Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Libraries and Information Science
On-line version ISSN 2304-8263
Print version ISSN 0256-8861
SAJLIS vol.87 n.2 Pretoria 2021
http://dx.doi.org/10.7553/87-2-1835
RESEARCH ARTICLES
Change management in the implementation of electronic health records (EHR) systems at Inkosi Albert Luthuli Central Hospital, South Africa
Mandisa MsomiI; Trywell KalusopaII; Lungile Precious LuthuliIII
ILecturer in the Department of Information Science, University of South Africa. mandisamsomi89@gmail.com ORCID: 0000-0002-5751-9765
IIAssociate Professor (Records & Archives Management), University of Namibia. tkalusopa@unam ORCID: 0000-0001-9331-1307
IIILecturer in the Department of Information Studies, University of Zululand, South Africa. ngidil@unizulu.ac.za ORCID: 0000-0002-4310-8148
ABSTRACT
For decades, public hospitals have relied on managing records manually using different formats of classification. However, driven by an eHealth strategy, hospitals in South Africa are now changing to electronic health records (EHR) systems for their day-to-day functioning. Earlier studies conducted on health records management in the South African provinces of KwaZulu-Natal (KZN), Limpopo, Eastern Cape, Gauteng and Western Cape, all point to minimal evidence of change management in EHR system implementation in public hospitals. This paper presents empirical results of an investigation into the management of change in the implementation of an EHR system at the Inkosi Albert Luthuli Central Public Hospital in the eThekwini area of KZN. The findings show that an ill-defined change management approach in the EHR system implementation hinders the progress of the implementation and thus the improvement of health service delivery. The study recommends that the implementation of a robust and functional EHR system be accompanied equally by a viable, parallel and executable change management blueprint.
Keywords: Change management, electronic health records system, health information technology, EHR, Inkosi Albert Luthuli Central Hospital, public hospital.
1 Introduction
Most hospitals in South Africa have relied on managing records manually using different formats of classification (Msomi 2020). However, recently, hospitals have been changing to electronic health records (EHR) systems for their day-to-day functions in order to provide better service delivery. As Schutzbank and Fernandopulle (2014: 14) declared, the "digital age of medicine is upon us". The efficient adoption and implementation of an EHR system depends on understanding the factors contributing to and influencing change management. EHR systems are designed to preserve the structure of records and to validate their content and framework and the interactions between them to facilitate accessibility and sustain value for hospital referrals (Hoffman & Podgurski 2008). Challenges facing the South African public health sector in records management have been extensively examined by different authors (Luthuli 2017, Thomas 2016, Erasmus & Van der Walt 2015, Katuu 2015, Weeks 2013, Marutha 2011, O'Mahony 2009) and common issues have been revealed, including misfiled or missing files, duplication of files, illegal access and destruction of records, long waiting times to receive medical attention, limited human resources, poor handwriting and more. The authors endorsed the execution and use of an EHR system. Although Marutha and Ngoepe (2018) suggested a medical records management framework that could assist public hospitals to implement successful record keeping, in-depth concerns about managing change in the implementation process were not fully considered. Change management has become a requirement for organisations that are incorporating the use of Information and Communication Technology (ICT) for effective service delivery. The term 'change management' refers to the process of implementing plans for change that lead to the desired results based on an initial motive or need or on the urgency of the situation (Hayes 2014).
This study sought to examine change management in EHR system implementation at Inkosi Albert Luthuli Central Public Hospital. The Inkosi Albert Luthuli Central Hospital is located in the eThekwini area of KwaZulu-Natal (KZN) in Vusi Mzimela Road, Cator Manor, Durban, with the N2 to the west and M10 to the east. It is a tertiary and quaternary hospital and patients are referred from other hospitals via an electronic telephone booking system. The hospital offers primary care services such as radiology and pathology, and it consists of medical, surgery, perioperative care, mother and child, and professions allied to medical support (PAMS) departments. Inkosi Albert Luthuli Central Hospital is the first hospital in Africa to deploy the MEDITECH 6.1.5 platform, the EHR system that assists with hospital administration. The system helps to manage information for HIV and TB-related treatment; care and support services for terminally and chronically ill patients; treatment of mental illnesses; services for pregnant women; and it offers facilities for handling medical assessments and referrals (MEDITECH 2018). The 846-bed Inkosi Albert Luthuli Central Hospital implemented the MEDITECH system in August 2016 to replace the workflow system that was previously used.
2 Problem statement
The overall problem is that, for many years, South Africa has been attempting to implement EHR systems in both public and private hospitals yet concerns and issues of managing change in the implementation have not been fully addressed. Even though several previous studies (Luthuli 2017, Marutha 2016, Thomas 2016, Katuu 2015, Marutha& Ngulube 2012, Weeks 2012) pointed out the necessity of implementing EHR systems to improve health service delivery in South Africa, the question regarding management of change has not been fully examined. There is no notable evidence regarding management of change in the KZN setting or specifically at Inkosi Albert Luthuli Central Hospital. For example, Luthuli (2017), in a comparative analysis of public and private hospitals in KZN, acknowledged the need for ICT integration to improve management of health records for public health service delivery but did not examine change management in this integration process. Likewise, Marutha (2012) focused on the assessment of medical records management in healthcare service delivery in Limpopo Province and mentioned the need for adopting EHR systems to ensure successful delivery of health services, but the research falls short of recommending change management strategies in systems implementation. Thomas (2016) examined the EHR system implementation in primary healthcare and underscored the high degree of change that should be managed during pre- and post-adoption of the EHR systems. The study was restricted to primary healthcare and it did not focus on the issues regarding change management in the implementation of EHR systems. Weeks (2012) indicated that human socio-technology factors in changing to EHR systems needed to be actively managed, yet the researcher did not look in detail into how those factors could be addressed.
The existing literature reveals little evidence of empirical studies conducted on change management in the implementation of EHR systems in South Africa, particularly in KZN (Msomi 2020). This study sought to evaluate change management orientation in the operation of EHR systems in the eThekwini area, with specific reference to Inkosi Albert Luthuli Central Hospital. It is anticipated that it will contribute to the development of an EHR system framework that supports successful implementation of health information technology to improve healthcare service delivery. This study will provide some insights into management of change to healthcare professionals, hospital management, ICT experts and records management personnel in the integration of ICT for the improvement of healthcare and service delivery.
3 Aim of the study
The main purpose of this study was to assess change management in the implementation and operation of an EHR system at Inkosi Albert Luthuli Central Hospital, eThekwini Municipality.
4 Objectives of the study
The following were research objectives for the study:
• To determine factors facilitating the adoption of an EHR system at Inkosi Albert Luthuli Central Hospital.
• To assess changes experienced by the hospital due to the implementation of an EHR system.
• To examine how the hospital monitors and evaluates the impact of the EHR system implementation.
• To determine the tools used by hospital leadership to reinforce change and sustain results.
5 Literature review
Like most developing countries, South Africa is in the process of improving health information management by means of technology application. The National Health Act (Act 61 of 2003) by the National Department of Health of South Africa has the statutory mandate to facilitate and coordinate the establishment, implementation and sustainability of comprehensive health information systems across national, provincial and local levels, including in the private health sector, with the aim of using healthcare information technology as a means of increasing access to healthcare services and improving level of care.
5.1 Factors facilitating the adoption of an EHR system at Inkosi Albert Luthuli Central Hospital
In South Africa, the public sector has recognised the need for and importance of developing EHR systems. Marutha and Ngulube (2018) indicated the significance of implementing EHR systems in public hospitals to make certain improvements in records management. Electronic health records are digital versions of patients' collected information that is available instantly and securely to authorised users (Katuu 2015). Putting EHR systems into practice appears to be a serious challenge in the public health sector (Marutha & Ngulube 2012). Although EHR systems have been executed in other hospitals in South Africa, half of the public health sector still make use of manual record administration and management (Katurura & Cilliers 2018: 2). The implementation of an EHR system assists decision-making by allowing hospitals to share updated patient information and access medical histories (Katurura & Cilliers 2018: 1).
5.2 Changes experienced by hospitals due to implementation of EHR systems
Change management is regarded as an essential process in the development of an EHR system (Nguyen 2009). It is in that regard that change management remains a central ingredient for the successful implementation of EHR systems in South Africa (Marutha 2016, Katuu 2015). The adoption of EHR systems in South Africa is driven by an eHealth strategy that regulates the use of ICT for health purposes (Department of Health 2012). The National eHealth Strategy in South Africa is set to lead to improving patient information systems nationwide (Health-e News 2014). One of the aims of the eHealth strategy of South Africa is to lay a foundation for future incorporation and coordination of eHealth initiatives in the public and private health sectors (Department of Health 2012: 8). The eHealth Strategy supports the effective adoption and successful implementation of ICT in records management (Erasmus & Van der Walt 2015: 187). Fast technological changes and improvements have influenced the way the corporate world functions in the public and private sector (Shonhe 2017: 19). Thomas (2016) indicated that the use of technology alone remains inadequate in guaranteeing successful EHR system implementation in hospitals. The National Archives of Australia (2011: 8) supports the opinion that the implementation of an electronic records management system in any organisation, including public hospitals, does not solve all information management problems.
5.3 Monitoring and evaluating the impact of EHR system implementation
Many organisations in the health sector internationally have progressed to electronic records management systems in hospitals and they acknowledge that change management is vital for the effective management of electronic records. In South Africa, however, the importance of change management has not been provided for, as is evident in inadequate directives provided by the National Archives of South Africa on change management in electronic records management systems. The National Archives of Australia (2011: 13) identifies change management as the key consideration for implementing electronic records systems and attests that introducing electronic records management systems needs to be undertaken as part of a larger change management movement. It further points out that developing innovative systems with which individuals are not familiar unavoidably creates concerns about how effective and reliable the new system will be (National Archives of Australia 2011). Some of these concerns are based on the following:
• effectiveness of the information retrieval tool;
• protection and confidentiality of sensitive information;
• the flexibility of the system, its user friendliness and efficiency; and
• impact when the system goes offline (National Archives of Australia 2011: 13)
The aforementioned concerns need to be part of the change management project to prevent EHR system failure. All the perceived concerns and issues about the former system also need to be addressed before implementing innovations to manage the change successfully. Marutha and Ngulube (2012) focused on the implementation of EHR systems in the public health sector and underscored that hospitals were not properly taking advantage of information technology (IT) to support health service delivery. Implementing EHR systems in the hospital setting required more effort to reshape the mindset of healthcare professionals towards change and progressive processes (Weeks 2013). This includes reviewing and upgrading organisational tools to support users and to provide skills development to guide all parties involved in the digital evolution (National Archives of Australia 2011). EHR systems are complex to implement owing to the human capital mindset, electronic records management system identification, and organisational culture (Marutha 2016). According to National Archives of Australia (2011: 8), "maximising the potential benefits requires improvement in business processes and change in people's behaviour". Although EHR systems have been implemented in some areas of South Africa, more than half of the public health sector still makes use of paper-based record keeping (Katurura & Cilliers 2018: 2). Hence, there is a necessity to understand EHR system adoption from a South African public health perspective (Thomas 2016: 37). Unfortunately, ICTs are introduced in hospitals without crucial processes and procedures to control access to electronic records management systems (Marutha 2011: 32). It is in this regard that change management has become a necessity for public health organisations integrating the use of ICT to deliver health services. Management of change minimises occurrences that can lead to failure or the ineffectiveness of the ICT implementation.
6 Theoretical framework
The study adopted the Leading Change model integrated with the Technology Acceptance model (TAM). The study triangulated the Leading Change model with the TAM in order to understand various factors that influence implementation, acceptance, use and benefits of the EHR system at Inkosi Albert Luthuli Central Hospital. Triangulation theory involves at least two set theories interpreting a single dataset (Saldana & Omasta 2017). The models were chosen based upon the study of Martin and Voynov (2014) that utilised the Leading Change model with TAM to assess the implementation and operation of EHR systems in physicians' practices. Both models allowed the researchers to gain an insight into the pre- and post-implementation functioning and acceptance of the EHR system. Even though this EHR system implementation was done many years ago, its results are still relevant currently. The Leading Change and TAM models also evaluated the changing behaviour of hospital employees when using the EHR system while performing their daily duties. Martin and Voynov (2014: 629) indicated that the Kotter Change Management model serves as a foundation for understanding complex settings. The Inkosi Albert Luthuli Central Hospital is one of the biggest and most complex hospitals in KZN, with different segments and health professionals working directly or indirectly for the hospital, and therefore top management, doctors, nurses and administrators working directly or indirectly with the EHR system (Antwi & Kale 2014: 2).
7 Methodology
The study focused on Inkosi Albert Luthuli Central Hospital's management of change in the implementation of an EHR system. Bryman (2012: 67) stated that the word 'case' is often associated with an intensive analysis of location, community or organisation; in this study, the hospital is the area of attention. The study thus used a case study design, as it comprised a detailed analysis of a single case (Bryman 2012). The case study is concerned with change management techniques in the execution of an EHR system in the Inkosi Albert Luthuli Central Hospital. Luthuli (2017) carried out a case study examining medical records at Ngwelezane public hospital (also in KZN) in order to provide an in-depth understanding of aspects that prompted changes and developments in the organisation. Similarly, Marutha (2011) focused on electronic records management systems in the Limpopo Province using a case study design to gain an in-depth understanding of the public health sector perspective on the application of ICT in the province. This study utilised a quantitative approach to assess the effect of change management in the implementation and use of an EHR system in the Inkosi Albert Luthuli Central Hospital.
For the data collection, the study used questionnaires to measure behavioural patterns of users of the system; interviews and direct observation were used to validate and support information collected from EHR system users. The population of the study was drawn from Inkosi Albert Luthuli Central Hospital. The total sample size was 108 participants. The study sampled three groups of hospital employees (EHR system users) with different duties. Out of forty-four departments, twenty-four were randomly selected. For the first group, two nurses and two doctors who directly rendered health services were conveniently selected in each department which resulted in a total of forty-eight nurses and, due to availability challenges, thirty-one doctors participating in the study. For the second group, hospital administrative staff were conveniently selected based on their availability. There were ten patient administrators, ten ward clerks and one records management staff member. As there were very few managers, eight were purposefully selected to form the third group. The concurrent triangulation method was used to strengthen the credibility of the study. Descriptive analysis was used for quantitative data. Data from interviews were thematically categorised and are presented in narrative form.
8 Findings and discussions
The findings of the study are presented and discussed below.
8.1 Factors facilitating the adoption of the EHR system at the hospital
The first objective of the study was to find factors facilitating the implementation of EHR systems at hospitals. When a new technological system is introduced to an organisation, there would be a motive for implementing it (Msomi 2020). The study asked the Inkosi Albert Luthuli Central Hospital management about factors that facilitated the adoption of the EHR system. One member of hospital management said that one of the motives was to address the inequalities in the public health sector that were created during the apartheid era. The rest of the respondents commonly stated that patient files were often lost or misfiled, so the EHR system ensured the privacy and security of patient information. One respondent specified that the Inkosi Albert Luthuli Central Hospital was one of the biggest referral hospitals in KZN and thus a strong support system for other hospitals inside and outside the province. The EHR system enables it to operate completely electronically in its support of other hospitals.
Other respondents indicated that, with the many challenges faced by public hospitals in the country, Inkosi Albert Luthuli Central Hospital responded to the need to improve health service delivery by implementing an EHR system. It helped by minimising patient waiting times, by consolidating patients' history for medical attention, decision or litigation purposes, and by avoiding duplication of tests and their costs. Common challenges have been identified by various authors who have studied records management in the public health sector: Katuu (2015) revealed that poor data gathering in hospitals resulted in duplication of files and failure of hospitals to track and locate original files; Luthuli (2017) found that, in Ngwelezane public hospital, their manual record management system was time consuming and resulted in long waiting times for patients to receive medical care, which negatively impacted the delivery of health services; and van der Walt and Katuu (2016) highlighted that the impact of apartheid affected the public health service delivery negatively, therefore, most challenges facing health records management originated from the past health system.
8.2 Change management in EHR system use at the hospital
The second objective focused on changes experienced by the hospital on implementation of the EHR system. The hospital management indicated that, from time-to-time, changes were made in the EHR system for improving health service delivery and due to new developments in treatments, problems encountered and system upgrades. The hospital management further indicated that, since the hospital was opened, it had moved from one system to another for various reasons. In August 2016, the hospital introduced the new system for which all employees had to undergo training to utilise efficiently. One interviewee mentioned that training was an issue when upgrading or changing the system as, at times, users resisted the change. Training people who were on duty was challenging, as the hospital needed to continue operating as usual. Boonstra, Versluis and Vos (2014: 11) emphasised that ensuring continuity of healthcare services during implementation can be challenging. One of the respondents said that:
One of the main challenges of using an EHR system in the hospital is that, at times, companies developing the system software leave the country and it becomes a problem for the hospital to manage the system [without their support] over a period of time. Therefore, that results in the hospital initiating and implementing a new system that can be easily managed locally.
The hospital management indicated that, for ICT-related matters, the hospital, together with the Department of Health in KZN, had an agreement with the IT company based on the premises of the hospital. The company covered the entire scope of the EHR system and provided most change management requirements in all projects initiated for successful project implementation and sustainability. The hospital management ensured that all changes met the requirements of the Department of Health.
8.2.1 Problems encountered in managing the EHR system change
The following were the problems encountered by the hospital in managing the change at Inkosi Albert Luthuli Central Hospital:
• Some respondents said that the interface of the system did not meet user requirements. For example, each doctor had a different way of keeping records, but the system did not always accommodate what the doctor wanted to do.
• The hospital staff emphasised that re-training whenever moving from one system to another was sometimes met with user resistance.
• They said that, when the number of patients captured and treated reached a certain number, the data storage capacity of the system became insufficient.
• From time to time, the EHR system needed to be updated to increase storage and to accommodate changes in the way new or existing patients were treated.
8.2.2 Involvement of users in discussions about the implementation of the EHR system
The Leading Change model attests that sharing a clear vision of changes and user involvement in change processes is important for every organisation going through changes (Kotter 1995). The hospital management generally agreed that there were various levels of steering committees involving various protocols, including private partners communicating directly with users, that ensured that there was a clear vision for using the EHR system. However, when other respondents were asked about how often they were involved in the implementation of the EHR system, 56.6% indicated that they were never involved. Table 1 illustrates the results.
8.2.3 Communicating EHR system changes with users
The literature indicated that frequent communication within an organisation is a vital part of managing change in health information systems, enabling each individual easily to understand the direction an organisation is moving towards (Antwi & Kale 2014). The hospital management generally said that meetings and emails were tools utilised to communicate with users about all the EHR system changes taking place. On the other hand, when users were asked about how often the hospital shared reasons for making any changes in the system, the majority indicated that the hospital never did so. As can be seen on Figure 1, this was confirmed by 45% of the respondents. An additional 23% confirmed that they sometimes received communication, 19% hardly received any information about changes, and 13% of the respondents said that they often received communication about changes in the EHR system in place.
8.2.4 Job restructuring or changes in duties due to EHR system implementation
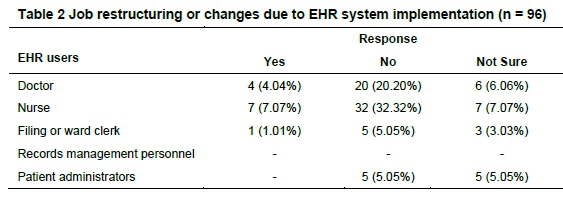
Different users were asked about changes in their job description as a result of the implementation of an EHR system. The word 'implementation' in the study covers system modification, upgrading or changing from one system to another (Msomi 2020: 132). The majority of doctors indicated no changes to their job description due to the implementation of the system; this was confirmed by twenty (20.20%) respondents, as shown in Table 2. Thirty-two (32.32%) nurses had the same response: that their tasks were not altered by using the EHR system. Half of the filing clerks (five; 5.5%) also indicated that there were no notable changes to their jobs, whereas three (3.03%) of the clerks and five (5.05%) patient administrators indicated that they were not sure. The majority of the hospital employees confirmed there were no changes in their job description as a result of the implementation of the EHR system, or of modifications or upgrades to it. However, Boonstra, Versluis and Vos (2014) attested that changes might have occurred without employees realising it. Alpay, Toussaint and Zwetsloot-Schonk (2004) confirmed that executing and sustaining EHR systems in the hospital setting necessitated staff training and development, as continuous ICT system upgrades lead to organisational shifts, changes in operational workflows and responsibilities as job descriptions evolve over time.
8.3 Monitoring and evaluating the use of the EHR system
The third objective of the study was to examine how the hospital monitored and evaluated the impact of a new EHR system. The execution of an EHR system is regarded as a process that requires a commitment to ongoing evaluation in order to have positive results (Msomi 2020). The majority of users indicated that the effectiveness of the EHR system was measured by the number of common problems reported about the system. Eighty-three (83%) of users confirmed that these reports informed their division and the IT department about any challenges faced by them when using the system. They also indicated that their performance and competency on the system was evaluated through assessment tests completed after EHR system training. They needed at least 75% to pass to be regarded as competent to use the system. If they did not pass, they repeated the training and rewrote the test.
One of the respondents from hospital management indicated that information about users was monitored to determine user training needs or the development of particular training modules based on the respective duties of the users. The quality of data captured was monitored by identifying errors and missing patient information. Verification of correct procedures being followed when recording patient information was done using data coding. Another interviewee from hospital management specified that the Admissions department was able, using the EHR system, to monitor the registration process according to the number of patients in the waiting area, those admitted, those attended to and those discharged. Another respondent from hospital management pointed out that case studies (occurrences based on system usage) and user studies in the form of a survey, where questionnaires were distributed to users (based on the EHR system use), were used to measure and monitor staff productivity and system relevance to health services delivered by Inkosi Albert Luthuli Central Hospital. The hospital also monitored and measured the effectiveness of the EHR system through statistical data generated from the above-mentioned areas and perceived patient waiting time as an indicator of system efficacy. Erasmus and van der Walt (2015) discovered that patient waiting time can be used as an indicator of success when evaluating the EHR system. Falchook et al. (2015) confirmed that time spent by personnel searching for patient files or patient information allowed hospitals to review and monitor the effectiveness of the system. Literature revealed that time spent finding and retrieving patient paper files resulted in long queues and increased patient waiting time (Weeks 2015). It is for these reasons that the hospital monitored and evaluated the use of the EHR system based on time as an indicator for effectiveness. Thomas (2016) attested that continuous monitoring of the EHR system allows the executors and the hospital to evaluate if any alterations to the system are needed.
8.4 Tools used by hospital leadership to reinforce change and sustain results
The fourth objective of the study determined tools used by Inkosi Albert Luthuli Central Hospital to reinforce change and sustain positive results. Good leaders acquire interpersonal skills in order to manage efficiently any organisational changes and needs (Kotter & Schlesinger 2008). The hospital management indicated they provided in-depth training for users. The training comprised basic computer training for all hospital employees prior to commencing duties. To ensure everyone in the hospital was computer literate, they further trained employees on the EHR system using modules related to their duties. The hospital management indicated that they made sure users utilised the changed or upgraded system fully too, as the old system only allowed users to refer and view records, but not to edit or add to the information. The hospital management further indicated that calls logged by users were used to analyse common problems or challenges faced when performing duties using the system, thus giving an indication of whether the vendor needed to be involved to improve the system or if the problem was with the users. The hospital management liaised with the departments involved to sustain the effectiveness of the system. They further specified that setting targets for users encouraged them to perform, which resulted in positive outcomes for patients being served promptly. The hospital management added that demonstration videos were also provided to users to refresh their knowledge of modules related to their daily tasks to assist when they encounter challenges. The hospital management also provided handbooks simplifying all steps involved in the actual workflow to support users to understand the EHR system in relation to their respective duties.
9 Recommendations
The study makes the following recommendations with regards to an effective change management approach in the implementation of EHR systems.
9.1 Involvement of users in EHR system changes or upgrades
The study revealed a communication breakdown between actual users (employees) and Inkosi Albert Luthuli Central Hospital top management in the discussion of EHR system changes. Therefore, the study recommends the following:
• The hospital must organise regular departmental presentations, allowing users to present advantages and disadvantages of utilising the EHR system in their daily tasks. In this manner, the hospital will know the benefits and challenges facing each department making use of the system.
• The EHR system users must also help the hospital management by being willing to have them more involved in the discussion of any changes or system upgrades.
• The hospital should open a suggestion tool to be used by EHR system users if they want to offer ideas for improvement or changes to the system, especially relating to areas that cannot be tracked by the system.
9.2 Communicating EHR system changes with users
The study established that the majority of the users hardly received reasons for changes made to the system when they occurred. The following is, therefore, recommended:
• The hospital must always make it a priority that users understand reasons for change and what value these changes will add to their daily tasks, prior to changes being implemented.
• The hospital must develop a constant communication plan to support fully the change process, especially communicating reasons for change with staff representatives from all levels of involvement in planning and decision making.
9.3 Implementation of change management at Inkosi Albert Luthuli Central Hospital
The study revealed that the IT company covered the entire scope of change management at Inkosi Albert Luthuli Central Hospital.
• Even though the IT company works hand-in-hand with the hospital in guiding changes, the hospital should be leading the change management initiatives to bridge the gap in communication between users and the IT company, as they work more closely with employees.
• The Inkosi Albert Luthuli Central Hospital should establish its own change management agents to work together with the IT company to cover the management of change in the operation of the EHR system or any IT project initiated in order to gather knowledge and develop strategies that are specific to the unique context.
9.4 Monitoring and evaluating the use of the EHR system
The study revealed that there was no formal directive or standard from the Department of Health guiding the monitoring and evaluation of the EHR system in the hospital.
• The Department of Health, working together with the hospital, should develop its own change management framework for the implementation of EHR systems that will include a formal monitoring and evaluation process in the hospital.
• The hospital must do regular evaluations of the use of the EHR system for each department to understand broader concerns from the user's perspective.
10 Conclusion
This paper presents empirical results about change management in the implementation of an EHR system at Inkosi Albert Luthuli Central Hospital. The aim was to assess management of change in the implementation of an EHR system in the hospital. It emphasises importance of the change management process in EHR system operation and its progress in the hospital. It posits that a change management strategy in EHR system execution is necessary for positive outcomes for users of the system. The evidence shows that choosing a change management approach that is not customised to the specific context of the EHR system implementation could hinder the progress of operating to the exceptional benefit of the hospital as system upgrades and advancement conspire to improve the system for its users. The study recommends that the hospital develop its own change management framework in the implementation of an EHR system that will include formal monitoring and evaluation of the process in the hospital. The Department of Health should establish an external monitoring and evaluation committee focusing on the implementation of EHR systems, consisting of peer reviewers from different branches so that those who are knowledgeable about information systems can evaluate the process used by vendors in preparing the hospital for any forthcoming technology implementation.
References
Alpay, L., Toussaint, P. and Zwetsloot-Schonk, B. 2004. Supporting healthcare communication enabled by Information and Communication Technology: can HCI and related cognitive aspects help? Proceedings of the Conference on Dutch Directions in HCI. 10 June 2004. Amsterdam: Association for Computing Machinery. DOI:10.1145/1005220.1005236. [ Links ]
Antwi, M. and Kale, M. 2014. Change management in healthcare: literature review. Kingston, Ontario: The Monieson Centre for Business Research in Healthcare, Queen's University.
Boonstra, A., Versluis, A. and Vos, J.F. 2014. Implementing electronic health records in hospitals: a systematic literature review. BMC Health Services Research, 14: 370. DOI:10.1186/1472-6963-14-370. [ Links ]
Bryman, A. 2012. Social Research Methods. 4th ed. New York: Oxford University Press. [ Links ]
Department of Health. 2012. e-Health strategy South Africa 2012-2017. [Online] https://health-e.org.za/wp-content/uploads/2014/08/South-Africa-eHealth-Strategy-2012-2017.pdf (15 March 2018).
Erasmus, L.E. and Van der Walt, T. 2015. Electronic medical records system user acceptance. Proceedings of the IAMOT Conference 2015. 8-11 June 2015. Cape Town: IAMOT. 1390-1407. [Online] http://researchspace.csir.co.za/dspace/handle/10204/8866 (01 April 2018). [ Links ]
Falchook, A.D., Tracton, G., Stravers, L., Fleming, M., Reeve, B.B., Basch, E.M. and Chera, B.S. 2015. Use of mobile device technology to collect patient-reported symptoms during radiotherapy for head and neck cancer: A prospective feasibility study. Journal of Critical Oncology, 22(13) suppl. [Online] https://ascopubs.org/doi/abs/10.1200/jco.2015.33.15_suppl.9599 (30 March 2019). [ Links ]
Hayes, J. 2014. The Theory and Practice of Change Management. 4th ed. Houndmills, Basingstoke, Hampshire: Palgrave Macmillan. [ Links ]
Health-e News. 2014. Report: eHealth Strategy South Africa 2012-2017. [Online] https://health-e.org.za/2014/09/11/report-ehealth-strategy-south-africa-2012/ (30 March 2019).
Hoffman, S. and Podgurski, A. 2008. Finding a cure: the case for regulation and oversight of electronic health record systems. Harvard Journal of Law and Technology, 22(1): 103-166. [Online] [ Links ]
https://heinonline.org/HOL/Page7collection=journals&handle=hein.journals/hjlt22&id=106&men_tab=srchresults (30 March 2019).
Katurura, M. C. and Cilliers, L. 2018. Electronic health record system in the public health care sector of South Africa: a systematic literature review. African Journal of Primary Health Care and Family Medicine, 10(1): 1-8. DOI:10.4102/phcfm.v10i1.1746. [ Links ]
Katuu, S.A. 2015. Managing records in South African public health care institutions: a critical analysis. PhD thesis. University of South Africa. [ Links ]
Kotter, J.P. 1995. Leading change: why transformation efforts fail. Harvard Business Review, May-June 1995. [Online] https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2.
Kotter, J.P. and Schlesinger, L.A. 2008. Choosing strategies for change. Harvard Business Review, July-August 2008. [Online] https://hbr.org/2008/07/choosing-strategies-for-change.
Luthuli, L.P. 2017. Medical records management practices in public and private hospitals in Umhlathuze area, South Africa. Master's dissertation. University of Zululand. [ Links ]
Martin, W. and Voynov, S. 2014. Electronic health records and change management. International Journal of Computer and Information Technology, 3(3): 626-630. [ Links ]
Marutha, N.S. 2011. Records management in support of service delivery in the public health sector of the Limpopo Province in South Africa. Pretoria: University of South Africa. [ Links ]
Marutha, N.S. 2016. A framework to embed medical records management into the healthcare service delivery in Limpopo Province of South Africa. Pretoria: University of South Africa. [ Links ]
Marutha, N.S. and Ngoepe, M. 2018. Medical records management framework to support public healthcare services in Limpopo province of South Africa. Records Management Journal, 28(2): 187-203. DOI:10.1108/RMJ-10-2017-0030. [ Links ]
Marutha, N.S. and Ngulube, P. 2012. Electronic records management in the public health sector of the Limpopo province in South Africa. Journal of the South African Society of Archivists, 45: 39-67. [Online] https://www.ajol.info/index.php/jsasa/article/view/85723 (28 March 2019). [ Links ]
Marutha, N. S. and Ngulube, P. 2018. Enterprise content management system implementation readiness to improve medical records management in Limpopo Province, South Africa. Library Philosophy and Practice (e-journal), 1769. [Online] https://digitalcommons.unl.edu/libphilprac/1769/. [ Links ]
MEDITECH. 2018. MEDITECH expands solutions in the KwaZulu-Natal Province of South Africa. [Online] https://ehr.meditech.com/news/meditech-expands-solutions-in-the-kwazulu-natal-province-of-south-africa-0 (20 March 2019).
Msomi, M. 2020. Change management in the implementation of electronic health records systems in public and private hospitals in the eThekwini area, South Africa. Masters thesis. University of Zululand. [ Links ]
National Archives of Australia. 2011. Implementing an EDRMS - key considerations. [Online] https://www.naa.gov.au/sites/default/files/2019-09/IM-Standard-Implementing%20an%20EDRMS%20key%20considerations-V1.0%202011.pdf (04 April 2019).
National Health Act, Act 61 of 2003. 2003 [Online] https://www.gov.za/documents/national-health-act (18 March 2019).
Nguyen, T. H. 2009. Information technology adoption in SMEs: an integrated framework. International Journal of Entrepreneurial Behavior & Research, 15(2): 162-186. [ Links ]
O'Mahony, D. 2009. Implementing an electronic medical record system in a rural general practice. South African Family Practice, 51(2): 1-2. [Online] https://journals.co.za/content/mp_safp/51/2/EJC80346 (13 April 2019). [ Links ]
Saldana, J. and Omasta, M. 2017. Qualitative research: analyzing life. Los Angeles: Sage Publications. [ Links ]
Schutzbank, A. and Fernandopulle, R. 2014. Doubling down: lessons learned from building a new electronic health record as part of primary care practice redesign. Healthcare 2(1): 14-18. DOI:10.1016/j.hjdsi.2013.12.007. [ Links ]
Shonhe L. 2017. Change management practices in the implementation of records management programs: a case study of Tlokweng Land Board. Master's thesis. Gaborone: University of Botswana. [ Links ]
Thomas, S. 2016. An analysis of the adoption of electronic health records in primary healthcare. MBA report. Gordon Institution of Business Science, University of Pretoria.
Van der Walt, T. and Katuu, S. 2016. Assessing the legislative and regulatory framework supporting the management of records in South Africa's public health sector. South African Journal of Information Management, 18(1): 1-7. [ Links ]
Weeks, R.V., 2012. Healthcare services management: a systems perspective. Journal of Contemporary Management, 9(1): 382-401. [ Links ]
Weeks, R.V. 2013. Electronic health records: managing the transformation from a paper-based to an electronic system. Journal of Contemporary Management, 10(1): 135-155. [ Links ]
Weeks, R.V. 2015. Managing the services encounter: the moment of truth. Journal of Contemporary Management, 12(1): 360-378. [ Links ]
Received: 17 September 2020
Accepted: 15 July 2021














