Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Occupational Therapy
versão On-line ISSN 2310-3833
versão impressa ISSN 0038-2337
S. Afr. j. occup. ther. vol.43 no.2 Pretoria Ago. 2013
COMMENTARY
Using the Occupational Therapy Practice Framework-ll to treat a rare condition - brain abscess and empyema
Katherine GradidgeI; Daleen CasteleijnII; Denise FranzsenIII
IMSc(OT) Lecturer, Occupational therapy Department, Faculty of Health Sciences, University of Witwatersrand
IIPhD, Senior Lecturer, Occupational therapy Department, Faculty of Health Sciences, University of Witwatersrand
IIIMSc (OT), Senior Lecturer, Occupational therapy Department, Faculty of Health Sciences, University of Witwatersrand
ABSTRACT
Brain abscess and Empyema are potentially disabling conditions with lifelong consequences, yet there is a paucity of literature on occupational therapy assessment and treatment of these patients.
A recent record review found that the most important presenting problems were neuro- musculoskeletal, movement and mental deficits. Based on this review, and the lack of literature on the guidelines for assessment and treatment of these conditions, the need for an occupational therapy practice guideline was established.
The Occupational Therapy Practice Framework- II was used as a scaffold to draw up a guideline that will give occupational therapy clinicians working with this group of rare conditions a guideline for rehabilitation priorities for intervention.
Key words: Brain abscess, empyema, Occupational Therapy Practice Framework II, clinical practice guidelines
INTRODUCTION
Brain abscess (or cerebral abscess) and empyema are festering infections in the central nervous system1,2. Both disorders are rare1-3 with an international incidence of approximately 2- 3 patients per million per year4. A study conducted at Red Cross Children's Hospital in Cape Town reported on a 25 year experience (1966- 1991) in the department of Paediatric Neurosurgery on brain abscess in childhood. Their retrospective analysis indicated an age range of 3 months to 14 years and a mean age of 8 years. Sixty one of the 98 children were males (60.7%) 5. A study that reviewed management and outcomes of adults with brain abscess in the department of Neurosurgery at Groote Schuur Hospital found an incidence of 121 patients between 1993 and 2003. The mean age was 33 years with a 5:1 male: female ratio6.
Common sequelae of brain abscess and empyema include focal neurological deficits, cognitive impairment and seizures. Hemiplegia and aphasia are the most common neurological deficits seen3. Focal seizures are common, but of more concern is this patient groups' predisposition to status epilepticus3,5. Seizures were found to occur in between 10, 7% 6 and 30- 50% of all patients preoperatively3. Postoperatively seizures occur in 10 to 72% of patients3. Despite the difference in cause, the signs and symptoms that occupational therapy deal with are the same as in other patients with neurological deficits.
Cognitive impairments are one of the most serious long term implications. Studies carried out in the 1980's found on follow up, that cognitive impairments were still significant problems at follow up 6 and 20 years post initial incident7. More recent studies showing the long term implications of brain abscess and empyema could not be found and recent advances in medical and surgical treatment such as computed tomography, antibiotics and improved surgical evacuation of the infection may mean the incidence of these problems is lower3.
A study done at Chris Hani Baragwanath Hospital between December 2005 and May 2007 reviewed occupational therapy records retrospectively. All occupational therapy records between December 2005 and May 2007 were reviewed and 33 records were found8.This study confirmed that at least half of the subjects (n = 16) had some neuro-musculoskeletal and movement deficits and a third (n = 11) had mental deficits8. Studies are in agreement that brain abscess and empyema are serious conditions with sequelae such as depressed level of consciousness, cognitive deficits and focal neurological deficits being common presentations3,5,7. Mortality rates have been reported as ranging between 7.5% to over 40%6. With the severity of the reported sequelae it is a given that there will be an impact on functioning. Surgical and medical information is readily available, however, no information could be found on the impact on function and no occupational therapy related literature could be found on the assessment and treatment of patients with these conditions.
Databases searched included Medline, Scirus and Cinahl, using the search terms brain abscess, empyema, occupational therapy and rehabilitation. Initially a search of five years was used but as nothing relevant was found in this period, all literature was searched. Furthermore there was a paucity of literature on deficits that occur in brain abscess and empyema other than for hemiplegia. No research on the consequences of these diseases on a patient's occupational performance has been published. The rarity of the condition should not negate how important it is that the patients receive adequate intervention. Anecdotally it was found that occupational therapy clinicians in South Africa who are working in the neurosurgical field have little knowledge of the condition and therefore there is poor consensus on the focus of assessment and treatment for patients presenting with brain abscess and empyema.
The purpose of this paper was therefore to present a guideline for the assessment and treatment of patients with brain abscess and empyema in occupational therapy with the view to extending this guideline to other rare conditions with little evidence and established assessment and treatment recommendations.
There are different ways to draw up practice guidelines. Cul-leton described clinical practice guidelines as systematically developed statements to assist practitioners reach appropriate health care decisions9. An abundance of published evidence is needed to draw up sound clinical practice guidelines. Following the review of the literature and the record review and finding the lack of evidence based practice that could be used to guide assessment and treatment; it was decided to explore the Occupational therapy Practice Framework: Domain and Process. 2nd Edition (OTPF-II) as a framework for developing these guidelines10.
LITERATURE REVIEW
"The occupational therapy Practice Framework: Domain and process. 2nd Edition (Framework- II) is an official document of the American Occupational Therapy Association to guide occupational therapists in practice. Intended for occupational therapists and other health professionals, it presents a summary of interrelated constructs applied in occupational therapy practice"10:625.
The Framework- II was developed by the American Commission on Practice to explain occupational therapy's role with individuals and organisations health and participation and ultimately engagement in occupation10. This framework is the revised version of the Occupational Therapy Practice Framework: Domain and Process11. The first framework was in turn developed following the revision and updating of the Uniform Terminology for Occupational therapy- Third Edition (UT- III). The review of the UT- III document indicated the need to incorporate the International Classification of Function (ICF) terminology to make occupational therapy understandable for others ". It was felt that this would make the profession and contribution of occupational therapy to health more understandable to external audiences12. Occupational therapists, themselves, needed to understand their position within the greater context in order to place themselves within established and rising areas of practice12. The revisions of the UT- III incorporated occupation more clearly and explicitly and showed the inter-relationship between the domain and the process sections12. The Framework I received both praise and criticism. It was praised for the centrality it reinstated for occupation in occupational therapy13. However it was criticised for being illogical, and the poor reliability between the Framework I and occupational therapists in practice14,15. As a result the above research concluded that the Framework I was not helpful in clinical or academic fields. This research recommended that the basis of such frameworks should be on consensus that makes occupational therapy easy for outsiders to understand.
Further to the above criticisms the Framework I was also criticised for ignoring the importance of standardised assessments that can successfully measure interventions13. It also neglected activity analysis, fundamental to our ability as occupational therapists to successfully use activity and occupation in the evaluation and intervention of a patient13. Moreover despite the comprehensive nature of the framework there is little evidence of its use in clinical practice13.
The American Occupational Therapy Association (AOTA) reviewed the Framework and using feedback from members, academics and clinicians updated it to include emerging themes and changes in occupational therapy. These updated changes were published in 200810. The document emphasises the importance of the founding tenets of occupational therapy that occupations can be used as a therapeutic means, but acknowledges that it is a developing document and welcomes feedback10. Only one article was found that used the OTPF-II. This article described using the OTPF-II in combination with a specific approach and model16. The authors of the OTPF-II found there was good integration of this framework, approach and model due to a shared ideology of the importance of the interaction between the patient, task and environment16. Despite the OTPF-II10 being published in 2008 no literature was found that uses the OTPF-II in clinical practice. This begs the question whether this is due to the lack of use of the OTPF-II in clinical practice or whether clinicians are not publishing articles on its use.
Evidence based practice (EBP) is a reality in current health care practice, as the demand on health care providers is to supply thorough intervention based on sound evidence of its effectiveness17,18. Evidence based practice is in line with the profession's Code of Ethics which calls for us to provide occupational therapy based on current and accurate information19. Occupational therapy is a developing, growing profession and occupational therapists have been encouraged to use a more academic approach to clinical prac-tice19. Despite the importance of using EBP in practice occupational therapists are faced with a number of challenges in implementing current research into practice. These challenges include lack of time and support, poor knowledge on how to critically evaluate the evidence and how to implement research information into practice20. Ikiugu et al.21 also emphasised the need for occupational therapists to understand the theoretical basis of practice, as well as the implementation of this clinically before they are able to evaluate research, determine if it is pertinent and be able to implement it21. Despite this, research shows that occupational therapists often do not see the importance of theory and are reluctant to use it in practice, resulting in a gap between development of theory and its clinical implementation21. Clinical practice guidelines are therefore a channel through which evidence can be accessed and the best clinical outcomes for patients can be promoted20.
Clinical practice guidelines are recommended ways of practising and provide a set of procedures to deal with a patient22 . The Canadian Association of Occupational Therapists (CAOT) state that these clinical practice guidelines should improve outcomes in patient care. Development of specific occupational therapy clinical practice guidelines will emphasise occupational therapy's role in patient care and highlight the importance of interdisciplinary patient care20.
Sackett et al23, one of the key thinkers behind EBP, stressed the importance of using a mix of evidence from research and clinical experience23. This is especially important with reference to brain abscess and empyema. As these are rare conditions most commonly seen in underdeveloped countries24 there is a paucity of research related to their assessment and treatment, the same for the occupational therapy literature . Furthermore the input of clinical experience is especially relevant in the South African (SA) context, as Joubert points out that historically SA occupational therapists have subscribed to western knowledge systems which are often poorly translated and implemented in SA24. This raises the question as to whether current occupational therapy assessment and treatment guidelines are clinically relevant in SA and other developing countries.
RECORD REVIEW
A retrospective record review was conducted by the author to obtain information about the neuro-musculoskeletal and movement deficits, and mental deficits found following brain abscess and empyema8. All occupational therapy records of patients with brain abscess and empyema admitted to Chris Hani Baragwanath Hospital Neurosurgery ward between December 2005 and May 2007 were reviewed. Thirty three occupational therapy records were available.
Sixteen of the 33 patients presented with neuro-musculoskeletal and movement deficits, some patients presenting with more than one deficit. The most common was Hemiplegia (50% of the deficits).
Of the 33 patients only 10 had mental deficits (30.3%). Some patients presented with more than one of listed deficits. The most common deficit seen in Figure 1 was poor body concept.
There was poor completion of the records accessed in the initial part of the study, with incomplete, incorrect data and poor consistency between records of what was recorded8. This limitation means that it is difficult to state whether all deficits were recorded and severity of deficits is not apparent from these records. The problems encountered in this study were commonly found in other record review studies25-27.
Despite the limitations of using a record review methodology it is still evident that patients with brain abscess and empyema present with neuro-musculoskeletal and mental problems and would benefit from occupational therapy assessment and treatment.
DEVELOPMENT OF THE ASSESSMENT AND TREATMENT GUIDELINE
Following the research into brain abscess and empyema it was found that there was a need for specific practice guidelines for occupational therapy assessment and treatment of this patient group. Occupational therapists may experience anxiety about treating novel conditions and as brain abscess and empyema are rare conditions they may experience a lack of confidence in their selection of assessment and treatment techniques.
It was also found in talking to occupational therapy clinicians working in the neurosurgical field that there was little knowledge and therefore limited consensus on the focus of assessment and treatment for this patient group.
In drawing up these practice guidelines the normal clinical reasoning process was needed and this practice guideline is intended to help take clinicians through this process. As a result there are generic aspects to the process that can be applied to other similar conditions. Theoretical frameworks need to drive practice guidelines and OTPF-II is well documented in the literature and has been used by the University of Witwatersrand as the framework for undergraduate training. It has been found to be helpful in clearly explaining the occupational therapist's domain of practice to the rest of the health care community as well as explicitly delineating the occupational therapy process for students during clinical practice. This indicates that it is a useful structure to use in clinical practice.
It was found in the literature review that the OTPF-II gave a summary of the different facets that guide occupational therapy assessment and treatment. The OTPF- II was never intended for use alone but in combination with different frames of reference and as a scaffold on which to hang concepts10. The scaffold can be used as a platform on which a clinician can add their own clinical reasoning, frames of reference, types of intervention and context.
Conceptual outline of the guideline
The OTPF-II consists of the two sections- the domain and process. The process was used as a guideline to determine which domains would be focused on in each stage of the process (Evaluation, Intervention and Outcomes). Central to the OT process is collaboration between the patient and occupational therapist. This collaboration should be done by evaluating the patient's goals, his problem areas and using theories and knowledge to guide this process10. This collaboration should include the family and support groups if possible. Throughout the process the occupational therapist is engaged in clinical reasoning regarding her assessment findings, treatment ideas and the outcomes that she is working towards10.
The OTPF-II provides a scaffolding that recommends assessment and treatment over a timeline, in this case using the different phases of treatment28. Due to the chronicity of the condition, the therapist is involved for long periods of time. As a result the programme should be adapted to changes in condition and the patient's development over time. The different phases were used to indicate what should occur at each stage in the assessment- treatment continuum. The first phase in the occupational therapy process involves evaluation of the patient's occupational profile10. The occupational profile gives the occupational therapist insight into the patient's background and priorities. Using the occupational profile as the first step in developing the guideline the following important areas were highlighted.
Areas that were highlighted as most important can be seen in Figure 2 on page 36. The strengths and limitations of the patient are important to note as the pre-morbid abilities of the patient may affect how much potential for recovery the patient has. Support systems are essential in patients with brain abscess and empyema but since these conditions occur in developing countries3,28 the access to support systems may be limited. Without support systems easy access to health care and follow up facilities becomes problematic.
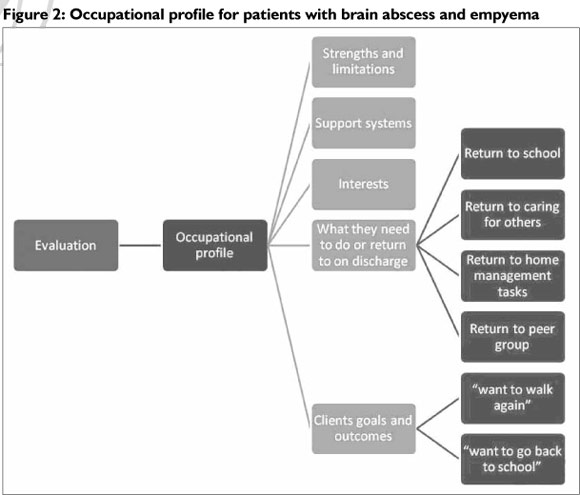
In drawing up an occupational profile of a patient it is important to acknowledge the age group as this diagnosis affects patients from childhood into adulthood5,6. Roles over the lifespan change and may also differ depending on the family structure of the patient, as well as the patients expression of independence29. The cultural context of each patient is important to the understanding of the nuances in his different roles.
Within the client centred approach interests are always important in planning outcomes with the patient to determine modalities of treatment as well as the focus of intervention. For example in teenagers the transition from adolescence to early adulthood changes the clients interests due to the movement out of the family setting to the peer group29. The patient's own goals and outcomes need to strongly influence the modality and direction of treatment. Examples of common goals as articulated by the patients are "I want to walk again" or "I want to go back to school" again indicating that the age of the patient group is important.
This occupational profile will change as the patient goes through the life stages and stages of recovery and therefore continual reassessment is paramount.
When the occupational profile is clearly understood the analysis of occupational performance needs to be completed, which looks at the interaction of the performance skills, client factors, environ- ment and performance of occupation10. (See Figure 3)
When considering this aspect of evaluation the occupational therapist needs to consider the phase of treatment the patient is in. Because of the life- threatening, serious nature of the diagnosis24,33 all patients will be acutely ill initially. During this phase of treatment the remediation or restoration approach should be used in order to improve skills that have become impaired10. In this case the focus will be on global mental functions, including functions like level of consciousness and arousal and orientation to person, place and time. During this acute phase the therapist will also focus on assessing the patient's tolerance to all sensory input as well as awareness and discrimination of sensory inputs. Finally as the most common physical problem these patients are presented with is hemiplegia8 the occupational therapist will focus on assessing control of voluntary movement, muscle tone and muscle strength. Other performance skills that need to be considered during assessment of these patients are balance and praxis8.
During the restorative and pre- discharge phase the remediation and restoration approach will still be used. There will be some overlap of skills and abilities that will be focused on but in addition there will be increased focus on performance of occupations and specific mental functions. The particular problems that have been raised with this patient group were attention and experience of self8. A study by Gormley et al.3 also found that these patients struggle to perform at school indicating that all specific mental functions should be thoroughly assessed. Finally the patient's engagement in occupations should be evaluated. Taking into account the information gained during the evaluation of the occupational profile one needs to evaluate the occupations relevant to the patients roles, environment and where they will return to.
During the chronic phase the approaches used will be maintenance and modification. The maintenance approach is used to provide assistance to allow patients to perform occupations using their improved skills10. The modification approach entails changing the patient's environment or the way in which they carry out occupations to make them easier10. During this phase the focus will be on assessing the patient to determine what skills, strengths and support he has in order to determine what modifications need to be implemented and in which areas supervision or support is needed to maintain existing skills.
Once the full evaluation of the occupational profile and analysis of occupational performance has been carried out outcomes need to be determined together with the patient. (See Figure 4).
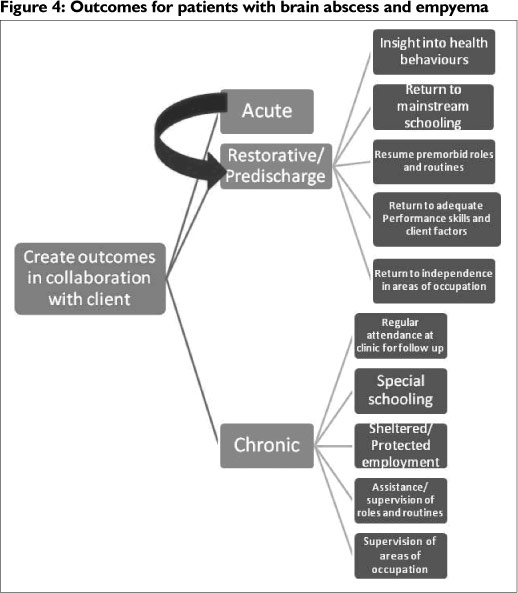
"Supporting health and participation in life through engagement in occupation"10625 is the all encompassing goal of occupational therapy. This statement includes three important aspects of a patient's life when drawing up outcomes- health, participation in life and engagement in occupation. Therefore when drawing up outcomes with patients with brain abscess and empyema these three aspects have been taken into account. Theorists have emphasised the importance of drawing up main outcomes as a means to appraise intricate interventions31.
Outcomes should also involve the interaction of three decision making areas. The outcomes should involve the family and patient's desires and expectations, the actual possibilities of each patient and the multidisciplinary team's treatment provision and abilities. Based on these three inter-acting decision making dynamics one can begin to draw up outcomes for each patient in each phase of treatment.
Outcomes for the patient in the acute phase entail stabilisation of the medical condition and improvement to the restorative and pre-discharge phase. In the restorative / pre-discharge phase the outcomes focus on improving underlying performance skills to allow the patient to return to their pre-morbid roles and occupations as soon as possible.
As the therapist determines that there is a plateau of improvement and the patient's condition moves to the chronic phase the outcomes for patients with brain abscess and empyema will change slightly. In this phase the types of outcomes will include adaptation, ensuring participation in occupations and quality of life10. During the chronic phase the outcomes will focus on ensuring there is continued support for the medical condition. Some outcomes will involve adaptation of occupations, for example changing the type of educational environment the patient attends or looking at alternate employment options. The outcomes still encourage participation in all areas but the participation may be adapted by changing a setting, way in which an occupation is completed, changing the demands or encouraging the use of supervision.
Clinical appeal of the guideline
Clinicians often complain of demanding caseloads which leave little time for investigation of novel conditions21, such as brain abscess and empyema, as well. When clinicians do encounter literature for these novel conditions it is usually not occupational therapy specific32. It is unfortunate that there is a paucity of literature on brain abscess and empyema as this curtails the development of rigorous clinical practice guidelines.
In these cases practice guidelines are welcomed by clinicians as they assist in providing a user- friendly way of assessing and treating novel conditions. The hope is that the practice guideline will help to make assessment and treatment of brain abscess and em-pyema concrete and easily understandable. As this is a first attempt to fill the gap in this area feedback on the guidelines use in clinical practice will be highly appreciated and can be communicated with the authors.
It has been recommended that simply publishing clinical practice guidelines will not result in any improvement of patient treatment. Rather there needs to be input from different stakeholders on the guideline28. The guideline may also be helpful in treating other space occupying lesions. Feedback on the usefulness of the guideline in these cases would be welcomed. A case study has been included to demonstrate how the guideline could be used clinically.
Case study
Ms BP is a 9 year old girl, admitted to a large academic hospital in Gauteng, SA on the 19/02/2012 with a history of headache, decreased level of consciousness and seizure. Computed Tomography Brain (CTB) confirmed a diagnosis of complicated sinusitis with subdural empyema and multiple abscesses. On the 20/02/2012 she underwent a right ethmoidectomy and surgical drainage of the subdural empyema and abscesses.
She was initially screened by occupational therapy on the 20/02/2012. Due to her fluctuating levels of arousal the OT monitored her condition until the 2/03/2012 when a full assessment was completed. On assessment the occupational profile was outlined. Her limitations were an expressive aphasia and low socio- economic status. Her support system was limited due to her distance from home. Her family lived about 350km away in another province. It was difficult to ascertain her interests and what she would need to return to on discharge due to the aphasia. However she was quite adamant that she wanted to return to school and therefore this was a goal that was decided on based on the client's expressed needs and the Occupational therapists assessment. As she was in the restorative phase of treatment the following aspects of occupational performance were evaluated. On assessment of her specific mental functions it was found that she had decreased attention span, a left unilateral neglect, apraxia and poor basic concepts such as colour and poor spatial relations and figure ground perception. On evaluation of her neuro-musculoskeletal and movement related functions she had a left hemiplegia with consequent poor control of voluntary movement and poor muscle strength. Her gait was also affected. Ms BPs performance of occupations was assessed and she was dependant in all areas of personal management. Her engagement in play and school would be assessed later.
Based on this assessment outcomes were created in collaboration with client. The main focus on treatment was to return her to adequate performance skills and client factors and independence in performing personal management tasks. Working on the performance skills and client factors, specifically mental functions was in keeping with the client's goal of returning to school. The treatment therefore focused on improving concepts, standing balance, control of movement and strengthening of left upper and lower limbs. Spatial relations, attention and improving awareness of left side were also treated in therapy.
On the 13/04/2012 Ms BP was transferred back to a regional hospital in her province of residence. On final evaluation she was found to be independent in washing, dressing, feeding and eating and toileting. However she still had difficulties with the following neuro-musculoskeletal performance skills and client factors: strength of left upper limb and lower limb, gait, standing balance and hand function. In terms of specific mental functions she still had difficulty with concepts and spatial relations as well as planning and problem solving. She also continued to present with an expressive aphasia and perseverated on certain words.
The therapists treating this patient therefore re-evaluated her as being in a chronic phase. They also assessed her school performance more thoroughly and found due to continued underlying deficits in client factors and performance skills she would be unable to return to mainstream schooling currently. As a result the outcomes were modified slightly. These modified outcomes were communicated to the therapists at the regional hospital. The modified outcomes included special schooling and continued occupational therapy and physiotherapy to continue to improve her underlying client factor and performance skill deficits as well as her performance of OPAs. The therapists also recommended that her caregivers be contacted and educated about her condition and the importance of follow up appointments at the hospital. The caregivers should also be alerted to the possible need for supervision of tasks she could previously do unsupervised.
Most occupational therapists that treat rare conditions rely on colleagues' input and information from other sources such as the internet. This guideline will give therapists a starting point in treating this rare and often complicated condition, as was illustrated in the case of Ms BP.
CONCLUSION
Brain abscess and empyema are rare yet serious conditions that require medical treatment as well as rehabilitation. It has been found that approximately half of patients with these conditions present with neuro- musculoskeletal deficits and a third with mental deficits. This necessitates occupational therapy treatment. The OTPF-II was chosen as a scaffold on which to hang the concepts needed to develop guidelines for assessment and treatment of patients with brain abscess and empyema. It is felt that the OTPF-II and the structure of this guideline would be a useful tool in assessment and treatment of any rare conditions when there is a lack of evidence regarding assessment and treatment. Implementation and critical review of this guideline by occupational therapists would be welcomed as this is an attempt to bridge the gap for guidelines for rare conditions like brain abscess and empyema.
REFERENCES
1. Saez- Llorens X. Brain Abscess in children. Seminars in paediatric infectious diseases, 2003; April 14(2):108- 14. [ Links ]
2. Maertens P Cohen M, Krawiecki N. The use of neuropsychologi-cal evaluation in the medical management of subdural empyema. Archives of clinical neuropsychology, 1987; 2: 145- 54. [ Links ]
3. Gormley W, Del Busto R, Saravolatz L, Rosenblum M. Cranial and intracranial Bacterial infections. In: Youmans J (Ed). Neurological Surgery 4th Edition. Volume 5. Philadelphia: W. B. Saunders Company, 1996. [ Links ]
4. Lindsay K, Bone I. Neurology and Neurosurgery illustrated. 3rd edition. Bath: Churchill Livingstone; 2002. [ Links ]
5. Domingo Z, Peter J. Brain abscess in childhood. South African Medical Journal, 1994; 84:13- 5. [ Links ]
6. Sichizya K, Fieggen G, Taylor A, Peter J. Brain abscesses- the Groote Schuur experience, 1993- 2003. South African Journal of Surgery, 2005; 43(3):79- 82. [ Links ]
7. Nielsen H, Harmsen A, and Gyldensted C. Cerebral Abscess: a long term follow up. Acta Neurology Scandinavia, 1983; 67:330- 7. [ Links ]
8. Gradidge K, Franzsen D. Record review of patients with Brain Abscess and Empyema. The Internet Journal of Neurology, 2010; 13(1). [ Links ]
9. Culleton B. Development and limitations of clinical practice guidelines. Methods in molecular biology, 473: 251- 61 [ Links ]
10. American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and process, 2nd Edition. The American Journal of Occupational Therapy, 2008; 62(6):625-83. [ Links ]
11. American Occupational Therapy Association. Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 2002; 56(6):609- 39. [ Links ]
12. Youngstrom M. The Occupational Therapy Practice Framework: The evolution of our professional language. The American Journal of Occupational Therapy, 2002; 56(607- 608). [ Links ]
13. Gutman S, Mortera M, Hinojosa J, Kramer P Revision of the Occupational Therapy Practice Framework. The American Journal of Occupational Therapy, 2007; 61(1):119- 26. [ Links ]
14. Nelson D. Critiquing the logic of the Domain section of the Occupational Therapy Practice Framework: Domain and Process. The American Journal of Occupational Therapy, 2006; 60(5):511 -23. [ Links ]
15. Butts DS, Nelson DL. Agreement between Occupational Therapy Practice Framework Classifications and Occupational Therapists' Classifications. American journal of Occupational Therapy, 2007; 61(5):512- 8. [ Links ]
16. Yancosek KE, Howell D. Integrating the dynamical systems theory, the Task Oriented Approach and the Practice Framework for clinical reasoning. Occupational therapy in Health Care, 2010; 24(3):223- 38. [ Links ]
17. Bennett S, Bennett J. The process of evidence based practice in occupational therapy: Informing clinical decisions. Australian Occupational Therapy Journal, 2000; 47:171-80. [ Links ]
18. Grimmer K, Bialocerkowski A, Kumar S, Milanese S. Implementing evidence in clinical practice: the "therapies" dilemma. Physiotherapy, 2004; 90:189- 94. [ Links ]
19. Dirette D, Rozich A, Viau S. Is there enough evidence for Evidence- based practice in Occupational Therapy? The American Journal of Occupational Therapy, 2009 November/ December; 63(6):782-6. [ Links ]
20. Canadian Association of Occupational Therapy "CAOT Position Statement Clinical Practice Guidelines: Implications for Occupational Therapy (2005)" http://www.caot.ca/pdfs/PIF%20Report%20CPG%20Final.pdf (23/5/11, 2007). [ Links ]
21. Ikiugu M, Smallfield S, Condit C. A framework for combining theoretical conceptual practice models in occupational therapy practice. Canadian Journal of Occupational Therapy, 2009 June 2009; 76(3):162-70. [ Links ]
22. Austin C, Herbert SI. Clinical guidelines: Should we be worried? British Journal of Occupational Therapy, 1995; 58(11):481-4. [ Links ]
23. Sackett DL, Rosenberg WMC, Gray MGA, Haynes RB, Richardson WS. Evidence Based Medicine; What it is and what it isn't. British Medical Journal, 1996; 312-72. [ Links ]
24. Joubert R. Evidence based practice: a critique based on occupational therapy within the SA context. South African Journal of Occupational Therapy, 2005 September 2005; 35(2):8- 12. [ Links ]
25. Palmer J. Intracranial Abscess. In: Palmer J (Ed). Neurosurgery '96 Manual of Neurosurgery. Edinburgh: Churchill Livingstone, 1996. [ Links ]
26. Badcock D, Kelly A, Kerr D, Reade T. The quality of medical record review studies in the international emergency medicine literature. Annals of Emergency research, 2005; 45(4):444- 7. [ Links ]
27. Lowenstein S. Medical record reviews in emergency medicine: the blessing and the curse. Annals of Emergency research, 2005; 45(4):452- 5. [ Links ]
28. Harris J. Development, Use, and Evaluation of Clinical Practice Guidelines. Journal of Occupational & Environmental Medicine, 1997; 39(1):22-34. [ Links ]
29. Kielhofner G. A model of human occupation. Theory and application. 2nd ed. Baltimore: Williams and Wilkins; 1995. [ Links ]
30. McGillicuddy J, Hoff J. Infections of the central nervous system. In: Crockard A, Hayward R, Hoff J (Eds). Neurosurgery The scientific basis of clinical practice. Volume 2. Boston: Blackwell Scientific Publications, 1992. [ Links ]
31. Gracey F, Evans JJ, Malley D. Capturing process and outcome in complex rehabilitation interventions: A Y-shaped model. Neuropsychological Rehabilitation, 2009; 19(6):867-90. [ Links ]
32. Dubouloz C, Egan M, Vallerand J, von Zweck C. Occupational Therapists' perceptions of Evidence- based Practice. The American Journal of Occupational Therapy, 1999 September/ October; 53(5):445-53. [ Links ]
 Correspondence:
Correspondence:
Katherine Gradidge
katherinegradidge@gmail.com














