Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Obstetrics and Gynaecology
versão On-line ISSN 2305-8862
versão impressa ISSN 0038-2329
SAJOG vol.29 no.1 Cape Town Mai. 2023
http://dx.doi.org/10.7196/SAJOG.2023.v29i1.2110
RESEARCH
Post-caesarean section outcomes of obstetric patients with valvular heart disease at Charlotte Maxeke Johannesburg Academic Hospital, South Africa
Z MfekaI; A NkunaII; P Motshabi ChakaneIII
IMB ChB; Department of Anaesthesia, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
IIMMed (Anaesth); Department of Anaesthesia, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
IIIFCA (SA), PhD Department of Anaesthesia, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand and Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Valvular heart disease presents a unique set of conditions during pregnancy and delivery, with the potential for adverse outcomes increased by prior interventions and anticoagulation.
OBJECTIVES. To describe the profile and outcomes of obstetric patients with valvular heart disease who delivered via caesarean section at Charlotte Maxeke Johannesburg Academic Hospital, South Africa.
METHODS. A 5-year retrospective descriptive cross-sectional study was performed. All patients with valvular heart disease who underwent caesarean section, irrespective of age, were included. Exclusion criteria were absence of important clinical data relevant to the study and outcomes data. All records of patients who delivered by caesarean section and were booked in the obstetric cardiac unit were reviewed. Data for those who had valvular heart disease were separated from non-valvular heart disease data. A total of 69 patients were included in the analysis. Univariate logistic regression analysis was done to assess the predictors of maternal and fetal outcomes.
RESULTS. The mean (standard deviation) age of the patients in the study was 30.1 (5.6) years, 82.6% were gravida 1 - 3 and 89.8% para 0 - 2, and the majority (56.5%) had an elective caesarean section. General anaesthesia was the most common mode used, and most of the patients had fixed-interval analgesia postoperatively. Approximately two-fifths of the patients (n=28; 40.6%) were on anticoagulants. A significantly higher percentage of those who were on anticoagulants had complications (n=12/28; 42.9%) compared with those who were not on anticoagulants (n=3/41; 7.3%) (p<0.001). There was a total of 19 complications, mainly bleeding (n=7) and cardiac arrhythmias (n=6). New York Heart Association class and use of anticoagulants were individually associated with adverse maternal outcomes after univariable logistic regression analysis (p=0.006 and p=0.017, respectively). In univariable logistic regression analysis, a low ejection fraction was associated with adverse fetal outcome (odds ratio 0.94; 95% confidence interval 0.90 - 0.99; p=0.032). One infant (1.4%) died, in the early neonatal period.
CONCLUSION. Pregnancy in women with cardiac disease is possible, but it is not without risk, and a structured plan and multidisciplinary team approach to provide prehabilitation is therefore necessary. Our patients were young and with relatively good functional status (metabolic equivalent >4), and most pregnancies continued to term or early term (median (interquartile range) 37 (36 - 38) weeks). Some patients experienced adverse outcomes, mainly related to bleeding and arrhythmias, but none died. There was one early neonatal death. These patients need a structured multidisciplinary team care plan.
The incidence of cardiac disease in pregnancy is estimated to be in the range of 1 - 1.5%.[1,2] Cardiac disease represents a significant cause of poor maternal and fetal outcome in pregnancy.[2,3] Valvular heart disease related to rheumatic fever has declined in high-income countries, but remains a significant health problem in low-income countries.[2,4] It affects the heart and the body's ability to adapt to the normal physiological changes of pregnancy[5,6] and also often exacerbates the physiological changes of pregnancy, with many patients being diagnosed with valvular heart disease for the first time during their pregnancy.[7-9] Associated complications include thromboembolism, cardiac arrhythmias, pulmonary oedema, and bleeding after caesarean section due to the use of anticoagulation.[2,10,11] Valvular heart disease has adverse effects on fetal outcome and can result in preterm birth, respiratory distress, low birthweight even at term (although no distinction between small for gestational age and fetal growth restriction could be made), increased resuscitation rates in severely preterm babies, and fetal or neonatal death.[11,12] A multidisciplinary team approach is essential to ensure that the mother and the baby can cope with the challenges of pregnancy and delivery, and survive the postpartum period and beyond.[4,13]
Data on outcomes after caesarean section in women with valvular heart disease in sub-Saharan Africa are scarce. Knowledge about the perioperative course of these patients is necessary for the development of protocols to assist with management in our resource-limited settings. This study aimed to evaluate maternal perioperative outcomes, namely cardiac failure, pulmonary oedema and embolism, haemorrhage, atrial fibrillation and mortality. Fetal outcomes such as low birthweight, preterm birth, respiratory distress and death were also included.
Methods
This was a retrospective descriptive cross-sectional study in the Department of Anaesthesia at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), South Africa (SA). All patients with valvular heart disease who underwent caesarean section, irrespective of age, were included. Exclusion criteria were absence of essential clinical and outcomes data. All records of patients who delivered by caesarean section and were booked in the obstetric cardiac unit were reviewed over a period of 5 years by the primary investigator (ZM). Files of those who had valvular heart disease were separated from non-valvular heart disease patients. Data (anaesthetic charts, patient files and echocardiographic reports) for 69 patients with valvular heart disease who delivered by caesarean section over a period of 5 years from January 2016 to December 2020 were included. Adverse maternal outcomes were defined as the presence of any of the following: bleeding, cardiac arrhythmias, cardiac failure, pulmonary oedema, thromboembolic events and in-hospital death, and adverse neonatal outcomes as preterm birth, low birthweight, fetal respiratory distress and death.
Permission to perform the study was obtained from CMJAH, and ethics approval was obtained from the Human Research Ethics Committee of the University of the Witwatersrand (ref. no. M200751) before proceeding with the research. Patient information was de-identified and confidentiality was maintained.
Statistical analysis
Data were collected on an Excel spreadsheet (Microsoft Corp., USA). Frequencies and percentages were used to describe demographic data. Clinical and outcomes data were reported as means with standard deviations (SDs) if normally distributed and as medians with interquartile ranges (IQRs) if not normally distributed. Associations between patient characteristics and outcomes were determined using Fisher's exact test or the Wilcoxon rank-sum test, depending on the data distribution. Univariate logistic regression analysis was done to assess the predictors of maternal and fetal outcomes. Factors with a p-value <0.1 were included in a multivariable regression analysis model. A p-value <0.05 was accepted as statistically significant.
Results
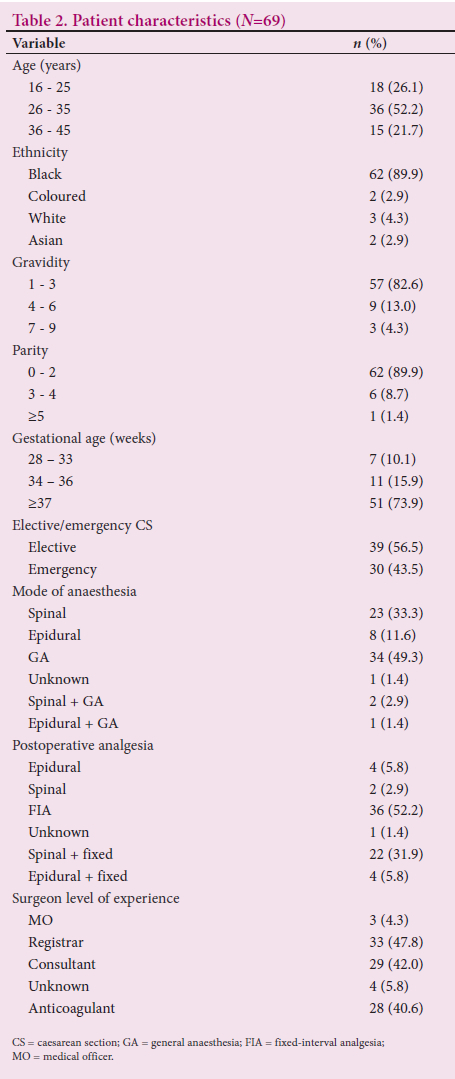
A total of 69 records were analysed from all files collected during the study period, and none were excluded. The valve lesions ranged from isolated mitral, tricuspid, pulmonary and aortic valves to mixed valve lesions (Table 1). Patients had their caesarean section under regional anaesthesia (spinal/epidural), general anaesthesia (the most commonly used mode) or a combined technique (Table 2). The mean (SD) age of the patients was 30.1 (5.6) years, with a range of 18 - 41 years, and 89.9% (n=62) were black. A total of 82.6% were gravida 1 -3 and 89.8% were para 0 - 2. Most neonates (75.4%) were born at term or early term, with a median (IQR) gestation of 37 (36 - 38) weeks. The majority of the patients (56.5%) had an elective caesarean section, with 43.5% having an emergency caesarean section, and the majority had fixed-interval analgesia (FIA) postoperatively. Mitral valve disease accounted for most of the lesions, tricuspid valve disease was the least reported, and 40.6% of the patients were on anticoagulants. Cardiac arrhythmias and mechanical valves were the reasons noted for the use of anticoagulation in some of these patients. All the patients were on enoxaparin, some having been changed from warfarin in early pregnancy, probably because warfarin is teratogenic.
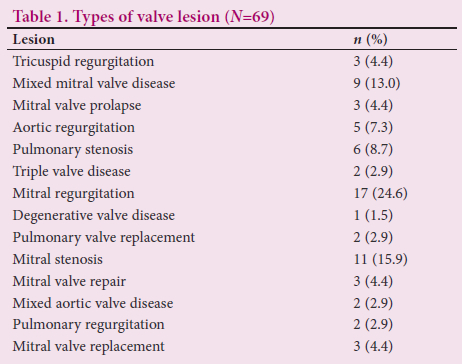
Most of the patients (62.3%) had mild to moderate valvular disease, only 26.1% presenting with severe disease (Table 3). The cause of the valvular heart disease was mainly rheumatic, as opposed to congenital pathology (75.4% v. 24.6%, respectively).
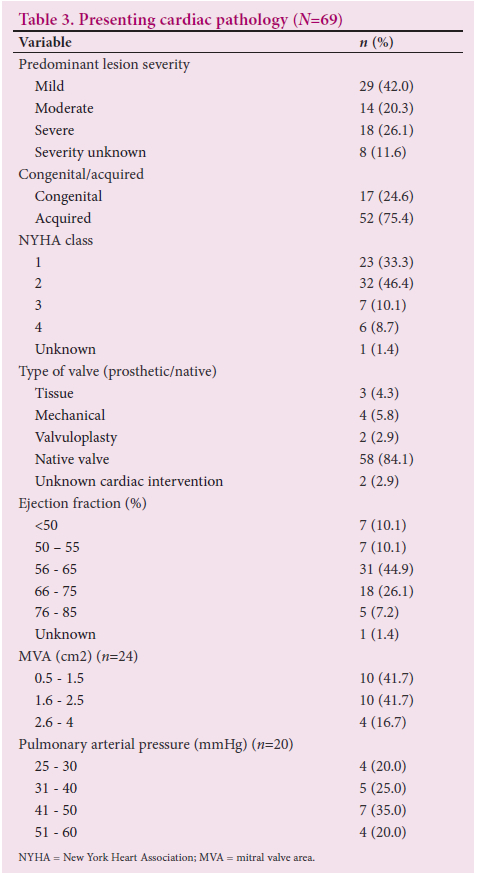
Of the patients, 79.7% fell into New York Heart Association (NYHA) classes 1 and 2. Records showed that 58 (84.1%) of the patients had not had any surgical intervention for their cardiac lesion prior to the caesarean section, with only 11 (15.9%) having had a surgical intervention such as valvuloplasty, valve repair or valve replacement. The mitral valve was the commonest valve to have been replaced in this study, followed by the aortic valve (n=3; 27.3% and n=1; 9.1%, respectively). Of 24 patients with mitral valve disease who had echocardiography reports, 10 (41.7%) had a mitral valve area <1.5 cm2.
There was a total of 19 complications, mainly bleeding (n=7) and cardiac arrhythmias (n=6), with rates of 10.1% and 8.7% of the total number of patients, respectively (Table 4). Some patients had more than one complication. The majority of those who bled were on anticoagulants (n=6/7; 85.7%). Nineteen patients (27.5%) were cared for in an intensive care unit (ICU) postoperatively, 35 (50.7%) were in high care, and 15 (22.4%) were in the general ward. No patient died in hospital. The majority of the infants (68.1%) weighed >2 500 g at birth (Table 4). Fourteen infants (20.3%) had respiratory distress at birth and 1 infant (1.4%) died, in the early neonatal period.
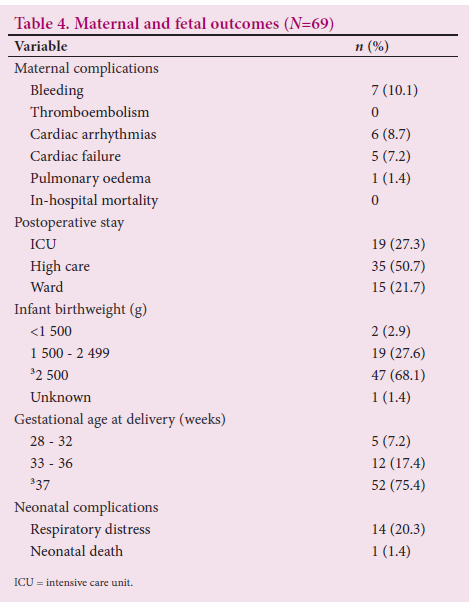
There was a significant univariable association between both NYHA class and patients who were on anticoagulants and adverse maternal outcome (odds ratio (OR) 3.22; 95% confidence interval (CI) 1.56 - 6.66; p=0.002 and OR 0.075; 95% CI 0.026 - 0.42; p=0.002, respectively). Both NYHA class and anticoagulation remained significant in an adjusted model (adjusted odds ratio (aOR) 3.77; 95% CI 1.45 - 9.79; p=0.006 and aOR 0.11; 95% CI 0.018 - 0.67; p=0.017, respectively). A low ejection fraction (EF) was the only factor univariably associated with adverse fetal outcome (OR 0.94; 95% CI 0.90 - 0.99; p=0.032) (Fig. 1).
The main method of postoperative analgesia used was FIA (52.2%). Significantly more patients operated on by consultants had poor outcomes (37.9%) compared with those operated on by registrars (9.1%) (p=0.035). The majority of the patients (49.3%) had a general anaesthetic; however, there was no significant relationship between the mode of anaesthesia and poor maternal outcomes (p>0.1).
Discussion
The patients in our study were relatively young, with a mean age of 30.1 years. The majority were black, gravidity and parity were low, and the majority of the pregnancies reached term or early term. A high proportion of the patients were in NYHA classes 1 and 2, with mild
to moderate disease. Symptoms of valvular heart disease are often unmasked during pregnancy because of the physiological changes that take place.[7-9] Higher NYHA classes were associated with adverse maternal outcome, whereas low EFs adversely affected fetal outcome. However, the majority of our patients (n=62/69; 89.9%) had normal EFs, making the extrapolation difficult. Similar to our outcomes, it has been shown by others that severity of maternal disease affects fetal outcome.[1] In obstetric patients with heart disease, high NYHA class has been shown to be associated with the highest risk of maternal and fetal morbidity and mortality.[14,15]
Of concern in the present study was that the majority of the patients were not on anticoagulants despite having valvular heart disease and cardiac arrhythmias. However, the main complication was postoperative haemorrhage, associated mostly with those on anticoagulation, as 85.7% of the women who bled were on anticoagulants. Most of the patients were cared for in an ICU or high-care unit. The cardiac lesions were mainly acquired as opposed to congenital, reflecting the ongoing presence of rheumatic heart disease in our communities.
The majority of the patients in this study (n=58/69; 84.1%) had had no cardiac surgical intervention prior to this pregnancy, possibly because many had only been diagnosed with cardiac pathology during their pregnancy. This finding may be attributable to limitations in access to healthcare services in SA, similar to the situation reported in other low- to middle-income (LMIC) countries.[1,12] The main lesion in the present study was mitral valve disease; this is most common in rheumatic heart disease, which predominantly affects the mitral valve.[4] Of 24 patients with mitral valve disease who had an echocardiography report, 10 (41.7%) had a mitral valve area <1.5 cm2. Among those with mitral stenosis (n=11), 7 (63.6%) had critical stenosis. Of the 20 patients with pulmonary hypertension (PHT), 2 (10.0%) had severe PHT.
Complications such as postpartum haemorrhage and cardiac arrhythmias have been reported in previous studies.[10,12] The type of anaesthetic, timing of surgery (gestational age at caesarean section), whether the procedure was an emergency, parity and gravidity seemed to have no bearing on maternal outcomes. The choice of regional or general anaesthesia is often determined with the patient's haemodynamic stability in mind and the goals associated with each valve lesion.[10,16] Most of the women in this study had mild to moderate cardiac disease, with good EFs and good NYHA functional status, and received general anaesthesia.
Significantly more patients operated on by consultants had poor outcomes such as bleeding, arrhythmias, pulmonary oedema and cardiac failure compared with those operated on by registrars, possibly because the consultants operated on more complex cases. Bleeding was probably due to anticoagulation, as 6 out of the 7 women who bled were on anticoagulants.
Study strengths and limitations
There is a paucity of literature on this important subject, and the present study adds a crucial body of data, particularly in our LMIC setting. Our cohort over 5 years was small, and data therefore cannot be extrapolated to the whole population.
Conclusion
It is evident that our patients were young, and in relatively good functional status considering their valve lesions. Some patients experienced adverse outcomes, mainly related to bleeding and arrhythmias, but none died. As healthcare has improved, many women with cardiac disease, including those with congenital cardiac lesions, now reach reproductive age. A multidisciplinary structured care plan is therefore crucial to improve maternal and neonatal outcomes.
Declaration. The research for this study was done in partial fulfilment of the requirements for ZM's MMed (Anaesth) degree at the University of the Witwatersrand.
Acknowledgements. The authors thank Dr H Remtula for his assistance with data availability.
Author contributions. All authors contributed equally to the preparation of the manuscript. The study data are available from the corresponding author (PMC) on reasonable request.
Funding. None.
Conflicts of interest. None.
References
1. Sawhney H, Aggarwal N, Suri V, Vasishta K, Sharma Y Grover A. Maternal and perinatal outcome in rheumatic heart disease. Int J Gynaecol Obstet 2003;80(1):9-14. https://doi.org/10.1016/s0020-7292(02)00029-2 [ Links ]
2. Abdel-Hady ES, El-Shamy M, El-Rifai AA, Goda H, Abdel-Samad A, Moussa S. Maternal and perinatal outcome of pregnancies complicated by cardiac disease. Int J Gynaecol Obstet 2005;90(1):21-25. https://doi.org/10.1016/j.ijgo.2005.03.008 [ Links ]
3. Luthra A, Bajaj R, Jafra A, Jangra K, Arya VK. Anesthesia in pregnancy with heart disease. Saudi J Anaesth 2017;11(4):454-471. https://doi.org/10.4103/sja.SJA_277_17 [ Links ]
4. Sartain JB, Anderson NL, Barry JJ, Boyd PT, Howat PW. Rheumatic heart disease in pregnancy: Cardiac and obstetric outcomes. Int Med J 2012;42(9):978-984. https://doi.org/10.1111/j.1445-5994.2012.02725.x [ Links ]
5. Anthony J, Osman A, Sani MU. Valvular heart disease in pregnancy. Cardiovasc J Afr 2016;27(2):111-118. https://doi.org/10.5830/cvja-2016-052 [ Links ]
6. Lesniak-Sobelga A, Tracz W, KostKiewicz M, Podolec P, Pasowicz M. Clinical and echocardiographic assessment of pregnant patients with valvular heart diseases - maternal and fetal outcome. Int J Cardiol 2004;94(1):15-23. https://doi.org/10.1016/j.ijcard.2003.03.017 [ Links ]
7. Siu SC, Colman JM, Sorensen S, et al. Adverse neonatal and cardiac outcomes are more common in pregnant patients with cardiac disease. Circulation 2002;105(18):2179-2184. https://doi.org/10.1161/01.cir.0000015699.48605.08 [ Links ]
8. Wolfe DS, Hameed AB, Taub CC, Zaidi AN, Bortnick AE. Addressing maternal mortality: The pregnant cardiac patient. Am J Obstet Gynecol 2019;220(2):167.e1-167.e8. https://doiorg/10.1016/j.ajog.2018.09.035 [ Links ]
9. Sobhani NC, Schultz H, Kheiwa A, et al. Contraceptive choices in the immediate postpartum period in patients with cardiac disease. Am J Cardiol 2019;123(8):1364-1369. https://doi.org/10.1016/j.amjcard.2019.01.006 [ Links ]
10. Nanna M, Stergiopoulos K. Pregnancy complicated by valvular heart disease: An update. J Am Heart Assoc 2014;3(3):e000712. https://doi.org/10.1161/jaha.113.000712 [ Links ]
11. Perelshtein Brezinov O, Simchen MJ, Ben Zekry S, Kuperstein R. Maternal and neonatal complications of pregnant patients with mitral stenosis. Isr Med Assoc J 2019;21(2):88-93. https://www.ima.org.il/FilesUploadPublic/IMAJ/0/333/166576.pdf (accessed 27 November 2019). [ Links ]
12. Diao M, Kane A, Ndiaye MB, et al. Pregnancy in women with heart disease in sub-Saharan Africa. Arch Cardiovasc Dis 2011;104(6-7):370-374. https://doi.org/10.1016/j.acvd.2011.04.001 [ Links ]
13. Joubert I, Dyer R. Anaesthesia for the pregnant patient with acquired valvular heart disease. Update Anaesth 2005:15-20. https://resources.wfsahq.org/wp-content/uploads/uia-19-ANAESTHESIA-FOR-THE-PREGNANT-PATIENT-WITH-ACQUIRED-VALVULAR-HEART-DISEASE.pdf (accessed 15 November 2019). [ Links ]
14. Dua S, Maurtua MA, Cywinski JB, Deogaonkar A, Waters JH, Dolak JA. Anesthetic management for emergency cesarean section in a patient with severe valvular disease and preeclampsia. Int J Obstet Anesth 2006;15(3):250-253. https://doi.org/10.1016/j.ijoa.2005.10.016 [ Links ]
15. Drenthen W, Boersma E, Balci A, et al. Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J 2010;31(17):2124-2132. https://doi.org/10.1093./eurheartj/ehq200 [ Links ]
16. Chohan U, Afshan G, Mone A. Anaesthesia for caesarean section in patients with cardiac disease. J Pak Med Assoc 2006;56(1):32-38. [ Links ]
 Correspondence:
Correspondence:
P Motshabi Chakane
palesa.motshabi@wits.ac.za
Accepted 13 June 2023














