Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Obstetrics and Gynaecology
versão On-line ISSN 2305-8862
versão impressa ISSN 0038-2329
SAJOG vol.29 no.1 Cape Town Mai. 2023
http://dx.doi.org/10.7196/SAJOG.2023.v29i1.883
RESEARCH
The safety and efficacy of immediate post-placental IUD insertion versus the post-puerperal IUD insertion in women undergoing caesarean delivery
M A M DawoudI; O M HelalI; R O El KomyI; M M El SherbiniI; M O AwadII
IMD; Obstetrics and Gynecology, Faculty of Medicine, Cairo University, Egypt
IIMRCOG; Obstetrics and Gynecology, Faculty of Medicine, New Giza University, Cairo, Egypt
ABSTRACT
OBJECTIVE: To assess the safety and efficacy of immediate intrauterine contraceptive copper device (IUD) insertion following delivery of the placenta in women undergoing caesarean delivery.
METHODS: In this randomised clinical trial, 66 women were evenly divided into two arms, with 33 patients in each arm. The first group had an IUD inserted 10 minutes after delivery of the placenta (post-placental group), while the second group had their IUD inserted at 6 weeks following delivery (interval group).
RESULTS: The complication rate for post-placental IUD insertion was comparable with that of interval insertion. The expulsion and displacement rates were similar for both post-placental and interval groups at the 6-week and 3-month follow-up.
CONCLUSION: Post-placental IUD insertion is a safe and attractive option for postpartum contraception that should be offered to all women undergoing elective caesarean section after proper counselling.
Addressing contraceptive needs for postpartum women is crucial. However, two-thirds of patients in over 21 countries report unmet needs for family planning methods, within the first two years of childbirth.[1] The importance of postpartum contraception lies in mitigating the risks associated with unplanned pregnancies, especially in the first year after childbirth.[2]
The copper intrauterine contraceptive device (Cu-IUD) is a long-acting reversible contraception (LARC) method that is both safe and effective in reproductive-aged women who do not desire to become pregnant.[3] LARC has shown the highest continuation rate, with an effectiveness exceeding 99%.[4]
Immediate post-placental IUD insertion refers to the placement of the IUD within 48 hours of placental delivery, in both vaginal and caesarean delivery. Post-placental IUD insertion, on the other hand, involves placing the IUD within 10 minutes following placental delivery.[5] The benefits of immediate postpartum IUD insertion lie in the accessibility of service provision, thus avoiding the risks of unplanned pregnancy associated with delayed postpartum visits.[6]
Post-caesarean IUD insertion is associated with lower expulsion rates compared with vaginal delivery. Post-placental insertion results in higher expulsion rates compared with interval insertion (6 weeks postpartum). However, post-placental postpartum IUD insertion (within 10 minutes of placental separation) was associated with lower expulsion rates compared with delayed postpartum insertion (from 10 minutes after placental delivery up to 48 hours).[7]
This study aimed to compare the efficacy of post-placental insertion of Cu-IUD following caesarean deliveries with that of insertion 6 -8 weeks post-caesarean delivery.
Methods
This study included 66 women scheduled to deliver a live singleton via caesarean delivery and desired a Cu-IUD for postpartum contraception. Patients were recruited from Kasr Al-Aini Hospital (Obstetrics and Gynecology Department, Faculty of Medicine, Cairo University) between December 2020 and December 2021. The study was approved by the Research Ethics Committee of the Faculty of Medicine at Cairo University (approval number: MD-123-2020).
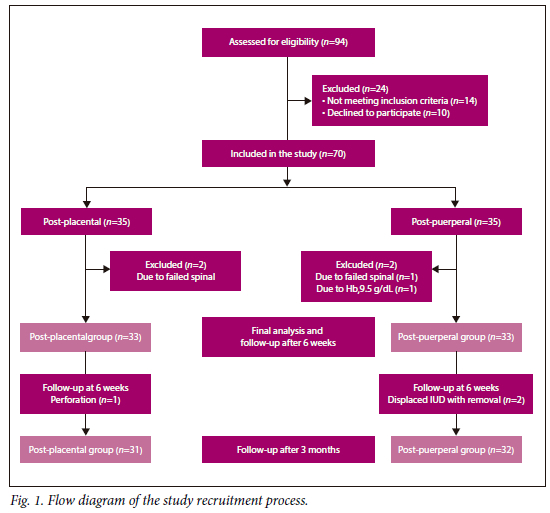
A flow diagram of the study recruitment process is shown in Fig. 1. Participants were divided into two groups: the post-placental group (n=33), which had an IUD insertion within 10 minutes following placental delivery, and the post-puerperal group (n=33), which had an IUD insertion 6 - 8 weeks post delivery.
The study included women aged 20 - 40 years old who desired IUD placement and who were eligible for elective caesarean delivery with regional anaesthesia and having a singleton full-term pregnancy >37 weeks' gestation as confirmed by the last menstrual period (LMP) and first-trimester ultrasound.
Excluded from the study were patients with contraindications for IUD insertion, including uterine abnormalities, Wilson's disease or copper allergy; active or suspected gonococcal or chlamydial infection; a history of chorioamnionitis indicated by prolonged rupture of membranes; fever and puerperal sepsis. Those who developed postpartum haemorrhage or underwent a prolonged procedure (>2 hours) were also excluded from the study.
Sample size calculation
The sample size calculation was performed to compare the incidence of expulsion between post-placental IUD insertion and puerperal IUD insertion. The calculation involved comparing two proportions from independent samples in a prospective study using the Fisher Exact test, with a fixed α-error level of p<0.05 and a power of 80%. The group ratio was set at 1. According to a study by Jatlaoui et al.[8] the expulsion rate for post-placental IUD insertion was 29.7%, while it was 1.9% for puerperal insertion. Accordingly, the minimum optimal sample size required in each group is 33 participants. Sample size calculation was conducted using PS Power and Sample Size Calculations software for MS Windows (Vanderbilt University, USA).
Patients were counselled during their antenatal care regarding their postpartum contraception plan. They were then randomly allocated in a 1:1 ratio to either the post-placental (10 minutes after placenta delivery) or the interval (6 - 8 weeks postpartum) insertion group. Computerised block randomisation was used, thus generating blocks of alternating sizes of 4, 6 and 8. To eliminate any potential bias, opaque-sealed envelopes were used to allocate participants to either group.
Experiment procedures
Informed consent was obtained by providing each patient with a thorough explanation of the nature of the study, intended benefits and outcomes, and potential risks. Each participant's medical, surgical and obstetric history was collected. They then underwent a comprehensive clinical examination, including general (maternal body weight and vital signs) and full obstetric assessment. Next, obstetric ultrasonography was performed to confirm gestational age, fetal presentation and placental localisation to ascertain the eligibility of recruited patients for participation in the study.
A caesarean section was performed, and the placenta was delivered through a uterine wall incision made high in the uterine fundus, either by hand or using its applicator. Before uterine incision closure, the IUD strings were guided to the lower uterine segment without trimming. In cases of a closed cervix, a dilator was used for dilation. Precautions were taken to prevent the displacement of the IUD from its fundal position and to avoid entangling the strings in uterine sutures. If the IUD threads protruded through the cervix and caused discomfort, they were trimmed during follow-up. Upon discharge, each patient received a card containing details about the intervention done (date and procedure), the follow-up schedule and investigator contacts. Additionally, they were informed about normal postpartum symptoms, possible complications and side-effects related to IUD insertion, such as abdominal cramps, heavy puerperal bleeding, and expulsion or protrusion of string, and were advised to seek medical assistance by contacting the principal investigator. Patients were also instructed to immediately report any of the following warning symptoms: severe lower abdominal pain, severe vaginal bleeding, infected discharge or lochia, fever, IUD expulsion and suspicion of pregnancy.
Participants randomised for IUD insertion during the post-puerperal period were reassessed at their scheduled postpartum visit to confirm that they met the aforementioned criteria, and IUD placement was carried out during the same visit (n=33).
Haemoglobin levels before insertion had to be >9.5 gm/dL.
The IUD was inserted 6 - 8 weeks after the caesarean delivery (during the post-puerperal visit).
The vaginal speculum was used to expose the cervix and to exclude concomitant infection or bleeding. The anterior lip of the cervix was grasped using ring forceps followed by uterine sounding to assess uterine cavity length. The IUD-loaded sheath applicator (CuT 380 IUD) was introduced gently through the cervical canal and advanced slowly towards the uterine fundus. Once fundal placement was confirmed by abdominal ultrasound, the IUD was released and the sheath was withdrawn, followed by trimming of the IUD string to 1 cm below the level of the cervix.
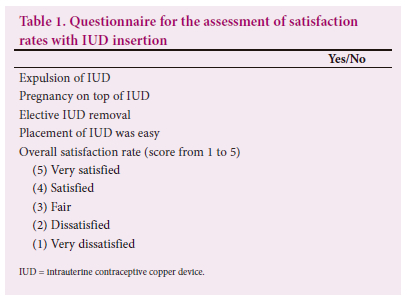
The correct fundal placement was confirmed using the Transvaginal ultrasound. Difficulties in insertion and patient discomfort were recorded. One week post insertion we contacted participants by telephone to enquire about the presence of warning symptoms, such as infected discharge or high-grade fever. Six weeks after insertion we conducted ultrasound and speculum examinations to confirm the correct placement of the IUD. At 3 months after delivery we contacted all participants via phone to schedule an examination and administer a questionnaire (Table 1). The examination included ultrasound and speculum examinations to detect the IUD site and the threads. The questionnaire included the following topics: whether they experienced expulsion, pregnancy, or opted for elective IUD removal, as well as their satisfaction levels with the ease and timing of placement.
The IUDs used were copper based, known by trade names such as Copper T, PREGNA, SILVERLINE and ParaGard. These IUDs have a duration effect of 5 - 12+ years.
Primary outcome
To compare the rate of expulsion between immediate post-placental IUD insertion and standard puerperal IUD insertion (expulsion was determined when the patient gave a history of expulsion, and the IUD was not observed in both ultrasound and pelvic X-ray).
Secondary outcomes
We also investigated the incidence of missed threads (defined as threads not observed via speculum examination), the occurrence of complications, the patient's experience of insertion at the interval and the incidence of pregnancy.
Statistical analysis
Comparisons of numerical variables between the study groups were performed using the Student's t-test for independent samples in comparing two groups when normally distributed and the Mann-Whitney U-test for independent samples when not normally distributed. To compare categorical data, a Chi-square (χ2) test was performed. Fisher's exact test was used instead when the expected frequency was less than five.
A p-value less than 0.05 was considered statistically significant. All statistical analyses were performed using Excel 2007 (Microsoft Corp., USA) and SPSS for Windows (IBM Corp, USA).
Results
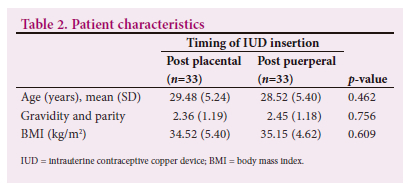
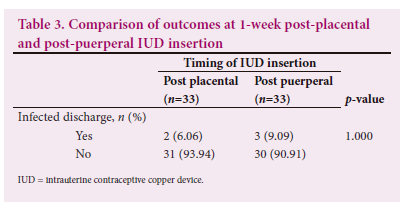
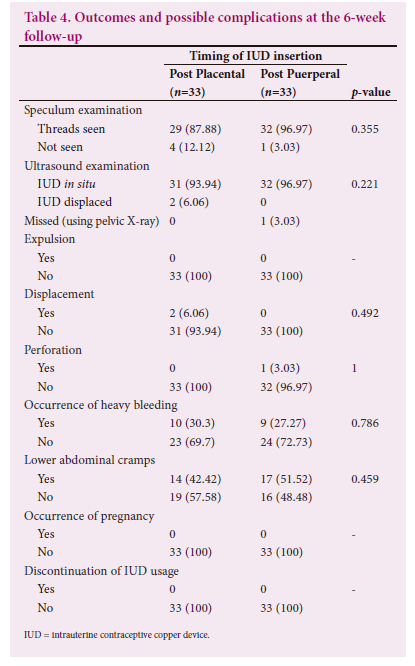
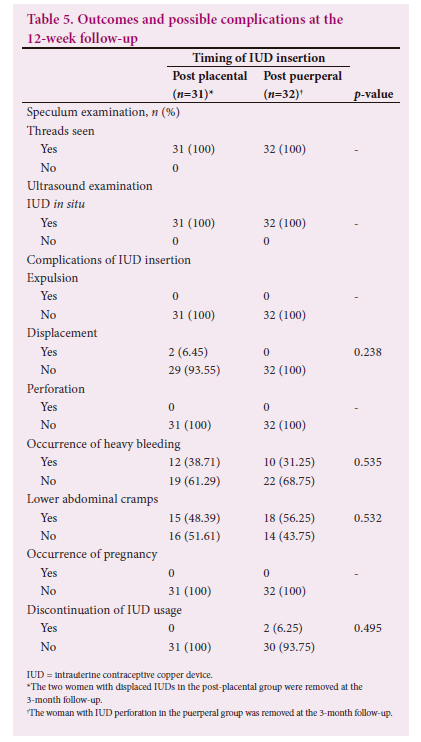
A total of 66 pregnant women aged 20 - 40 years who were scheduled to deliver a live singleton via caesarean section and desiring a copper IUD for postpartum contraception were finally analysed after participation in the current study (Table 2). The participants were randomly dichotomised into two groups of 33. The post-placental group underwent IUD insertion within 10 minutes following placental delivery, whereas the post-puerperal group had an IUD insertion 6 - 8 weeks post delivery. The IUD displacement in the post-placental insertion group was higher than in the interval group (6.06% v. 0%). However, this was not statistically significant (p = 0.49) (Table 3). No case of missed threads was reported by examination either in the post-placental group or in the interval group. Neither expulsion nor perforation was reported in either group at the 6-week follow-up (Table 4). However, at the 12-week follow-up, one case of perforation was reported in the interval group (Table 5).
Discussion
The results of our study show that post-placental IUD insertion is as safe as interval insertion. Different studies with different methodologies have agreed on the safety of post-placental IUD insertion.[6-11] Infection and pelvic inflammatory disease following IUD insertion are very concerning complications, owing to both short- and long-term sequelae. In our study, the occurrence of infected discharge was higher in the interval group compared with the post-placental group 9.1% v. 6.1%; however, this difference was not statistically significant. No case of pelvic inflammatory disease was reported in either group. The results of this study show that the infection risk in the post-placental group was as low as in the interval group. The proper selection of patients and exclusion of those at higher risk of infection, such as those with active gonococcal or chlamydial infection, chorioamnionitis or risk factors for puerperal sepsis, and adherence to antibiotic prophylaxis before skin incision would make the occurrence of such infections in the post-placental IUD insertion group very unlikely. This was corroborated by Welkovic et al.,[9]who reported a low risk of endometritis as long as there was strict adherence to these criteria. To the best of our knowledge, no study has assessed the incidence of infected discharge in the first week following insertion.
One case of uterine perforation occurred during IUD insertion in the interval group, while no such incidences were reported in the post-placental group; however, this was not statistically significant. Uterine perforation was reported to be higher in the interval group in a study by Abd Al Ghany et al.[11] that included 200 patients (100 patients in each arm). They also reported lower failure rates regarding insertion in the post-placental group compared with the interval group. Post-placental IUD insertion requires formal training as interval insertion, and with proper training and supervision, the risk of uterine perforation is as low as interval insertion.[5] Post-placental insertion has the benefit of being inserted into the cavity under direct vision when compared with interval insertion.
Regarding other complications such as heavy bleeding, abdominal cramps and incidence of pregnancy, both groups were comparable. This was in agreement with other studies.[7,9-11]
In our study, no cases of expulsion were reported in either group at the 6 weeks of follow-up. However, two cases in the post-placental group had their IUD displaced by ultrasound examination; this was not of statistical significance. The comparable results between both groups make the post-placental IUD insertion an attractive option. Those results were contradicted by other studies that showed higher expulsion rates in the post-placental group compared with the interval group.[6,11-13] In a study conducted by Bayomui et al.,[13] including 500 patients, the expulsion rates were as high as 13.9% (n=58/416) compared with 1.9% (n=4/214) in the puerperal group. The larger number of participants in their study would explain this difference in the results.
In an updated systematic review by Kapp and Sonalkar,[14] expulsion rates were the same in both groups, which is in agreement with our study. Those findings were supported by a similar study by Abdel Ghany et al.[11] in which both expulsion and displacement rates were again comparable in both post-placental and interval groups (5% v. 2% and 10% v. 5%, respectively).
The discontinuation rate at 3 months was comparable in both groups. Bayoumi et al.[13] in their study showed higher continuation rates for IUD usage at 12 months when compared with the interval group. Celen et al.[15] performed post-placental IUD insertion in 245 women undergoing caesarean section and the continuation rate was as high as 81% and 62% at 6- and 12-month intervals, respectively.
Participants in both groups showed equal satisfaction rates of 4.19 and 4.20, which makes the post-placental approach as convenient as the interval approach.
The strength of our study is that it addressed immediate and short-term complications, and the groups were comparable regarding patient characteristics, thus reducing bias.
The limitation of our study was the small number of participants and the short duration of the follow-up. We recommend that further studies employ a larger sample size and longer duration of up to 12 months.
In conclusion, post-placental IUD insertion is a safe and convenient practice that should be implemented in national family planning programmes, especially in countries with high and rapid population growth. In addition, it is cost-effective[16] and ensures timely delivery of contraception to prevent unintended pregnancies.[5]
Declaration. None.
Acknowledgements. To the hospital staff, residents, nurses and workers who helped us accomplish our work.
Author contributions.
Funding. None
Conflicts of interest. None.
References
1. Ross J, Winfrey W. Contraceptive use, intention to use and unmet need during the extended postpartum period. Int Fam Plann Perspect 2001;27:20-27. [ Links ]
2. Tocce KM, Sheeder JL, Teal SB. Rapid repeat pregnancy in adolescents: do immediate postpartum contraceptive implants make a difference? Am J Obstet Gynecol 2012;206:481.e1-7. [ Links ]
3. Long-acting reversible contraception: implants and intrauterine devices. Practice Bulletin No. 121. American College of Obstetricians and Gynecologists. Obstet Gynecol 2011;118:184-196. [ Links ]
4. Hatcher RA, Trussell J, Nelson AL, Cates WJ, Kowal D, Policar MS. Contraceptive technology. 20th rev. ed. New York (NY): Ardent Media; 2011. [ Links ]
5. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice Long-Acting Reversible Contraception Working Group. Committee Opinion No. 642: increasing access to contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol 2015;126:e44-e48. [ Links ]
6. Royal College of Obstetricians and Gynaecologists. Best Practice in Postpartum Family Planning. Best Practice Paper No. 1. London: RCOG; 2015. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/bpp1/ (accessed June 2023). [ Links ]
7. Sothornwit J, Kaewrudee S, Lumbiganon P, Pattanittum P, Averbach SH. Immediate versus delayed postpartum insertion of contraceptive implant and IUD for contraception. Cochrane Database Syst Rev 2022;10(10):CD011913. doi:10.1002/14651858.CD011913.pub3 [ Links ]
8. Jatlaoui TC, Whiteman MK, Jeng G, et al. Intrauterine device expulsion after postpartum placement, A Systematic Review and Meta-analysis. Obstet Gynecol 2018;132(4):895-905. https://doi.org/10.1097/AOG.0000000000002822 [ Links ]
9. Welkovic S, Costa LO, Faundes A, deAlencar Ximenes R, Costa CF. Post-partum bleeding and infection after post-placental IUD insertion. Contraception 2001;63:155-158. [ Links ]
10. Bhutta SZ, Butt IJ, Bano K. Insertion of intrauterine contraceptive device at caesarean section. J Coll Physicians Surg Pak 2011;21:527-530. [ Links ]
11. 1Abdel-Ghany A, Khalifa E, El-Din MZ, et al. Intrapartum versus postpartum insertion of intrauterine device in women delivering by cesarean section. BMC Pregnancy Childbirth 2022;22(1):365. https://doi.org/10.1186/s12884-022-04681-4 [ Links ]
12. Rosa Bolling K, Wahdan Y, Warnock N, et al. Utilisation, effectiveness, and safety of immediate postpartum intrauterine device insertion: a systematic literature review. BMJ Sex Reprod Health 2023;49(2):e1. https://doi.org/10.1136/bmjsrh-2022-201579 [ Links ]
13. Bayoumi YA, Dakhly DMR, Bassiouny YA, Gouda HM, Hassan MA, Hassan AA. Post-placental intrauterine device insertion vs puerperal insertion in women undergoing caesarean delivery in Egypt: a 1 year randomised controlled trial. Eur J Contracept Reprod Health Care 2020;25(6):439-444. https://doi.org/10.1080/13625187.2020.1823366 [ Links ]
14. Sonalkar S, Kapp N. Intrauterine device insertion in the postpartum period: a systematic review. Eur J Contracept Reprod Health Care 2015;20:4-18. https://doi.org/10.3109/13625187.2014.971454 [ Links ]
15. Çelen Ş, Sucak A, Yildiz Y, Danişman N. Immediate postplacental insertion of an intrauterine contraceptive device during cesarean section. Contraception 2011;84:240-243. https://doi/10.1016/j.contraception.2011.01.006 [ Links ]
16. Washington CI, Jamshidi R, Thung SF, Nayeri UA, Caughey AB, Werner EF. Timing of postpartum intrauterine device placement: a cost-effectiveness analysis. Fertil Steril 2015;103:131-137. https://doi/10.1016/j.fertnstert.2014.09.032 [ Links ]
 Correspondence:
Correspondence:
MAR Moussa
dr.manal959@hotmail.com
Accepted 25 September 2023














