Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Occupational Therapy
On-line version ISSN 2310-3833
Print version ISSN 0038-2337
S. Afr. j. occup. ther. vol.43 n.3 Pretoria Mar. 2013
ARTICLES
The rehabilitation programme and functional outcomes of persons with lower limb amputations at a primary level rehabilitation centre
Jerome P FrederiksI; Surona VisagieII
IBSc occupational therapy (UWO), MSc Rehabilitation (US). Junior Lecturer, University of Stellenbosch
IIBSc Physiotherapy (US), MSc rehabilitation (US). Extra-ordinary senior lecture, Stellenbosch University
ABSTRACT
The study aimed at evaluating the rehabilitation programme offered to clients who had undergone a lower limb amputation at an outpatient rehabilitation centre and to determine the functional outcomes of the clients who participated in the programme. Amputations have a severe physical, psychological and socio- economic impact. Effective rehabilitation can assist the individual in dealing with these. A quantitative, descriptive design was implemented in the study. Thirty clients with lower limb amputations who received rehabilitation and the two therapists working at the centre participated in the study. A questionnaire based on the International Classification of Function, Disability and Health, folder audit form and interviews were used for data collection.
No programme vision, mission or objectives for the programme could be identified. Rehabilitation focussed on impairment. The impact of prosthetic rehabilitation on outdoor activities requiring mobility was statistically significant, with p values ranging from 0.00069 to 0.037.'Lack of indoor mobility training' significantly decreased participants ability to lift and carry objects (p 0.011), stand up (p = 0.042), get around inside the house (p = 0.00023), pick up objects from the floor (p = 0.00068), get up from the floor (p = 0.0072), get out of the house (p = 0.0016) and move around in the yard (0.0013). The 'Failure to address community mobility" had a statistically significant negative impact on all aspects of community mobility scores except transfers and driving.
Recommendations include that a service vision and objectives be developed. In addition services should be evaluated and monitored on an ongoing basis and mentorship provided to therapists.
Key words: Lower limb amputation, rehabilitation, programme evaluation and prosthetic training.
INTRODUCTION
Amputation is sometimes the only option if a limb has been damaged through vascular diseases, diabetes, trauma, tumours, infection or congenital deformities resulting in lost viability of the limb1,2. The amputation of a limb is likely to be accompanied by a profound sense of loss and psychological stress, since it leads to an altered body image, loss of mobility, restrictions in terms of leisure and employment as well as unforeseen expenses and possibly loss of income. From a socio-cultural perspective, people who have had an amputation may experience discrimination, and stereotyping3. Therefore, comprehensive rehabilitation is very important to retrain physical and functional abilities, to assist with psychological and emotional adjustment and to ensure social and community integration3.
Rehabilitation services should be based on the social model of disability and have as their main focus, the equalisation of opportunities and social and economic integration of persons with disabilities4,5. Furthermore, rehabilitation of people with amputations who use government services in the Western Cape of South Africa, is guided by provincial guidelines6. Rehabilitation programmes should be continually monitored and evaluated to ensure that they provide services that comply with National Rehabilitation policy5.
Study setting
The study setting was a primary-level, out-patient physical rehabilitation centre in a peri-urban area of the Western Cape. Historically, rehabilitation services in this area have focussed on individual therapy rendered within the medical model approach. Little attention has been paid to the role of the environment or to the facilitation of social integration. As a result, most disabled people living in the area have been socially excluded and have faced barriers such as inaccessible buildings and unemployment. The centre at which the study was carried out, was opened fourteen years prior to the study with the specific purpose of addressing these challenges. During his speech at the opening of the centre in 2000, Dr Y. Cupido, Director of Health in the Western Cape emphasised that the aim of the centre's programmes was to ensure the inclusion and equalisation of opportunities through the implementation of the social model of rehabilitation. Rehabilitation services at the centre were provided on an outpatient basis by a speech therapist, an occupational therapist and a physiotherapist who worked together as a multidisciplinary team.
Problem statement
It is not clear how successful the centre has been in the implementation of its strategies since no programme monitoring or assessment was done.
Study Aim
This study aims to describe and evaluate the amputee rehabilitation programme at the centre. This has been done to determine if the programme was consistent with the social model of disability and had at its core the social integration and economic self-sufficiency of its clients.
STUDY METHODS
Research design
A descriptive, quantitative study was conducted.
Study population and participants
The study population included two groups. The first group was to have included all persons who underwent rehabilitation, both prosthetic and non prosthetic, at the centre after a major lower-limb amputation [through or proximal to the ankle joint1] during the period 1 September 2000 (the opening date) to 31 December 2010. However, the client study population could not be identified from the centre's records since all records were kept electronically and lost due to computer theft. Thus while all efforts were made to identify the entire population the authors cannot be sure that they did in fact identify all amputees who received rehabilitation at the centre during the study period.
Various avenues were explored to identify participants. These are presented in Table I.
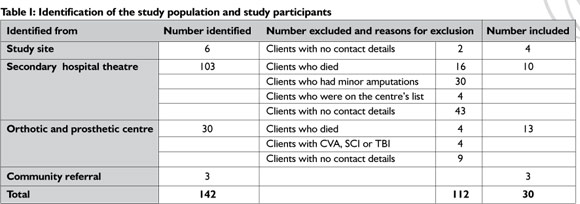
Of the 142 people with a lower limb amputation identified, 112 had to be excluded, either because of the exclusion criteria of the study or because their contact details were not available (see Table I for details). The exclusion criteria of the study were:
♣ Clients who had a minor lower limb amputations [distal to the ankle joint1]
♣ Clients who had died
♣ Clients who had suffered a further amputation or other major trauma to the body, since discharge from the rehabilitation programme, as this may have effected the outcomes
♣ Clients with cerebro-vascular accidents, spinal cord injuries or head injuries, in addition to the amputation, since the additional impairments caused by these conditions will influence the outcome of the amputation rehabilitation programme
♣ Clients who received further amputation rehabilitation at another facility since their discharge from the centre, although the reasons for this were explored.
Thus 30 clients participated in the study in the first group.
The second group of participants consisted of the occupational therapist and physiotherapist who provided amputatee rehabilitation at the centre in July 2010, when data for this study was collected.
Data collection instruments and methods
Data were collected using five tools adapted or developed by the primary author, as indicated:
♣ Structured questionnaire on demographic details, the rehabilitation programme, client satisfaction with the programme, and secondary complications.
This questionnaire was also used to gather data on the nature of the amputation, rehabilitation and the client's satisfaction with the rehabilitation programme. The questionnaire was developed by the primary author after a review of the literature7, and the assistance of a statistician and an expert in the field of amputations.
♣ The International Classification of Function, Disability and Health (ICF)8 based questionnaire on activities, participation and environmental factors.
This questionnaire was developed by combining components of the ICF and checklist8, the WHO Disability Assessment Schedule 119 (DAS 11) and adding some detail from the Locomotor Capabilities Index (LCI)10 as well as the Craig Hospital Inventory of Environmental factors (CHIEF)11.
The questionnaires were combined and a new format developed for various reasons. Firstly, the disability assessment schedule does not include all areas of concern e.g. acknowledging wheelchair use as a form of mobility, toileting, lifting and carrying objects. Secondly, in some instances the ICF did not include some important issues for people with an amputation such as: standing up from sitting, going up and down stairs and walking in poor weather - details which are covered in the LCI. Thirdly, questions on contextual factors from the DAS II such as; 'How much of a problem did you have because of barriers or hindrances?' were removed as they are covered in greater detail in the ICF checklist on contextual factors. Further contextual factors from the CHIEF11 were added. These included; crowds, terrain and availability of information. Some aspects of both the DAS II and the ICF were removed as it was felt that these were not directly related to the impairments experienced by a person with a lower limb amputation. These included; questions on learning and applying knowledge, as well as communication. Finally, the examples were expanded to make them more relevant to the South African context. Areas addressed by this questinnaire included mobility, self care, domestic life, community integration, productive activity and environmental factors (products and technology, natural environment and human made changes to it, support and relationships, attitudes, discrimination and prejudice as well services systems and policies). Scoring was done according to the five point scale used and explained in the ICF checklist8.
♣ Data coding form for relevant programme statistics
This form was also developed by the primary author to gather information such as: the number of clients treated in a year, the average length of treatment periods, the number of sessions per client, the length of sessions, the use of group sessions, the running costs of the centre and other inputs into the programme. This information was used to describe the programme and determine it's efficiency in terms of inputs such as time and money spent compared to the outputs12.
♣ Folder audit form
This form was developed by the primary author to gather data from the folders of persons who received amputee rehabilitation at the centre. The purpose of this was to determine from the records contained in the folders what rehabilitation interventions clients had received in order to gain a further understanding of the programme and to be able to triangulate information from various sources13. The audit form asks specifically about aspects that were identified in the literature3 as important for amputee rehabilitation, such as psychological counselling, education on prevention of complications and self-directed health monitoring, stump care, muscle strengthening, cardio vascular fitness, retraining of activities of daily living, indoor and community mobility, prosthetic fit and alignment, management of environmental barriers, integration to home, sport, recreation and productive activity, evidence of client centred management and interdisciplinary teamwork.
♣ Interview questions for therapists
These questions were developed by the primary author and were used as a guideline during the interviews with the therapists. The purpose of the interview was to obtain an understanding of the programme from their point of view and it included questions on the programme vision, mission objectives; the structure of the programme such as length and frequency of sessions, assessments (initial and follow up) and use of measuring instruments, identification of prosthetic candidates, contents of treatments, education and information given to amputees, provision of assistive devices, environmental barriers experienced by amputees and the role of therapists in addressing these, secondary complications experienced by amputees; community integration of amputees; advantages and limitations of the programme; role of the community in the programme and liaison with other sectors.
Pilot study
The data collection tools were piloted with one therapist and three clients who had received rehabilitation at a Community Health Care Centre in the Western Cape. The pilot study indicated that none of the questions were unclear or redundant and that sufficient data were collected to achieve the aims and objectives of the study.
Data collection
Data were collected in Afrikaans - the language preferred by all 32 participants. The tools developed by the primary author were also developed in Afrikaans. The other tools were translated into Afrikaans by the primary author. The participants were contacted to obtain their provisional consent and to make an appointment with them to collect data at their homes. Data were collected first by using the demographic questionnaire followed by the ICF-based questionnaire.
Six folder audit forms were completed as these were the only folders that could be located. The primary author was unable to find yearly reports, financial records or programme statistics and was therefore unable to complete the checklist on programme inputs.
An appointment was made to interview each of the two therapists employed by the centre on a date suitable to them and data were collected from them using the questionnaire developed for this purpose.
Data analysis
Data were entered onto an Excel spread sheet and analysed by a statistician using Statistica, Version 8. The Spearman rank order correlations and the Mann-Whitney U tests were used, because the data was not normally distributed13. This was to determine any correlation between the rehabilitation provided and client outcomes. A 'p' value of < 0.05 was regarded as statistically significant.
As the data collection tools were either self-designed or developed using a combination of existing tools, their reliability and validity were not tested. This was offset to an extent through triangulation of information from clients, with information from folders and from therapists which went some way towards verifying the validity of findings11.
Ethical concerns
The study was registered with the Committee for Human Research at the University of Stellenbosch. (Reference number NO09/05/147). Permission was obtained from the Western Cape Department of Health to carry out the study and to peruse client records. Written informed consent was obtained from all the participants. Participation in the research was voluntary and it was made clear that refusal to participate would not have any future negative consequences for participants. All information was treated as confidential. The contact details and names of the therapists working at the centre would have been provided to any client in need of intervention.
Results
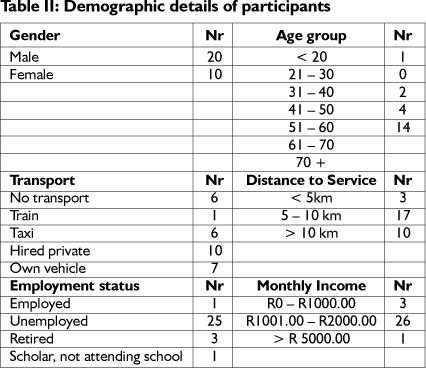
Demographic details of the client participants
The clients' demographic details are presented in Table II. The majority (14) was between 51 and 60 years old. Only one of the participants was employed. The 25 participants who were unemployed cited their amputation as the main reason for their unemployment.
History of the amputation gathered from the client participants
The most common level of amputation was transtibial and the most common cause was Diabetes Mellitus (Table III).
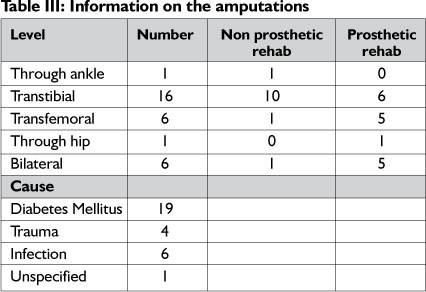
Thirteen clients received prosthetic rehabilitation and 17 received non-prosthetic rehabilitation.
The amputee rehabilitation programme offered at the study site - information gathered from both the client and therapist participants (see Table IV).

The therapists could not provide any information on treatment objectives, vision or mission statements. In addition, annual reports, financial statements and client registers could not be found. According to therapists these had been kept on computer and were lost when the computers were stolen in 2009.
According to client participants they all received individual, outpatient treatment and treatment sessions lasted 30 minutes on average. Client participants indicated the average waiting between referral and the commencement of rehabilitation to be between 15 and 30 days. One participant waited less than 14 days and five waited more than 90 days. Therapists and clients indicated that the distance that clients lived from the centre as well as their financial situation determined how regularly they could access services and thus how often they were treated. Twelve participants received therapy once a week, four received it more often and three less than once a month.
According to the therapists and the folder audit no standardised assessment tools were used during client evaluation. According to the therapists, evaluations at the first visit consisted of observations, an interview to gain information on the personal and medical background of clients, as well as to elicit information about the clients' home and community environment. In addition, a physical examination that included assessing clients gait and their need for assistive devices, such as a wheelchair, balance tests and muscle strength tests were carried out. Progress was determined by constant re-assessing of the clients.
The therapists indicated that they set goals and treatment plans based on assessment findings. The therapists further indicated that they discussed the treatment plan with clients to determine if they met the expectations of the clients. However, twelve clients felt they were not at all involved or only involved to a limited extent in treatment planning. According to the therapists, the content of prosthetic and non-prosthetic programmes was the same except for additional prosthetic training in the prosthetic rehabilitation programme. The focus of prosthetic training was on balance retraining and weight transfer onto the prosthetic leg. According information provided by the therapists, they used the following criteria to determine if a client was a candidate for a prosthesis:
♣ Clients who were young and in the productive phase of their lives
♣ Good physical endurance
♣ The ability to use elbow crutches without difficulty
♣ Good upper and lower extremity muscle strength
♣ Good cardio-respiratory fitness
♣ No neurological comorbidities
Table IV contains the results from both the client and therapist interviews and shows that rehabilitation addressed mostly muscle strengthening, stump range of movement, cardiovascular fitness and indoor mobility. Services relating to psychological counselling, stump maturation, stump desensitisation, problems with transport, community mobility, environmental barriers, home visits and liaison with employers were provided to a limited extent as the numbers in Table IV shows.
Therapists said that clients were discharged once their goals had been reached. Clients did not receive follow up dates after discharge. Therapists felt that although the clients' families were involved in the programme, the broader community was not. According to the therapists no collaboration with local governments, provincial departments such as transport, labour and education, or the private sector had occurred.
All of the following information regarding provision of assistive devices and programme outcomes was gathered from the client participants.
Provision of assistive devices
All of them who had a need for crutches or walking frames received them. The picture for wheelchairs was slightly different, with 18 participants having received one, while eight were still waiting for their wheelchairs. Twenty-one of the participants needed wheelchair cushions. Two participants were waiting for their prostheses. Where participants needed devices which they did not have, they did not know whether the devices had been ordered or not. This information was obtained from client participants and could not be verified from folders due to the unavailability of these and limited information in those that could be found. When the therapists were asked about waiting lists they said that they started a new one in 2010 since all previous data had been on the computer that was stolen. No attempt was made to obtain lost data either from clients or other sources.
Programme outcomes
Client satisfaction with the programme
Data collected from the structured questionnaire on demographic details, the rehabilitation programme, client satisfaction with the programme, and secondary complications, indicated high levels of client satisfaction. Clients expressed gratitude for being able to walk again and being empowered to deal with personal problems and connected these abilities to the rehabilitation they had received. Twenty-eight participants indicated that the services were sufficient. All thirty clients found the staff to be friendly and helpful. Clients felt that they had received personal attention from staff, were attended to punctually and experienced very few administrative problems. The same trend was seen when it came to the meeting of expectations or rehabilitation: of the 30 clients, 27 indicated that their expectations had been met.
Compliance with preventative measures and secondary complications
According to 18 clients, they were taught measures to prevent further amputations. This seemed to have the desired effect as only one client cut corns, three clients used a heater, three clients wore inappropriate socks and five walked barefoot, all practices that can compromise limbs with poor circulation and sensation and lead to further amputations. Ten participants required to adhere to a diabetic diet had failed to do so.
Secondary complications
The most commonly experienced secondary complication was phantom limb pain (14 participants). This was followed by joint and muscle tightness (13 participants), stump pain (11) and depression (10).
Indoor mobility
As indicated in Table V,with regard to mobility, the main challenge experienced was lifting and carrying objects.
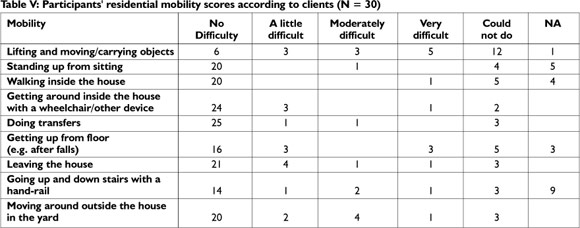
According to the results of the Mann-Whitney U test, significantly more participants who received prosthetic rehabilitation could walk in the house (p = 0.039), pick up objects from the floor (p = 0.031) get up from the floor (p = 0.00069), leave the house (p = 0.023), go up and down stairs with a handrail (p = 0.037) and move around in the yard (p = 0.0069) than those who did not receive prosthetic rehabilitation.
While indoor mobility training was provided by the programme, not all clients received it, as indicated in Table IV. The Spearman rank order correlations found that a lack of indoor mobility training had a statistically significant negative impact on the ability to lift and carry objects (p 0.011), to stand up after sitting (p = 0.042), get around inside the house (p = 0.00023), pick up objects from the floor (p = 0.00068), get up from the floor (p = 0.0072), leave the house (p = 0.0016), go up and down stairs with a handrail (p= 0.019) and move around in the yard (0.0013).
Community integration
Table VI indicates that clients experienced problems with community mobility and community integration.
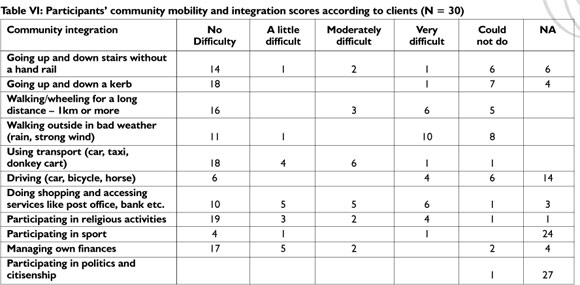
The Mann-Whitney U test indicated that prosthetic rehabilitation had a significantly positive effect on the ability to climb stairs (p = 0.037), go up and down a kerb (p = 0.0082) walk or wheel more than 1km (0.0089) and walk in bad weather (0.017). According to the Spearman rank correlations, failure to address indoor mobility during rehabilitation had a statistically significant negative impact on going up and down stairs without a hand rail (p = 0.019), going up and down a kerb (p = 0.0022), walking or wheeling 1km or more (p = 0.0032) and using transport (p = 0.0034).
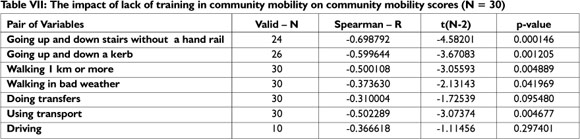
Similarly to indoor mobility training, not all clients received community mobility training (see Table IV). Failure to address community mobility during rehabilitation had a statistically significant impact on all aspects of community mobility scores except doing transfers and driving, as indicated by Table VII.
Productive activity
Twenty-nine participants indicated that the need to work or attend school did not apply to them. In addition, 15 indicated they were not economically self-sufficient.
Discussion
Profile of the study population
The increased ratio of males to females as found in the study is in accordance with the literature2,14,15,16. The majority of participants (21) was younger than 60 years old. This is similar to results from other African studies14,15, but contrasts with those of Hendry18, who found a mean age of 60.3 years in a study based at Tygerberg Hospital. It appears that Diabetes Mellitus (DM) caused amputations at relatively younger ages in the current study population, since Table III shows that DM was the cause of the amputation in 19 instances. Reasons for this might be multifaceted and related to race, South Africa's stage of economic development and poverty18,19. The findings pointed to a lower rate of traumatic amputations than those found by Bakkes15 and Kidmas et al16 and were more in line with the findings from Hendry18 and those in developed countries19. The study population was too small to draw any epidemiological inferences from the findings, but in view of the shortage of literature on the subject, the findings indicate a need for epidemiological studies on amputations in the Western Cape, South Africa and Africa, as it is not possible to plan effective services and design rehabilitation programmes without adequate epidemiological data.
Record keeping
Without annual reports, budget information and clinical statistics, service auditing is not possible and it will also be difficult to motivate for the provision of additional resources or even the continued existence of the service. Client clinical notes are legal documents and are used for clinical audits, teaching, research and administrative purposes20. They should be stored for at least six years after the final consultation with the client21. Of the 24 client folders that could not be located for the current study, 22 were still within the prescribed six year period. When records are stored in electronic format, a backup copy should be stored in a different physical location from the original21.
The lower limb amputee rehabilitation programme
Rehabilitation is a "goal-oriented" process5. In order to set specific, measurable, participation-focussed goals, a comprehensive client assessment, using valid, reliable and relevant measuring instruments is essential22. For instance, in this case, therapy included muscle strengthening and range-of-movement exercises, but no baseline measurements were recorded. In order to develop individual programmes according to the needs of the client, it is necessary to have the results of the baseline and follow-up assessments recorded.
In addition, no participation measurement, such as the ICF Checklist8 or Re-integration to Normal Living Index22 was used by the therapists. Furthermore assessments appeared not to include an evaluation of the activities of daily living, home environment, community integration and participation needs, or of contextual barriers and facilitators as the ICF checklist8 or CHIEF11 can provide. This might be one of the reasons why little attention was given to community integration and participation during the rehabilitation process as indicated by therapists. Challenges related to these areas were further exposed when these findings were triangulated with client data which indicated that transport problems and environmental barriers were poorly addressed in 26 and 27 instances respectively.
Treatment seemed to follow a set routine to the point where therapists indicated that prosthetic and non-prosthetic rehabilitation were the same except for the provision of prosthetic training. Some aspects are expected to be similar, but a client who receives a prosthesis would require more input into stump preparation than clients who use a wheelchair or crutches for mobility. In their case, there is a need for enhanced upper limb strength. A difference in treatment should become especially obvious as treatment progresses towards residential and community integration. The wheelchair user requires wheelchair dexterity and transfer skills, as well as environmental and home management strategies focused on wheelchair access23. Prosthetic training must focus on functional prosthetic use in the community. In addition more emphasis should be placed on outside mobility, the negotiation of uneven terrain, slopes, busy streets, escalators and how to get in and out of cars, busses or trains, whichever is applicable3.
The importance of prosthetic rehabilitation is underlined by the fact that clients with prostheses performed significantly better in various areas of domestic and community integration. This improvement in function can partly be attributed to the prostheses, since a prosthesis facilitates walking, thereby decreasing the barriers caused by the built and natural environmental. It must however, be pointed out that individuals who received prostheses from the Provincial Government of the Western Cape (PGWC), the province in which the study centre is situated, were by the nature of the selection process, fitter and more functionally able than their non-prosthetic counterparts6. This could influence the above findings and prevent one from attributing the improvement in function solely to the prosthesis. However, the positive impact on function cannot be ignored and it is desirable that every person who could possibly function with a prosthesis should receive one. This might not have been true for the current participants, as the evidence-based guidelines of the PGWC6 were not used to determine whether a client was a prosthetic candidate or not.
While crutches and walking frames were supplied to all clients who needed them, prostheses and wheelchairs were not. When the waiting list for these devices was lost, no measures were taken to recapture the information. In addition, the names of the eight clients who were waiting for wheelchairs could not be found on the provincial waiting list. When funding becomes available, these clients will be provided with a wheelchair24. Furthermore, this waiting list is also used to motivate the provision of additional funds. If the names of clients are not on the list, one cannot accurately quantify the need.
Part of comprehensive rehabilitation is to provide post-discharge follow-up for as long as is necessary. When clients received assistive devices such as prostheses and wheelchairs, these devices must be serviced and replaced when they wear out25. The centre has an open-door policy, however, assessing one's own health needs and utilising an open-door policy is part of an empowerment process that begins with guidance towards self-directed health monitoring.
This was only partially addressed during rehabilitation, as indicated by the findings (See Table IV).
Client Outcomes
Client satisfaction with the programme
Clients were satisfied with the services they received as reported in the results. They reported that staff was always very friendly, supportive and well-mannered. Clients also reported they were satisfied that they had been seen promptly after making appointments. This was a positive finding in a government health care system seeing that clients often spend entire days waiting to be assisted26.
Education and prevention of secondary complications
A positive finding was that clients had a sound knowledge of aspects that might lead to common complications and, according to the results, generally adhered to the necessary preventative measures.
Two findings raised concerns, firstly, it seems that counselling and referral for supportive psychological services were neglected in the case of the ten clients who reported that they suffered from depression. Secondly, in the case of the three clients with stump wounds; these are generally caused by poorly fitting prostheses. This reinforces the urgent need for follow-up.
Functional outcomes and community integration
A lack of identification and addressing of environmental barriers and retraining of community mobility were a big shortfall. Mobility training was done at the centre and opportunities were not created to address the mobility of clients in the community. The centre is situated in the community in which the clients have to function and community integration can commence on exiting the gates of the centre and walking down the road.
Productive activity
One of the cornerstones of rehabilitation is the reintegration of the individual into the community as an independent and productive member of society5,27. In this study 25 participants cited amputation as the reason for their unemployment. Re-employment figures compared poorly with international figures that indicate a 60% to 87% return to work rate28,29,30. However, there is a need to place employment figures in context. At 25.5%32 unemployment rates in South Africa are high and participants had a low level of education, both factors making it difficult to find employment30. On the other hand legislation in South Africa guarantees non-discrimination and employment equity for designated groups including persons with disabilities32. Rehabilitation staff has the responsibility to empower clients to invoke relevant legislations and state policies so as to enhance the quality of their lives. In addition, rehabilitation therapists at primary level should mobilise community resources and play an advocacy role5,33. This includes initiating processes with the Department of Labour, the local municipality and private businesses in the area, to identify employment and training opportunities for clients34.
One participant was a learner for whom re-integration into the schooling system was crucial. However, she dropped out of school after the amputation. There was no mention in her folder of counselling or any discussion with her or her parents about her return to school, school visits or referral to education authorities.
CONCLUSION
The study centre failed to implement the shift from the impairment-focussed, medical model and an individual-orientated approach to rehabilitation designed to encourage social integration, the equalisation of opportunities and collaboration as required by the social model of rehabilitation and underscored by NRP and CBR principles5,34,35. The programme failed to address important aspects of rehabilitation such as community mobility and integration, economic self-sufficiency, as well as liaison with local government, district and provincial departments and the community.
On an individual level, the programme was impairment-focussed and issues such as community integration and participation in life roles were not adequately addressed. On a societal level, no evidence could be found of the promotion and protection of the rights of persons with disabilities or the inclusion of persons with disabilities through intersectoral collaboration, advocacy and the addressing of environmental barriers35.
Other shortcomings were an absence of programme vision, mission or objectives, of monitoring and assessment and of the use of measuring instruments, as well as a lack of basic administration procedures such as statistic records, the maintenance of comprehensive client treatment notes and more advanced activities such as the compilation of an annual report.
Study recommendations
There is a need for a fundamental shift in philosophy from a medical model approach to a client-centred, social model approach to rehabilitation. Management, service providers and client representatives need to look at policy requirements of the service, and to see how they can meet these requirements. Measurable objectives and a vision need to be developed to provide guidelines for service providers. Client-outcome measures and programme monitoring and evaluation practices need to be implemented. Fail-safe systems for the gathering and storing of statistics and client notes need to be developed and the implementation of these monitored and enforced. These should culminate in a yearly report of services. Structured client follow-up procedures need to be established and adhered to. Even though this is an outpatient service, clients should receive follow-up dates in a year or six months' time, especially those with assistive devices such as wheelchairs or prosthesis. Therapists should play an advocacy role in the community and through liaison, start a process of collaboration with businesses and other government departments. They should be provided the support (such as transport) and authority to do this. All this might require that therapist's job descriptions are revisited and changed accordingly.
It is essential that service providers receive supervision, guidance and mentorship in many areas including clinical practice, community based rehabilitation practices, interdisciplinary teamwork, client and programme evaluation and the importance of record keeping.
The PGWC guidelines must be used to determine suitable prosthetic candidates, as well as to provide guidance during non-prosthetic rehabilitation, prosthetic preparation and prosthetic rehabilitation6.
LIMITATIONS OF THE STUDY
The number of participants (30) was small. This impacted negatively on statistical analysis and the interpretation of statistical findings. It is uncertain how many potential participants could not be identified because of a lack of records and thus to what extent findings are subject to generalisation. The missing client records also contributed to the missing clinical data bias. In addition, combining or self-designing measuring instruments meant that these instruments were not tested for validity and reliability. Thus results from this study must be used with caution.
ACKNOWLEDGEMENTS
We would like to acknowledge Ms Siphokazi Gcaza, University of Stellenbosch, for her assistance and input on the study.
A special thanks goes to Dr Justin Harvey, University of Stel-lenbosch, for his invaluable assistance in the statistical analysis of this study.
We would also like to thank all the participants who took part in the study.
REFERENCES
1. Godlwana L, Nadasan T, Puckree T. Global trends in Incidence of Lower Limb Amputation: A review of the literature. SA Journal of Physiotherapy, 2008; 64(1): 8 - 12. [ Links ]
2. Gutacker N, Neumann A, Santosa F Moysidis T, Kröger K. Amputations in PAD patients: Data from the German Federal Statistical Office, Vasc Med, 2010; 15(1): 9 - 14. [ Links ]
3. Manderson L, Warren N. The Art of (Re) Learning to Walk: Trust on the Rehabilitation Ward. Qual Health Res, 2010; 20(10): 1418 - 1432. [ Links ]
4. United Nations (UN). Convention on the Rights of Persons with Disabilities. http://www.un.org/disabilities/convention/convention-full.shtml 2006 (accessed 17 January 2011). [ Links ]
5. Department of Health (DOH). National rehabilitation policy, Rehabilitation for all. 2000. [ Links ]
6. Western Cape Department of Health (WCDoH). Provincial Circular 176 of 2010. [ Links ]
7. Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ, 2004; 328:1312-1315. [ Links ]
8. WHO. International classification of functioning, Disability and Health. Geneva. Switzerland. 2001 http://www.who.int/classification.icfwhoasii/en/index.html (Accessed 25 March 2009). [ Links ]
9. WHO-DASII. 1981. World Health Organisation. Disability assessment schedule II. [ Links ]
10. Gauthier-Gagnon C, Grise MC, Lepage Y. The Locomotor Capabilities Index: Content Validity. J of Rehab Outcomes measure-ment,1981; 2(4): 40 - 46. [ Links ]
11. Whiteneck, G.C., Harrison-Felix C.L., Mellick D.C., Brooks, C.A., Charlifue S.B. and Gerhardt K.A. Quantifying environmental factors: A measure of physical, attitudinal, service, productivity and policy barriers. Archives of Physical Medicine and Rehabilitation. 2004, 85(8): 1324-1335. [ Links ]
12. Kettner, P Moroney, R. and Martin, L. Designing and managing programs: An effectiveness-based approach, 3rd edition. Thousand Oaks, CA: Sage Publications 2008. [ Links ]
13. Domholdt, E. Rehabilitation research: Principles and applications. 3rd ed. Missouri USA Elsevier Saunders, 2005. [ Links ]
14. Manderson L. and Warren N. The Art of (Re)Learning to Walk: Trust on the Rehabilitation Ward. Qual Health Res, 2010, 20(10) 1418 - 1432. [ Links ]
15. Bakkes ES. Possible predictors of functional prosthetic ambulation in adults with unilateral above knee amputation in the Western Cape. Unpublished Master Thesis. Centre for Rehabilitation studies. Stel-lenbosch University. 1999. [ Links ]
16. Kidmas AT, Nwadiaro CH, Igun GO. Lower Limb Amputation in Jos, Nigeria. East African Medical journal, 2004; 81(8): 427 - 229. [ Links ]
17. Asano M, Rushton P Miller WC, Deathe BA. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int, 2008; 32: 231 - 243. [ Links ]
18. Hendry J. A. A descriptive survey study of lower - limb amputees admitted to Tygerberg Hospital (1985 - 1987). Unpublished Master of Medical Science (Epidemiology) thesis, University of Stellenbosch. 1993. [ Links ]
19. Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular Diseases: Part I: General Considerations, the Epidemiologic Transition, Risk Factors, and Impact of Urbanization. Circulation, 2001; 104: 2746-2753. [ Links ]
20. Unwin J, Kacperek L, Clark C. A prospective study of positive adjustments to lower limb amputation. Clinical rehabilitation, 2009; 23(11): 1044 - 1050. [ Links ]
21. Health Professions Council of South Africa (HPCSA). Guidelines for good practice in the Health Care Professions Guidelines on the keeping of patient records booklet 14 Pretoria. 2008. [ Links ]
22. Landrum PK, Schmidt ND, Mclean A. Outcome-oriented Rehabilitation. lst ed. Gaithersburg. Aspen. 1995. [ Links ]
23. Routhier F Vincent C, Desrosiers J, Nadeau S. Mobility of wheelchair users: A proposed performance assessment framework. Disability and rehabilitation, 2003; 25(1): 19 - 34. [ Links ]
24. RSA. DoH. Guidelines on the provision of mobility assistive devices. 2003. [ Links ]
25. World Health Organization (WHO). Guidelines on the provision of manual wheelchair in less resourced settings. 2008. [ Links ]
26. Day C, Gray A. Health and Related Indicators In: Barron P Roma-Reardon J, editors. South African Health Review 2008. Durban: Health Systems Trust. 2008. URL: http://www.hst.org.za/publications/841. [ Links ]
27. McColl MA, Davies D, Carlson P Johnston J, Minnes P The community integration measure: development and preliminary validation. Arch Phys Med Rehabil, 2001; 81:292-300. [ Links ]
28. Burger H, Marincek C. 2007. Return to work after lower limb amputation. Disability and Rehabilitation, 2007; 29(17): 1323 - 1329. [ Links ]
29. Schoppen T, Boonstra A, Groothoff JW, van Sonderen E, Goeken LNH, Eisma WH. Employment status job characteristics, and work-related health experience of people with lower limb amputation in the Netherlands. Arc Phys Med Rehabil, 2001; 82:239-45. [ Links ]
30. MacKenzie EJ, Bosse MJ, Kellam JF Pollak AN, Webb LX, Swiontkowski MF Smith DG, Sanders RW, Jones AL, Starr AJ, McAndrew MP, Patterson BM, Burgess AR, Travison T, Castillo RC. Early predictors of long-term work disability after major limb trauma. J Trauma, 2006; 61(3):688-94. [ Links ]
31. Statistics South Africa. Census. 2006. www.statssa.gov.za/census01 (accessed 25 September 2008). [ Links ]
32. Republic of South Africa RSA. Employment Equity Act No.55. 1998 http://www.dpsa.org.za/policies/employmentequityact.php Retrieved 01/04/2010. [ Links ]
33. Pollard N, Sakellariou D. Operationalizing community participation in community based rehabilitation: Exploring the factors. Disability & Rehabilitation, 2008; 30(1): 62 - 70. [ Links ]
34. Joint position paper: ILO, UNECSO, WHO. Community-Based Rehabilitation: A strategy for rehabilitation, equalization of opportunities, poverty reduction and social inclusion of people with disabilities. 2004. [ Links ]
35. Bury T. Primary Health Care and community based rehabilitation: Implications for physical therapy. Asia Pacific Disability Rehabilitation Journal, 2005; 16(2): 30 - 42. [ Links ]
 Correspondence:
Correspondence:
Jerome P Frederiks
jpf@sun.ac.za
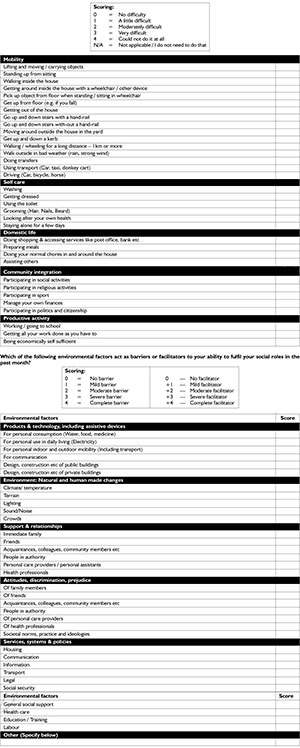
APPENDIX I
ICF based questionnaire on activities, participation and environmental factors
Participants reference number: _________________________________________
The purpose of this questionnaire is:
1) To determine if you struggle to perform your normal duties and roles because of your amputation and
2) To determine what environmental factors act as barriers or facilitators in performing these tasks.
How difficult was it to perform the following tasks over the last month?