Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.46 n.3 Pretoria Dec. 2016
http://dx.doi.org/10.17159/2310-3833/2016/v46n3a5
SCIENTIFIC ARTICLES
Stroke management and functional outcomes of stroke survivors in an urban Western Cape Province setting
Judy CawoodI; Surona VisagieII
IBOT (SU), M Phil (SU). Private practice
IIBSc Physio (SU), MSc and Phd (Health Sciences) (SU). Post-doctoral fellow, Centre for Rehabilitation Studies, University of Stellenbosch
ABSTRACT
INTRODUCTION: Long-term disability caused by stroke can be decreased through comprehensive rehabilitation.
AIM: This article aims to describe the functional outcomes achieved by stroke survivors in an urban Western Cape Province setting to add to the information on stroke management.
METHODS: A descriptive mixed methods study was done. Proportional, stratified random sampling was used to select 53 participants from a population of 267. Quantitative data were collected with the Stroke Impact Scale Version 3.0 and the Modified Barthel Index, and analysed with the Mann-Whitney test. A p value of < 0.05 was deemed statistically significant. Five of the 53 participants were purposively sampled for the qualitative phase of the study. Qualitative data were analysed according to predetermined themes.
RESULTS: Seventy-five per cent of participants were managed in a general medical ward. Four were admitted to a specialised inpatient rehabilitation centre. Eighty-three per cent received physiotherapy, 62% received occupational therapy and 57% received both physio-and occupational therapy. Fifty-one per cent experienced communication difficulties, but only 18% received speech therapy.
CONCLUSION AND RECOMMENDATIONS: Sufficient inpatient therapy (preferably in a stroke unit /ward) and family education /training should be received before discharge. Occupational therapy, speech therapy, physiotherapy as well as psychological, social work, vision screening and dietetic services should be expanded at both hospital and community level.
Key words: Stroke, rehabilitation, occupational therapy
INTRODUCTION
While stroke often leads to death its true impact has not been realised if the extent of disability (often long term or permanent) is not taken into account1. Stroke is ranked 9th in terms of major causes of disability in South Africa2. A lack of basic medical and diagnostic services as well as a lack of access to therapy and rehabilitation in middle and low-income settings such as can be found in South Africa, impact negatively on stroke outcomes. These factors can lead to higher than expected mortality and disability rates amongst stroke survivors1,3,4.
This article presents findings from a mixed method descriptive study. The aim of the article is to add to the body of knowledge on stroke management by describing the functional outcomes achieved by stroke survivors in an urban Western Province setting.
LITERATURE REVIEW
According to "The South African guideline for the management of ischemic stroke and transient ischemic attack" by Bryer and colleagues5 (2011), acute stroke care should be provided by a co-ordinated multidisciplinarya team of trained professionals who have a special interest in stroke care, in a designated space, with beds reserved for stroke care. Comprehensive assessments, skilled nursing care, early mobilisation, initiation of strategies to prevent secondary complications, early discharge planning and an early start to rehabilitation, are recommended5. These guidelines are not achieved in South Africa: Management of persons with stroke is more common in general medical wards instead of dedicated stroke care wards and stroke survivors are not always referred to therapy6,7,8.
Stroke can cause multiple impairments which might necessitate a variety of rehabilitation interventions. Therefore it is often necessary for stroke rehabilitation to be provided by service providers from different professions working together, preferably as an interdisciplinary team5,9. Rehabilitation plays a vital role in lessening the effects of impairments and activity limitations and in facilitating the return to active participation in community life and economic self-sufficiency after stroke2,10,11. A longitudinal, observational study showed a clinically and statistically significant (p<0.0l) improvement (mean Barthel Index score improved with 23% from 58.85 to 8l.59) in functional outcomes of stroke survivors who received inpatient rehabilitation at the Western Cape Rehabilitation Centre (WCRC). The WCRC is a specialised, dedicated rehabilitation facility in the Western Cape province of SA11. The functional status of 67 stroke survivors, of whom 63 received occupational therapy, was measured directly after admission and within two days prior to discharge. No information on the nature of the occupational therapy intervention or general rehabilitation was provided by the authors; neither was the impact of any of the therapies on function directly assessed.
Unfortunately South African stroke survivors are not always referred for in- or outpatient rehabilitation. None of the 30 consecutively sampled stroke survivors who participated in a longitudinal descriptive study performed in rural KwaZulu-Natal in 2007 were referred for rehabilitation after discharge7. What little support they got came from community-based workers trained to manage HIV, a visit from a physiotherapist (30%) and consulting social workers (7%). They showed some functional improvement at follow-up assessment three months post discharge, with an average increase of 9% on the Barthel Index, but their ability to do housework and participate in cultural and social activities were severely impaired. In contrast, many of the 196 stroke survivors consecutively sampled between 2004 and 2006 in a district hospital in the Western Cape Metro health district, to participate in a longitudinal, observational study, were referred for in- or outpatient rehabilitation3. Those who were immobile and dependent for activities of daily living, but with the potential to recover functionally were referred for inpatient rehabilitation, those who were mobile were referred for outpatient rehabilitation and those who were dependent prior to the stroke were referred for home based care. Those referred to outpatient rehabilitation received approximately 30 minutes individual therapy per week or fortnight. (This excluded speech therapy that was unavailable.)
A 2009 study found that 97% of their participants received physiotherapy, 35% occupational therapy and 8% speech therapy in the first 6 months post-stroke, at community health care centres (CHCs) in the Western Cape Metro12. To some extent these findings reflect the availability of service providers. All CHCs in the Western Cape Metro health district provided physiotherapy services, 50% had an occupational therapist, and only 1% had a speech therapist12. The majority of participants had between one and five therapy sessions.
One South African study, an observational cohort study, statistically analysed the impact of physiotherapy provided at a CHC on the functional outcomes of stroke survivors (n=25)13. No information on the location of the study is provided. The authors reported that an hour of physiotherapy (exercises included rolling with momentum, bridging, trunk rotation, joint approximation exercises in sitting and standing, ball therapy for shoulder and trunk, hand activities and gait re-education) every fourteen days did not have a clinically (the average mean BI score improved with 5%) or statistically significant impact on the function of participants. The article does not provide any information on whether participants received input from other team members such as an occupational therapist.
METHODS
A descriptive mixed methods study with a sequential exploratory strategy as described by Kroll et al14 was done. Qualitative measures (phenomenology) were used secondary to cross sectional, descriptive quantitative methods, to contextualise and explore the quantitative findings, and to highlight individual perceptions and experiences. The study population included people living in a section of the eastern, sub-district of the Western Cape Metropole Health District, who had strokes in 2009 and 2010, and who had accessed public health services. Participants were at least six months post stroke at the time of data collection since the first six months post stroke is considered to be the period of fastest recovery15. People younger than 18 and those who received health care and rehabilitation through private health care services were excluded. The study population was identified from the records of a public hospital, CHCs and various non-governmental organisations (NGO). With the assistance of administrative staff at these institutions, 326 potential participants were identified of whom 59 were excluded since they resided outside the study area. This left 267 potential participants of whom 53 were selected to participate in the study through proportional, stratified random sampling. The primary author in consultation with a statistician decided that approximately 50 participants would allow completion of the study within a reasonable timeframe (extensive data were collected from each participant) while ensuring a large enough sample to allow statistical analysis of quantitative data. Strata were formed according to the geographical areas in which people lived to ensure that participants from all communities in the study setting were represented. The names of stroke survivors were placed alphabetically in each stratum and numbered. Random numbers generated by computer were drawn by a statistician for inclusion.
Data were collected by the primary author between March and August 2011. Depending on their choice, data were collected either at participants' homes or at a central venue. Transport was provided where required. Data collection tools included a data coding form; the Stroke Impact Scale (SIS) Version 3.016, and the Modified Barthel Index (MBI)17.
The 58-item SIS was selected since it is completed by the stoke survivor and provides information from their perspective on eight domains i.e. strength, hand function, mobility, activities of daily living, emotion, memory, communication and social participation, through a five point Likert scale. A score between 0 and 100 can be achieved16. Duncan et al18 showed that all SIS domains (Cronbach coefficients ranged from 0.83 to 0.90) bar emotion (Cronbach co-efficient 0.57) have excellent reliability. Validity scores ranged between 0.82-0.84 for mobility and activities of daily living and 0.44-0.58 for memory and communication when comparing the SIS to other tools. Participation domain scores correlated moderately with the Short Form Health Survey (SF-36)18. According to Carod-Artel et al "...the...SIS 3.0 is a psychometrically robust specific health related quality of life measure that may be useful to evaluate the consequences of stroke in different cultural contexts."19:2483.
MBI scoring was done through observation of the activities and according to the guidelines provided by the Australian Government Department of Health20. For certain domains (bladder and bowel) or where it was not possible to observe the activity, self-reporting was done by the index person (stroke survivor) or the proxy caregiver. The MBI assesses 10 domains i.e. personal hygiene, bathing, feeding, toilet, stair climbing, dressing, bowel and bladder control, ambulation, wheelchair mobility and transfers20 and is often used in studies with stroke survivors21. Items are scored numerically to a maximum of 100. Scores of 0-24 denote total dependency, 25-49 severe dependency, 50-74 moderate dependency and 75-90 little dependency20. Internal consistency and validity of the MBI is well established as excellent22.
Although the primary author, who collected all data, speaks a limited amount of IsiXhosa and has a reasonably good understanding of the language, a translator was used with IsiXhosa-speaking participants to ensure questions were clearly understood and answers were interpreted correctly. Quantitative data were entered onto a spreadsheet and statistically analysed with STATA. Data were analysed to provide descriptive statistics (range, means and standard deviations) and statistical significance was determined using the Mann-Whitney test. A p value of <0.05 was deemed statistically significant.
A heterogeneous group of five participants (two women and three men) was purposively sampled for the qualitative phase of the study. This was based on the perception of the primary author that they would be able to provide rich, nuanced information which could enhance understanding of the quantitative figures. Their ages ranged from 44 - 69 years. They had varying functional ability, from needing assistance with all activities to being totally independent. One was employed. Three of the participants had their spouses present who acted as proxy respondents. These three participants were encouraged to participate in any way they could. (E.g. A participant with aphasia was asked to raise her hand if she did not agree with what her husband said.) Data were collected through semi-structured interviews guided by an interview schedule that focused on the following aspects:
• Causes and prevention of stroke.
• How they managed at home.
• Role and importance of therapy and rehabilitation.
• Access to therapy and rehabilitation.
• Sufficiency of therapy and rehabilitation.
Qualitative data were analysed through content analysis by the primary author according to predetermined themes based on the study objectives. The themes were:
• Participants understanding of the causes and prevention of stroke (not dealt with in this paper).
• Environmental barriers experienced by partici-pants23.
• Therapy and rehabilitation received by participants.
• Participants perception of therapy and rehabilitation.
• Barriers to accessing therapy and rehabilitation.
On reading the transcripts, narratives that addressed specific themes were coded. These were then ordered under the themes.
Participation in the study was voluntary and participants signed informed consent forms in order to participate. They were assured that all personal or identifying information would be kept confidential. Approval for this study was obtained from the Committee for Human Research at Stellenbosch University (Ethics clearance number: N10/11/375). Permission to acquire the names and contact details of people who had strokes in 2009 and 2010 was obtained from the Western Cape Department of Health, the relevant points of service delivery and NGOs.To minimise selection bias, the primary author accessed various sources in order to identify as many uninsured people who had strokes in 2009 and 2010 as possible. In addition, stratified random sampling was used, to ensure inclusion from participants of all communities since services and access might differ in the different communities. The SIS and MBI are reliable valid instruments as discussed earlier. The purpose of the qualitative data was to provide possible explanations and further explore quantitative findings. Thus the traditional practices to ensure rigour, such as data saturation and member checking were not done. Triangulation of the different methods showed that qualitative findings confirm quantitative findings and thus enhanced the credibility of the findings.
RESULTS
Demographic profile
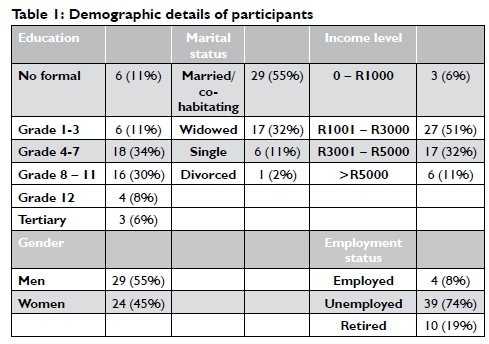
The ages of the 53 participants ranged from 29-years to 94-years old. The mean age of participants was 62.56 (SD 12.08). Educational levels were generally low, with 45% of participants having a primary school education and 11% having no formal education. Poverty was common with 57% of households surviving on less than R3 000 per month. Table 1 provide further demographic information of study participants.
Hospitalisation during the acute phase
Initially the majority of participants (40; 75%) were managed in a general medical ward at the district hospital in the study setting, while six (11%) were managed as outpatients at CHCs, 4 (8%) accessed a tertiary hospital, two (4%) did not seek immediate medical intervention and one (2%) was first managed at a private hospital and then transferred to a government hospital. As indicated in Figure 1, 42% of participants were hospitalised for more than 14 days while 19% were not admitted to a hospital after the stroke.

Functional scores
The mean SIS score was 48.3/100 (sd 29.4). Scores ranged between 0 and 98. Mobility scores (as determined by the ability to balance in sitting and standing, move from bed to chair, walk indoors, walk/ propel one block, climb one and more flights of stairs and get in and out of a car) ranged from 0 to 100 with a mean of 51.5 (sd=28.6). The mean score for the Modified Barthel Index was 70.58 out of a possible 100 (Range 0 - 100). Figure 2 (on page 24) shows that more than 70% of participants were independent or only needed a little assistance with feeding, toileting, bladder and bowel control, walking and transfers. The two domains that created challenges for the largest number of patients were 'wheelchair mobility' and 'stair climbing'.

Therapy and Rehabilitation
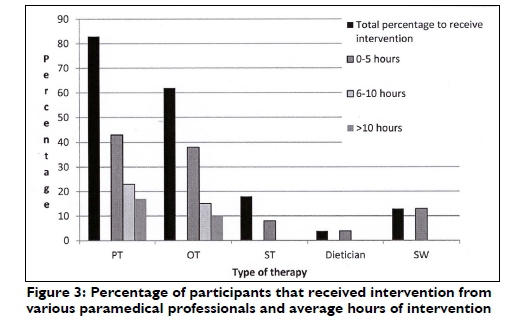
Physiotherapy was the most common therapy intervention with 83% of participants receiving physiotherapy as in- and/or outpatients. This was followed by occupational therapy, received by 62% of participants as in- and/or outpatients. Fifty seven percent of participants received both physiotherapy and occupational therapy. Seven (13%) participants reported that they received a home visit from an occupational therapist or physiotherapist. While SIS scores indicated that 51% of participants had some form of speech and communication difficulty post stroke, only 18% received speech therapy. The importance of speech therapy and the lack thereof in the study setting was highlighted by qualitative findings:
Speech therapy is very important. It is one of the first things that must be attended to after a stroke so that the patient can communi-cate...It is very difficult to get an appointment with the speech therapist at the hospital. One of the most difficult things at the State Hospital: perhaps you will get an appointment and that will be in about three months' time. I can't see how one appointment in three months can help. (Husband of 45-year-old female participant)
Input from social workers and dieticians were also limited (Figure 3). None of the participants received any intervention from a psychologist. With regard to hours of input none of those who did receive speech therapy, social work and dietary intervention received more than five hours' intervention. Fewer than 20% of participants received more than 10 hours physiotherapy and occupational therapy respectively (Figure 3).
The average BI and SIS mobility scores of the participants who received occupational therapy at CHCs were higher than those who did not receive OT. BI average scores of those who did not receive OT were 62 versus 84 for those who did receive OT. SIS mobility average scores of those who did not receive OT were 44 versus 63 for those who did receive OT. The difference was statistically significant (BI; p = <0.01, SIS mobility; p = 0.02). Those who received physiotherapy at CHCs did not show statistically significant higher functional scores as measured by the BI (p = 0.04). However, clinically, participants who received physiotherapy had higher average BI scores than those who did not (74 versus 67). Those who received physiotherapy also did not have a statistically (p = 0.78) or clinically higher mobility score as determined by the average SIS scores (50 versus 52.5). Those who received both physio-and occupational therapy at CHCs had an average BI score of 82 versus a mean score of 76 for those who did not receive both these therapy interventions. BI scores for the group who received both therapies ranged from 32 - 100 and for those who did not receive both interventions scores ranged from 0 - 100.
Lack of access to ophthalmology and/or optometry services further created challenges for many participants. Vision impairments were common and included hemianopia (8%), double vision (6%), diabetic retinopathy (11%), cataracts (19%) and progressively poorer vision with age (66%). This was recorded as presbiopia, but would need to be confirmed by an ophthalmologist as it is possible that these vision impairments could be related to cataracts, diabetic retinopathy or other visual impairments. Participants struggled to access vision services and at the time of the study had to travel approximately 35 - 50 kilometres (depending on where they were living) for vision testing and obtaining spectacles through government services.
Comprehensive inpatient rehabilitation
According to participants, ten (19%) of them were referred for comprehensive rehabilitation at an inpatient rehabilitation centre about 40km from the district hospital. Of these, four were admitted. Reasons for non-admission given to participants included:
• The stroke not being serious enough: They told us it is only for people with more serious strokes -people that can do nothing for themselves. (Wife of 54-year-old participant.)
• That the centre was only admitting younger people with the potential to return to work.
• The centre was at capacity and there were no beds available.
Transport challenges also made it difficult for participants to access the facility.
According to a doctor at the rehabilitation centre, the centre admits patients from all over the Western Cape Province and is often at capacity. The centre does have admissions guidelines and preference is given to clients who require input from three or more disciplines, have the potential to return to work, require comprehensive rehabilitation, and/or do not have access to alternative rehabilitation services.
Reasons for not receiving therapy
Where therapy services were available, 55% of participants reported lack of referral or knowledge of the service as the reason for not receiving therapy:
If this happens for the first time - you are in the dark. You are somewhere where you have not been before. Now what is the next step? Is there someone that can help? You hear how someone says you must go and see that person. Guidelines - not just on paper, but that are practical - if you go from A to B that person will help you and tell you what the next step is. (Husband of 45year-old female participant)
Transport created further barriers: 25% of participants did not receive therapy or only attended a few sessions because of the cost of transport while 23% said they had no transport. Thirteen percent of participants specifically reported on the lack of transport for wheelchair users.
Other reasons included:
• Caregiver strain.
• No one to accompany the person.
• The stroke survivor was too weak to go out or was not feeling well.
• Difficulty transferring and pushing overweight people to CHCs in a wheelchair.
• Other responsibilities like caring for grandchildren.
• Dissatisfaction with therapy. Reasons included therapist not keeping appointments and therapy being painful.
DISCUSSION
Current study participants were admitted to general wards of various hospitals and not managed in specialised units that provide organised stroke care by teams of suitably trained service providers, the gold standard for acute stroke management2,5,24. While mean and median length of stay could not be determined from the data (answer options did not reflect precise numbers of days), it seems from Figure 1 as if length of stay might be in line with findings from two studies in the Western Cape Province, published in 2013 and 2011 respectively: mean inpatient length of stay of 10.4 days in a tertiary hospital8 and median length of stay of 8 days in a district hospita12 with a six bed stroke unit. A 2009 study in rural KwaZulu-Natal7 found an average inpatient length of stay of 6 days.
A short length of stay allows very little time for modification of the impairments, learning of compensatory strategies and training and education of family members and carers. In addition, difficulty getting off work, transport challenges, the condition of the stroke survivor and the initial shock experienced by family can combine to provide little opportunity for effective education and training. Family members must be actively involved in education and training, which should be provided on more than one occasion25. In some instances current study participants/caregivers didn't think physiotherapy/occupational therapy was necessary. The reasons for this are unclear. It might be that they did not understand the benefits, or that caregivers were so overwhelmed with day-to-day responsibilities that they were disinclined to make the effort to access existing rehabilitation services.
The information provided earlier on the lack of services at community level, and the finding that very few participants were actually admitted to the provincial rehabilitation centre, highlights two critical needs: for stroke survivors to receive as much inpatient therapy as possible during their stay in the acute hospita124, if possible in an acute stroke unit5,25, and for family to receive sufficient education and training before discharge occurs25,26. Kalra and col-leagues26 found in a randomised control trail with 300 participants in the United Kingdom that caregiver training results in improved quality of life and a lessening of anxiety and depression after stroke for stroke survivors as well as a decrease in cost of care, caregiver burden and anxiety and depression amongst caregivers.
Creating a seamless network of stroke care in the study setting would further support improved outcomes as according to Walker et a125 optimal recovery after stroke requires specialist hospital care in the acute phase and coordinated rehabilitation for many months after discharge. Acute care can be supported through the establishment of a stroke ward as described by De Villiers27 in a different secondary hospital in the same health district. According to the authors this was done with no extra staff and at no extra cost. Service delivery in this ward was based on the stroke management guidelines5 and has shown improved outcomes in terms of decreased mortality and more referrals for inpatient rehabilitation27. Further exploration is needed to determine the way community stroke care should be organised in terms of type of provider, optimal length and intensity of interventions as it is unclear25. Community stroke care in South Africa is often provided through therapists employed at CHCs. Current findings showed that these services seemed to be clinically beneficial. Established NGOs can play a positive role in the provision of support. In a phenomenological study with 12 stroke survivors, conducted by Reed et a128 in England, it was found that support groups provide stroke survivors with exercise, peer interaction, a social support network and information.
The cross sectional nature of the current study means that cause and effect cannot be proven and many variables might have influenced the findings. This may explain why those who received occupational therapy had significantly higher BI and mobility scores versus those who did not, and those receiving just physiotherapy or physiotherapy and occupational therapy presented with differing results. Previous studies as summarised in a meta-analysis indicated that physiotherapy had a significant positive effect on ambulation, arm and hand activities, ADL and physical fitness29. Similarly two systematic reviews21,30, indicated that occupational therapy impacted the outcomes of stroke survivors positively.
The limited number of therapy sessions that participants in the current study received is of concern particularly as Veerbeek et a129 concluded from a meta-analysis of studies on the impact of physical therapy post stroke, that "there is strong evidence that a higher dose of practice is better"29:e87987. The South African study by Puckree et al13 confirms that a physiotherapy session once a fortnight did not lead to significant improvment.
Studies confirm a lack of speech therapy services at CHCs3,12. At the time of the current study the only speech therapy available for stroke survivors in the study setting was through group sessions offered by a NGO in the area. Although valuable, many stroke survivors were excluded from this service due to transport problems. The high demand has also caused the group to grow to the extent that it is not always possible to meet the individual needs of those who attend.
The importance of counselling stroke survivors and caregiv-ers on adapting to their changed circumstances and roles are generally recognised2. Depression is a fairly common occurrence after a stroke, which has a negative impact on rehabilitation and can ultimately lead to poor outcomes2. Social workers are often employed at CHCs in the Western Cape metro12. They can play an important role in counselling, providing a link between family and health care team and assessing the home circumstances and financial situation of stroke survivors. With their knowledge of the person's socio-economic circumstances they are also ideally placed to advise the team on which patients need priority admission to inpatient rehabilitation facilities or should stay longer in hospital.
As visual impairments were common and vision problems greatly compound the difficulties faced by stroke survivors, the lack of services for visual screening is something that needs to be investigated further. Early identification and treatment of certain conditions can prevent blindness31. Various visual aids can promote involvement in activities and promote participation in life situations.
The study is not without limitations. It is generally accepted that the larger the sample, the greater the validity of a study and 53 participants may be considered a relatively small sample, especially since no power calculation to determine sample size was done. Due to the nature of the response options in the demographic data collection tool mean and median length of stay could not be determined. The amount and type of therapy or intervention received (physiotherapy, occupational therapy and speech therapy) and assistance from psychologists, dieticians and social workers were mostly obtained from information provided by participants and caregivers. Where uncertainty or discrepancies were apparent the researcher did verify information with the relevant facility or therapist with the permission of the participant. These limitations must be kept in mind when considering the conclusion and recommendations.
CONCLUSION AND RECOMMENDATIONS
The many challenges faced with regard to stroke care in South Africa - management of stroke survivors in a general medical ward, no dedicated beds, no or limited treatment protocols, lack of funding and human resources, early discharge due to pressure on bed numbers, too few neurological rehabilitation centres with demand exceeding supply, and limited therapy at community leve15 - were all evident in the current study.
The feasibility of forming a stroke unit/ward at district hospitals according to guidelines provided by De Villiers et a127 should be investigated through further study. In the interim it is recommended that stroke survivors spend longer time as inpatients and receive stroke care in accordance with the guidelines published in 20115. Carers need to be involved actively with rehabilitation and receive training from physiotherapists and occupational therapists to assist from an early stage with mobility, transfers, and activities of daily living. A specific team member needs to be given the responsibility of contacting family members and ensuring that caregivers do come to the hospital to receive the necessary guidance and training. In particular, a concerted effort needs to be made to ensure that stroke survivors requiring comprehensive rehabilitation are referred and admitted to a rehabilitation centre.
Occupational therapy services in this and similar settings should be strengthened, expanded, and made accessible to more clients. This then would imply motivating for an increase in numbers of occupational therapists, as the study done at community health centres in the Western Cape Metro revealed that not all facilities that provided services to stroke survivors had an occupational therapist on staff12.
Considering the devastating effect that speech and language disorders have on stroke survivors and caregivers it is imperative that speech therapy is available to stroke survivors. In view of the difficulties experienced with transport it would seem particularly important that these and other rehabilitation services be available at CHCs and clinics within various communities.
The prevalence, prevention and treatment of vision problems amongst uninsured populations in South Africa should be investigated in future studies.
ACKNOWLEDGEMENT
The authors want to thank Professor Martin Kidd from the Centre for Statistical Consultation at Stellenbosch University for assistance with sampling and data analysis.
REFERENCES
1. Norrving B, Kissela B. The global burden of stroke and need for a continuum of care. Neurology, 2013; 80(3 Supplement 2): S5-S12. [ Links ]
2. Bryer A, Connor M, Haug P Cheyip B, Staub H, Tipping B, Duim W, Pinkney-Atkinson V South African guideline for management of ischaemic stroke and transient ischaemic attack 2010: A guideline from the South African Stroke Society (SASS) and the SASS Writing Committee. South African Medical Journal, 2010; 100(11): 747-778. [ Links ]
3. De Villiers L, Badri M, Ferreira M, Bryer A. Stroke Outcomes in a socio-economically disadvantaged urban community. South African Medical Journal, 2011; 101(5): 345-348. [ Links ]
4. Thorogood M, Connor MD, Lewando-Hundt G, Tollman S, Ngoma B. Secondary prevention of stroke: results from the Southern Africa Stroke Prevention Initiative (SASPI) study. Bulletin of the World Health Organization, 2004; 82: 503-508. [ Links ]
5. Bryer A, Connor MD, Haug P Cheyip B, Staub H, Tipping B, Duim W, Pinkney-Atkinson V. The South African guideline for the management of ischemic stroke and transient ischemic attack: recommendations for a resource-constrained health care setting. International Journal of Stroke, 2011; 6 (August): 349-354. [ Links ]
6. Norrefalk J. How do we define multidisciplinary rehabilitation? Rehabil Med, 2003; 35: 100-101. [ Links ]
7. Wasserman S, de Villiers L, Bryer A. Community-based care of stroke patients in a rural African setting. South African Medical Journal, 2009; 99(8): 579-583. [ Links ]
8. Parekh I, Rhoda A. Functional outcomes of stroke patients admitted to a tertiary hospital in the Western Cape, South Africa. South African Journal of Physiotherapy, 2013; 69(2): 10-14. [ Links ]
9. World Health Organization (WHO). World Report on Disability. Geneva: World Health Organization, 2011. [ Links ]
10. Young J, Forster A. Review of Stroke Rehabilitation. British Medical Journal, 2007; 334: 86-90. [ Links ]
11. Joseph C, Rhoda A. Activity limitations and factors influencing functional outcome of patients with stroke following rehabilitation at a specialised facility in the Western Cape. African Health Sciences, 2013; 13(3): 646-654. [ Links ]
12. Rhoda A, Mpofu R, DeWeerdt W. The rehabilitation of stroke patients at community health centres in the Western Cape. South African Journal of Physiotherapy, 2009; 65(3): 3-8. [ Links ]
13. Puckree T, Uthum P Effectiveness of a community based programme of physiotherapy on stability, balance and function of stroke patients. South African Journal of Physiotherapy, 2013; 70(1): 3-7. [ Links ]
14. Kroll T, Neri MT, Miller K. Using mixed methods in rehabilitation research. Rehabilitation Nursing, 2005; 30(3): 106-112. [ Links ]
15. Kwakkel G, Kollen B, Twisk J. Impact of time on improvement of outcome after stroke. Stroke, 2006; 37(9): 2348-2353. [ Links ]
16. Duncan PW, Bode RK, Min Lai S, Perera S. Rasch analysis of a new stroke-specific outcome scale: the Stroke Impact Scale. Archives of Physical Medicine and Rehabilitation, 2003; 84(7): 950-963. [ Links ]
17. Shah S, Vanclay F Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. Journal of Clinical Epidemiology, 1989; 42(8): 703-709. [ Links ]
18. Duncan PW, Wallace D, Lai SM, Johnson D, Embretson S, Laster LJ. The Stroke Impact Scale Version 2.0 Evaluation of Reliability, Validity, and Sensitivity to Change. Stroke, 1999; 30: 2131-2140. [ Links ]
19. Carod-Artal FJ, Coral LF Trizotto DS, Moreira CM. The Stroke Impact Scale 3.0. Evaluation of Acceptability, Reliability, and Validity of the Brazilian Version. Stroke, 2008; 39: 2477-2484. [ Links ]
20. Australian Government Department of Health. The claim and advance payment cycle-information for the Transition Care Program, Modified Barthel Index. 2006. [ Links ] [Online]. Available: www.health.gov.au/internet/main/publishing.nsf. [Accessed 2011, July 24].
21. Steultjens EMJ, Dekker J, Bouter LM, Van de Nes JCM, Cup EHC, Van den Ende CHM. Occupational Therapy for Stroke Patients: A Systematic Review. Stroke, 2003; 34: 676-687 [ Links ]
22. Wade D. Measurement in Neurological Rehabilitation. Oxford: Oxford University Press, 1996. [ Links ]
23. Cawood J, Visagie S. Environmental factors influencing participation of stroke survivors in a Western Cape setting. African Journal of Disability, 2015; 4(1): Art. #198, 9 pages. http://dx.doi.org/10.4102/ajod.v4il.198. [ Links ]
24. Chen L, McClaran J, Buchan AM. Impact of acute stroke unit on hospital length of stay. Archives of Gerontology and Geriatrics, 2009; 49 e12-e15. [ Links ]
25. Walker MF Sunnerhagen KS, Rebecca J. Fisher RJ. Evidence-Based Community Stroke Rehabilitation. Stroke, 2013; 44: 293-297. [ Links ]
26. Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M, Donaldson N. Training carers of stroke patients: Randomised controlled trial. BMJ, 2004; 328 (May): epub. [ Links ]
27. De Villiers L, Kalula SZ, Burch VC. Does multidisciplinary stroke care improve outcome in a secondary-level hospital in South Africa? International Journal of Stroke, 2009; 4(2): 89-93. [ Links ]
28. Reed M, Harrington R Duggan A, Wood VA. (2010). Meeting stroke survivors' perceived needs: A qualitative study of a community-based exercise and education scheme. Clinical Rehabilitation, 2010; 24: 16-25. [ Links ]
29. Veerbeek JM, Van Wegen E, Van Peppen R Van der Wees PJ, Hendriks E, Rietberg M, Kwakkel G. What Is the Evidence for Physical Therapy Poststroke? A Systematic Review and Meta-Analysis. Plos One, 2014; 9(2): e87987. [ Links ]
30. Legg L, Drummond A Leonardi-Bee J, Gladman JRF Corr S, Donkervoort M, Edmans J, Gilbertson L, Jongbloed L, Pip Logan P Sackley C, Walker M, Langhorne P Occupational therapy for patients with problems in personal activities of daily living after stroke: Systematic review of randomised trials. BMJ, 2007; 335: epub. [ Links ]
31. National Eye Institute. Facts about Diabetic Retinopathy. [ Links ] [Online]. Available: www.nei.nih.gov/health/diabetic/retinopathy.asp#2a. [Accessed 2011, September 12].
 Correspondence:
Correspondence:
Judy Cawood
judycawood@gmail.com
a The three teamwork approaches referred to in this article are defined here to ensure clarity.
Multidisciplinary teamwork "refers to activities that involve the efforts of individuals from a number of disciplines. These efforts are disciplinary-orientated and, although they may impinge upon clients or activities dealt with by other disciplines, they approach them primarily through each discipline relating to its own activities".
Interdisciplinary teamwork requires of "individuals...the skills of their own disciplines [and] the added responsibility of the group effort on behalf of the activity or client involved. This effort requires the skills necessary for effective group interaction and the knowledge of how to transfer integrated groups activities into a result, which is greater than the simple sum of the activities of each individual discipline. The group activity of an interdisciplinary team is synergistic, producing more than each individually and separately could accomplish".
In Transdisciplinary teamwork "one member of the team acts as a primary therapist, with the other members feeding information and advice with regard to management through a single primary person... all borders are broken between the individual professionals".














