Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Obstetrics and Gynaecology
versão On-line ISSN 2305-8862
versão impressa ISSN 0038-2329
SAJOG vol.28 no.2 Cape Town Dez. 2022
http://dx.doi.org/10.7196/sajog.2022.v28i2.2097
RESEARCH
Prevalence of and sociodemographic factors associated with antenatal depression among women in Limpopo Province, South Africa
M C RamohlolaI; E MaimelaII; T S NtuliIII
IBCur, MPH; Department of Public Health, Faculty of Healthcare Sciences, University of Limpopo, Polokwane, South Africa
IIMSc, PhD; Department of Public Health, Faculty of Healthcare Sciences, University of Limpopo, Polokwane, South Africa
IIIMSc, PhD; Department of Statistical Science, School of Science and Technology, Sefako Makgatho Health Sciences University, Pretoria, South Africa
ABSTRACT
BACKGROUND: Pregnancy-related depression is a common psychiatric disorder and a major public health concern in both developed and developing countries, but the disorder receives little attention and few resources, particularly in developing countries
OBJECTIVES: To assess the prevalence of antenatal depression and its sociodemographic risk factors among pregnant women in Limpopo Province, South Africa
METHODS: This was a cross-sectional descriptive study conducted in a district hospital from 8 March to 12 April 2021. Consecutive women attending antenatal care services during the data collection period were included in the study. The Edinburgh Postnatal Depression Scale was used to assess depression symptoms
RESULTS: The prevalence of antenatal depression was 31% (95% confidence interval 26.1 - 36.3). Being unmarried, being a smoker, being without financial support from a partner, having a violent partner and having a less-educated partner were significant predictors of antenatal depression in these women
CONCLUSION: Nearly one-third of the pregnant women in our study had depressive symptoms. The important predictors of antenatal depression included being unmarried, smoking, lack of financial support from a partner, intimate partner violence and having a less-educated partner. These findings may help healthcare workers to identify women at risk early, so that support can be offered during pregnancy and childbirth
Maternal mental disorders are common complications in pregnancy worldwide.[1,2] However, these disorders have received little attention and few resources, particularly in low- and middle-income countries.[3] The most frequent maternal mental disorder occurring during the antenatal or postpartum period is depression[4] which contributes to the risk of obstetric complications such as preterm birth, miscarriage, stillbirth, low birth weight and early neonatal death.[5-7] The prevalence rates of antenatal depression vary across different countries and regions. Globally, epidemiological studies have reported prevalence rates of antenatal depression ranging between 7.0% and 29.6%.[8-13] In sub-Saharan African countries, prevalence rates have ranged from 17.7% to 50.0%.[14-23]
Several studies have identified various sociodemographic risk factors that contributed to antenatal depression in developing countries. These include maternal age,[24,25] being unmarried,[26-28] having a lower level of education,[25,26,29] smoking,[26,30,31] consumption of alcohol,[30] being HIV infected,[31,32] poor nutritional status,[33,34] partner violent behaviour,[21,35-37] and lack of partner financial support.[38,39] In South Africa (SA), studies have found that antenatal depression is common in the first trimester of pregnancy and is influenced by partner and family relationships.[22,23] An SA study conducted among HIV-infected women attending antenatal clinics at regional hospitals found that maternal age and employment status were risk factors for antenatal depression.[24] Despite the high rates and adverse outcomes of depression in pregnancy, there is a paucity of data regarding the magnitude of antenatal depression and its associated risk factors in Limpopo Province (LP), a largely rural province of SA. The objective of the present study was therefore to determine the prevalence of antenatal depressive symptoms and the associated sociodemographic risk factors among pregnant women at Helene Franz Hospital, LP.
Methods
Study design and setting
A facility-based cross-sectional study was conducted at Helene Franz Hospital, a district hospital in a rural area of LP. The hospital provides a wide range of healthcare services, including routine antenatal care (ANC). It has 22 feeder primary healthcare clinics, and provides ANC to ~1 000 women annually. The study was conducted from 8 March to 12 April 2021.
Study population
The study population comprised pregnant women aged >18 years who attended ANC at Helene Frans Hospital. Women aged <18 years and those who were mentally ill were excluded, because they required consent from their parents or legal guardian to participate in the study.
Sample size and sampling techniques
Consecutive groups of women who attended ANC during the data collection period were asked to participate in the study. A minimum sample size of 336 was calculated based on a 95% confidence interval (CI), 5% sampling error, and 38.5% prevalence of depression among pregnant women in SA.[18]
Data collection
The research team explained the purpose of the study to each group of women while they awaited their routine ANC appointment. A self-administered questionnaire, including the informed consent document, was given to women who agreed to participate. The tool was translated into Sepedi for those who did not understand English, and back-translated to English to confirm the validity of the translation. The questionnaire had three sections. The first section, on maternal demographics, included age, marital status, level of education, employment status, alcohol use, smoking status, financial support from partner, partner violent behaviour, whether the pregnancy was planned, parity and HIV status. The second section included partner demographics such as employment status, education level, smoking status and drinking alcohol. The last section of the questionnaire was the Edinburgh Postnatal Depression Scale (EPDS) a screening tool widely used to assess depressive symptoms during pregnancy.[40] The EPDS consists of 10 questions, each asking about depressive symptoms over the past 7 days. Each question has a 4-point Likert scale, with a score of 0 - 3. Items were summed, with a possible score ranging from 0 to 30.
A meta-analysis of the screening accuracy of the EPDS to detect depression in pregnant and postpartum women reported various cut-off values, with values of >10 and >13 found to have higher sensitivity and specificity.[41] Studies carried out in low-resource settings found possible depressive symptoms at scores >8.[13,14] In our study, we therefore defined depressive symptoms as a score of >10 because it has higher sensitivity and specificity.[41] Women found to have possible depressive symptoms (EPDS scores >10) were informed of their scores and then allowed to decide whether or not to seek further assessment and treatment. If they accepted, they were assisted to make an appointment with the psychiatry personnel after the completion of their medical appointment.
Statistical analysis
Data were entered into an Excel spreadsheet, 2016 version (Microsoft Corp., USA), and then exported to SPSS version 21.0 statistical software (IBM Corp., USA) for analysis. Descriptive statistics such as means and standard deviations (SDs) were used to interpret continuous variables, while frequencies and percentages were used for categorical variables. To assess the predictors of antenatal depression, bivariate logistic regression analysis was performed and all independent variables with a p-value <0.2 were considered statistically significant and included in the multivariable logistic regression analysis.[14-16] In multivariable logistic regression analysis, variables with a p-value <0.05 were considered statistically significant. The Hosmer-Lemeshow goodness-of-fit test was used to test for model fitness. The multicollinearity of independent variables was assessed using the variance inflation factor and was found to be <5, which indicates that the independent variables are not linear combinations of each other.
Ethical considerations
The University of Limpopo granted ethical approval for this study (ref. no. TREC/326/2020: PG). Permission to conduct the study was obtained from the provincial Department of Health Research Committee of LP (ref. no. LP_2020_11_028) and the CEO of the hospital. The women were fully informed about the objectives of the study, and those who agreed to participate completed the informed consent form.
Results
Sociodemographic characteristics
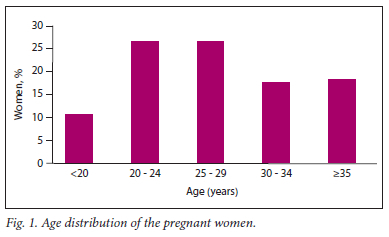
Three hundred and thirty-five pregnant women were included for further analysis. One woman was excluded from the study owing to incomplete information on the EPDS. Overall, the mean (SD) age of the participants was 27.8 (6.9) years, ranging from 18 to 47 years. Slightly more than half of the women (54%) were in the age group 20 - 29 years (Fig. 1). The majority of the women (82%) were unmarried and 67% had secondary education, followed by those with tertiary education (26%). Most of the women (84%) were unemployed, 71% said that their pregnancy was planned, 94% did not drink alcohol and 96% did not smoke. More than one-third of the women (40%) were primiparous, and only 15% were HIV positive. Seventy-four per cent of the women indicated that their partners supported them financially, and only 9% said that their partners were violent.
Prevalence of sociodemographic factors associated with antenatal depression
The mean (SD) depression score for the women was 7.87 (5.2), ranging from 0 to 23, and the prevalence rate of symptoms of depression was 31% (95% CI 26.1 - 36.3). Table 1 shows predictors of antenatal depression among the women. On the bivariate logistic regression analysis, maternal age, level of education, partner employment status and smoking status showed a significant association with depression (p<0.2). However, in the multivariate logistic regression analysis, no variable was statistically significant (p>0.05).
In the multivariate logistic regression model, unmarried pregnant women (odds ratio (OR) 1.93; 95% CI 0.04 - 1.02; p<0.05), women who smoked (OR 4.19; 95% CI 1.20 - 14.6; p<0.05), women without financial support from the partner (OR 2.35; 95% CI 1.35 - 4.06; p<0.05), and women with a violent partner (OR 3.39; 95% CI 1.51 - 7.54; p<0.05) were more likely to experience depression than their counterparts. Women with a partner who had secondary education (36%) and tertiary education (66%) were significantly less likely to experience depression.
Discussion
This study measured the prevalence of antenatal depression and its associated risk factors among women attending ANC at a rural district hospital in LP. Nearly one-third (31%) of the women in our study had symptoms of antenatal depression. This finding is higher
than the rates of 13.6% in Greece,[10] 29% in South America,[11] 22.3% in Colombia,[121 29.6% in Sri Lanka,[131 17.7% in Tanzania,[14] 27.1% in Uganda[15] and 24.5% in Ethiopia[16] but lower than the 38.4% found in Kenya.[17] The prevalence of antenatal depression in our study was lower than the rates observed in previous studies in SA, which were 39.5%, 47% and 48.7% in a peri-urban area in Cape
Town[20] and rural areas in KwaZulu-Natal[18] and Mpumalanga[21] provinces, respectively. Our prevalence is, however, higher than the rates of 22% reported in an urban setting in Cape Town[19] and 27% in two studies conducted in Soweto.[22,23] Possible reasons for these variations could be the types of instruments used for measuring antenatal depression and the use of different EPDS cut-off values to define pregnancy depressive symptoms.[41] The EPDS is a commonly used screening tool to assess antenatal depression symptoms and has been validated among antenatal outpatients at King Edward VIII Hospital in KwaZulu-Natal,[42] and in our study, the reliability coefficient was found to be 0.78.
Regarding the predictors of antenatal depression, the present study replicated the finding of Sheeba et al.[43] that maternal age did not predict the occurrence of antenatal depression, whereas other studies have found that women of younger age were at increased risk of antenatal depression.[24,25,30] Several studies found that being unmarried was a significant independent predictor of depression.[26-28] In agreement with this finding, our study showed that unmarried women had a 2-fold increased risk of developing antenatal depression. Sheeba et al.[43] found that maternal level of education was not significantly associated with depression on bivariate analysis. In contrast, in our study, maternal level of education was found to be a risk factor for antenatal depression on bivariate but not on multivariate logistic regression analysis. However, some studies do report a significant relationship on multivariate logistic regression analysis.[25,26,29]
Women with a history of cigarette smoking are significantly more likely to develop depression than non-smokers.[1,26] The present study found that women who smoked cigarettes had a 4-fold increased risk of antenatal depression. In contrast, some studies have not found maternal smoking status to be significantly associated with depression.[25] Our finding concurs with a cross-sectional study conducted in KwaZulu-Natal, which found that antenatal depression did not differ significantly between HIV-infected and HIV-uninfected women.[24] In contrast, other studies have reported a statistical relationship between HIV status and antenatal depression[31,32,42] The partner's violent behaviour[22,23,27,37] and lack of support[37,38] are well-documented risk factors for developing antenatal depression. In the present study, women who lacked financial support from a partner and had a violent partner were 2 and 3 times more likely to develop antenatal depression, respectively. We also found that partner employment and smoking status were associated with antenatal depression in the bivariate analysis, but that these were not statistically significant in the multivariate analysis.
Study limitations
This study has several limitations. Firstly, it was a cross-sectional study, so it was difficult to determine the causality inferences. Moreover, although stage of gestation has been reported to be a risk factor for antenatal depression in previous studies,[22,44] in our study, the stage of gestation of the participants was not recorded, so we were unable to assess the prevalence of antenatal depression per trimester. In addition, the study was conducted in one hospital and the results can therefore not be generalised to the whole province. There is a wide variation in the EPDS cut-off value for depression, with some studies using a score as high as >14 while others used a score as low as >8.[41 For our study, we decided to use >10 based on the findings of a study in Tanzania with a low-resource setting similar to ours.[14] However, our results might have been different had we used a different cutoff score. Lastly, even though the EPDS is widely used as a screening tool to assess the symptoms of antenatal depression, the lack of a confirmed clinical diagnosis of antenatal depression can be considered a limitation of our study.
Conclusion
Nearly one-third of pregnant women in the present study had antenatal depressive symptoms, which were found to be associated with being unmarried, smoking, lack of financial support from a partner, partner violence and a less-educated partner. These findings may help healthcare workers to identify at-risk pregnant women early so that support can be offered during pregnancy and childbirth.
Declaration. The research for this study was done in partial fulfilment of the requirements for MCR's MPH degree at the University of Limpopo.
Acknowledgements. The authors thank the Limpopo Department of Health and the Helene Franz Hospital management for granting permission to conduct this study in the hospital. They also thank all the pregnant women who participated in the study.
Author contributions. MCR: conceptualised and developed the study protocol, designed the methods, and conducted data collection. EM: provided guidance to MCR with regard to the scientific conduct of the study, contributed to the development of the data collection tools, and critically reviewed the manuscript. TSN: supervised data collection, analysed the data, interpreted the results, and contributed to the writing of the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: An umbrella review. BMC Public Health 2020;20(1):173. https://doi.org/10.1186/s12889-020-8293-9 [ Links ]
2. Dadi AF, Miller ER, Mwanri L. Antenatal depression and its association with adverse birth outcomes in low and middle-income countries: A systematic review and meta-analysis. PLoS ONE 2020;15(1):e0227323. https://doi.org/10.1371/journal.pone.0227323 [ Links ]
3. Baron EC, Hanlon C, Mall S, et al. Maternal mental health in primary care in five low- and middle-income countries: A situational analysis. BMC Health Serv Res 2016;16:53. https://doi.org/10.1186/s12913-016-1291-z [ Links ]
4. Mongan D, Lynch J, Hanna D, et al. Prevalence of self-reported mental disorders in pregnancy and associations with adverse neonatal outcomes: A population-based cross-sectional study. BMC Pregnancy Childbirth 2019;19(1):412. https://doi.org/10.1186/s12884-019-2572-4 [ Links ]
5. Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 2015;28(3):179-193. https://doi.org/10.1016/j.wombi.2015.02.003 [ Links ]
6. Lefkovics E, Baji I, Rigó J. Impact of maternal depression on pregnancies and on early attachment. Infant Ment Health J 2014;35(4):354-365. https://doi.org/10.1002/imhj.21450 [ Links ]
7. Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. The impact of maternal depression during pregnancy on perinatal outcomes: A systematic review and meta-analysis. J Clin Psychiatry 2013;74(4):e321-e341. https://doi.org/10.4088/JCP.12r07968 [ Links ]
8. Eastwood J, Ogbo FA, Hendry A, Noble J, Page A; Early Years Research Group (EYRG). The impact of antenatal depression on perinatal outcomes in Australian women. PLoS ONE 2017;12(1):e0169907. https://doi.org/10.1371/journal.pone.0169907 [ Links ]
9. Coll CVN, da Silveira MF, Bassani DG, et al. Antenatal depressive symptoms among pregnant women: Evidence from a Southern Brazilian population-based cohort study. J Affect Disord 2017;209:140-146. https://doi.org/10.1016/j.jad.2016.11.031 [ Links ]
10. Koutra K, Vassilaki M, Georgiou V, et al. Pregnancy, perinatal and postpartum complications as determinants of postpartum depression: The Rhea mother-child cohort in Crete, Greece. Epidemiol Psychiatr Sci 2018;27(3):244-255. https://doi.org/10.1017/S2045796016001062 [ Links ]
11. Martínez-Paredes JF, Jácome-Pérez N. Depression in pregnancy. Rev Colomb Psiquiatr (Engl Ed) 2019;48(1):58-65. https://doi.org/10.1016/j.rcp.2017.07.003 [ Links ]
12. Vergel J, Gaviria SL, Duque M, Restrepo D, Rondon M, Colonia A. Gestation-related psychosocial factors in women from Medellin, Colombia. Rev Colomb Psiquiatr (Engl Ed) 2019;48(1):26-34. https://doi.org/10.1016/j.rcp.2017.06.003 [ Links ]
13. Palfreyman A. Addressing psychosocial vulnerabilities through antenatal care - depression, suicidal ideation, and behavior: A study among urban Sri Lankan women. Front Psychiatry 2021;12:554808. https://doi.org/10.3389/fpsyt.2021.554808 [ Links ]
14. Massae AF, Larsson M, Leshabari S, Mbekenga C, Pembe AB, Svanberg AS. Predictors of fear of childbirth and depressive symptoms among pregnant women: A cross-sectional survey in Pwani region, Tanzania. BMC Pregnancy Childbirth 2021;21(1):704. https://doi.org/10.1186/s12884-021-04169-7 [ Links ]
15. Atuhaire C, Rukundo GZ, Nambozi G, et al. Prevalence of postpartum depression and associated factors among women in Mbarara and Rwampara districts of south-western Uganda. BMC Pregnancy Childbirth 2021;21(1):503. https://doi.org/10.1186/s12884-021-03967-3 [ Links ]
16. Beyene GM, Azale T, Gelaye KA, Ayele TA. Depression remains a neglected public health problem among pregnant women in northwest Ethiopia. Arch Public Health 2021;79(1):132. https://doi.org/10.1186/s13690-021-00649-6 [ Links ]
17. Mochache K, Mathai M, Gachuno O, vander Stoep A, Kumar M. Depression during pregnancy and preterm delivery: A prospective cohort study among women attending antenatal clinic at Pumwani maternity hospital. Ann General Psychiatry 2018;17(1):31. https://doi.org/10.1186/s12991-018-0202-6 [ Links ]
18. Rochat TJ, Tomlinson M, Bárnighausen T, Newell ML, Stein A. The prevalence and clinical presentation of antenatal depression in rural South Africa. J Affect Disord 2011;135(1-3):362-373. https://doi.org/10.1016/j.jad.2011.08.011 [ Links ]
19. Heyningen TV, Myer L, Onah M, Tomlinson M, Field S, Honikman S. Antenatal depression and adversity in urban South Africa. J Affect Disord 2016;203:121-129. https://doi.org/10.1016/j.jad.2016.05.052 [ Links ]
20. Tsai AC, Tomlinson M, Comulada WS, Rotheram-Borus MJ. Food insufficiency, depression, and the modifying role of social support: Evidence from a population-based, prospective cohort of pregnant women in periurban South Africa. Soc Sci Med 2016;151:69-77. https://doi.org/10.1016/j.socscimed.2015.12.042 [ Links ]
21. Peltzer K, Rodriguez VJ, Jones D. Prevalence of prenatal depression and associated factors among HIV-positive women in primary care in Mpumalanga province, South Africa. SAHARA J 2016;13(1):60-67. https://doi.org/10.1080/17290376.2016.1189847 [ Links ]
22. Redinger S, Norris SA, Pearson RM, Richter L, Rochat T. First trimester antenatal depression and anxiety: Prevalence and associated factors in an urban population in Soweto, South Africa. J Dev Orig Health Dis 2018;9(1):30-40. https://doi.org/10.1017/S204017441700071X [ Links ]
23. Redinger S, Pearson RM, Houle B, Norris SA, Rochat TJ. Antenatal depression and anxiety across pregnancy in urban South Africa. J Affect Disord 2020;277:296-305. https://doi.org/10.1016/j.jad.2020.08.010 [ Links ]
24. Nydoo P, Naicker T, Moodley J. Depressive scores in newly diagnosed HIV-infected and HIV-uninfected pregnant women. S Afr J Psychiatry 2017;23:1085. https://doi.org/10.4102/sajpsychiatry.v23i0.1085 [ Links ]
25. Li X, Gao R, Dai X, et al. The association between symptoms of depression during pregnancy and low birth weight: A prospective study. BMC Pregnancy Childbirth 2020;20(1):147. https://doi.org/10.1186/s12884-020-2842-1 [ Links ]
26. Fellenzer JL, Cibula DA. Intendedness of pregnancy and other predictive factors for symptoms of prenatal depression in a population-based study. Matern Child Health J 2014;18(10):2426-2436. https://doi.org/10.1007/s10995-014-1481-4 [ Links ]
27. Brittain K, Myer L, Koen N, et al. Risk factors for antenatal depression and associations with infant birth outcomes: Results from a South African birth cohort study. Paediatr Perinat Epidemiol 2015;29(6):505-514. https://doi.org/10.1111/ppe.12216 [ Links ]
28. Srinivasan M, Reddy MM, Sarkar S, Menon V. Depression, anxiety, and stress among rural South Indian women - prevalence and correlates: A community-based study. J Neurosci Rural Pract 2020;11(1):78-83. https://doi.org/10.1055/s-0039-1700595 [ Links ]
29. Muraca GM, Joseph KS. The association between maternal age and depression. J Obstet Gynaecol Can 2014;36(9):803-810. https://doi.org/10.1016/S1701-2163(15)30482-5 [ Links ]
30. Silva MMJ, Leite EPRC, Nogueira DA, Clapis MJ. Depression in pregnancy: Prevalence and associated factors. Invest Educ Enferm 2016;34(2):342-350. https://doi.org/10.17533/udea.iee.v34n2a14 [ Links ]
31. Zhu QY, Huang DS, Lv JD, Guan P, Bai XH. Prevalence of perinatal depression among HIV-positive women: A systematic review and meta-analysis. BMC Psychiatry 2019;19(1):330. https://doi.org/10.1186/s12888-019-2321-2 [ Links ]
32. Ngocho JS, Watt MH, Minja L, et al. Depression and anxiety among pregnant women living with HIV in Kilimanjaro region, Tanzania. PLoS ONE 2019;14(10):e0224515. https://doi.org/10.1371/journal.pone.0224515 [ Links ]
33. Van Heyningen T, Myer L, Onah M, Tomlinson M, Field S, Honikman S. Antenatal depression and adversity in urban South Africa. J Affect Disord 2016;203:121-129. https://doi.org/10.1016/j.jad.2016.05.052 [ Links ]
34. Abrahams Z, Lund C, Field S, Honikman S. Factors associated with household food insecurity and depression in pregnant South African women from a low socio-economic setting: A cross-sectional study. Soc Psychiatry Psychiatr Epidemiol 2018;53(4):363-372. https://doi.org/10.1007/s00127-018-1497-y [ Links ]
35. Garman EC, Schneider M, Lund C. Perinatal depressive symptoms among low-income South African women at risk of depression: Trajectories and predictors. BMC Pregnancy Childbirth 2019;19(1): 202. https://doi.org/10.1186/s12884-019-2355-y [ Links ]
36. Schneider M, Baron E, Davies T, Munodawafa M, Lund C. Patterns of intimate partner violence among perinatal women with depression symptoms in Khayelitsha, South Africa: A longitudinal analysis. Glob Ment Health (Camb) 2018;5:e13. https://doi.org/10.1017/gmh.2018.1 [ Links ]
37. Ogbo FA, Eastwood J, Hendry A, et al. Determinants of antenatal depression and postnatal depression in Australia. BMC Psychiatry 2018;18(1):49. https://doi.org/10.1186/s12888-018-1598-x [ Links ]
38. Rwakarema M, Premji SS, Nyanza EC, Riziki P, Palacios-Derflingher L. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in Northern Tanzania: A cross-sectional study. BMC Womens Health 2015;15:68. https://doi.org/10.1186/s12905-015-0225-y [ Links ]
39. Noordzij M, Tripepi G, Dekker FW, Zoccali C, Tanck MW, Jager KJ. Sample size calculations: Basic principles and common pitfalls. Nephrol Dial Transplant 2010;25(5):1388-1393. https://doi.org/10.1093/ndt/gfp732 (erratum in: Nephrol Dial Transplant 2010;25(10):3461-342). [ Links ]
40. Cox JL, Holden J, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-786. https://doi.org/10.1192/bjp.150.6.782 [ Links ]
41. Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD; DEPRESsion Screening Data (DEPRESSD) EPDS Group. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: Systematic review and meta-analysis of individual participant data. BMJ 2020;371:m4022. https://doi.org/10.1136/bmj.m4022 [ Links ]
42. Manikkam L, Burns JK. Antenatal depression and its risk factors: An urban prevalence study in KwaZulu-Natal. S Afr Med J 2012;102(12):940-944. https://doi.org/10.7196/SAMJ.6009 [ Links ]
43. Sheeba B, Nath A, Metgud CS, et al. Prenatal depression and its associated risk factors among pregnant women in Bangalore: A hospital based prevalence study. Front Public Health 2019;7:108. https://doi.org/10.3389/fpubh.2019.00108 [ Links ]
44. Tamiru D, Misgana T, Tariku M, et al. Prevalence and associated factors of common mental disorders among pregnant mothers in rural eastern Ethiopia. Front Psychiatry 2022;13:843984. https://doi.org/10.3389/fpsyt.2022.843984 [ Links ]
 Correspondence:
Correspondence:
T S Ntuli
tsntuli@hotmail.com
Accepted 27 September 2022














