Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Obstetrics and Gynaecology
versão On-line ISSN 2305-8862
versão impressa ISSN 0038-2329
SAJOG vol.27 no.1 Cape Town Abr. 2022
http://dx.doi.org/10.7196/SAJOG.2022.v27i1.2066
RESEARCH
Diathermy v. scalpel Pfannenstiel incision in repeated caesarean sections: A randomised controlled trial
A A-MageedI; I A El-FotohI; R FouadI; N GamalII; E N SalamaIII; M Abdel-RasheedIII; D FaroukI
IMD; Department of Obstetrics and Gynecology, Faculty of Medicine, Cairo University, Egypt
IIMSc; Department of Obstetrics and Gynecology, Defense Industrial Medical Centre, Cairo, Egypt
IIIPhD; Department of Reproductive Health Research, National Research Centre, Cairo, Egypt
ABSTRACT
BACKGROUND. Most surgeons do not choose diathermy over scalpel skin incision, as they speculate that the thermal effect produced owing to tissue resistance to electrical current may lead to postoperative pain, delayed wound healing and wound complications.
OBJECTIVE. To compare the use of cutting diathermy skin incision with scalpel skin incision with regard to incision time, haemostasis, postoperative pain, wound healing and wound complications.
METHODS. A randomised controlled trial was performed on 476 women who underwent caesarean sections. They were randomised into two groups: group 1 (women scheduled for conventional scalpel skin incision) and group 2 (women scheduled for cutting diathermy skin incision).
RESULTS. The incision time, blood loss, visual analogue scale (VAS) pain score and doses needed for analgesia were significantly lower in group 2 than in group 1 (p<0.001). The groups did not show any significant difference regarding wound complications. Wound healing in both groups was by primary intention.
CONCLUSIONS. Diathermy skin incision is superior to scalpel skin incision, with no postoperative pain and good wound healing.
Caesarean section (CS) is a major surgical procedure that is frequently performed worldwide. Anaesthetic and antiseptic measures have been advanced to an extent that allows obstetricians to focus on finding improved techniques to be performed in CS.[1] Surgeons have developed different operative techniques for uterine and skin incision, which have changed over time.[2]
Since 1929, electrosurgery has been used widely. It has now become one of the essential tools during surgical procedures in most specialties. After introducing halothane, electrosurgery was used to maintain haemostasis and to control bleeding[3,4] It has been used in different specialties, such as dermatological, otorhinolaryngological, cardiac, plastic, orthopaedic, urological, ocular, neurological and general surgery.[5] Although diathermy was widely performed in operating theatres globally, few surgeons used it to make skin incisions. The belief that diathermy increases devitalised tissue of the wound, which may lead to delayed wound healing, wound infection and scar formation, was behind the lack of surgeons' preference towards diathermy skin incisions[6] However, the introduction of pure sinusoidal current delivered by oscillator units has increased interest in electrosurgery[3,7]
Post-CS pain comprises a set of pain pathways that originate mainly from somatic and visceral sources, but also from psychosocial factors. Somatic pain is characterised by localisation and fades within 2 - 3 days. Electrical and chemical activities in the nerves, stimulated by tissue damage, lead to pain perception. The manipulation of abdominal organs and the peritoneum during an operation, as well as the uterine involution process (after pain), stimulated visceral pain[8] Visceral pain is characterised as being diffuse and extended. Complete uterine involution is reached ~2 weeks after CS. Another important factor is psychosocial pain, which can aggravate pain perception and may stimulate the chemical neurotransmitters of pain.[9]
This study was performed to compare skin incision methods to determine differences in postoperative pain, haemodynamic changes, incisional time, blood loss during incision, wound healing and wound complications.
Methods
This randomised controlled clinical trial was carried out at the Department of Obstetrics and Gynecology, Kasr El-Ainy Hospital, Cairo, Egypt, between May 2019 and December 2020, after being approved by the Research Ethics Committee of the Faculty of Medicine, Cairo University (ref. no. MS-242-2019). All women admitted to the hospital were informed regarding the nature of the study. Written consent was obtained from all the women included in the study.
The inclusion criteria were: women with a history of only one previous CS, age 18 - 40 years, gestational age 38 - 41 weeks and body mass index (BMI) <30 kg/m2. Women were excluded if they had a medical disorder that could affect wound healing, such as diabetes, chronic anaemia, chronic skin conditions, history of allergy or history of an infected surgical wound. Women who underwent primary or emergency CS, cardiac patients with pacemakers, patients on anticoagulants, or women refusing to participate in the study were also excluded.
Study participants were randomly allocated to group 1 (women who received conventional scalpel skin incision) and group 2 (women who received cutting diathermy skin incision). Randomisation was done using computer-generated random sequence numbers. We standardised the surgical procedures. Surgery in both groups was similarly performed by two surgeons with comparable surgical skills, who were evaluated in a previous training programme. CS in both groups was done under spinal anaesthesia. Evaluation of pain and wound complications in both groups were standardised using a visual analogue scale (VAS) scoring system.
A Pfannenstiel skin incision was performed through the subcutaneous tissue and the rectus sheath, and dissected from rectus muscle until the peritoneum was exposed. In the scalpel group, the incision was made by the traditional method, with proper haemostasis, by applying pressure to cutaneous blood vessels and ligating the subcutaneous vessels. In the diathermy group, the incision was made using a small flat blade pen electrode, set on cutting mode and delivering a 120 watt (maximum) sinusoidal current, with electrosurgical cutting performed without pressure or mechanical displacement. We compared incision time using a digital clock. The incision time was established as follows: when a skin incision was made, the surgeon called out, 'start the clock'. Once the rectus sheath was visualised, the surgeon called out, 'stop the clock'. The incision time was the difference between start and stop.
We also compared the incision blood loss. This was calculated by pre- and postoperative weighing of the swabs (1 mg = 1 mL) after complete haemostasis had been achieved. No suction device was used in the incision site. Women in both groups received pethidine 50 - 100 mg intramuscularly in the operating theatre. Closure of the skin in all CSs was done by using polypropylene 2.0 sutures in a subcuticular technique, followed by disinfecting the wound with povidone-iodine (Betadine), drying it with sterile gauze and then covering it with a sterile self-adhesive non-woven dressing with an absorbent pad.
Postoperatively, women in both groups received parenteral paracetamol every 8 hours. All dressings were inspected on postoperative day 5 or earlier, if required, to check for complications, followed by disinfecting and covering the wound using the same procedure. We compared the patients clinically with regard to postoperative pain for 24 hours by VAS score, a psychometric response scale. It is an instrument used to measure subjective characteristics or attitudes that cannot be measured directly. The scale ranges from 0 (one pain extreme, e.g. no pain) to 10 (the other pain extreme, e.g. pain as bad as can be imagined or worst pain imaginable). This score was recorded for each participant at 2, 4, 6, 8, 10,12 and 24 hours postoperatively.
Lastly, we compared both groups with regard to wound healing and complications, such as seroma, haematoma, ecchymosis, dehiscence (separation of the subcutaneous tissues and skin) and infection.
Sample size calculation
We calculated that the minimum appropriate patient sample size was 227 to reject the null hypothesis, with 95% power at a=0.05 level using one-way analysis of variance (ANOVA), and the test ratio between the two groups being 1:1. An accommodated 5% drop-out rate with sample size calculation was done using OpenEpi version 3 (www.openepi.com) open-source calculator (mean sample size).
Statistical analysis
Data were analysed with SPSS version 25 (IBM Corp., USA). Normally distributed quantitative variables were expressed as mean (standard deviation (SD)), while non-normally distributed variables were expressed as median (interquartile range (IQR)). Qualitative variables were expressed as numbers and percentages. To compare group 1 (skin incision with a scalpel) with group 2 (skin incision with diathermy), we used the independent sampled i-test for normally distributed variables and the Mann-Whitney test for non-normally distributed variables. The p-value was considered significant if p<0.05 and highly significant if p><0.001.
Results
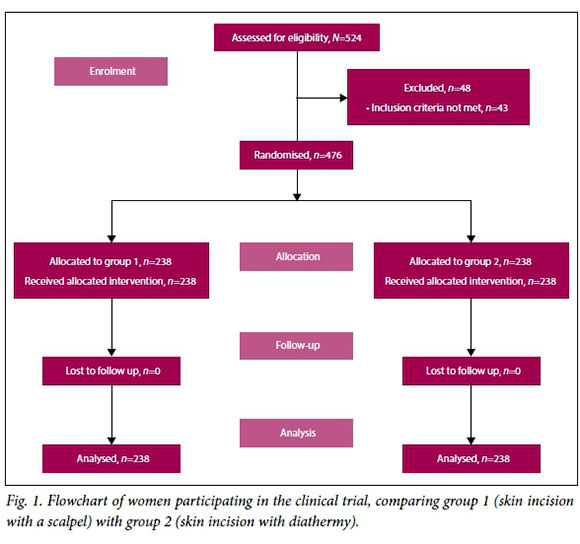
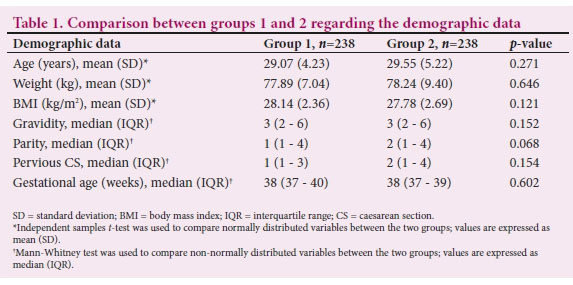
Following the CONSORT (Consolidated Standards of Reporting Trials) recommendations, we assessed 524 women who underwent elective CS. We excluded 48 women from the study: 5 declined to participate, while the remaining 43 did not meet the eligibility criteria (Fig. 1). Regarding the participants' baseline characteristics, their mean age was 29.31 (5.4) years and their mean BMI was 27.96 (2.8) kg/m2. According to the Pfannenstiel skin incision method, they were divided into two groups: group 1 (women who underwent skin incision with a scalpel) and group 2 (women who underwent skin incision with diathermy). When comparing the demographic data, the groups showed no significant difference regarding age, weight, BMI, gravidity, parity, history of previous CS and gestational age at delivery (Table 1).
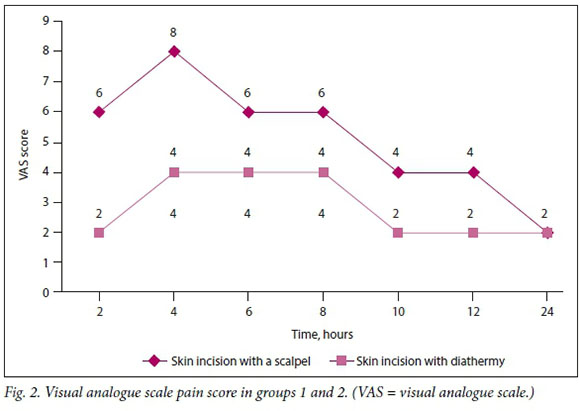
The incision time, blood loss, analgesic doses, wound healing, wound complications and VAS pain score 24 hours postoperatively were evaluated for both groups. Group 2 showed significantly lower incision time, blood loss, doses needed for analgesia and VAS pain score than group 1 (p><0.001). Fig. 2 displays the VAS pain score for both groups during the 24 hours after the operation. Wounds healed by primary intention in all women in both groups, who did not show any significant difference regarding wound complications (Table 2).
Discussion
Recently, after the introduction of advanced electrocautery units, there has been an increased tendency towards the use of diathermy for skin incisions.[11] We investigated the incision time, blood loss, analgesia doses, VAS pain score, wound healing and wound complications when cutting diathermy was used in skin incisions.
As in other studies, a statistically significant shorter incision time and less blood loss were biased toward diathermy v. scalpel.1111 To reach haemostasis with a scalpel incision, surgeons needed multiple sutures, many instruments and coagulation diathermy, especially with subcutaneous tissue. Such haemostatic procedures take longer to perform with a scalpel than with diathermy. Many studies have reported less blood loss with diathermy incision than with scalpel incision.[10,12,13] This result could be due to the coagulative effect of diathermy, which plays an essential role in keeping the area of incision haemostatic. However, Prakash et al.[[12] found no difference regarding incision time. This inconsistency could be owing to the difference in skin incision type, as they studied midline skin incision - not Pfannenstiel skin incision.
Incisions made with cutting diathermy showed a significant difference on the first postoperative day VAS pain score compared with scalpel incisions. This finding is consistent with the results of two meta-analyses[12] In our study, we recorded significantly reduced postoperative pain in the diathermy group. On the first postoperative day, we monitored pain every 2 hours and found the same results as other researchers. Some researchers concluded that total or partial injury to the cutaneous nerves in the surgical skin wound by diathermy showed reduced postoperative pain.[14] Yet we believe that diathermy ablation may lead to disruption of nerve impulse transmission owing to localised sensory nerve destruction. The use of pure sinusoidal current causes cell vaporisation and immediate nerve necrosis, without markedly affecting the nearby structures.
Many studies assessed electrocautery v. use of a scalpel in midline incisions, but few investigated electrocautery use in transverse incision surgery.141 The latter could affect the results regarding healing and wound complications but, as in many studies, our study did not find any significant differences regarding postoperative wound healing or complications.[10,15,16] The prophylactic use of antibiotics might theoretically decrease the wound infection rate, but not bacterial colonisation. Many studies commented on wound healing and complications. Cruse and Foord[17] were the first to observe a significant relationship between wound infections and diathermy use, which they attributed to a sizeable quantity of necrotic burnt tissue left in the wound. Later, Cruse and Foord1171 acknowledged that with less destructive tissue, the infection rate in women after surgery was the same if diathermy was used/not used. Most later studies found no statistical difference in wound infection between cutting diathermy and scalpel surgery.[1820] However, Amin et al[211]reported that wound healing complications were related to diathermy incision wounds in more instances. Soballe et al[22]found a high incidence of wound infection with diathermy incisions, indurated margins and durability of the incision site compared with scalpel use.
Cutting diathermy in caesarean skin incision has shown shorter incisional time, reduced incisional blood loss and less postoperative pain than scalpel skin incision. Neither scalpel nor diathermy incisions showed any significance towards the rate of wound healing and complications.
Conclusions
The use of cutting diathermy in caesarean skin incision is superior to scalpel skin incision regarding incision time, haemostasis, postoperative pain and wound healing. Also, the diathermy skin incision showed fewer wound complications.
Declaration. None.
Acknowledgements. We would like to thank our colleagues from the Faculty of Medicine, Cairo University, who provided insight and expertise that greatly assisted our research.
Author contributions. IAE-F and AA-M: conceived and designed the study; DF and NG: collected the data; MA-R and ENS: analysed and interpreted the data; all authors contributed to writing of the manuscript and approved the final version.
Funding. None.
Conflicts of interest. None.
References
1. Elbohoty AE, Gomaa MF, Abdelaleim M, et al Diathermy versus scalpel in transverse abdominal incision in women undergoing repeated cesarean section: A randomised controlled trial J Obstet Gynaecol Res 2015;41(10):1541-1546. https://doi.org/10.1111/jog.12776 [ Links ]
2. Dahlke JD, Mendez-Figueroa H, Rouse DJ, et al. Evidence-based surgery for cesarean delivery: An updated systematic review. Am J Obstet Gynecol 2013;209(4):294-306. https://doi.org/10.1016/j.ajog.2013.02.043 [ Links ]
3. Kearns S, Connolly E, McNally S, et al Randomised clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg 2001;88(1):41-44. https://doi.org/10.1046/j.1365-2168.2001.01625.x [ Links ]
4. Club DHRJ. Randomised clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg 2001;88(1):1129. [ Links ]
5. Dodde RE, Bull JL, Shih AJ. Bioimpedance of soft tissue under compression. Physiol Measure 2012;33(6):1095. [ Links ]
6. Patil VB, Mule VD, Raval RM, et al Observational study of scalpel versus electrocautery for subcutaneous incision in elective gynaecological surgeries. Int J Reprod Contracept Obstet Gynecol 2017;6(3):950-954. [ Links ]
7. Feldman L, Fuchshuber P, Jones DB. The SAGES Manual on the Fundamental Use of Surgical Energy (FUSE). New York: Springer, 2012. [ Links ]
8. Bourne S, Machado AG, Nagel SJ. Basic anatomy and physiology of pain pathways. Neurosurg Clin N Am 2014;25(4):629-638. https://doi.org/10.1016/j.nec.2014.06.001 [ Links ]
9. Chin EG, Vincent C, Wilkie D. A comprehensive description of postpartum pain after cesarean delivery. J Obstet Gynecol Neonatal Nurs 2014;43(6):729-741. https://doi.org/10.1111/1552-6909.12483 [ Links ]
10. Aird LN, Brown CJ. Systematic review and meta-analysis of electro cautery versus scalpel for surgical skin incisions. Am J Surg 2012;204(2):216-221. https://doi.org/10.1016/j.amjsurg.2011.09.032 [ Links ]
11. Priya N, Lamture Y, Luthra L. A comparative study of scalpel versus surgical diathermy skin incisions in clean and clean-contaminated effective abdominal surgeries in AVBRH, Wardha, Maharashtra, India. J Datta Meghe Inst Med Sci Univ 2017;12(1):21. https://doi.org/10.4103/jdmimsu.jdmims u_15_17 [ Links ]
12. Prakash LD, Balaji N, Kumar SS, et al. Comparison of electrocautery incision with scalpel incision in midline abdominal surgery - a double blind randomised controlled trial. Int J Surg 2015;19:78-82. https://doi.org/10.1016/j.ijsu.2015.04.085 [ Links ]
13. Nandurkar VS, Prakash M, Suma S. Diathermy versus scalpel incisions in elective abdominal surgery: A comparative study. Int Surg J 2018;5(9):3124-3128. https://doi.org/10.18203/2349-2902.isj20183734 [ Links ]
14. Chrysos E, Athanasakis E, Antonakakis S, et al. A prospective study comparing diathermy and scalpel incisions in tension-free inguinal hernioplasty. Am Surg 2005;71(4):326-329. https://doi.org/10.1177/000313480507100410 [ Links ]
15. Bostanci EI, Guler I, Akdulum FC, et al Electrocautery versus scalpel in women undergoing primary cesarean section and neonatal outcomes. Gynecol Obstet Reprod Med 2020;26(3):184-187. https://doi.org/10.21613/GORM.2019.921 [ Links ]
16. Mukherjee MP, Patole MM. Scalpel versus diathermy skin incision: A randomised clinical trial. Int Surg J 2019;7(1):258-262. https://doi.org/10.18203/2349-2902.isj20195981 [ Links ]
17. Cruse PJ, Foord R. The epidemiology of wound infection: A 10-year prospective study of 62 939 wounds. Surg Clin North Am 1980;60(1):27-40. https://doi.org/10.1016/s0039-6109(16)42031-1 [ Links ]
18. Kearns S, Gilmore M, McCabe J, et al. Diathermy versus scalpel incisions for hemiarthroplasty: A randomised prospective trial. Bone Joint J 2004;86:129. [ Links ]
19. Eren T, Balik E, Ziyade S, et al. Do different abdominal incision techniques play a role in wound complications in patients operated on for gastrointestinal malignancies? Scalpel vs. electro cautery. Acta Chir Belg 2010;110(4):451 -456. https://doi.org/10.1080/00015458.2010.11680654 [ Links ]
20. Ahmad NZ, Ahmed A. Meta-analysis of the effectiveness of surgical scalpel or diathermy in making abdominal skin incisions. Ann Surg 2011;253(1):8-13. [ Links ]
21. Amin M, Nadeem K, Aziz I. Randomised comparative study of electrosurgical and conventional scalpel incisions in general surgery. Surgery 2010;20(25):15-22. [ Links ]
22. Soballe PW, Nimbkar NV, Hayward I, et al Electric cautery lowers the contamination threshold for infection of laparotomies. Am J Surg 1998;175(4):263-266. https://doi.org/10.1016/s0002-9610(98)00020-8 [ Links ]
 Correspondence:
Correspondence:
E N Salama
drehabnrc@gmail.com
Accepted 6 December 2021














