Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Occupational Therapy
versión On-line ISSN 2310-3833
versión impresa ISSN 0038-2337
S. Afr. j. occup. ther. vol.47 no.3 Pretoria dic. 2017
http://dx.doi.org/10.17159/2310-3833/2017/v47n3a9
COMMENTARY
The Analytical Survey Method: A valuable tool for efficient and effective Occupational Therapy service provision for a patient/client population
van der Reyden DI; Wilson SII; White BIII
INatDip OT (Pretoria), Dip Ed Voc (Pretoria), BA (UNISA), LLM Med Law ( Natal)- Senior lecturer ( Hon) University of KwaZulu Natal
IIMSc, DipCOT UK- Manager Mental Health in-patient Occupational Therapy and Physiotherapy services for adult and older adults, Northamptonshire Healthcare NHS Foundation Trust, UK, Director, Vona du Toit Model of Creative Ability Foundation (UK) Community Interest Company
IIIBsc OT (Hons) UK- Clinical Lead, Occupational Therapy, Berrywood Hospital, Northamptonshire NHS Foundation Trust, UK. Director, Vona du Toit Model of Creative Ability Foundation (UK) Community Interest Company
ABSTRACT
This paper describes the effective integration and application of a hybrid analytical survey method in order to obtain a substantive profile and resource information about a patient/client population. Integrating the Vona du Toit Model of Creative Ability, the survey is used as a primary tool for planning intervention, evaluation and planning in occupational therapy practice. The process has been used extensively in action research in practices throughout South Africa and the United Kingdom and results have shown that it allows for a more targeted and efficient provision of intervention and treatment. This paper briefly describes the development of the Analytical Survey Method and details how the procedure is implemented using the example of its application in a UK mental healthcare facility. Its contemporary relevance is highlighted in the context of healthcare challenges and the need to demonstrate efficient and effective occupational therapy provision.
Key words: Occupational Therapy; analytical survey; analytical survey method: OT service planning and evaluation; Vona du Toit Model of Creative Ability; action research: service efficiency
INTRODUCTION
Occupational therapists from all practice areas and settings must evaluate whether the methods they are using are appropriate, effective and efficient for their particular patient population. This regular and ongoing evaluation is integral to providing an efficient and effective service. It is necessary for service growth, support, funding and practitioner job satisfaction and motivation, this being even more so in situations of decreasing resource allocation for services coupled with increasing expectations on service outcomes. The Analytical Survey Method (ASM)1 incorporating the Vona du Toit Model of Creative Ability (VdTMoCA)2,3,4 is a tried-and-tested, purpose-designed, user-friendly means of addressing this need. It enables practitioners to undertake systematic investigation; to record, analyse and evaluate clinical information within their own setting and to address service needs effectively and efficiently.
This method has at its core the description and compilation of data on an entire population which may comprise for example, all patients attending a specialised mental health care unit; all persons in a residential care facility for the independent aged, or even all the children in a particular class/grade/level attending an educational facility. The subsequent planning and/or evaluation of interventions is based upon the population profiles generated. The Analytical Survey Method is not an individual patient/client assessment tool, it does not replace traditional assessment and does not require additional assessment by any team member, but rather utilises knowledge and insights team members already have of each patient/client included in the Analytical Survey process.
The ASM, containing both descriptive and analytical survey characteristics1,5, and which is described in this paper was developed by van der Reyden6,7 during the 1980s and 90s and was further refined by her through practise and ongoing review in a facility that provided care and therapeutic programmes for 1,300 persons with mental health disorders8. Since then it has been applied effectively in numerous and varied settings in South Africa and more recently by Wilson and White9,10,11 in the United Kingdom. It therefor helps to answer the question "is what we are providing as a service, meeting the needs of the population that we serve?" The ASM has been found to be an effective means of answering this question in keeping with the guidelines provided by the World Federation of Occupational Therapists (WFOT)12 and the World Health Organisation (WHO)13.
This ASM can be used when reviewing a population to determine needs, recognise strengths, weaknesses and barriers and to plan appropriate intervention. This can be for a small caseload such as a ward, a broader group of clients such as all adult wards or a much larger population i.e. an entire healthcare facility, school or even community facility. The ASM furthermore indicates how effective an established intervention programme is and will highlight areas for improvement and guidelines for the nature of intervention required. Alternatively an occupational therapist acting in an advisory capacity is able to use the ASM to gain quick and robust data about the population and service to inform decision making and action planning.
The survey is tailor-made to suit each population surveyed; the attitude, clinical expertise, skill and knowledge of the practitioners within each setting being crucial to the outcomes of the process. What makes the use of this ASM unique and so effective in directing changes to service provision is the integration of the tenets of the VdTMoCA2,3,4 alongside individual biographical and performance data, coupled with the demographics and contextual analysis of the particular population.
This method does not replace traditional individual and small group assessment and treatment planning; it does however provide a powerful data base allowing for an often new and enlightening perspective on the defined patient population as a whole. A well-documented example9,10,11 of the effective implementation of the ASM is used to illustrate and elucidate the process in the form of vignettes interspersed throughout the text of this paper. These describe a government-funded (National Health Service) adult acute in-patient mental health occupational therapy service in Northamptonshire Healthcare NHS Foundation Trust (NHFT) in the United Kingdom, which faced various service challenges requiring review of current practices. The ASM was implemented fully at this service with evident success.
The ASM process as illustrated in Figure 1 below, comprises of 5 Steps.
LITERATURE REVIEW
The financial pressures on healthcare providers and the need to prove efficient allocation of occupational therapy resources are pertinent to all therapists, regardless of their location or area of practice. All services and departments must consider ways in which to review service provision against the backdrop of available resources, population needs and best practice. Heasman and Morley13 identified challenges to occupational therapists to improve productivity, enhance quality and deliver services that are cost efficient while working with limited resources and still prioritising best use of occupational therapy.
A WFOT12 document providing guidance on developing and managing occupational therapy services emphasised the need to determine the population served and identification of needs in order to deliver appropriate interventions. Other factors must also be considered such as the personnel required, accessibility and design of interventions, materials and resources required, underpinning processes and systems as well as leadership and overall governance and financial issues. The WFOT document suggested that surveys could be used to identify population needs and gaps in provision as part of the review and design process. A systematic process is required to consider the multitude of variables impacting on a particular intervention to ensure effective and efficient service provision.
The WHO14, literature identifies the gap between healthcare services provided to patients and recommended practice, detailing the growing interest in clinical audit in assisting healthcare professionals to assess and adjust their services based on data from their routine practice. The intention of an audit is to enhance professional performance, thereby improving the quality of healthcare and patient outcomes. The ASM comfortably meets both the WFOT and WHO criteria and is therefore of contemporary relevance to occupational therapists in practice today.
Principles for best practice in clinical audit 200215 identifies a five-step process in the audit cycle: Preparing for audit (defining the purpose, providing a structure, making time and collaboration with staff); selecting criteria (deciding what to measure, using guidelines); measuring performance (planning data collection, identifying and sampling the population, data sources and data analysis); making improvements (such as changing behaviours, identifying barriers and establishing the right environment); and sustaining improvement (monitoring and evaluating changes).
It is clear that a systematic process is required to consider the multitude of variables that impacts on a particular intervention in order to ensure that services provided are effective and efficient. The ASM enables practitioners to meet this requirement. The ASM considers characteristics of the patient population and the numerous variables that impact on interventions. The survey process is closely aligned to the five-step process in the audit cycle and clearly facilitates therapist evaluation and service delivery improvement in a similarly systematic manner. The design of the ASM referred to in this paper does not fit any theory perfectly, as may happen with surveys, but is best described as an ongoing unstructured observational survey. It conforms to the general objective of the use of both analytical and descriptive surveys1,5, namely: to provide sufficient descriptive information in order to make inferences about the characteristics or features of a particular population1. The design-based approach is further evident as it was used as the basis of and applied to circumscribed samples, in other words, populations of patients within particular service areas (in this case users of mental health care services). It is described as an analytical survey due to the manner in which it is applied in practice but also aligns itself to an extended clinical audit process.
As the ASM was developed through action research16,17. During this development, continual systematic recording and clinical application in a variety of settings ensured that the criteria for practitioner action research were further met. To clarify, the development of the ASM was essentially evolutionary and was an attempt to address questions such as how an occupational therapist working alone with support staff or assistants could provide an effective and efficient service to large numbers of clients, in excess of 1000 at any one time; how to practically obtain relevant valid data sufficient to plan and implement interventions; and how to ensure continued service provision6,7. According to van der Reyden11 action and plans were not research driven but rather evidence of ongoing reflective practice as is the case in action research. The end result was an encompassing programme for the entire population which provided therapeutic services at institutional, unit, disorder/disability and specific functional performance (creative ability) levels representing various components and layers of care provision as described by van der Reyden7.
Publications on the use of ASM are limited, however presentations have been delivered at several congresses/workshops and many clinicians have been given hands-on assistance by van der Reyden, and more recently also by Sherwood, Wilson and White to develop and implement the ASM in their clinical areas. The integration of the VdTMoCA within the ASM compilation, the data analysis and subsequent planning and implementation lies at the core of the particular efficacy of this method and merits a brief review.
The VdTMoCA is a practice model based on theory developed in South Africa in the late 1960's - early 1970's from work undertaken by Vona Du Toit2,3,4 , an occupational therapist.
The VdTMoCA, which has human motivation as its core tenant describes directedness, strength and manifestation of motivation within a developmental framework of nine sequential and interrelated levels of creative ability. These levels manifest on a continuum through different life cycles. The primary construct on which the theory is based is that motivation governs action (doing) and that action can be observed as the manifestation or expression of motivation. Intrinsic human motivation is believed to drive the development of skills or behaviour as environmental, social, relationship or occupational demands change and influence a person throughout life. In the event of illness, trauma, and injury or in response to changing life demands, the model maintains that a person's performance may stagnate or regress to a lower level of creative ability; conversely, a person may also show progression and/or recovery in level of creative ability. The VdTMoCA details the levels of creative ability according to defined descriptors, with each level encompassing the abilities developed in the previous level and containing the fundamentals for progression to the next level. The levels of creative ability as described may be applied to normal developmental stages as well as levels of recovery, impairment and deterioration of performance4.
Within mental health in-patient services it has been found, through survey data and clinical observation, that there is a predominance of individuals whose overall functioning corresponds to the first five levels of creative ability (Table 1). The performance of thealigns itself to an extended clinical audit process.
majority of individuals using mental health care services have been found to correspond to self-presentation and passive participation. It is important to keep in mind that the creative ability levels describe performance on a continuum, from mere biological existence (Tone) to competitive contribution at a society/community and that levels may change. A person may also show characteristics of more than one level at a particular time.
Table 1 on page... contains very brief descriptors for "Motivation" and 'Action" for each of the levels of creative ability as relevant to mental health care, and as adapted from the summary chart of levels of creative ability provided by de Witt4.
The value of the VdTMoCA lies not only in its provision of descriptors of the creative ability levels, but also in the detailed guidelines for the determination of goals, principles for application and intervention planning (programmes) for persons or groups of persons functioning at each level.
THE ANALYTICAL SURVEY METHOD PROCESS
This paper describes a five-step process for the ASM with examples of its practical application. The process is straightforward and often, to those participating, enlightening. The vignettes included within the text contextualises the application of the ASM and provides an insightful practitioner narrative as occupational therapists at NHFT reflect on the ASM at various stages of its implementation. Permission for the use of the NHFT information was obtained by Wilson and White. The service vignettes are from an adult acute in-patient mental health service that consisted of two hospitals each with four wards for patients between the ages of 18 and 65 - one mixed gender admission ward (up to 12 beds), one male recovery ward (up to 17 beds), one female recovery ward (up to 17 beds) and one psychiatric intensive care ward (up to 7 beds). The occupational therapy services in each of these hospitals at that time predominantly provided a group programme in a centrally located department with a kitchen, craft / art room, garden, gymnasium and group rooms.
The five steps within the analytical survey method consist of preparation, completion and administering, data analysis, action planning and evaluation. The implementation which usually follows on the action planning is logical and strongly recommended but not discussed as a step of the ASM.
Step 1: Preparation
The decision to undertake the ASM is best taken at a departmental, facility and service level whereas the rationale for this decision is preferably determined through team collaboration; the purpose must be specific and clear to all participants from the outset; this will impact on not only the "buy in" but also the type and extent of data required within the survey itself. The identification of a working group or task team will facilitate the process. The drivers behind undertaking the ASM may vary within each organisation and can range from a simple desire to check that what is being provided is still appropriate to the patients, to a more specific service delivery evaluation for the purpose of redesigning service provision to meet cost efficiency targets (see Vignette 1).
Vignette 1: As part of a service evaluation and improvement project, the occupational therapy services embarked on a process of reviewing and redesigning the intervention and treatment provided. The rationale for service change was multi-faceted and was based on ongoing challenges due to the changing nature of mental health care: length of stay was becoming shorter, illnesses appeared more acute and generally more complex, and patients were discharged much sooner after slight improvements in performance were seen. Defining and implementing a structured occupational therapy pathway which was realistic to the pace and challenges of the setting and met the needs of the patients was necessary. Staff were working exceptionally hard yet feeling that they were not achieving their potential outcomes, negatively impacting on staff satisfaction and role confidence.
In addition the service needed to demonstrate improving healthcare outcomes and efficiency in line with government drivers such as 'Equity and Excellence: Liberating the NHS,19 but wanted effectiveness to be demonstrable by more than just the amount of treatment groups provided or number of attendees.
To ensure success of the process, parameters must first be defined. The population must be circumscribed and may comprise an entire hospital facility, a specific ward or wards, one or more outpatient clinics or individual therapist caseloads. From clinical experience no population has yet been identified which could not be surveyed. Service managers and key stakeholders must be involved at the outset to support the proposed process identify potential limitations or barriers, areas requiring service changes or resources needed. These may vary from issues such as negative institutional cultures impacting on service delivery; the need to improve or adapt the environment to support better patient outcomes; or the need to review the skill mix of staff. Barriers such as time, commitment and resources are carefully considered in advance so that staff time is ring-fenced not only to complete the survey, but more importantly to implement the ensuing action plans. Without this, the process will be limited to an information gathering exercise without impacting intervention and thus not ensuring the desired outcomes for the population of service users.
As many occupational therapists and other team members with responsibility for the patient population must be involved in completing the survey, it is essential that they know their population well and are able to chart information about the functioning of the population members. It is advisable and appropriate to involve multidisciplinary team members to enhance the perspective of assessment of functioning.
All staff involved need to be informed of the entire process, taught how to use the survey tool and ideally will have a working knowledge of the VdTMoCA to improve consistency and reliability of data and to facilitate the planning process. The lead person for the survey process must be named and identified; s/he should ensure that ethical approval has been obtained, should this be required, and that data and findings are handled in line with relevant information governance and service provider data collection guidelines (see Vignette 2).
Vignette 2: Within our service development project the VdTMoCA was identified as a new model of choice to begin to address some of the issues faced, a decision made based on the strength of its developmental nature; level descriptors enabling practitioners to identify small functional improvement through levels and phases; its interrelatedness between motivation and action; and the structured and detailed treatment guidance provided. Emerging clinical evidence of the efficacy of the VdTMoCA was also a strong motivating factor. Our aim in undertaking the ASM was to identify the overall needs of the population in relation to occupational functioning and levels of creative ability in order to provide us with a robust baseline picture to guide required service changes. The intention was to examine this against the treatment interventions that were currently provided in order to identify strengths and limitations and guide service transformation and delivery changes underpinned by the use of the VdTMoCA. We obtained approval from NHFT's clinical audit and effectiveness committee to carry out this work as a service evaluation.
Facilitation of the survey process is most effectively undertaken by an individual experienced in using the ASM and is skilled in the analysis of data and interpretation of findings. The facilitator will require expertise in both the practice area and the VdTMoCA in order to guide the working group and other staff to analyse and interpret findings, identify population needs, relate these to current best professional practice and formulate plans for optimal intervention and service (see Vignette 3).
Vignette 3: The staff in NHFT were introduced to the ASM and thereafter supported and guided in the development and analysis components in the survey process by the developer of the method. Her knowledge and experience of the VdTMoCA helped to ensure that the interrogation of the information about our population's needs against current occupational therapy provision and desired implementation of the VdTMoCA was well guided. We have since completed the analytical survey process on an annual basis without her input, but initially her involvement was crucial in our understanding of the steps within the process and how to objectively view, analyse and interpret the data we had collected.
Step 2: Compilation and administering the ASM
2.1. Compilation of the survey schedule
The schedule is compiled in a table format with each column representing an item for input, starting with the name and other identifiers of the users of the service such as their admission number. A schedule usually includes a minimum of 60 and often up to 75 items, depending on the population surveyed. The survey schedule typically includes items that reflect demographic and biographical data, needs, strengths/abilities, lifestyle, functional performance, skills, level of creative ability, programme or activity participation of the individual, environmental factors and resources. The rows are used to record the data for each individual.
The specific items are printed in cells created by the columns and the 2 top rows. The top row indicates the broader category of items such as biographical data and the next row specifies aspects of that category, for example the category 'self-care' may include items such as 'hygiene', 'dressing', 'nail care', 'continence' and so on. Each item indicator is usually abbreviated to fit space limitations, hence a need for a list of descriptors and an explanation of what each means. Each item may again have one or more aspects, for example, 'Hygiene' may include aspects such as 'bathing', 'care of teeth' and 'uses AD (assistive device)'. The detail included per item is determined by contextual knowledge of the population and the information required.
The other rows are used to record the individual patient/client information as per item. Of particular significance to occupational therapists is the detailing of occupational performance and creative ability in addition to the environmental factors that may impact on occupational functioning and programme design/implementation.
The survey is population specific, for example, a survey schedule prepared for an elderly population suffering from dementia together with physical frailty will differ significantly from that for a group of children with special educational needs; similar categories may be represented but actual detail of items / aspects will differ. The format is thus consistent but with the content changing to fit the population and survey need. The information to be gathered should be easily accessible, preferably from the prior knowledge of the staff.
The content is tabulated with rating scales and appropriate scoring / coding systems applied different items or clusters of items to facilitate analysis. As the survey may deal with populations exceeding 250 individuals, these scales need to be easily accessible and user-friendly. Scales may vary from using an ordinal scale for items used to determine severity of need for example a 5-point scale (wherel indicates 'Independent' to 5 which indicates 'Needs supervision and assistance from others'). For other items a simple Likert scale or a binary scale may suffice, whereas other items may need a code such as for diagnosis, or even a descriptive word.
Items for recording as well as rating scales used, must ultimately accurately and clearly reflect the profile characteristics of the population and provide substantive indicators for intervention and/ or environmental change i.e. highlight those items which need to be addressed in programme analysis or planning.
The instructions for the compilation of the survey and the rating scales including the VdTMoCA level descriptors are best compiled as a separate document and used by staff as reference during the process. However, should space on the survey form allow, this information may also be indicated on the survey form for quick reference, as in Table II below. The VdTMoCA level determined by matching the person's performance with a concise VdTMoCA level descriptor and indicating this under the specific item. These concise level descriptors are best provided on a separate schedule. The level is however further confirmed through correlation with other items on the schedule for example performance at level of Self Differentiation will be further confirmed by scoring in items such as self-care, social skills and participation in programmes.
Table II is an excerpt from an ASM schedule and illustrates the table format used. There will be additional items required to those illustrated which will be determined by the staff in the particular service area. In cases where an existing programme needs to be evaluated, items for recording participation in different activities and events on offer will also be required. This is best represented in a table with columns showing the different activities/events/interventions offered by occupational therapy and other disciplines. The rows are again used to record patient or client information. This enables cross-checking of items of information such as VdTMoCA level, diagnoses and participation.
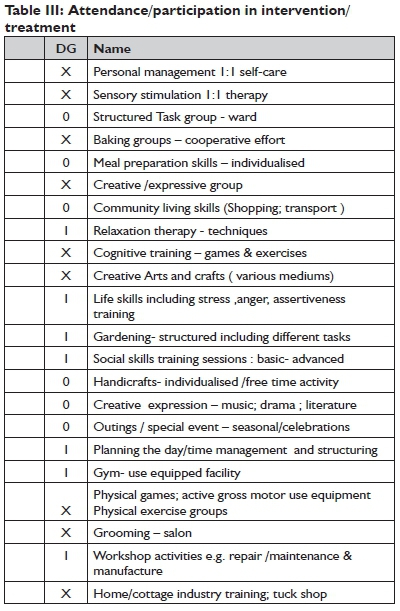
Table III contains examples from a survey schedule used, listing some interventions offered; the list is not all inclusive and should preferably also reflect services other than occupational therapy. Interventions included must be situation specific. Activities/sessions recorded on the schedule should include that which is offered whether in individual, selected small group or general group activities/sessions and reflected as such. A scale (ratio measurement) to capture attendance and/or participation in intervention/treatment as offered in each setting is needed which is then correlated with the basic population survey findings. This correlation indicates the appropriateness of the current programme for identified population needs and as such is a very powerful evaluation and planning tool. Attempting to effectively record attendance participation is complex as individual needs, contextual factors and day to day issues may impact, these include for example physical access, availability, resources, disorder and disability as well as performance levels, which all need to be factored into the analysis and findings. The rating scale must be simple to use but also effective in identifying efficacy of the programme mix. By way of example a hypothetical 6-day programme consisting of 20 sessions (individual/group) is used to illustrate an effective 4-point scale where: "O" represents Optimal/adequate attendance/participation of appropriate or prescribed sessions (clinically found to be at 70% plus, which would translate into 15 or more out of 20 possible sessions per week). "I" = Inadequate attendance or participation (Inconsistency, frequent absences 25-50% which, translates into 5 -10 sessions per week), "NA" = Non-attendance, which may include an occasional 'pop in' (0- 20% which means 1-2 sessions per week) and "X" = Inappropriate or not prescribed for the individual.
A 70%+ attendance rating was determined through clinical discussion and validated by experience of the authors during several surveys conducted as the "optimal, realistic and consistent level of attendance" in a particular case. This percentage makes allowance for ad hoc factors which may decrease attendance, such as investigations required, illness or family commitments.
2.2. Administering the ASM
The actual survey component of the ASM is conducted by a 'survey team' (i.e. the staff allocated to lead the project and which may include representatives from all units involved,), according to a prearranged plan and time table. It is worth repeating that the survey is completed without the presence of the patients/clients.
Staff and caregivers to whom the patients/clients are well known have been found to provide the most valuable inputs; it is thus recommended that such persons be involved in providing the data on the individuals being surveyed.
It is preferable to survey a complete ward, unit or population in one 'sitting', or at least on consecutive days to increase interrater reliability. As a general guide, the process takes approximately seven minutes per patient/client once al involved are familiar with the procedure. It is well worth spending extra time initially with the 'survey team' to ensure that those administering the survey have a clear understanding of the process, terminology, descriptors and the coding used in the survey as well as the prompts used to illicit the required information, the rating scale criteria and the recording procedure to ensures consistency of implementation and evaluation and thus reliability. The process is thereafter undertaken methodically and with minimal deliberation, to facilitate the swift charting of information. For the sake of expediency all the required information should be at hand. Practically, it has been found to work most efficiently when the staff involved sit around a table, each with a hard copy of the printed schedule as well as the guidelines for recording and rating scales. Patient/client files/lists should be at hand. Staff then systematically contribute information on each patient/client from their own perspective. One person needs to be responsible for the 'official' recording of the decision on each item on what becomes the 'master' survey schedule used for analysis.
Collecting all information on one or two days may not be feasible or desirable in all settings and the survey process can then be adapted accordingly. An on-going, 'rolling survey', where each new client is recorded soon after admission, may be completed over a 3-month period.
Step 3: Analysis
The compilation of findings happens in two phases: The primary (initial) phase, consists purely of the analysis of the data as recorded on the survey schedule for each individual, as part of the population, whilst the second phase comprises a contextual review of the findings through interdisciplinary discussion and in-depth consideration of all issues/aspects requiring intervention.
The primary phase during which the baseline population profile is obtained, is undertaken once all information is charted for each patient/client with all items and aspects requiring intervention and major areas or needs identified. This is done by calculating the frequencies of incidence of need and correlating data for different items. This is usually most efficiently executed by a small group of no more than three persons to ensure the consistency and thus reliability of interpretation.
During this phase, as a rule, only the items with a frequency of need above 40% are considered as priority areas to interrogate further with a view to action planning for the population. This percentage, determined through practical clinical experience using the survey, has been found effective in ensuring that the primary needs of the population are addressed. Problems/needs which are reported for less than 40% of the population are addressed on a small group or individual basis as appropriate. For example if 29 out of 40 persons were identified as being unemployed, this would identify it as a area for intervention for 72.5% of that population, indicating an apparent need for the implementation of a prevoca-tional/work skills training programme. On the other hand, if 6 out of the 40 persons had mobility challenges, this would be shown as a problem for only 15% of that population and would be addressed on an individual patient/client basis.
As a further example, should the survey indicate the incidence of patients functioning at a creative ability level of Self-differentiation this would immediately indicate a need for inclusion of sensory stimulation, concept formation and basic self-care training inputs.
The primary phase also gives an indication of skills/abilities, performance and participation.
Implicit in this primary phase of analysis and provisional planning is the application of collective clinical knowledge and experience.
The second phase of analysis consists of presenting the provisional findings to a wider group of practitioners/managers, indicating limitations, strengths and needs of the population as identified in phase one, along with proposals for action plans relevant to the population surveyed. This phase provides an opportunity to ensure accuracy of information, consideration of contextual factors and the correlation of findings as reflected for different items, each area of need identified being thoroughly interrogated by the team. This phase thus provides for the generation of ideas, and enhances the quality of planning to achieve a common goal or vision leading to Step 4, namely Action Plan Formulation which addresses the compilation of practical action plans for each goal. This phase may be undertaken primarily as an informative planning exercise, as described above and/or may be used to evaluate the current offerings in view of the ASM findings use all this available information to inform change.
The population profile frequencies are thus, as mentioned above, often further correlated and scrutinised in conjunction with information about the existing intervention /treatment and uptake by patients/clients. This is a critical step which must be undertaken with much care as it may at once be the most exciting and at times alarming step as the reality of the extent to which the actual needs of the population are being addressed and any disjunction become unequivocally apparent. Staff must be open to the possibility of revelations which may highlight limitations in the current services provided; whilst offering clear indications for addressing issues identified. It is furthermore an affirming and encouraging step as areas of good practice are confirmed by the data. This phase has been found to lead to an increase in staff motivation as staff are intimately involved in the process and the formulation of the end results based on solid facts, statistics and principles for best practice.
Vignette 4: The results of the analytical survey in NHFT confirmed the need and desire for service change and assisted in clarifying the areas that the occupational therapy staff were struggling with. Although the data showed us a great deal, we prioritised as a team the most important findings upon which we constructed action plans:
With the very acutely ill patients at Tone and Self-differentiation level of creative ability, the survey clearly identified that occupational therapists were unintentionally neglecting nearly one fifth of the population because of the severity of their illness, deeming them too unwell for occupational therapy. This figure provided a powerful message and provoked questioning by the staff who realised that in an acute mental health facility, with severity of illness ever increasing, it was unacceptable to maintain the viewpoint that individuals were too unwell for treatment until such time as they stabilised. The data highlighted the issue that treatment needed to be provided from day one of admission and the VdTMoCA provided the understanding and framework of how to begin treatment with those who were the most unwell.
The survey frequencies highlighted that attendance of occupational therapy groups was poor for patients functioning at the Self-presentation level of creative ability, which made up over half of the population. The majority of group interventions were targeted and had participation from patients functioning at Passive participation and above of creative ability, who made up just over a quarter of the population. The analytical survey data clearly highlighted this imbalance, as well as providing valuable data about overall group attendance and the types of groups that were popular or well attended. Application of clinical knowledge and experience also allowed staff to further evaluate the therapeutic value of treatment sessions offered while taking into account the impact that symptomatology such as avolition and fatigue may have on participation.
The survey identified that two-thirds of the patient population had poor self-care. This was enlightening as individual therapists were aware of this regarding certain individuals within their own caseloads, but seeing the data for the population as a whole clearly demonstrated that this was a functional area of need to prioritise as a service, which had not been done up to that point.
Having identified that over three quarters of the population was unemployed, the programme was considered and it was acknowledged by the team that interventions did not specifically address prevocational or vocational skills. Again this served to confirm the need to change the underpinning model of practice to the VdTMoCA which had a more skill-building focus to its treatment interventions, in order to work on pathways for development of prevocational skills at all levels of functioning.
Thus, the findings from the initial analytical survey clearly provided a structured starting point for the priority areas to address in terms of applying the VdTMoCA to a targeted treatment programme for our adult acute in-patient mental health service.
Step 4: Action Plan Formulation
Those involved in each setting need to take ownership of the findings of the survey, acknowledging what it shows them about their population and where the strengths and weaknesses of their current programmes appear to lie, and should strive to combine ideas in order to formulate relevant action plans. Without commitment to further planning and implementation, the survey process entails a little more than a mere data-gathering exercise. Action plans should be informed by:
whether the data indicates the need for additions, eliminations or a change of focus of interventions,
whether additional resources will be required to meet the identified needs or need to be reallocated;
whether staff need to work in alternative ways;
whether procedures such as assessment processes, timetabling, timing of interventions, ward routines and so on require adjustment;
whether the current spread and skill mix of staffing is appropriate to meet the identified needs;
whether staff may require additional training as a result of identified needs that have not been addressed before; and lastly,
what the realities of the setting may bring to the process in terms of barriers or challenges such as staff motivation, politics of the workplace, staff confidence, senior management support, resistance to change and so on.
Key stakeholders must be informed and as far as possible involved in planning to ensure that the reason for change and anticipated positive outcomes are understood and supported. Robustly collected data which has been presented well is difficult to contest and serves as an indication of innovative forward-thinking and a commitment to ensuring cost effectiveness and treatment based on patient need rather than "custom and practice".
Within the action plan review dates and targets are required to keep the process on track and ensure that all individuals involved are aware of their role in the delivery of the plan. The timeframes will vary depending on the amount and depth of change indicated. Some changes will be "quick wins" and can be achieved in relatively short timeframes, while others will take more time and effort.
The crucial component for efficient and effective implementation is the establishment of a management structure with an identified leader or leaders, realistic timeframes and other resource allocation. This cannot be overemphasised. Systems and procedures need to be put in place to keep the programme on track, to monitor progress and when necessary, to revitalise programmes.
Vignette 5: Once the important items for attention were identified, these were used to form the basis of our action plan for change. One action was to address the needs for patients at Tone and Self-differentiation levels of creative ability, developing an appropriate treatment pathway based on sensory approaches and targeted intervention for personal management and self-care activities. As this was not in place currently, we identified the need to up-skill staff in delivering sensory based treatments through external courses and in-house development sessions. Resources to support the delivery of sensory and self-care treatments were identified and a bid submitted to management with supporting information from the analytical survey to elicit additional funding to purchase items. Staff were allocated duties to compile a resource file with session outlines for different self-care tasks such as dental hygiene, hair care and shaving. The clinical lead occupational therapist was tasked with discussing alterations to the ward morning routines to allow occupational therapy staff to work with identified patients on self-care activities. The workload of occupational therapy support staff was reviewed in order to free up two daily slots to carry out regular sensory and physical based individual work with identified patients at Tone and Self-differentiation levels of creative ability across all of the wards.
Progress towards each identified action point on the action plan was reviewed within the weekly occupational therapy development meetings and wider procedural elements were discussed in the regular multidisciplinary and strategic forums to ensure sustain-ability of service changes.
The day to day practical implementation of the new/revised/ expanded programmes is not described as a distinct/defined step of the ASM, it is however implicit in the effective execution of the ASM that the action plans will be implemented and follow-up done, The actual extent and time frames according to which this is done however, rests entirely with the facility/unit management and staff. Action plans may for example be delayed; implemented gradually over time or otherwise be implemented in their totality as from a certain date - or anything else in between. The implementation is seen as an in-house stage although the procedures and processes would have had to be effectively planned and organised as part of the action planning.
Looking at the 5 step ASM process the reader would have noticed that the implementation is not discussed as part of the ASM, although this would seem logical and is recommended. It is however entirely up to the facility/setting and the staff involved as to how the process will proceed. The most effective outcomes for both staff and clients occur when plans are directly implemented; planning without action may indeed be found to be futile, but this cannot be prescribed.
Step 5: Evaluation
This step describes a process which is essentially an accelerated repetition of steps l, 2 and 3, coupled with a comparative analysis of findings from the initial analysis and the findings of a follow-up survey. For services wishing to quantify the impact of change, a follow-up analytical survey will provide comparison data to the baseline data collected, thus providing a tool for evaluation as well as planning.
A minimal time for a follow-up ASM application is 12 months, although 6 months has been found to be effective and due to the shorter time frame adds a sense of urgency. To allow for effective comparison and evaluation the follow-up survey must be completed using the same format and procedure.
Comparison of baseline and follow-up data alongside staff and patient/client/carer questionnaires, which may be compiled to assess satisfaction and change, will provide a robust and clear picture of the impact of the changes made. Findings of follow-up surveys should, as was done initially, be shared with all stakeholders. The follow-up survey provides documented evidence of progress in attaining goals set as well as an indication of areas needing further attention, modification or revitalisation. This step allows for review of staff efforts and achievements and the efficacy of the ASM as tool. Should Action Plans not have been implemented this step may still be used to determine whether a change of need has occurred.
Vignette 6: A second analytical survey was conducted in NHFT, nine months after full implementation of the VdTMoCA (see Table IV). This enabled staff to chart the progress they had made so far, demonstrating a clear improvement in service provision and outcomes and supporting on-going use of the VdTMoCA as an underpinning model of practice. Having this evaluative data was highly empowering and furthered staff's motivation to continue with their process of service delivery changes.
Table IV on page 61 clearly illustrates the substantive difference which the correctly managed implementation and follow up of the ASM brought about. This is only a small sample of the changes which occurred and were extracted for illustrative purposes.
Staff dedication and sound management of the entire process with strict attention to monitoring and follow-up is essential for achieving the remarkable improvements made at the facility which has provided the data to illustrate the ASM.
The reader may well ask what then?
The simple answer is that the ASM may be used as a once-off or the process may continue as part of the ongoing cycle of evaluation, planning and implementation, with the focus changing as the need arises at different times.
CONCLUSION
This paper has explained the rationale behind the implementation and development of a situation-specific analytical survey, the ASM, as a mechanism and model for improved service provision in any setting and with any size of population. The paper used an actual mental health service user population of an identified mental health care facility within the UK to illustrate the process. The five-step process has been outlined with examples of application to enhance the readers' understanding and to demonstrate its applicability in practice.
With current healthcare and financial demands becoming more intense the ASM has been highlighted as being of contemporary value, despite being developed 30 years ago. It remains a powerful tool in enabling practitioners to evaluate and develop their services, thereby ensuring cost-efficient and therapeutically effective treatment outcomes for the patients/clients they serve. The VdTMoCA has been identified as crucial to the ASM in ensuring that service delivery has a robust occupational performance foundation with clear pathways for patients functioning at all levels of ability.
The implementation of the ASM has proved to be effective in many and varied settings, with varied and numerous benefits which include:
Benefits to a facility such as greater efficiency of resources, the direct impact on resource allocation enables the identification of specific areas of need and thus resource requirements.
Benefits to service provision including focussed, appropriate services to the entire population
Benefits to the staff are evidenced in a greater sense of accomplishment; confidence in own contribution and the ability to justify clinical decisions effectively; it also helps staff to effectively apply the VdTMoCA across diagnostic, age and cultural groupings.
Benefits to patient/client include effective therapeutic input which is focussed on the real needs existing within a entire setting thus leading to better outcomes in terms of not only the individual patient/client performance level increases and higher discharge but overall patient/client satisfaction with the input they are receiving.
It may also be used when planning for expansion or refocus of services.
With current healthcare and financial demands becoming more intense the ASM has been highlighted as being of contemporary value, despite being developed 30 years ago. It remains a powerful tool in enabling practitioners to evaluate and develop their services, thereby ensuring cost-efficient and therapeutically effective treatment outcomes for the patients they serve.
The VdTMoCA has been identified as crucial to the ASM in ensuring that service delivery has a robust occupational performance foundation with clear pathways for patients functioning at all levels of ability.
Limitations to the process are that it is dependent on practitioner knowledge and understanding of the VdTMoCA and is initially
more effective if facilitated by an expert in the process.
Occupational therapists in care settings are urged to consider its application within their own area of work. It is recommended that practitioners develop the use of the ASM to support their work as an individual as well as within a wider service context. Newly qualified practitioners or students on placements could effectively use the process to understand their small / initial caseloads and provide structure to ensure their work is targeted, while teams and larger services could use the process on a regular basis to ensure they adapt and change their service provision in order to remain efficient and effective over time.
The authors may be contacted for further information and ASM tool sharing.
REFERENCES
1. Caldwell JG. Sample Survey Design for Evaluation (The Design of Analytical Surveys), 20 March 2009, updated 16 June 2010 posted at http://www.foundationwebsite.org/SampleSurveyDesignForEvaluation.pdf ( January 2015). [ Links ]
2. Du Toit HJV An Investigation into the Correlation between patient Volition and its expression in Action. SAJOT. 1974; 4(2): 6-17. In: Patient Volition and Action in Occupational Therapy. Vona & Marie du Toit Foundation; Pretoria, 2009. [ Links ]
3. Du Toit HJV The implementation of a programme aimed at evaluating the current level of Creative Ability in an individual and stimulating the growth of his Creative Ability which would lead to Work Capacity. In: Patient Volition and Action in Occupational Therapy. Vona & Marie du Toit Foundation; Pretoria, 2009. [ Links ]
4. de Witt P Creative Ability: A Model for Individual and Group Occupational Therapy for Clients with Psychosocial Dysfunction. In: Crouch R, Alers V editors. Occupational Therapy in Psychiatry and Mental Health (5th edition). London: Wiley Blackwell; 2014: 3-5, 9-31. [ Links ]
5. Shadish W R ,Cook T D, Campbell D T, Experimental and Quasi-experimental Designs for Generalized Causal Inference. Houghton Mifflin; 2002. [ Links ]
6. van der Reyden D. The Smith Mitchell System for the Rehabilitation of Long Term Psychiatric Patients. SAJOT. 1984; 14(1): 37- 47. [ Links ]
7. van der Reyden D. Planning an Occupational Therapy Programme for Large numbers of institutionalised Patients. In Crouch RB & Alers VM, editors. Occupational Therapy in Mental Health and Psychiatry (3rd edition). Durban: Maskew Miller Longman; 1997: 95-124. [ Links ]
8. van der Reyden D. The value, development, application of an analytical survey in conjunction with the VdTMoCA to evaluate, develop/or enhance OT services. Paper presented at Creative Ability conference, II June 2011. Hosted by University of Pretoria, University of Witwatersrand and OTASA. South Africa. [ Links ]
9. Wilson S, White B. Transforming Lives and Sustaining Change using the Vona du Toit Model of Creative Ability. Paper presented at Creative Ability Conference, II June 2011. Hosted by University of Pretoria, University of Witwatersrand and OTASA. South Africa. [ Links ]
10. Wilson S, White B. The Journey to Service Redesign. Occupational Therapy News. UK, 2011; August: 36-37. [ Links ]
11 Wilson S, White B. Understanding the needs of service users. Occupational Therapy News. UK: Royal College of Occupational Therapy; 2012 April: 24-25. [ Links ]
12. World Federation of Occupational Therapists. Developing and Managing an Occupational Therapy Service. 2008. <http://www.wfot.org/ResourceCentre.aspx>. (23 June 2014) [ Links ]
13. Heasman D, Morley M. Introducing prioritisation protocols to promote efficient and effective allocation of mental health occupational therapy resources. British Journal of Occupational Therapy. 2012; 75(11): 522-526. [ Links ]
14. Flottorp SA, Jamtveld G, Gibis B, McKee M. Using audit and feedback to health professionals to improve the quality and safety of health care. European Office: WHO ; 2010. http://www.euro.who.int/_data/assets/pdf_file/0003/I244I9/e94296.pdf. [ Links ]
15. National Institute for Clinical Excellence. Principles for best practice in clinical audit, 2002. <http://www.nice.org.uk/usingguidance/implementationtools/clinicalaudit.jsp?domedia=I&mid=79613703-19B9-E0B5-D4FI4A0429022FC0> (23 June 2014) [ Links ]
16. McNiff J. Action Research for Professional Development (3rd edition). London: Routledge; 2002. [ Links ]
17. McNiff J. Action Research - Principles and practice, (3rd Edition ). London: Routledge; 2013. [ Links ]
18. Casteleijn D and Smit C. The Psychometric properties of the Creative Participation Assessment. SAJOT. 2002; 32(1): 6-11. [ Links ]
19. Department of Health. Equity and Excellence: Liberating the NHS. London: Her Majesty's Stationery Office; 2010. [ Links ]
 Correspondence:
Correspondence:
Dain van der Reyden
dainic@telkomsa.net
















