Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Obstetrics and Gynaecology
versão On-line ISSN 2305-8862
versão impressa ISSN 0038-2329
SAJOG vol.28 no.1 Cape Town Jun. 2022
http://dx.doi.org/10.7196/SAJOG.2022.v28i1.2062
RESEARCH
Safe caesarean sections in South Africa: Is internship training sufficient?
L TemlettI; D G BishopII; N MoranIII
IDA (SA); Department of Anaesthesiology and Critical Care, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IIPhD; Department of Anaesthesiology and Critical Care, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IIIFCOG (SA); KwaZulu-Natal Department of Health; Department of Obstetrics and Gynaecology, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: In Africa, the maternal mortality rate after caesarean section (CS) is 50 times higher than that in high-income countries. In South Africa (SA), women who undergo CS have a three times higher mortality rate than those who deliver vaginally. Anaesthetic complications and obstetric haemorrhage are major drivers of poor outcomes, and the case fatality rate for CS at district hospitals is particularly high
OBJECTIVES: To assess the adequacy of anaesthetic and obstetric internship training in preparing interns to perform CS independently and safely
METHODS: This was an observational cross-sectional survey of all community service officers (CSOs) in KwaZulu-Natal (KZN), SA, in 2020. Data were collected via an electronic survey that comprised 68 questions in 4 domains, covering personal information, obstetric surgical training, obstetric anaesthetic training and support received as a CSO
RESULTS: Surveys were sent to 228 CSOs in KZN, with 160 responses received (70% response rate). Respondents included participants from 8 medical schools and 33 internship facilities across the country. One in 8 interns (n=21/160) did not perform the required 10 CSs. Supervision in theatre was provided by an obstetric specialist for at least 1 CS in n=57/160 (35.62%; 95% confidence interval (CI) 28.54 - 43.39) participants, and n=45/160 (28.13%; 95% CI 21.66 - 35.64) interns never performed an emergency CS. Interns had limited opportunity to be the primary surgeon for complicated cases. Only 1/5 interns performed >5 obstetric general anaesthetics
CONCLUSIONS: This survey showed that there are deficiencies in the current CS-related training of interns in SA. A lack of exposure to adequate obstetric surgical training and obstetric general anaesthesia is likely to impact on the performance of CSOs and on the safety of the CS service provided at district hospitals. The content and quality of the CS-related intern training programme needs to be enhanced to improve the competence of CSOs. The Health Professions Council of South Africa (HPCSA) s stipulations for internship training must be adhered to and should look to include simulation training, basic surgical skills courses and prioritisation of exposure to complicated surgical scenarios
The United Nations Sustainable Development Goals for 2030 aim to reduce the global maternal mortality ratio (MMR) to <70 per 100 000 live births.[1] In sub-Saharan Africa, the MMR is 546 per 100 000 live births, a rate more than double the global average.[2,3] Maternal complications after caesarean section (CS) occur three times more commonly in Africa than in high-income countries (HICs), but maternal mortality after CS is 50 times more common than in HICs.[3] Women who undergo emergency CS in low-and middle-income countries (LMICs) are twice as likely to die than those undergoing elective CS.[4] The South African Saving Mothers Report, 2017 - 2019 revealed that women who undergo CS have a three times higher mortality rate than those who deliver vaginally[5] The report noted that anaesthetic complications and obstetric haemorrhage were major drivers of poor outcomes, and that the case fatality rate for CS at district hospitals was particularly high.[5] It is therefore essential that medical officers deployed to work in district hospitals are adequately trained to deal with perioperative obstetric care.
The Health Professions Council of South Africa (HPCSA) stipulates that the aim of internship training is to facilitate the transition from undergraduate student to competent medical practitioner.[6] Internship is a 2-year programme, including a 3-month (reduced from 4 months in 2020) obstetrics and gynaecology rotation in the first year and a 2-month anaesthetic rotation in the second year. Interns are required to complete logbooks during their training, with compulsory procedures and skills to be signed off by their supervisors. After internship, doctors become community service officers (CSOs) for 1 year before registering as independent practitioners.
The community service year often occurs in district hospitals and rural locations. Community service requires doctors to have adequate skills and knowledge to practise without specialist supervision. It is expected that CSOs can independently provide perioperative CS care, including the obstetric and anaesthetic components.[7] Few studies have evaluated the adequacy of the current intern training programme in preparing interns for community service. According to Nkabinde et al.,[8] CSOs felt that they required supervision in the management of complications from spinal anaesthesia or in the provision of general anaesthesia (GA). These doctors also felt that they required supervision to perform CSs and to manage the resultant complications. It is a common misconception that spinal anaesthesia for obstetric patients is uniformly safe.[9] This misconception can lead to inappropriate administration of spinal anaesthesia to unstable patients and to inadequately treated complications."
Our study aimed to assess the adequacy of internship training for the provision of the obstetric and anaesthetic components of perioperative CS care. Our objective was to evaluate whether doctors had received the prescribed stipulated training and whether they felt that the training adequately prepared them for their community service year
Methods
Study design and setting
This was an observational cross-sectional survey of all CSOs working in KwaZulu-Natal (KZN), South Africa (SA), in 2020. The survey was conducted using an electronic data collection tool and comprised 68 questions in 4 domains. Domain 1 comprised personal information regarding the CSOs' studies and training sites; domain 2 consisted of questions relating to training they received in obstetric surgery during internship; domain 3 covered their internship anaesthetic training; and domain 4 comprised their current level of support and practice as CSOs (Appendix A: https://www.samedical.org/file/1798).
Questionnaire development and testing
The questionnaire was developed by the authors and consisted of quantitative data in the form of yes/no questions, multiple-choice questions and Likert-scale questions. The initial survey was pilot tested among 20 medical practitioners in 3 separate rounds of pretesting and was refined based on feedback. The pretesting was conducted among medical officers, registrars and consultants in tertiary and district hospitals in the field of family medicine, internal medicine, anaesthetics and obstetrics. We assessed clarity and ambiguity at this phase and consulted an independent expert for completeness of the survey. We did not test the survey on CSOs, as they were intended to be the target population.
Data collection
KZN is the third smallest province of SA, but the second highest populated province in the country. The questionnaire was sent to all CSOs working in KZN. We aimed to reach graduates from all 8 medical schools in SA, as well as from a wide selection of internship facilities in the country. Contact details were obtained from the KZN Department of Health. The CSOs were first contacted telephonically to request their participation in the survey. This was followed up by an email containing the link to the survey, with a comprehensive explanation of the study. Those who could not be reached telephonically were emailed only. The survey was anonymous, and responses were returned electronically to the primary investigator via the electronic data collection tool. All participants were emailed two reminders. The survey was administered between 12 November and 31 December 2020.
Statistical analysis
Data were captured onto a Microsoft Excel (Microsoft Corp., USA) spreadsheet by one of the study investigators. Data were then exported to a statistical program (Stata 15) (StataCorp., USA) for further analysis. Descriptive analysis was conducted Baseline data were reported as mean (standard deviation) for continuous normally distributed variables, as median (range) for not normally distributed data, and count (percent) for categorical variables. Internal consistency was calculated using Cronbach's alpha coefficient.
Ethical approval
The study was approved by the University of KwaZulu-Natal (UKZN) Biomedical Research Ethics Committee (ref. no. BREC/00001913/2020) and by the KZN Department of Health (ref. no. NRD KZ_202009_056).
Results
The KZN Department of Health was allocated 232 CSOs in 2020. Three doctors relocated to another province. Contact details were available for n=228/229 (99.6%) CSOs in KZN for 2020. Telephonic contact was successful for n=208/228 (91.2%) CSOs, and emails were sent to all participants. The first survey response was received on 12 November 2020 and the last response on 22 December 2020. Receipt of responses was closed on 31 December 2020. The final analysis comprised 160 respondents, with a 70.2% response rate. Survey completion rate for mandatory questions was 100%. Internal consistency was good (Cronbach's alpha coefficient 0.85).
Participant characteristics
Female CSOs comprised n=105/160 respondents (65.63%; 95% confidence interval (CI) 57.88 - 72.60) v. n=55/160 male respondents (34.37%; 95% CI 27.38 - 42.11). The median age was 27 (interquartile range (IQR) 27 - 28) years. Respondents included participants from 8 medical schools and 33 internship facilities across the country. Undergraduate training of participants predominantly occurred at UKZN (n=66/160; 41.25%; 95% CI 33.83 - 49.09), the University of the Witwatersrand (n=25/160; 15.63%; 95% CI 10.75 - 22.16) and the University of Cape Town (n=20/160; 12.50%; 95% CI 8.18 - 18.64). The other 5 SA universities comprised 4 - 6% of the sample per university. Three-quarters of respondents (n=119/160; 74.37%) completed their internship training in KZN.
Questions related to obstetric surgical training during internship
The HPCSA stipulates that, during internship training, interns need to perform 10 CSs under supervision.[6] Fig. 1 illustrates the number of CSs performed during internship by each respondent.
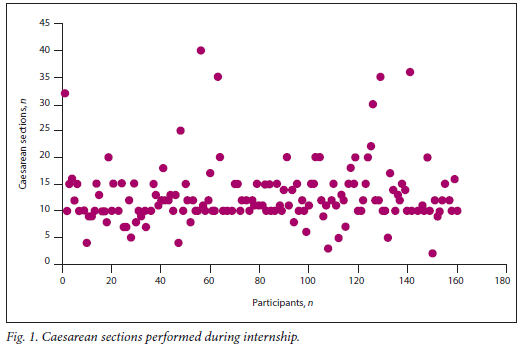
We found that 1 in 8 interns did not complete the stipulated 10 CSs (n=21/160). More than half of respondents (n=92/160; 57.50%; 95% CI 49.66 - 64.97) felt that the number of required CSs should be increased to >10. Only n=57/160 (35.62%; 95% CI 28.54 - 43.39) of participants were supervised in theatre for at least 1 CS by an obstetric specialist. Interns who did not receive specialist supervision, were predominantly supervised by obstetric medical officers (57.50%; 95% CI 49.66 - 64.97) and obstetric registrars (41.25%; 95% CI 33.83 - 49.08). One in 20 interns performed a CS without supervision (n=8/160; 5.00%; 95% CI 2.51 - 9.73). The surgical involvement in different categories of CS and approach to skin incision are shown in Table 1.
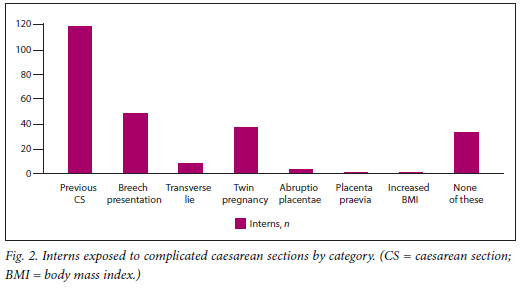
Interns had limited opportunity to be the primary surgeon during complicated CS cases (Fig. 2).
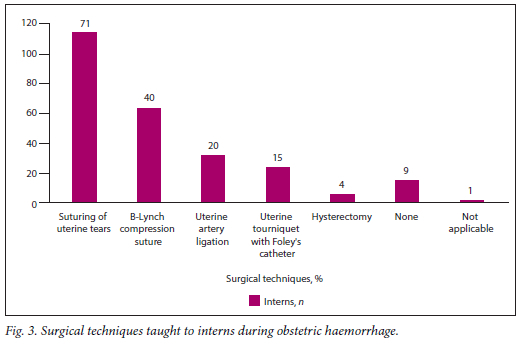
Respondents felt that they had been allowed to manage surgical complications during CS to some extent (median 3; IQR 2-3; Likert scale: 1 = never allowed, 5 = always allowed). However most were not confident regarding their ability to manage obstetric haemorrhage as the primary surgeon during CS (median 2; IQR 2-3; Likert scale: 1 = not confident, 5 = very confident). Specific techniques taught in the management of obstetric haemorrhage are shown in Fig. 3.
The ESMOE (Essential Steps in Managing Obstetric Emergencies) programme was attended in some form by n=147/160 (91.87%; 95% CI 86.45 - 95.24) CSOs. Only n=133/160 participated in the obstetric haemorrhage module, n=77/160 in the surgical skills module and n=61/160 in the anaesthetic module. Of those who participated in ESMOE, 74% found the course beneficial, of whom almost half felt that it was very beneficial.
Despite completing their obstetric rotation, most CSOs did not feel competent to perform CS surgery independently on uncomplicated cases (median 3; IQR 2-3; Likert scale: 1 = not competent, 5 = very competent). Only 48.75% (95% CI 41.03 - 56.52) of interns' surgical skills were formally assessed in theatre prior to being signed off for their rotation. Fewer than half of these interns (46%) were then formally accredited as 'being safe' to perform CSs on completion of their rotation.
Questions related to anaesthetic training during internship
Anaesthetic interns are required to perform 80 procedures under supervision, including at least 40 GA intubated patients, 10 GA non-intubated patients and 10 spinal anaesthesia patients. Most respondents completed this requirement (n=149/160; 93.13%; 95% CI 87.96 - 96.17) and formal assessments were conducted in >90% of interns (in the form of a written test, simulation assessment or a real case in theatre). Most of the in-theatre supervision for obstetric anaesthesia was provided by medical officers, either with a Diploma in Anaesthetics (DA (SA)) (52.50%; 95% CI 44.71 - 60.17) or without a DA (SA) (26.25%; 95% CI 19.97 - 33.67). Almost half of those surveyed had administered anaesthesia for CS without senior supervision (48.75%; 95% CI 41.04 - 56.52). Tutorials and teaching in the anaesthetic rotation were well conducted at internship sites. Only n=3/160 interns received no form of teaching.
Most interns (n=111/160; 69.38%; 95% CI 61.75 - 76.07) experienced a failed spinal anaesthetic during their rotation and only n=10/160 reported receiving no teaching in dealing with this complication. The remaining interns were taught in theatre on a real patient or received simulation training. Exposure to performing difficult spinal anaesthesia, e.g. in obese patients, was high, and most received teaching on the principles of managing spinal anaesthesia.
Almost all interns (n=155/160; 96%) received teaching on the use of vasopressors in the context of spinal anaesthesia and n=138/160 (86%) on the correct use of a wedge. Most interns (85%) were taught how to assess the level of the spinal anaesthesia and n=135/160 (84%) were taught the principles of the management of a high spinal anaesthesia. Similar results were found for teaching received on the principles of obstetric haemorrhage. Teaching occurred by means of real cases (n=47/160), theoretical cases (n=128/160), simulation drills (n=44/160) and informal in-theatre teaching (n=84/160). Interns were also given the opportunity to manage the complications of spinal anaesthesia (median 5; IQR 4-5; Likert scale: 1 = senior always took over, 5 = 1 was always allowed to manage).
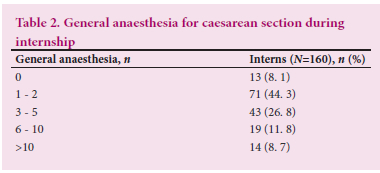
GA for CS exposure was limited (Table 2). Only n=5/160 respondents did not receive teaching on the management of difficult or failed intubation.
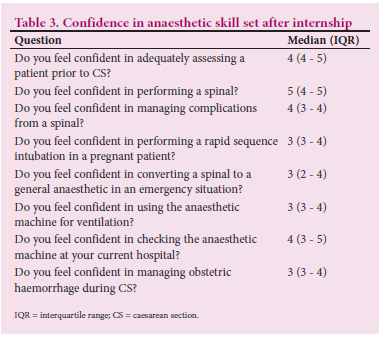
We assessed confidence in anaesthetic skills on completion of the anaesthetic rotation by means of Likert-scale questions (1 = not confident at all, 5 = very confident). Respondents were mostly confident in their abilities (Table 3).
Questions relating to the current situation during the community service year
We asked a limited set of questions related to the current practice of the respondents in KZN. Most CSOs felt that they required further interventions to improve their knowledge and skill set (Appendix B: https://www.samedical.org/file/1799).
Discussion
This survey demonstrated that there are key deficiencies in the current internship training programme. Obstetric training during internship offers insufficient exposure to emergency CS, complicated CS and approaches such as a midline skin incision, where only 1 in 10 respondents had used this approach. Senior supervision is lacking and more than half of respondents did not undergo a formal assessment of their surgical skills. One in 8 doctors did not reach their stipulated number of CSs and more than half felt that this number needed to be increased, which translated into a lack of confidence in their ability to handle obstetric surgical complications. Anaesthetic internship training appears to offer adequate training and exposure to the performance and handling of routine and complicated spinal anaesthesia. However, exposure to GA in obstetrics is lacking, with more than half of respondents performing <3 obstetric GAs during internship.
These findings have particular relevance, given the recent changes to the internship programme. The participants in our study finished their internship prior to these changes and completed a 4-month obstetrics and gynaecology (O&G) rotation. While the anaesthetic component remains a 2-month rotation, the O&G rotation has been shortened from 4 to 3 months. Obstetric surgical exposure during the O&G rotation may consequently be even more inadequate. Even after the 4-month rotation, our study demonstrated a low level of confidence in managing obstetric haemorrhage and insufficient training in the surgical techniques required to manage this problem perioperatively, which will be compounded by a shortened O&G rotation.
It is likely that obstetric surgical training is initiated in stable, elective CS. Once an intern becomes more confident, they generally are permitted to do CSs that need to be performed more speedily (emergency CS) and skilfully (complicated CS). This is necessarily a time-dependent process, and potentially difficult to achieve with a reduction in available time. Emergency CS carries a mortality rate that is more than double that of elective surgery and yet exposure to this category of CS is limited.[4] In our study interns had limited exposure to performing complicated CSs as the primary surgeon. Even at district hospitals, where most CSOs are placed, complicated emergency CSs are likely to occur. Our study revealed that the majority of interns are unprepared for complicated CSs. There was also a poor response to interns being allowed to manage intraoperative complications during CS; they therefore
have a low level of confidence in managing intraoperative obstetric haemorrhage. Bleeding during and after CS accounts for a case fatality rate of 23.6 per 100 000 CSs.[5] Approximately a quarter of maternal deaths after CS at district hospitals is attributed to obstetric haemorrhage during or after CS.[5]
Obstetric emergencies can arise at any time and clinicians need to be adequately prepared to deal with these. The American College of Obstetricians and Gynecologists support the use of simulation-based training and drills to teach and prepare clinicians for emergencies. These drills provide opportunities to practise standardised protocol-driven management of obstetric emergencies. [10] Obstetric simulation training is increasing globally and allows clinicians to train for low-frequency emergencies, such as shoulder dystocia, postpartum haemorrhage (PPH) and cord prolapse. After simulation training, recognition and management of PPH improved, as well as the medical management of the condition.[11] In SA, the ESMOE training course was developed after a key recommendation in the Saving Mothers Report.[5] It is a locally relevant training programme that consists of multiple modules, incorporating lectures, skills demonstrations and skills practice sessions. It includes emergency obstetric scenario simulation training known as 'fire drills'. These fire drills should be integrated into routine clinical practice, and must occur in the labour ward and in the antenatal and postnatal wards. Running these drills in real clinical settings facilitates the participation of more staff, as well as the identification of real problems that could occur in an emergency setting. Interns were the primary target of ESMOE training, as adequate preparation for the management of obstetric emergencies would improve their management of emergencies in their community service year.[12]
The Saving Mothers Report advises on interventions to reduce the MMR, including expansion of the ESMOE programme to incorporate management of bleeding during CS, a CS anaesthetic module and the use of tranexamic acid.[5] ESMOE must be incorporated into the O&G block at all internship training facilities; however, nearly 10% of interns surveyed had no exposure to the programme. While 83% of interns participated in the obstetric haemorrhage module, only 48% participated in the surgical skills module and 38% in the obstetric anaesthesia module. Similar figures were found in another study, showing that only 53% of interns surveyed attended ESMOE.[13] These figures are concerning, given that ESMOE participation is compulsory for interns. Other simple surgical measures that can be taught to doctors performing CS include uterine artery ligation, the B-Lynch suture and the Foley's catheter uterine tourniquet. Uterotonics, tranexamic acid and appropriate use of blood and fresh-dried plasma can be employed to manage bleeding medically.[14] We found that the technique of uterine artery ligation was taught to only 20% of interns, and the Foley's catheter uterine tourniquet to only 15%. These are simple life-saving procedures in the context of CS haemorrhage that all doctors performing CS should be familiar with.
To allow interns to start their surgical obstetric training as soon as possible, they should perhaps participate in a skills 'boot camp' at the start of their rotation. Training could include practical skills such as surgical knot tying and suturing, and simulation-based skills such as management of PPH and B-Lynch sutures. These skills could allow initial orientation and training regarding the essential basic skills, while they could practise and improve on these skills during the remainder of their rotation. Thus, the need would be eliminated for step-wise CS training, where interns are first taught how to close the skin, then the uterus and eventually allowed to perform the CS from start to finish. In surgical disciplines where surgical boot camps are run, participants find the programme valuable and also find that their confidence improves thereafter.[15]
The anaesthetic training was comprehensive and followed up by assessments during the rotation. This finding correlates with that in a study by Bola et al,[16] which reported that anaesthetics was the most supervised rotation during internship and obtained the highest score for departmental teaching. However, it is concerning that practical exposure to GA remains low, especially given the concerns regarding airway management raised in the Saving Mothers Report.[5] Despite this, high scores were obtained in the aspects of management of the maternal airway
With the increasing use of neuraxial techniques as the preferred form of anaesthetic for obstetric patients, interns have limited exposure to GA. A recently published study by Kiwalabye et al.[13] questions if anaesthetic training of interns is satisfactory. The authors assessed interns after completion of their rotation using a high-fidelity difficult obstetric airway simulation - only 40% of interns passed. More than half required a third intubation attempt, only 14% considered the use of a supraglottic rescue device, and one-third did not consider performing a rapid sequence induction. Simulation training is becoming an integral part of medical education. It provides exposure to life-like simulations of procedures/events that occur infrequently in a safe environment, with no impact on patient safety. With the use of simulations, one can develop technical and non-technical skills.[17] To overcome areas where there is lack of training and exposure, simulation training needs to have a larger role in internship training. It provides interns with surrogate training opportunities for rare obstetric events. Possible team simulations can also be performed for obstetric haemorrhage and intraoperative hypotension.[17] Another SA study assessed airway simulation training techniques among interns and it too found higher learner satisfaction, higher acquisition of new skills and improved practical skills in the simulator group compared with the didactic lecture group.[18] It is clear that simulation training has an important role in the development of skills in a fail-safe environment that interns may otherwise have limited exposure to. We determined that simulation training in the approach to a difficult and failed obstetric airway was provided to 40% of interns. This is encouraging, as it demonstrates that simulation-based teaching is becoming part of the anaesthetic internship programme.
To further improve training, we recommend ensuring that second-year interns complete at least 1 month of O&G at district hospital level as part of their 6-month family medicine block. This rotation will compensate for the reduction in the duration of the O&G block in the first internship year, and must include an opportunity to perform CSs at the district hospital under supervision.
Supervisors of internship blocks should not sign off that the intern has completed the block unless the former has verified that the intern has performed the minimum number of procedures required to complete that block. Every intern should ideally be directly supervised by a specialist at least once in the performance of a CS (during both the O&G and anaesthetic blocks). Where this is impossible because there are no specialists at the internship training site, there should be direct supervision by the most senior and experienced doctor. Prior to being signed off for their rotation, all interns need to have their surgical skills formally assessed in theatre by their seniors. If an adequate level has been reached, they should receive accreditation to perform CSs independently when they complete their internship.
Study limitations and strengths
Our study has several limitations. Firstly, it was based on subjective feedback from CSOs, as the data were self-reported, which may introduce bias. Additionally, assessment of confidence levels regarding knowledge and skills does not necessarily translate into clinical competence. However, much of the supporting data are quantitative and supportive of the subjective components. Our participants underwent internship training mainly in KZN, and undergraduate training mainly at UKZN. This may result in reduced national generalisability, particularly with regard to internship training. Strengths of the study include a very good response rate (>70%), and representation from all 8 medical schools and 33 internship training facilities in SA.
Conclusions
This survey showed that there are deficiencies in the implementation of the existing internship training programme that impact on the confidence and skill sets of CSOs in SA to perform CSs. A lack of exposure to adequate obstetric surgical training and obstetric GA is likely to impact on the performance of these CSOs in district hospitals nationally and on the safety of the CS service provided at district hospitals. Recent changes to the internship programme might compound these problems. The intern training programme requires strict compliance and should be enhanced to improve the competence of CSOs, e.g. by including simulation training, basic surgical skills courses and prioritisation of exposure to complicated surgical scenarios.
Declaration. The research for this study was done in partial fulfilment of the requirements for LT's MMed (Anaesthetics) degree at the University of KwaZulu-Natal, Durban, SA.
Acknowledgements. We would like to acknowledge Dr Zane Farina for his assistance in the composition and completeness of the survey.
Author contributions. LT contributed to the conceptualisation, design, analysis and interpretation of data, drafted the manuscript and approved the final version for publication. DGB contributed to the conceptualisation, design, primary statistical analysis and interpretation of data, manuscript revisions and approval of the final version for publication. NM contributed to the conceptualisation and design, critical revision of important scientific content, manuscript revisions and approval of the final version for publication.
Funding. None.
Conflicts of interest. None.
References
1. World Health Organi2ation. Strategies toward ending preventable maternal mortality (EPMM). 2015 https://www.who.int/topics/sustainable-development-goals/targets/en/ (accessed 7 April 2021). [ Links ]
2. Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 2016:387(10017):462-474. https://doi.Org/l0.1016%2Fs0140-6736%2815%2900838-7 [ Links ]
3. Bishop D, Dyer RA, Maswime S, et aL Maternal and neonatal outcomes after caesarean delivery in the African Surgical Outcomes Study. A 7-day prospective observational cohort study Lancet Glob Health 2019;7(4):e513-e522. https://doi.org/10.1016/S2214-109X(19)30036-1 [ Links ]
4. Sobhy S, Zamora J, Dharmarajah K, et al. Anaesthesia-related maternal mortality in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Glob Health 2016;4(5):e320-e327. https://doi.org/10.1016%2Fs2214-109x%2816%2930003-l [ Links ]
5. National Committee on Confidential Enquiries into Maternal Deaths. Seventh Triennial Report on Confidential Enquiries into Maternal Deaths in South Africa, 2017 - 2019. Pretoria: National Department of Health, 2019. [ Links ]
6. Medical and Dental Professions Board. Handbook on Internship Training. Guidelines for Interns, Accredited Facilities and Health Authorities. Pretoria: Health Professions Council of South Africa, 2021. [ Links ]
7. Kusel B, Farina Z, Aldous C. Anaesthesia training for interns at a metropolitan training complex: Does it make the grade? S Afr Fam Pract 2014;56(3):201-205.https://doi.org/10.1080%2F20786204.2014.936664 [ Links ]
8. Nkabinde TC, Ross A, Reid S, Nkwanyana NM. Internship training adequately prepares South African medical graduates for community service - with exceptions. S Afr Med J 2013;103(12):930-934. https://doi.org/10.7196%2Fsamj.6702 [ Links ]
9. Farina Z, Rout C. 'But it's just a spinal': Combating increasing rates of maternal death related to spinal anaesthesia. S Afr Med J 2013;103(2):81-82. https://doi.org/10.7196/samj.6308 [ Links ]
10. Committee Opinion No. 590. Preparing for clinical emergencies in obstetrics and gynecology Obstet Gynecol 2014;123(3):722-725. https://doi.org/10.1097%2F01.aog.0000444442.04111.c6 [ Links ]
11. Lawson W, Smith M, McCue B. Ochsner obstetrics and gynecology simulation program: A review of the literature and description of a multidisciplinary simulation program targeting management of obstetric emergencies. Ochsner J 2020;20(4):394-399. https://doi.org/10.31486%2Ftoj.20.0014 [ Links ]
12. Moran NF, Naidoo M, Moodley J. Reducing maternal mortality on a countrywide scale: The role of emergency obstetric training. Best Pract Res Clin Obstet Gynaecol 2015;29(8):1102-1118. https://doi.org/10.1016%2Fj.bpobgyn.2015.08.002 [ Links ]
13. Kiwalabye I, Cronjé L, Schoeman S, Sommerville T A simulation-based study evaluating the preparedness of interns' post-anaesthesia rotation in managing a failed obstetric intubation scenario: Is our training good enough? S Afr Med J 2021;111(3):265-270. https://doi.org/10.7196%2Fsamj.2021.V111i3.14443 [ Links ]
14. Sobhy S, Arroyo-Manzano D, Murugesu N, et al. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: A systematic review and meta-analysis. Lancet 2019;393(10184):1973-1982. https://doi.org/10.1016%2Fs0140-6736%2818%2932386-9 [ Links ]
15. Fernande2 GL, Page DW, Coe NP, et al. Boot camp: Educational outcomes after 4 successive years of preparatory simulation-based training at onset of internship. J Surg Educ 2012;69(2):242-248. https://doi.org/10.1016%2Fj.jsurg.2011.08.007 [ Links ]
16. Bola S, Trollip E, Parkinson F. The state of South African internships: A national survey against HPCSA guidelines. S Afr MedJ 2015;105(7):535-539. https://doi.org/10.7196%2Fsamjnew.7923 [ Links ]
17. Yunoki K, Sakai T. The role of simulation training in anesthesiology resident education. J Anesth 2018;32(3):425-433. https://doi.org/10.1007%2Fs00540-018-2483-y [ Links ]
18. Moodley T Gopalan D. Airway skills training using a human patient simulator. South Afr J Anaesth Analg 2014;20(3):147-151. https://doi.org/10.1080%2F22201173.2014.936778 [ Links ]
 Correspondence:
Correspondence:
L Temlett
leannetemlett@gmail.com
Accepted 3 November 2021














