.I177/1558944716660555js. [ Links ]
35. Madden K, Scott T, McKay P, et al. Predicting and preventing loss to follow-up of adult trauma patients in randomized controlled trials an example from the FLOW trial. J Bone Jt Surg - Am Vol. 2017;99(I3):1086-1092. https://doi.org/10.2106/JBJS.I6.00900. [ Links ]
36. Zelle BA, Buttacavoli FA, Shroff JB, Stirton JB. Loss of Follow-up in Orthopaedic Trauma. J Orthop Trauma. 2015;29(II):510-515. https://doi.org/10.1097/BOT.0000000000000346. [ Links ]
37. Tejwani NC, Takemoto RC, Nayak G, Pahk B, Egol KA. Who is lost to followup?: A study of patients with distal radius fractures. Clin Orthop Relat Res. 2010;468(2):599-604. https://doi.org/10.1007/sI1999-009-0968-6. [ Links ]
38. Badenhorst DHS, Chb MB, Sa FCO, et al. Lost to follow-up : Challenges to conducting orthopaedic research in South Africa. South African Med J. 2018; 108 (II): I-5. https://doi.org/10.7196/SAMJ.2018.v108iII.I3252. [ Links ]
39. Spark T. The impairments and functional outcomes of patients post flexor tendon repair of the hand at an academic hospital in Johannesburg, South Africa. A dissertation submitted to the Faculty of Health Sciences, University of the Witwatersrand. 2016. https://doi.org/10.I177/1558944716660555jv. [ Links ]
40. London DA, Stepan JG, Calfee RP Determining the Michigan hand outcomes questionnaire minimal clinically important difference by means of three methods. Plast Reconstr Surg. 2014;I33(3):6I6-625. https://doi.org/10.1097/PRS.0000000000000034 . [ Links ]
41. de Klerk S, Coetzee Z. The inter-rater reliability of the Smith hand function test: A South African perspective. Hand Ther. 2015;20(3):88-94. https://doi.org/10.1177/1758998315589653. [ Links ]
 Correspondence:
Correspondence:
Amy Buttle Naudé
amy.buttle@westerncape.gov.za














