Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Obstetrics and Gynaecology
On-line version ISSN 2305-8862
Print version ISSN 0038-2329
SAJOG vol.29 n.1 Cape Town May. 2023
http://dx.doi.org/10.7196/SAJOG.2023.v29i1.170
RESEARCH
The association of fetal macrosomia and neonatal hypoglycaemia
TR MoodleyI; NR MaharajII, III; J MoodleyIV
IBSc, MB ChB, FCOG (SA), MMed; Department of Obstetrics and Gynaecology, Prince Mshiyeni Memorial Hospital, Umlazi, Durban, South Africa
IIMB ChB, FCOG (SA), MMed, PhD; Department of Obstetrics and Gynaecology, Prince Mshiyeni Memorial Hospital, Umlazi, Durban, South Africa
IIIMB ChB, FCOG (SA), MMed, PhD; Department of Obstetrics and Gynaecology, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IVMB ChB, FRCOG, MD; Department of Obstetrics and Gynaecology, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: The clinical management of fetal macrosomia in pregnant women poses a challenge for obstetricians globally. This has become increasingly important in recent times due to the rising incidence of this condition and its associated risks to both the mother and infant, including birth injuries and neonatal hypoglycaemia.
OBJECTIVE: To investigate the association between neonatal hypoglycaemia and fetal macrosomia in a cohort of South African black non-diabetic women.
METHODS: This retrospective study analysed the clinical outcomes of 415 macrosomic babies born to non-diabetic women between 2015 and 2016 at a regional hospital in Durban, South Africa.
RESULTS: Of the 415 macrosomic babies, 52 had hypoglycaemia (<2.6 mmol/L). The prevalence rate of neonatal hypoglycaemia was therefore 12.53%.
CONCLUSION: Neonatal hypoglycaemia is a common complication in babies with macrosomia born to black non-diabetic South African pregnant women.
Fetal macrosomia, defined as a birthweight >4 000 g, is associated with significant maternal and fetal complications.[1] The incidence of fetal macrosomia is increasing and is estimated to affect 3 - 15% of all pregnancies.[2] The risk factors for fetal macrosomia include genetics, postdate pregnancies, high body mass index (BMI), previous fetal macrosomia, excessive weight gain in pregnancy and gestational diabetes.[3] Although fetal macrosomia is difficult to predict, these aforementioned risk factors can help make a timely diagnosis. In addition, the mode of childbirth affects fetal outcomes, with caesarean delivery appearing to positively impact fetal outcomes by reducing both maternal and perinatal morbidity.[4]
Neonatal hypoglycaemia commonly occurs in macrosomic babies born to non-diabetic mothers.[4] The risk of neonatal hypoglycaemia also increases with increasing birthweight.[5] Neonates with a birthweight >4 500 g have a 7-fold higher risk of hypoglycaemia compared with those with a weight appropriate for gestational age.[6] This risk increases further in the presence of gestational diabetes.[6]
Neonatal hypoglycaemia can be asymptomatic or symptomatic. Symptoms may include tachypnoea, apnoea, tremors, sweating, irritability, and seizures, emphasising the need for post-delivery glucose monitoring.[7]
The severity of neonatal hypoglycaemia is related to the duration of hypoglycaemia.[7] Severe glucose deficiency can result in cerebral energy failure, impaired cardiac performance, muscle weakness, glycogen depletion and diminished glucose production. Thus, ensuring a continuous supply of glucose to all organs is an essential physiological function.
Low Apgar scores are also associated with fetal macrosomia, with a higher risk linked to greater birthweight.[8] According to Boulet et al.,[8] the odds ratio (OR) for a 5-minute Apgar score <6 was 1.65 more likely for infants with birthweights between 4 500 g and 4 999 g, and 3.49 for those exceeding 5 000 g. The odds of a 5-minute Apgar score <3 was even higher, with corresponding ORs of 2.01 and 5.20, respectively.
The odds of perinatal asphyxia have also been shown to rise with an increase in birthweight. Specifically, the risk for perinatal asphyxia is 2.4 times higher in infants with macrosomia compared to those with normal birthweights.[9] In a study by Yu et al.[10] the OR was 2.3 for birthweights between 4 500 and 4 999 g and increased to 10.5 for birthweights >5 000 g.
Methods
This was a retrospective chart review of 415 fetal macrosomia babies born between 2015 and 2016 at a regional hospital in Durban, South Africa. Ethical clearance was obtained from the UKZN Biomedical Research Ethics Committee (ref. no. BREC168/17). Babies with a birthweight >4 kg were included in the study. Demographic data as well as maternal and fetal outcomes were analysed. The individual neonatal data was extracted from paediatric summaries recorded at birth. Fetal blood sugar monitoring was performed 6-hourly for 24 hours on babies diagnosed as having macrosomia. The data were analysed using SPSS software version 25.0 (IBM Corp., USA).
Results
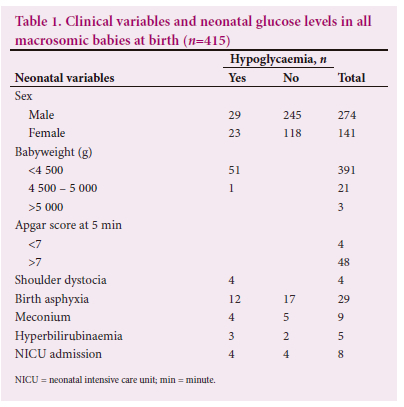
Table 1 shows the neonatal variables. Among the 415 babies with macrosomia, 66% were male and 33.97% were female. Of those, 52 (12.53%) were diagnosed with neonatal hypoglycaemia, consisting of 29 male and 23 female babies. Notably, the group with birthweights <4 500 g had the highest number of babies with a diagnosis of neonatal hypoglycaemia, totalling 51 (98%). Other fetal macrosomia-related complications included shoulder dystocia (n=4), birth asphyxia (n=12), meconium aspiration (n=4) and hyperbilirubinaemia (n=4). Regarding mode of delivery and hypoglycaemia, 28 pregnant women had caesarean deliveries and 24 delivered vaginally (Table 3). Planned caesarean delivery was associated with the lowest number of hypoglycaemic cases (n=4), compared with vaginal delivery. The emergency caesarean delivery group showed an even distribution, with 24 babies experiencing hypoglycaemia in each category (vaginal delivery, elective caesarean delivery, emergency caesarean delivery). The Apgar score at 1 minute was <7 for 10 babies in the vaginal delivery group, which was higher than that in the emergency caesarean delivery group (n=4). Birth asphyxia was highest in the emergency caesarean delivery group (n=22), while the vaginal delivery group had seven babies with asphyxia.
Meconium aspiration after caesarean delivery occurred in six cases, compared to three cases in the normal vaginal delivery group. Among mothers aged 20 - 34 years, 45 cases of hypoglycaemia (86.53%) were identified (Table 2).
Discussion
In our study, regarding the mode of delivery and hypoglycaemia, 28 women had caesarean deliveries (11.91%) and 24 delivered vaginally (13.33%). The incidence of neonatal hypoglycaemia was 12.5%. Existing literature reports varying findings, with Oral et al.[7]citing 23.5%, Cheng. et al.[8] reported 2.4%, Salim et al.[10]reported 22.8% and Ochoga et al.[11]found 11%. Ogunlesi[12] quoted figures for hypoglycaemia of 27.3%, while other authors noted percentages of 28.3%,[13] 30.5%,[14] and 41%.[15] The risk of neonatal hypoglycaemia was found to be higher in babies who weigh more, particularly those over 4 kg.[16]
In our study, the group with a birthweight ranging from 4 000 g to 4 500 g had a 98.1% incidence of neonatal hypoglycaemia (n=51). It is concerning that neonatal hypoglycaemia was a more frequent finding in babies born to non-diabetic mothers. It has been shown that infants with a birthweight >4 000 g delivered by non-diabetic mothers had a 2.4% risk of neonatal hypoglycaemia, whereas those with gestational diabetes had an incidence of 5.3%.[12] Hypoglycaemia was significantly associated with neonates with macrosomia born of non-diabetic mothers when compared with neonates with normal birthweight, and those with low birthweight, as reported by Efe et al.[13]Fetal macrosomia is a recognised cause of transient hypoglycaemia.[10] Efe et al.[13]stated that neonates with feeding intolerance were more likely to present with hypoglycaemia compared with those tolerating feeds. This finding is consistent with the report by Dedeke et al.[14]
In comparison to other studies, Hassan et al.[16]and Abassia et al. [17] both reported a high incidence of hypoglycaemia at 78% in the birthweight category of 4 - 5 kg. Neonates with a birthweight >4 500 g had a 7-fold higher risk of having neonatal hypoglycaemia, compared with those of appropriate gestational age, as demonstrated by Weissmann-Brenner.[17] Similarly, another study found a 2-fold increase in the rate of neonatal hypoglycaemia in macrosomic pregnancies.[18] Another study showed a 1.5-fold increase in the frequency of neonatal hypoglycaemia with increasing birthweight, with a rate of 14% in the 4 - 5 kg category, compared with 22% in those with birthweights >5 kg.[20]
In our study, hypoglycaemia was more common in male babies (56%, n=29) compared with female babies (44%, n=23) and, of the 415 macrosomic babies, 274 (66%) were male and 141 (34%) were female. In the literature, male dominance in the incidence of hypoglycaemia amongst fetal macrosomia babies was also confirmed by Hasan et al.,[20] with a male: female ratio of 1.6:1 (59%). Similar findings were reported by Cornblauth et al.[21]
In the present study, hypoglycaemia was prevalent in both modes of delivery. Emergency caesarean deliveries accounted for 24 cases (46%), there were 4 elective caesareans, and 24 normal vaginal deliveries. Modes of delivery had no association with neonatal hypoglycaemia.[13,16] Our cohort of elective caesarean delivery only had four hypoglycaemic neonates, which was low in comparison to the 24 cases in the emergency caesarean delivery group and 24 in the normal vaginal delivery group. Macrosomia has been associated with an increased caesarean delivery rate.[22] In our study, the caesarean delivery rate was 57% (n=235) for babies with macrosomia. Among these, 30 babies had hypoglycaemia. In contrast, in the vaginal delivery group (n=180 babies), 22 had hypoglycaemia.
A study in the US found a higher neonatal hypoglycaemia prevalence among large gestational-age neonates when compared with small gestational-age neonates.[23] Macrosomic neonates born to non-diabetic mothers have been shown to exhibit hyperplasia of the islet cells of the pancreas. The reason for this is unclear, but it is distinct to abnormally elevated levels of glucose in utero, as seen in infants born to diabetic mothers.[24] Macrosomic babies of non-diabetic mothers have hyperinsulinaemia at birth when compared with non-macrosomic babies.[24' Severance of the placental blood supply at birth likely leads to rapid development of hypoglycaemia due to hyperinsulinaemia.
Neonatal glucose reserves are rapidly depleted during feeding challenges because of the limited capacity to store glucose.[24] The above reasons underscore the importance of early and frequent breastfeeding as recommended by UNICEF and the World Health Organization in the Baby Friendly Hospital Initiative.[25]
In our study, other fetal complications associated with hypoglycaemia were birth asphyxia (12/29), meconium-stained liquor (4/9), and hyperbilirubinaemia (3/5). Birth asphyxia and meconium aspiration accounted for (16/52) of hypoglycaemia cases. Four hypoglycaemic babies required neonatal intensive care; however, there was no neonatal mortality, in our study. Hypoglycaemia is a significant cause of neonatal mortality as demonstrated by West et al.,[20] in their study, which reported a rate of 4.2%. Other studies by Dedeke et al.[14] have cited figures as high as 23.3%.
Glucose monitoring of macrosomic babies within the first 24 hours following birth is essential to prevent neonatal morbidity and mortality. In our study, maternal BMI seemed to be the strongest predictor of fetal macrosomia compared with other risk factors. All infants with birthweights >4 kg required admission to the nursery to monitor their blood glucose levels, as they constitute a vulnerable group for hypoglycaemia. As such, we advocated for routine blood glucose screening of macrosomic babies upon admission to neonatal units to enable early detection and prompt treatment of hypoglycaemia.
Declaration. None
Acknowledgements. None
Author contributions. None
Funding. None
Conflicts of interest. None
References
1. Turkmen S, Johansson S, Dahmoun M. Foetal Macrosomia and Fetal-Maternal Outcomes at Birth. J Pregnancy 2018;4790136. https://doi.org/10.1155/2018/4790136 [ Links ]
2. Mohammadbeigi A, Farhadifar F, Soufi Z. Fetal Macrosomia: Risk Factors, Maternal, and Perinatal Outcome. Ann Med Health Sci Res 2013;3(4):546-50. https://doi:10.4103/2141-9248.122098 [ Links ]
3. Nahavandi S, Seah JM, Shub A, Houlihan C, Ekinci EI. Biomarkers for Macrosomia Prediction in Pregnancies Affected by Diabetes. Front Endocrinol (Lausanne) 2018; 9:407. https:/doi:10.3389/fendo.2018.00407 [ Links ]
4. Fanaroff AA, Stoll BJ, Wright LL, et al. Trends in Neonatal Morbidity and Mortality for very low birthweight infants. Am J Obstet Gynecol 2007;196:147e1-8. https:/doi:10.1016/j.ajog.2006.09.014. [ Links ]
5. Hawdon JM. Best Practice Guidelines: Neonatal Hypoglycaemia. Early Hum Dev 2010;86(5):261. https://doi:10.1016/j.earlhumdev.2010.05.007 [ Links ]
6. Zhang X, Decker A, Platt RW, Kramer MS. How big is too big? The perinatal consequences of fetal macrosomia. Am J Obstet Gynecol 2008 May;198(5):517.e1-6. https://doi:10.1016/j.ajog.2007.12.005 [ Links ]
7. Oral E, Cagdas A, Gezer A, Kaleli S, Aydinli K, Ocer F. Perinatal and maternal outcomes of fetal macrosomia. Eur J Obstet Gynecol Reprod Biol 2001;99:167-171. [ Links ]
8. Cheng YK, Lao T. Fetal and maternal complications in macrosomic pregnancies. Res Rep Neonatol 2014;4:65-70. https://doi.org/10.2147/RRN.S39110 [ Links ]
9. Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X. Pre-pregnancy body mass index in relation to infant birthweight and offspring overweight/obesity. A systematic review and meta-analysis. PLoS One 2013;16;8(4);e61627. https://doi:10.1371/journalpone.0061627. Print 2013 [ Links ]
10. Said AS, Manji KP. Risk factors and outcomes of fetal macrosomia in a tertiary centre in Tanzania: a case control study. BMC Pregnancy and Childbirth 2016;16:243. https://doi:10.1186/s12884-016-1044-3 [ Links ]
11. Ochoga MO, Aondoaseer M, Abah RO. Prevalence of Hypoglycaemia. Open J Paediatric 2018;8. https://doi:189-198.10.4236/ojped.2018.82021 [ Links ]
12. Ogunlesi T. The role of significant hypothermia and hypoglycaemia. Iran J Neonatol 2015;6(1):1-7. [ Links ]
13. Efe A, Sunday O, Surajudeen B, Yusuf T. Neonatal Hypoglycaemia: Prevalence and clinical Outcome in a tertiary health facility in North-central Nigeria. Int J Health Sci Res 2019;9:246-51. https:/www.ijhsr.org/IJHSR_VoL9_Issue.6_Iune2019/IJHSR_Abstract.034.html [ Links ]
14. Dedeke IO, Okeniyi JA, Owa JA, Oyedeji GA. Point-of-admission neonatal hypoglycaemia in a Nigerian tertiary hospital: incidence, risk factors and outcome. Nig J Paediatric 2011;38(2):90-4. https://doi:10.4314/njp.v38i2.72252 [ Links ]
15. Esakoff TF, Cheng YW, Sparks TN, Caughey AB. The association between birthweight 4000g or greater and perinatal outcomes in patients with and without gestational diabetes mellitus. Am J Obstet Gynecol 2009; 200(6);672. https://doi.org/10.1016/j.ajog.2009.02.035 [ Links ]
16. Hasan S, Alatwani A. The Frequency of Hypoglycaemia in Macrosomic Neonates in Amarah. [ Links ]
17. Weissmann-Brenner A, Simchen MJ, Zilberberg E, Kalter A, Weisz B, Achiron R, Dulitzky M. Maternal and neonatal outcomes of macrosomic pregnancies. Med Sci Monit. 2012;18(9):PH77-81. https://doi:10.12659/msm.883340 [ Links ]
18. Akin Y, Comert S, Turan C, Picak A, Agzikuru T, Telatar B. Macrosomic newborns: A 3-year review. Turk J Pediatr 2010;52(4):378-83. https://pubmed.ncbi.nlm.nih.gov/21043383/ [ Links ]
19. Hedderson MM, Weiss NS, Sacks DA, Pettitt DJ, Selby JV, Quesenberry CP, Ferrara A. Pregnancy weight gain and risk of neonatal complications. Obstet Gynecol 2006; 108: 1153-61. https://doi:10.1097/01.AOG.0000242568.75785.68. [ Links ]
20. West BA, Aitafo JE. Prevalence and Clinical Outcome of Inborn neonates with hypoglycaemia in Rivers State University Teaching Hospital, Nigeria. J. Perinatol Child Health 2020:4(4):137-148. [ Links ]
21. Cornblauth M, Ichord R. Hypoglycaemia in the neonate. Semin. Perinatal 2000 [ Links ]
22. Li G, Kong L, Li Z, et al. Prevalence of macrosomia and its risk factors in China: A Multicentre survey based on birth data involving singleton term infants. Paediatr Perinat Epidemiol 2014;28(4):345-50. https://doi:10.1111/ppe.12133 [ Links ]
23. Adamkin DH. Metabolic screening and postnatal glucose homeostasis in newborn. Pediatr Clin North Am 2015;62:385-409. [ Links ]
24. Mai AH, Abassia D. The prevalence of Fetal Macrosomia. J Nutr Food Sci 2014;4:3. https://doi:10.1016/j.pcl.2014.11.004 [ Links ]
25. Magadla Y, Velaphi S, Moosa F. Incidence of hypoglycaemia in late preterm and term infants born to women with diabetes mellitus. SAJCH 2019;13(2):78-83. https://hdl.handle.net/10520/EJC-18a66a61c0 [ Links ]
26. World Health Organization. Nutrition: Ten steps to successful breastfeeding 2018 [ Links ]
 Correspondence:
Correspondence:
J Moodley
jmog@ukzn.ac.za
Accepted 1 October 2023














