Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Obstetrics and Gynaecology
versão On-line ISSN 2305-8862
versão impressa ISSN 0038-2329
SAJOG vol.28 no.1 Cape Town Jun. 2022
http://dx.doi.org/10.7196/SAJOG.2022.v28i1.2052
RESEARCH
Provision of postpartum long-acting reversible contraception: A quality improvement intervention with pre- and postintervention evaluation
E E WynneI; G J HofmeyrI, II
IMB ChB; Department of Obstetrics and Gynaecology, Walter Sisulu University; Eastern Cape Department of Health, South Africa
IIMB ChB; Department of Obstetrics and Gynaecology, University of Botswana, Gaborone, Botswana
ABSTRACT
BACKGROUND: Unintended pregnancies remain an important health challenge in South Africa (SA) and worldwide. Improving access to contraception and long-acting reversible contraception in particular, may reduce the number of unintended pregnancies
OBJECTIVE: To determine the impact of a training and supportive mentoring programme on postpartum uptake of long-acting reversible contraceptive (LARC) methods
METHODS: A quality-of-care improvement intervention with pre- and post-intervention evaluation of LARC uptake was conducted at a midwife-led, on-site obstetric unit in the Eastern Cape, SA. Midwives were trained in contraceptive counselling and postpartum etonorgestrel implant insertion. The researcher provided counselling and postpartum intrauterine device (IUD) insertion services
RESULTS: In the 10 weeks prior to the intervention, neither the IUD nor the implant were provided in the unit. In the 10 weeks after the intervention, uptake of the IUD was n=27/289 (9.3%) and the implant n=21/289 (7.3%). Use of no contraception or condoms increased from n=22/273 (8.1%) to n=41/289 (14.2%) (p<0.02). The increase was accounted for by a change in staff in the last 4 weeks of the intervention period (n=33/105 (31.4%) v. n=8/184 (4.4%) during the first 6 weeks; p<0.00
CONCLUSION: Competing responsibilities of maternity staff may limit the contraceptive options offered to postpartum women. A programme of training and supportive supervision resulted in a substantial increase in levels of LARC uptake. Strategies are needed to institutionalise comprehensive postpartum contraceptive provision nationally
Unintended pregnancies have important medical, psychological and social consequences, and contribute substantially to avoidable maternal mortality. Globally, in 2012 it was estimated that 40% of all pregnancies were unintended, representing 85 million pregnancies, of which 50% resulted in termination and 38% in a live birth.[1] The estimated number of unplanned pregnancies for sub-Saharan Africa was 14 million per annum in 2008.[2] Increased uptake and use of long-acting reversible contraceptives (LARCs) could decrease this number substantially.
Methods
The study was a quality-of-care improvement study that sought to improve uptake of LARC among low-risk postpartum women by improving nursing staff knowledge of LARCs, as well as, by improving their counselling of patients. The study took place in the five-bed postnatal ward of the Duncan Village Day Hospital Midwife Obstetric Unit, an 'on site' midwife-led obstetric unit on the premises of Frere Maternity Hospital, East London, South Africa (SA).[3] All patients over the age of 18 were eligible for the study. The control group were patients who delivered in the 10 weeks immediately prior to the intervention (1 November 2017 - 14 January 2018), while the intervention group were all those patients who delivered during the 10-week study period (15 January - 31 March 2018). Counselling took place between 07h00 and 08h00 prior to regular discharge of patients at 09h00. All patients receiving counselling gave written consent prior to being counselled. All postpartum patients are admitted in the postnatal ward and are discharged as early as 6 hours post-delivery. A small proportion of patients who deliver in the morning may be discharged in the afternoon 6 hours postpartum and thereby miss the 07h00 counselling.
The administration of the desired contraception took place immediately following counselling. Nursing staff received training in the two weeks prior to the commencement of the intervention. Both day teams of nursing staff were trained on insertion of implants and intrauterine devices (IUDs) (NovaT Bayer) as well as the important aspects of counselling. Nursing champions were identified and were encouraged to further their knowledge and skills.
After 6 weeks, there was a changeover between day and night shift staff, which had not been anticipated in the planning. In the last 4 weeks of the intervention, the new day nursing teams had not received the training and had not identified a contraceptive champion. This was a lack of foresight in the planning of the study. However, it afforded the opportunity to assess the impact of the nursing staff training.
Data analysis
Data from the routinely collected labour ward records were extracted onto a data collection form, entered onto an Excel spreadsheet (Microsoft Corp., USA) and analysed using Epi-info statistical analysis package (CDC, USA).
The following data were collected: contraception choice, age, parity, pregnancy booking and HIV status.
The primary objective was to measure the uptake of LARC during the study period (from a baseline of non-use). Sub-group analyses were planned for age (<20 years v. >=20 years), primiparous v. multiparous women and HIV-positive v. HIV-negative women. We also conducted a post hoc comparison of uptake during the periods with and without specific training of the midwifery staff.
Statistical comparisons were made using rate ratios with 95% confidence intervals (CI) as well as the Fisher exact test. p-values <0.05 were regarded as statistically significant.
Analysis was made on an intention-to-treat basis. Although every effort was made to counsel as many of the intervention group as possible, not all patients received comprehensive counselling but were nevertheless included in the intervention group statistics.
Ethical considerations
Approval was received from the Walter Sisulu University ethics committee (ref. no. 068/2016) and the institutional management. The study was a quality-of-care improvement intervention implementing current best practice according to national guidelines and presenting routinely collected, unlinked data. Individual patient consent was obtained from each participant prior to initiation of counselling.
Results
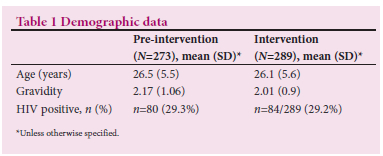
The demographic data for the pre-intervention (n=273) and post-intervention (n=289) groups were similar (Table 1).
Pre- and post-intervention contraceptive uptake are shown in Table 2. Table 3 shows the post intervention sub-group analysis. After the intervention, the IUD was chosen by 9.3% and the implant by 7.3% of women.
Results for intervention period 1 (15/1/2018 - 28/2/2018) (n=184) v. period 2 (1/3/2018 - 31/3/2018) (n=105) are shown in Table 4. In the second period, there was less uptake of the implant (which was administered by the nursing staff, as well as the researcher, during the first period): n=4/105 (3.8%) compared with n=17/184 (9.3%) in the first period, though the numbers were small and the difference not statistically significant (RR 2.43; 95% CI 0.84 - 7.2; p=0.07). The IUD was inserted only by the researcher and uptake was similar between the two periods (n=15/184 (8.2%) and n=12/105 (11.3%) respectively, RR 0.7; 95% CI 0.35 - 1.47; p=0.24). Uptake of IUDs was similar in both HIV-positive and HIV-negative groups.
There was less usage of IUDs among primiparous than multiparous women (n=2/88 (2%) v. n=25/160 (13.2%), RR 0.15; 95% CI 0.037 - 0.64; p=0.0009) and women younger than 25 (n=5/108 (4%) v. n=22/140 (13.4%), RR 0.3; 95% CI 0.12 - 0.76; p=0.0045).
Discussion
The HIV prevalences (29.3% in the pre-intervention group and 29.2% in the intervention group) are in keeping with known prevalence in the study area. Within the SA context there is a dearth of published studies on the topic of healthcare interventions to increase LARC uptake in the postpartum period. The best comparisons can therefore be made with studies from other low- and middle-income countries. Given that LARCs were not previously offered in this unit and that the IUDs is a relatively unfamiliar method in this community, the uptake of 9.3% for the IUD and 7.3% for the implant was considered a substantial result. The uptake of the IUD was not as high as the 37% found in an Indian study,[4] which showed an uptake of IUD of 37% after an intervention to allow IUD insertion by midwives. This success was attributed mainly to the administration of the IUD by nursing staff. It was thought that nursing staff work more closely with patients and are often from the same communities and therefore patients have greater trust in them. India is also noted to have a high acceptance of IUD use. A study in Bangladesh found that structured training of nursing staff already providing contraceptive services had no impact on the overall postpartum IUD insertion rate at 5 months post training.[5] The difference in our study may have been that the training was within the work environment and supported by mentoring from the researcher and the midwife champion and that prior to this study contraceptive services were very limited. Our study is in keeping with a systematic review assessing uptake of LARCs in low- and middle-income countries after healthcare provider training, which showed a tendency towards increased uptake.[6] A larger multilevel intervention to increase uptake of LARCs in Rwanda showed an uptake of nearly 30% of postpartum intrauterine device (PPIUD) and 10% uptake of implants post intervention. A pre-intervention insertion rate of 7.7 PPIUDs/ month, increased to 214.6 insertions/month.[7] This study is an example of addressing contraceptive insufficiencies by targeting multiple levels of care and counselling patients at multiple visits and having the capacity to provide chosen contraception as desired. An intervention of this scale within our communities may influence any stigma associated with LARCs and help to increase LARC uptake Many HIV-positive patients in the intervention group of this study showed interest in the use of an implant, but because of the current national policy of not providing implants to HIV-positive women using enzyme-inducing treatment, were counselled against this choice. This is a complex issue. While perfect use of DMPA is associated with lower failure rates than the implant in this group, actual failure rates are in general higher with DMPA, owing to difficulties in achieving perfect use. We would urge revision of the national guidelines in line with WHO recommendations to counsel on the relative failure rates for women using certain antiretroviral treatment but allowing women an informed choice. As the current guidelines are moving towards the use of dolutegravir from the use of efavirenz, this issue becomes less of a concern.
Depo medroxyprogesterone acetate remains the most widely used form of contraception among all age groups regardless of parity or HIV status. The greater use of no contraception in the post-intervention group appeared to be related to the change of staff in the latter part of the post-intervention period.
The aim of this study was not to investigate myths or mistrust of LARCs, but it was evident in the counselling process that many postpartum women were either unwilling or unable to verbalise their reasons for not wanting IUD insertion. A paucity of evidence exists in our environment as to why there has been a failure to dispel myths and misperceptions around the use of LARC, but a strategy of simple evidence-based counselling can overcome some of these barriers as has been seen in this study. Unstructured observations during the study were peer influences during group counselling sessions, the difficulty experienced by busy maternity staff to prioritise comprehensive contraceptive counselling among many other competing responsibilities and the positive impact of a highly motivated 'champion' among the nursing team.
Conclusions
Competing responsibilities of maternity staff within the South African context may limit access of postpartum women to LARCs. However, with specific interventions to empower midwives to counsel and provide a wider choice of methods, and supportive mentoring, provision of postpartum LARCS is achievable. Strategies are needed to institutionalise comprehensive postpartum contraceptive provision nationally.
Declaration. This study was performed for MMed degree purposes.
Acknowledgements. We acknowledge the support of the staff and management of the Duncan Village Day Hospital Midwives' Obstetric Unit and the patients who participated in this study.
Author contributions. EW and GJH conceived the study. EW wrote the protocol, conducted the study, analysed the data and wrote the first draft with mentoring from GJH. Both authors contributed to and approved the final draft.
Funding. None.
Conflicts of interest. None.
References
1. Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies in 2012 and recent trends. Studies Fam Planning 2014;45(3):301-314. https://doi.Org/10.1111/j.1728-4465.2014.00393.x [ Links ]
2. Hubacher D, Mavranezouli I, McGinn E. Unintended pregnancy in Sub-Saharan Africa: Magnitude of the problem and potential role of contraceptive implants to alleviate it. Contraception 2008;78(1):73-78. https://doi.org/10.1016/j.contraception.2008.03.002 [ Links ]
3. Hofmeyr GJ, Mancotywa T, Silwana-Kwadjo N, Mgudlwa B, Lawrie TA, Gulmezoglu AM. Audit of a new model of birth care for women with low risk pregnancies in South Africa: The primary care onsite midwife-led birth unit (OMBU). BMC Pregnancy Childbirth 2014;14:417. https://doi.org/10.1186/s12884-014-0417-8 [ Links ]
4. Bhadra B, Burman S, Purandare C, Divakar H, Sequeira T, Bhardwaj A. The impact of using nurses to perform postpartum intrauterine device insertions in Kalyani Hospital, India. Int J Gynaecol Obstet 2018;143(S1):33-37. https://doi.org/10.1002/ijgo.12602 [ Links ]
5. Fatima P, Antora AH, Dewan F, Nash, Sethi M. Impact of contraceptive counselling training among counsellors participating in the FIGO postpartum intrauterine device initiative in Bangladesh. Int J Gynecol 2018;143(S1):49-55. https://doi.org/10.1002/ijgo.12605 [ Links ]
6. Baekgaard RS, Damhaugh EG, Mrema D, Rasch V, Khan K, Linde DS. Training of healthcare providers and use of long-acting reversible contraception in low- and middle-income countries: A systematic review. Acta Obstet Gynecol Scand 2021;100(4):619-628. https://doi.org/10.1111/aogs.14127 [ Links ]
7. Espey J, Ingabire R, Nyombayire J, et al. Postpartum long-acting contraception uptake and service delivery outcomes after a multilevel intervention in Kigali, Rwanda. BMJ Sex Reprod Health 2021;47(3):173-178. https://doi.org/10.1136/bmjsrh-2020-200741 [ Links ]
 Correspondence:
Correspondence:
E Wynne
e.e.biggs@gmail.com
Accepted 3 April 2022














