Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Communication Disorders
versión On-line ISSN 2225-4765
versión impresa ISSN 0379-8046
S. Afr. J. Commun. Disord. vol.69 no.2 Johannesburg 2022
http://dx.doi.org/10.4102/sajcd.v69i2.899
ORIGINAL RESEARCH
Cochleovestibular findings linked to COVID-19: A scoping review for clinical care planning in South Africa
Katijah Khoza-Shangase
Department of Audiology, Faculty of Humanities, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: On 30 January 2020, the World Health Organization (WHO) officially declared an outbreak of the coronavirus disease 2019 (COVID-19) to be a global health emergency. Research has focused on the impact and response to life-threatening symptoms of COVID-19 across the lifespan; however, there is a need to investigate the effects of COVID-19 on the cochleovestibular system, as viral infections are known to impact this system. This is particularly important for contexts where resources are limited and prioritisation of resources requires strong risk versus benefit evaluations
OBJECTIVE: Therefore, the purpose of this scoping review was to investigate published evidence on the impact of COVID-19 on the cochleovestibular system across the lifespan in order to allow for strategic clinical care planning in South Africa, where capacity versus demand challenges exist
METHODS: Electronic bibliographic databases such as CINAHL, EBSCOHost, MEDLINE, ProQuest, PubMed, Scopus and ScienceDirect were searched for peer-reviewed publications between January 2020 and January 2022. These had to be published in English and related to the impact of COVID-19 on the cochleovestibular system, where the question was: 'what evidence has been published on the impact of COVID-19 on the cochleovestibular system?' Review selection and characterisation was performed by the researcher with an independent review by a colleague using pretested forms
RESULTS: Of a total of 24 studies that met the inclusion criteria, the current scoping review revealed limited conclusive published evidence linking COVID-19 to permanent hearing function symptoms. Current evidence supports the possibility of COVID-19, similar to other viral infections in adults, impacting the cochleovestibular system and causing tinnitus, vertigo and sudden sensorineural hearing loss (SSNHL), with the symptoms being generally temporary and resolving either partially or completely following therapy with steroids, with very inconclusive findings in the paediatric population
CONCLUSION: These findings raise global implications for properly designed studies, which include longitudinal follow-up of cases across the lifespan, examining this link with some focus on establishing the pathophysiologic mechanisms at play as well. In the meanwhile, current findings raise the value of polymerase chain reaction (PCR) testing for all patients presenting with unexplained cochleovestibular symptoms during the pandemic, as these may be the only presenting symptoms indicating COVID-19, thus requiring careful treatment and management
Keywords: audiology; cochleovestibular; clinical; COVID-19; hearing loss; planning; South Africa; steroids; tinnitus; vertigo.
Introduction
Since the advent of coronavirus disease 2019 (COVID-19), which was first reported in Wuhan, China, the World Health Organization (WHO) officially declared this novel coronavirus outbreak an international global public health emergency on 30 January 2020 and finally a pandemic on 11 March 2020 (WHO, 2020a, 2020b). As of 21 June 2022, the total global number of confirmed cases has escalated to 540 million with over 6.32 million deaths, with South Africa registering a cumulative total of 3.99 million cases and 102 000 total official deaths (WHO, 2022). These numbers were regardless of all the global efforts to contain the virus (Hui et al., 2020; WHO, 2022). Thus, prevention and control of the COVID-19 infection, including during research, as well as provision of clinical care and training, is a key strategy to save lives and livelihoods, while safeguarding the safety of healthcare professionals and patients (Beach et al., 2020; Khoza-Shangase, Moroe, & Neille, 2021; Wieten, Burgart & Cho, 2020; WHO, 2022).
During the current COVID-19 pandemic, the wearing of face coverings globally is one of the key prevention strategies recommended and in some countries mandated. Community-wide face covering wearing, particularly in public areas, as is the requirement in South Africa (Balkaran & Lukman, 2021), is aimed at decreasing possible symptomatic or pre-symptomatic transmission of COVID-19 to others, along with adhering to physical distancing and handwashing or sanitising (Ten Hulzen & Fabry, 2020). Logically, wearing of face coverings impacts aspects of communication such as visual cues (lip reading, facial expressions) during communication - particularly for those who rely on this compensatory strategy because of a hearing impairment (Chodosh, Weinstein, & Blustein 2020; Homans & Vroegop, 2021; Kataoka, Maeda, Sugaya, Omichi, & Kariya, 2021; Maru, Stancel-Lewis, Easton, & Leverton, 2021).
Evidence suggests that universal wearing of face coverings and adherence to physical distancing during COVID-19 has a serious negative impact on communication for the hearing impaired (Naylor, Burke, & Holman, 2020; Saunders, Jackson, & Visram, 2021; Ten Hulzen & Fabry, 2020). Goldin, Weinstein and Shiman (2020) found that masks lead to an attenuation of the speaker's voice in the 2000 Hz - 7000 Hz frequency range because of a low-pass filter effect. Furthermore, a reduction in sound intensity of 3 dB to 4 dB for medical mask to approximately 12 dB for the N95 mask (respirator or FFP) was found. This, coupled with physical distancing, exacerbates the deleterious impact of COVID-19 on communication, particularly for the hearing impaired (Ten Hulzen & Fabry, 2020). If COVID-19 directly impacts hearing function, a real hearing impairment may be overlooked by the patient and their family if these documented effects of mask wearing and physical distancing are taken into consideration.
In a recent online survey within the United Kingdom, where the goal was to explore experiences of interactions where face masks were worn and how these masks affected communication, Saunders et al. (2021, p. 495) found that face masks had a negative impact on 'hearing, understanding, engagement and feelings of connection with the speaker' with this impact being more pronounced in hearing-impaired individuals. Similar findings were reported by Naylor et al. (2020). Researchers such as Gallus et al. (2021) and Almufarrij and Munro (2021) reported on dizziness, rotatory vertigo, dynamic imbalance and static imbalance that is transitory in nature, without any solid evidence of clinically significant permanent vestibular damage post COVID-19 infection. This evidence has important implications for early identification of real cochleovestibular symptoms that might be linked to COVID-19 so that they are not lost in these 'perceived' temporary subjective impacts, hence the importance of careful documentation of the possible impact of COVID-19 on the cochleovestibular system. Vestibular symptoms may be more obvious and easier to identify and report, particularly in the absence of accompanying major COVID-19 symptoms, but hearing symptoms might remain hidden.
Viral infections such as cytomegalovirus, measles, herpes simplex virus, HIV, rubella and others have been associated with hearing loss (Assuiti et al., 2013; Caroça et al., 2017; Cohen, Durstenfeld, & Roehm, 2014; Dunmade, Segun-Busari, Olajide, & Ologe, 2007; Goderis et al., 2014; Khoza-Shangase, 2010; Khoza-Shangase & Anastasiou, 2020). Cohen et al. (2014) reported that viral infections impact cochleovestibular function by either directly causing damage to inner ear structures, such as the inner hair cells and the organ of Corti, or by stimulating an inflammatory response on the auditory system. It is thus not surprising to anticipate that COVID-19, as a viral infection, might also impact hearing and balance function, although cochleovestibular symptoms have not been reported as part of the core symptoms of the disease. Mustafa (2020) argued that COVID-19, as a new pandemic that is viral in nature, requires scrutiny insofar as its possible impact on the audiological system.
The commonly documented clinical features of COVID-19 include dry cough, sore throat, headache, fever, fatigue, loss of taste, loss of sense of smell and shortness of breath (Alimohamadi, Sepandi, Taghdir, & Hosamirudsari, 2020; Lai, Shih, Ko, Tang, & Hsueh, 2020; Tian et al., 2020). There is, however, a growing and solidifying body of evidence reporting on cochleovestibular signs and symptoms, such as sudden sensorineural hearing loss (SSNHL), tinnitus and vertigo in adults with COVID-19, and refer findings on hearing screening in neonates whose mothers were COVID-19 infected (Fancello et al., 2021; Jacob, Flannery, & Mostert, 2020; Karimi-Galougahi, Naeini, Raad, Mikaniki, & Ghorbani, 2020; Koumpa, Forde, & Manjaly, 2020; Parrino et al., 2022). Jacob et al. (2020) reported on the novel ear, nose and throat triad of hearing loss, anosmia and ageusia, which brings a closer relationship of the commonly reported symptoms of COVID-19 and hearing loss to the fore. Munro, Uus, Almufarrij, Chaudhuri and Yioe (2020) maintained that more than 1 in 10 adults with COVID-19 complain about changes in their hearing status when interviewed 2 months post hospital discharge. This is while Parrino et al. (2022) reported on overall significantly higher incidence of SSNHL and combined acute cochleovestibular involvement during the pandemic than before.
If COVID-19 impacts cochleovestibular function in a similar manner to other viruses such as HIV, that is, either directly (virus itself) or indirectly (iatrogenic causes because of the medications prescribed to treat it) (Khoza-Shangase, 2020), implications for ear and hearing care in low- and middle-income countries (LMICs) such as South Africa are significant. This concern is driven by the numbers of infections that have and continue to be high in the African context - with minimal success from vaccination drives because of vaccine hesitancy (Cooper, Van Rooyen, & Wiysonge, 2021; Hughes, Mbamalu, Okonji, & Puoane, 2021). With the numbers of infection and the documented capacity versus demand challenges insofar as provision of ear and hearing care services is concerned in South Africa (Pillay, Tiwari, Kathard, & Chikte, 2020), it becomes crucial that clear definition of morbidity, including cochleovestibular symptoms, in order to facilitate proper planning at all levels of preventive audiology from primordial to tertiary (Khoza-Shangase, 2022).
This clear categorisation of symptomatology is important because of numerous reasons that are risk factors for cochleovestibular pathology and would impact ear and hearing care in the South African context, including (1) the unique circumstances presenting in South Africa when compared with China or various other regions such as North America and Europe in terms of quadruple burden of disease (Khoza-Shangase, 2021; Mukandavire et al., 2020; Pillay-van Wyk et al., 2020), with most of these cases not on treatment (Hansoti et al., 2019); (2) the risk factors for COVID-19 infection and its consequent mortality, for example, comorbid conditions such as hypertension, diabetes and chronic pulmonary disease are documented to be highly prevalent in South Africa (Chutel & Dahir, 2020); and (3) vaccine access and hesitancy (Cooper et al., 2021; Pepperrell et al., 2021) and poor healthcare infrastructure (Mezue et al., 2020; Ogbolosingha & Singh, 2020), as well as the prevailing poor social determinants of health (Ataguba & Ataguba, 2020; Khoza-Shangase & Mophosho, 2021). These factors highlight the need for extending the COVID-19 discussions from mortality-focused deliberations only to acute and long-term effects of COVID-19 as part of both prevention of the disease and efficient management of those infected (Kilic et al., 2020).
At the initial stages of the COVID-19 pandemic, understandably, significant focus was placed on life-threatening symptoms of the disease; however, with increasing numbers of infections and more evidence becoming available, new symptoms are being reported and scrutinised as the virus presents deleterious effects on particular organs and structures of the body. These innumerable other symptoms that are constantly documented indicate involvement of multiple systems by COVID-19 (Eravci et al., 2020; Savtale, Hippargekar, Bhise, & Kothule, 2021). With COVID-19 being a viral infection with direct cytopathic effects (Eravci et al., 2020; Kaur, Bherwani, Gulia, Vijay, & Kumar, 2020), which Munro et al. (2020) argued may contribute to hearing or balance disorders, the importance of this study is highlighted. Furthermore, as COVID-19 is a viral infection, prompt diagnosis of hearing impairment is critical because prompt treatment of viral-induced hearing loss has been proven to yield positive outcomes, while unidentified or late-identified permanent hearing impairment has well-documented negative impacts on the quality of life of the individuals affected (Saniasiaya, 2021). Interestingly, Jin et al. (2021) also reported that quality of life has been impacted by COVID-19 by raising mental-related disease patients of the otolaryngology department (e.g. panic, anxiety, depression and sleep disorders).
While other rapid and systematic reviews have been conducted on this topic (Almufarrij & Munro, 2021; Jafari, Kolb, & Mohajerani, 2021; Saniasiaya, 2021), albeit with different questions being explored, the nature of the pandemic, confirmatory studies such as this study are justified by COVID-19's presentation and its management, as illustrated by (1) the rapid evolution of the virus along with new variants and subvariants; (2) the impact of individual and heard immunity developments; (3) the available COVID-19 treatments, including the different vaccines available to prevent it; and (4) the evolving nature of the clinical features from the initially reported to currently reported (Aleem & Slenker, 2021; Cascella, Rajnik, Aleem, Dulebohn, & Di Napoli, 2022; Wang et al., 2020; Zhou et al., 2020), among other things. In the context of a pandemic where the urgency of knowledge sharing is high, certain research and publication protocols that ensure research integrity may be relaxed (Fleming, Labriola, & Wittes, 2020; Park et al., 2021; Vindrola-Padros et al., 2020), thus replication of exploratory studies for confirmation of findings is arguably valuable, hence the importance of this study. Therefore, the purpose of this scoping review is to investigate published evidence, including case reports, on the impact of COVID-19 on the cochleovestibular system across the lifespan.
Methodology
Aim
This scoping review aimed to analyse published evidence on the impact of COVID-19 on the cochleovestibular system in line with the pandemic changes.
Review approach
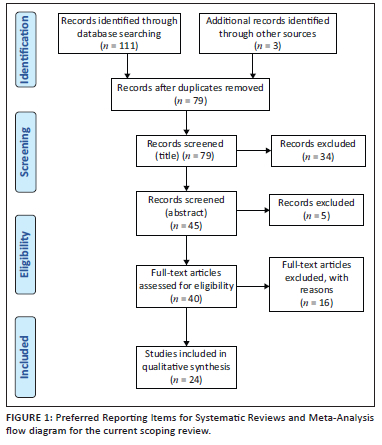
The Arksey and O'Malley's (2005) framework for performing scoping reviews was utilised, as detailed next, with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) followed during the screening process and for illustrating the process.
Stage 1: Identification of the research question
The population (COVID-19 infected and/or exposed), concept (cochleovestibular symptoms or effects) and context (globally) (PCC) framework by the Joanna Briggs Institute was used to formulate the research question. For this review, the following question was formulated, 'What evidence has been published on the impact of COVID-19 on the cochleovestibular system?'
Stage 2: Data sources and search strategy
Levac, Colquhoun and O'Brien (2010) recommended that the search strategy should follow a transparent format that can be reviewed and it should be comprehensive, without compromising feasibility. Therefore, in this review, the literature search was conducted in December 2021 on databases including CINAHL, EBSCOHost, MEDLINE, ProQuest, PubMed, Scopus and ScienceDirect. The following terms and combination of keywords were devised and used for the search based on the research question and to ensure congruency between the research question, search terms and inclusion criteria. These terms included 'COVID-19' OR 'SARS-CoV-2,' OR 'audiological effects of COVID-19' OR 'hearing loss and COVID-19' OR 'impact of COVID-19 on audiovestibular system' OR 'COVID-19 and cochleovestibular effects', 'auditory dysfunction', 'dizziness', 'hearing loss', 'vertigo', 'vestibular dysfunction' and 'otologic symptoms'. Ghalibaf et al. (2017) advised that utilising a combination of keywords enhances the search strategy to lead to an increased likelihood of finding more relevant articles while eliminates eliminating irrelevant articles.
Inclusion criteria
To yield contemporary evidence, the search was restricted to peer-reviewed studies published in English during the COVID-19 era (between January 2020 and January 2022). To be part of the scoping review, the studies had to report on cochleovestibular symptoms or effects of COVID-19.
Exclusion criteria
Review studies and studies not published in English were not eligible for inclusion. Studies were excluded if they did not address the research question, and if they did not include the combination of the search keywords. Studies that spoke about tinnitus on its own were excluded because of the limited objective evaluation of tinnitus in such studies and the multiple possible causal factors in the absence of hearing loss. Studies across the lifespan were included to ensure that findings assist with clinical planning across the lifespan, although it was obvious that identification of vestibular symptoms in the paediatric population would be challenging; however, hearing function findings would be valuable.
Stage 3: Study selection
All in all, the database search from all databases identified 114 articles. All identified database citations were exported to a web-based bibliography manager, Endnote. Through this bibliography manager, duplicate studies were identified and removed. Following removal of duplicate studies, 79 studies remained, and these were brought down to 45 after title screening, where 34 articles were eliminated. The 45 abstracts were consequently screened, guided by the search question, and 5 studies were excluded because they did not report on cochleovestibular effects of COVID-19. A total of 40 studies were then assessed for eligibility, and of these, 15 were excluded because they did not meet the inclusion criteria. Ultimately, a full-text screening resulted in 24 studies meeting the inclusion criteria and being included in this scoping review. Figure 1 shows a PRISMA flowchart for the literature search, retrieval and inclusion process of this scoping review.
Stage 4: Data extraction and charting
Following Peters et al.'s (2015) recommendation that the data must be charted in line with the objectives of the review, the charting was conducted. After the reference search, a total of 24 studies formed part of this review, and these are tabulated in Table 1. The table reflects the following data that were extracted from the included articles, with detailed analysis and discussion of the contents of the table presented next:
-
researcher(s) and the year of publication
-
title of the study
-
country of publication
-
aim of the article
-
signs and symptoms reported
-
conclusions
-
recommendations.
Data analysis was carried out through descriptive analysis, as the last step set out by Arksey and O'Malley (2005), with implications of the findings focusing on three broad categories: implications for teaching, research and practice - highlighting planning needs (Peters et al., 2015).
Ethical considerations
This scoping review followed all ethical standards for a study that does not involve direct contact with human or animal participants, including reflexivity and informed subjectivity, audience-appropriate transparency and purposefully informed selective inclusivity (Suri, 2020).
Results and discussion
The characteristics and main cochleovestibular findings documented in the 24 studies that met the eligibility criteria are depicted in Table 1. These articles varied in terms of type of study, including case reports, single group prospective, case-control prospective, retrospective or cross-sectional studies on the cochleovestibular impact of COVID-19. The articles are from both LMICs and high-income countries (HICs), with no evidence from Africa as a continent, except for some from transcontinental Egypt (Mustafa, 2020; Rhman & Wahid, 2020). The majority of the evidence was on adults, with minimal but emerging evidence from the paediatric population (Alan & Alan, 2021; Oskovi-Kaplan et al., 2022; Yıldız et al., 2021). The current findings are valuable for the South African context as they seem to flag a need for preventive ear and hearing measures planning, because they indicate the possibility of cochleovestibular presentation in COVID-19. Furthermore, current findings bring forward significant implications not only for therapeutic interventions insofar as prompt otorhinolaryngological management is concerned but they also highlight such implications for patient isolation should cochleovestibular symptoms be the first and only symptom, as well as for audiological service provision and human resource planning within this resource-constrained context.
As far as the cochleovestibular symptoms are concerned, there is no conclusive published evidence of cochlear or vestibular damage that is persistent and clinically relevant following COVID-19 recovery (Gallus et al., 2021). However, the current review appears to indicate a strong possibility of COVID-19 impacting cochleovestibular function in various ways across the lifespan (Alan & Alan, 2021; Gallus et al., 2021; Korkmaz et al., 2021); however, this evidence is not strong, and it remains difficult to confirm because of two key factors: (1) poor quality of studies and evidence that is based mainly on case studies (Almufarrij, Uus, & Munro, 2020; Munro et al., 2020), and (2) occurrence of other possible causes of cochleovestibular symptoms in these patients (Munro et al., 2020). Although in the current scoping review, the quality of the studies was not formally assessed, a scoping overview indicates the following features of the studies: (1) mostly case reports where other possible causes are a possibility; (2) limited use of objective audiological measures, but rather reports and complaints by patients were used; (3) where control groups are included, there is limited clarity provided on inclusion criteria for the control group participants, and so on. These limitations are, however, arguably expected during a new public health emergency where everything is new and novel and exploratory research is what is feasible.
Nonetheless, notwithstanding this research quality challenge, the limited evidence that exists seems to warrant the need for careful audiological assessment and monitoring and polymerase chain reaction (PCR) testing for COVID-19 diagnosis in patients with sudden unexplained cochleovestibular features during COVID-19 (Beckers et al., 2021; Jafari et al., 2021; Koparal & Yılmazer, 2021) and children born to mothers who were COVID-19 positive during pregnancy (Alan & Alan, 2021; Oskovi-Kaplan et al., 2022; Yıldız et al., 2021). This is particularly important as definitive evidence is required to ensure that appropriate treatment is provided that takes into cognisance the therapeutic dilemmas surrounding the use of steroids in this population, as raised by Karimi-Galougahi et al. (2020), the need for patient isolation and the possibilities of monitoring for late onset hearing loss in children born to mothers who were COVID-19 positive during pregnancy. The South African healthcare system and the audiology community would need to carefully plan around how to effectively manage these cases within the already resource-constrained context (Pillay et al., 2020), possibly within already existing programmes, adopting a programmatic approach to care (Khoza-Shangase, 2022).
Analysis in this review leads the current author to conclude that generally, cochleovestibular symptoms that have been reported in adults include sudden onset sensorineural hearing loss with varying severity levels, which can be unilateral or bilateral, mostly high-frequency configuration, with or without tinnitus and vertigo, with the presentation in the paediatric population remaining relatively obscure. The occurrence of cochleovestibular symptoms is reported to vary, with some patients presenting with SSNHL as a leading symptom of COVID-19, while in others the symptoms occur greater than 6 days after the COVID-19 diagnosis or long after recovery from the infection (Kilic et al., 2020; Munro et al., 2020; Pokharel et al., 2021; Ricciardiello et al., 2021). Even if some patients present with cochleovestibular symptoms, some evidence seems to indicate that these are mainly temporary in nature (Gallus et al., 2021; Munro et al., 2020). In paediatrics, refer findings have been documented during neonatal or newborn hearing screening (NHS) in neonates whose mothers were infected with COVID-19, particularly in the second trimester. In most of the cases, the symptoms are temporary and resolve either partially or completely following treatment with steroids, thus highlighting the importance of clear categorisation and identification of these symptoms for early intervention. The possibility of late onset of hearing loss in the paediatric population has not been eliminated by current data and warrants closer monitoring of these patients, thus raising implications for longitudinal follow-up of these children for early intervention to be instituted should the need arise, within the South African context.
The type of onset of the cochleovestibular symptoms is reported to be acute (Gallus et al., 2021; Koumpa et al., 2020; Savtale et al., 2021), with most of the patients reported to have achieved partial or complete resolution of symptoms after therapy with steroids (Bhatta et al., 2021; Chern et al., 2021; Koumpa et al., 2020; Ricciardiello et al., 2021). For example, Pokharel et al. (2021) reported on significant improvement in hearing following treatment with steroids. Early detection and diagnosis of SSNHL and other less familiar symptoms in this population provides patients with the prospect to receive early intervention (Koumpa et al., 2020; Ricciardiello et al., 2021). Koumpa et al. (2020) argued that this prompt screening and diagnosis of cochleovestibular symptoms post-COVID-19 facilitates prescription of an early course of steroids, thus providing the patient with the best chance of symptom resolution. Koparal and Yılmazer (2021) stressed that in cases presenting with unexplained hearing loss or vestibular dysfunction, it is critical to prioritise PCR testing to determine the possibility of COVID-19 causing the symptoms because of two important reasons: (1) prevention of virus spread (patient isolation) and (2) offering the patient therapy for acute hearing loss with steroids while taking into cognisance the therapeutic dilemmas surrounding the use of steroids in this population (Karimi-Galougahi et al., 2020), thus affording the infected patient an opportunity to recover from the symptoms.
From their review, Almufarrij et al. (2020) concluded that significantly few cochleovestibular symptoms can be confirmed to be COVID-19 related, with most of the cases presenting with minor symptoms. Mustafa (2020), however, highlighted that the lack of significant COVID-19 symptoms does not necessarily provide assurance that cochlear function is healthy and safe. Several studies reviewed indicate the presence of SSNHL with or without tinnitus and vertigo (Beckers et al., 2021; Chern et al., 2021; Gallus et al., 2021; Jin et al., 2021; Kimura et al., 2021; Korkmaz et al., 2021; Koumpa et al., 2020; Munro et al., 2020; Ricciardiello et al., 2021) with nonspecific symptoms such as SSNHL being reported as possibly being the sole feature that could be used to identify a COVID-19 case (Kilic et al., 2020). The reported rate of otological or vestibular symptoms varied significantly. For example, Korkmaz et al. (2021) reported the rate of hearing impairment (5.1%), tinnitus (11%), dizziness (31.8%) and true vertigo (6%); Gallus et al. (2021) documented their rate at 8.3% for hearing loss, 4.2% for tinnitus and 8.3% for dizziness; Bhatta et al. (2021) reported hearing loss in 3.9%, tinnitus in 1.8%, earache in 1.8% and aural fullness in 1.4% of their patients with COVID-19; and Munro et al. (2020) reported a change in hearing and tinnitus in 13.2% of their COVID-19 diagnosed patients. Munro et al. (2020) reported that testing showed vestibular symptoms, with Beckers et al. (2021) reporting a deficit of the anterior semicircular canals and Chern et al. (2021) documenting bilateral intralabyrinthine haemorrhage.
Ricciardiello et al. (2021) reported that both ears can equally be affected, and the impairment could be unilateral or bilateral, and if bilateral, the symptoms can be symmetrical or nonsymmetrical (Karimi-Galougahi et al., 2020; Koparal & Yılmazer, 2021; Koumpa et al., 2020; Sriwijitalai & Wiwanitkit, 2020), with the severity of the hearing loss documented to range from mild loss to profound hearing loss (Beckers et al., 2021; Chern et al., 2021; Koparal & Yılmazer, 2021; Koumpa et al., 2020; Pokharel et al., 2021) and some evidence of pure-tone average being substantially worse in patients with COVID-19 when compared with healthy control groups, particularly in the high frequencies (Koparal & Yılmazer, 2021). Mustafa (2020) found that pure-tone hearing thresholds in high frequencies and amplitudes of transient evoked otoacoustic emissions (TEOAE) were significantly worse in this population, thus concluding that COVID-19 infection potentially has adverse effects on cochlear hair cell function even when infected individuals are asymptomatic for the cardinal disease symptoms. Similar findings were reported by Dharmarajan et al. (2021), while Daher et al. (2022) only found the hearing loss in the ultra-high frequencies, thus highlighting the need for inclusion of sensitive audiological measures such as ultra-high frequency audiometry and distortion product OAEs (DPOAEs).
Among the paediatric population, COVID-19 positivity in pregnancy has been associated with an increased risk of refer screening results during NHS (Alan & Alan, 2021; Oskovi-Kaplan et al., 2022; Yıldız et al., 2021). Alan and Alan (2021) reported that PCR positivity during the second trimester of pregnancy may be associated with abnormal NHS findings, although these refer findings resolve on repeat screening later and results become similar to those of the control group (Alan & Alan, 2021; Yıldız et al., 2021; Oskovi-Kaplan et al., 2022). In fact, Oskovi-Kaplan et al. (2022), based on the lack of differences they found between the study and control groups at final screening, conclude that COVID-19 infection during pregnancy does not appear to be a risk factor for hearing loss - a sentiment not shared by Alan and Alan (2021), who asserted that maternal COVID-19 infection could potentially be a risk factor for hearing impairment, albeit the effect being temporary in nature. On the other hand, Yıldız et al. (2021) suggested that for conclusive findings about hearing loss because of COVID-19 in this population, larger patient series in newborns should be evaluated and that late onset hearing loss is also a possibility in this population. Oskovi-Kaplan et al. (2022) supports this suggestion by recommending that large-scale, multicentre studies of pregnant women be conducted to support current evidence and to make a definitive judgment regarding neonatal hearing outcomes post-COVID-19-exposure and infection. This raises research and clinical follow-up implications for the South African research and audiology communities.
Findings from the review reveal uncertainty and inconsistency regarding the underlying pathophysiology of the cochleovestibular symptoms in COVID-19 positive patients, with Pokharel et al. (2021) maintaining that the absence of a clear pathophysiologic mechanism linking COVID-19 to SSNHL creates a vague association. Therefore, Koparal and Yılmazer's (2021) recommended more research to examine the impact of COVID-19 on hearing, including the underlying pathophysiology. So far, current evidence suggests that otologic features found in this population are potentially because of (1) direct viral invasion of the labyrinth or cochlear nerve and intralabyrinthine haemorrhage from COVID-19-associated coagulopathy (Chern et al., 2021); (2) an inflammatory process in the cochlea (virus-triggered, immune-mediated inflammation), as observed in MRI findings (Degen et al., 2020); (3) the possibility of COVID-19 invading the neural pathways involved in hearing and balance (Karimi-Galougahi et al., 2020); and (4) in neonates, delayed neuromaturation because of factors such as preterm birth, foetal growth restriction and perinatal mortality (Alan & Alan, 2021). On the other hand, Kimura et al. (2021) argued that differentiating symptoms in COVID-19 from those of bacterial infections is difficult, while Munro et al. (2020) highlighted that many other potential causes of hearing loss linked to critical care such as auto-immune disease, systematic or local infections, ototoxic medications and vascular disorders should also be considered.
Numerous recommendations were found in the studies reviewed regarding establishment and assessment and management of cochleovestibular symptoms in patients with COVID-19. Key to the recommendations is one by Karimi-Galougahi et al. (2020) and Parrino et al. (2022), who argue that epidemiological correlations and bio-pathological mechanisms involved in cochleovestibular presentation of COVID-19 require further investigations. Linked to this recommendation, is ensuring that studies should not be of poor quality (Almufarrij et al., 2020; Fancello et al., 2021; Munro et al., 2020), with Almufarrij et al. (2020) suggesting that future high-quality studies be conducted once the life-threatening nature of the pandemic is under control. Such high-quality studies would ensure that the distinction between premorbid and current changes in hearing, balance and tinnitus is clear and that the possibility that environmental surroundings changes associated with use of masks and hospitalisation is not what may have caused recognition of pre-existing tinnitus and hearing loss (Munro et al., 2020). Jafari et al. (2021) suggested future directions including follow-up assessments utilising reliable objective measures, as well as studies with properly constituted research designs.
Fancello et al. (2021) believed that despite the fact that the quality of the current evidence is poor, there is sufficient support for cochleovestibular disorders to be included as possible important features of COVID-19. Such heightened awareness of cochleovestibular disorders as part of the nonspecific presentation of COVID-19 is important, as it facilitates prevention of the spread of this infectious pandemic through patient isolation and provision of and early COVID-19 specific interventions (Kilic et al., 2020; Koumpa et al., 2020). Pokharel et al. (2021) recommended a comprehensive history and diagnostic assessment for past or recent COVID-19 infection in individuals with SSNHL, because SSNHL could be a sequela of COVID-19 (Ricciardiello et al., 2021), with Beckers et al. (2021) recommending inclusion of PCR testing in the diagnostic evaluation of these patients with SSNHL during COVID-19. Furthermore, Munro et al. (2020) recommended meticulous following up of COVID-19 patients for establishment of its long-term consequences on cochleovestibular function.
Conclusion
The current scoping review aimed at answering the question 'what evidence has been published on the impact of COVID-19 on the cochleovestibular system?' revealed findings that highlight a need for high-quality research in the area so that definitive answers can be provided. Current evidence suggesting the possibility of cochleovestibular impact of COVID-19 across the lifespan is not strong enough; however, it does show that tinnitus, vertigo and SSNHL of mostly high frequencies occur either singly or in combination in adults and refer findings in neonatal hearing screening, albeit temporary. These cochleovestibular symptoms occur sometimes as the only symptom of COVID-19 in the absence of the standardly reported core symptoms, and these are generally temporary and resolve either partially or completely following treatment with steroids. The pathophysiologic mechanism for the cochleovestibular symptoms in this population remains obscure. This lack of clarity and definitiveness is the same in the adult and paediatric populations, thus raising a need for caution around assessment and management of patients presenting with unexplained cochleovestibular symptoms during this pandemic and a need for possible longitudinal monitoring of children born to mothers who were COVID-19 positive during pregnancy. Recommendations for PCR testing have been made to allow for accurate and safe treatment of these patients - including isolation should PCR come back positive for COVID-19, with safety and possible value around the use of steroids for treatment of SSNHL in this population being highlighted. These findings have important implications for clinical care planning and evidence development within the South African context, as detailed in the results and discussion section of this article. Considerations around preventive approaches from primordial to tertiary prevention levels are crucial for this context, with implications for resource allocation taken careful cognisance of.
Acknowledgements
Competing interests
The author declares that she has no financial or personal relationships that may have inappropriately influenced her in writing this article.
Author's contributions
K.K.-S. declares that she is the sole author of this research article.
Funding information
The author thanks the National Institute for the Humanities and Social Sciences (NIHSS) for providing financial assistance for the publication of this manuscript.
Data availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Disclaimer
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of any affiliated agency of the author.
References
Alan, M.A., & Alan, C. (2021). Hearing screening outcomes in neonates of SARS-CoV-2 positive pregnant women. International Journal of Pediatric Otorhinolaryngology, 146, 110754. https://doi.org/10.1016/j.ijporl.2021.110754 [ Links ]
Aleem, A., Ab, A.S., & Slenker, A.K. (2021). Emerging variants of SARS-CoV-2 and novel therapeutics against coronavirus (COVID-19). Treasure Island, FL: StatPearls. [ Links ]
Alimohamadi, Y., Sepandi, M., Taghdir, M., & Hosamirudsari, H. (2020). Determine the most common clinical symptoms in COVID-19 patients: A systematic review and meta-analysis. Journal of Preventive Medicine and Hygiene, 61(3), E304. [ Links ]
Almufarrij, I., & Munro, K.J. (2021). One year on: An updated systematic review of SARS-CoV-2, COVID-19 and audio-vestibular symptoms. International Journal of Audiology, 60(12), 935-945. https://doi.org/10.1080/14992027.2021.1896793 [ Links ]
Almufarrij, I., Uus, K., & Munro, K.J. (2020). Does coronavirus affect the audio-vestibular system? A rapid systematic review. International Journal of Audiology, 59(7), 487-491. https://doi.org/10.1080/14992027.2021.1896793 [ Links ]
Arksey, H., & O'Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice, 8(1), 19-32. https://doi.org/10.1080/1364557032000119616 [ Links ]
Assuiti, L.F.C., De Melo Lanzoni, G.M., Dos Santos, F.C., Erdmann, A.L., & Meirelles, B.H.S. (2013). Hearing loss in people with HIV/AIDS and associated factors: An integrative review. Brazilian Journal of Otorhinolaryngology, 79(2), 248-255. https://doi.org/10.5935/1808-8694.20130042 [ Links ]
Ataguba, O.A., & Ataguba, J.E. (2020). Social determinants of health: The role of effective communication in the COVID-19 pandemic in developing countries. Global Health Action, 13(1), 1788263. https://doi.org/10.1080/16549716.2020.1788263 [ Links ]
Balkaran, S., & Lukman, Y. (2021). Covid-19 and the impact of public policy in compulsory mask wearing in South Africa. Journal of Public Administration, 56(3), 576-594. [ Links ]
Beach, M.C., Lederman, H.M., Singleton, M., Brower, R.G., Carrese, J., Ford, D.E., ... Zenilman, J.M. (2020). Desperate times: Protecting the public from research without consent or oversight during public health emergencies. Annals of Internal Medicine, 173(11), 926-928. https://doi.org/10.7326/M20-4631 [ Links ]
Beckers, E., Chouvel, P., Cassetto, V., & Mustin, V. (2021). Sudden sensorineural hearing loss in COVID-19: A case report and literature review. Clinical Case Reports, 9(4), 2300. https://doi.org/10.1002/ccr3.4019 [ Links ]
Bhatta, S., Sharma, S., Sharma, D., Maharjan, L., Bhattachan, S., Sah, M.K., ... Ganesuni, D. (2021). Study of hearing status in COVID-19 patients: A multicentered review. Indian Journal of Otolaryngology and Head & Neck Surgery, 1-7. https://doi.org/10.1007/s12070-021-02710-w
Caroça, C., Vicente, V., Campelo, P., Chasqueira, M., Caria, H., Silva, S., ... Paço, J. (2017). Rubella in Sub-Saharan Africa and sensorineural hearing loss: A case control study. BMC Public Health, 17(1), 1-7. https://doi.org/10.1186/s12889-017-4077-2 [ Links ]
Cascella, M., Rajnik, M., Aleem, A., Dulebohn, S.C., & Di Napoli, R. (2022). Features, evaluation, and treatment of coronavirus (COVID-19). Statpearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554776/
Chern, A., Famuyide, A.O., Moonis, G., & Lalwani, A.K. (2021). Bilateral sudden sensorineural hearing loss and intralabyrinthine hemorrhage in a patient with COVID-19. Otology & Neurotology, 42(1), e10. https://doi.org/10.1097/MAO.0000000000002860 [ Links ]
Chodosh, J., Weinstein, B.E., & Blustein, J. (2020). Face masks can be devastating for people with hearing loss. BMJ, 370, m2683. https://doi.org/10.1136/bmj.m2683 [ Links ]
Chutel, L., & Dahir, A.L. (2020). With most coronavirus cases in Africa, South Africa locks down. New York Times. Retrieved from https://www.nytimes.com/2020/03/27/world/africa/south-africa-coronavirus.html
Cohen, B.E., Durstenfeld, A., & Roehm, P.C. (2014). Viral causes of hearing loss: A review for hearing health professionals. Trends in Hearing, 18, 2331216514541361. https://doi.org/10.1177/2331216514541361 [ Links ]
Cooper, S., Van Rooyen, H., & Wiysonge, C.S. (2021). COVID-19 vaccine hesitancy in South Africa: How can we maximize uptake of COVID-19 vaccines? Expert Review of Vaccines, 20(8), 921-933. https://doi.org/10.1080/14760584.2021.1949291 [ Links ]
Daher, G.S., Nassiri, A.M., Vanichkachorn, G., Carlson, M.L., Neff, B.A., & Driscoll, C.L. (2022). New onset tinnitus in the absence of hearing changes following COVID-19 infection. American Journal of Otolaryngology, 43(1), 103208. https://doi.org/10.1016/j.amjoto.2021.103208 [ Links ]
Degen, C., Lenarz, T., & Willenborg, K. (2020). Acute Profound Sensorineural Hearing Loss After COVID-19 Pneumonia. Mayo Clinic Proceedings, 95(8), 1801-1803. https://doi.org/10.1016/j.mayocp.2020.05.034 [ Links ]
Dharmarajan, S., Bharathi, M.B., Sivapuram, K., Prakash, B.G., Madhan, S., Madhu, A., ... Ramya, S.B. (2021). Hearing loss-a camouflaged manifestation of COVID 19 infection. Indian Journal of Otolaryngology and Head & Neck Surgery, 73, 494-498. https://doi.org/10.1007/s12070-021-02581-1 [ Links ]
Dunmade, A.D., Segun-Busari, S., Olajide, T.G., & Ologe, F.E. (2007). Profound bilateral sensorineural hearing loss in Nigerian children: Any shift in etiology? Journal of Deaf Studies and Deaf Education, 12(1), 112-118. https://doi.org/10.1093/deafed/enl019 [ Links ]
Eravci, F.C., Alafifi, M., Dündar, M.A., Korkmaz, C., Demirbaş, S., Vatansev, H., ... Arbağ, H. (2021). Neurotological manifestations of patients with COVID-19. Journal of Ear Nose Throat and Head Neck Surgery, 29(3), 168-175. https://doi.org/10.24179/kbbbbc.2021-82151 [ Links ]
Fancello, V., Hatzopoulos, S., Corazzi, V., Bianchini, C., Skarżyńska, M.B., Pelucchi, S., ... Ciorba, A. (2021). SARS-CoV-2 (COVID-19) and audio-vestibular disorders. International Journal of Immunopathology and Pharmacology, 35, 20587384211027373. https://doi.org/10.1177/20587384211027373 [ Links ]
Fleming, T.R., Labriola, D., & Wittes, J. (2020). Conducting clinical research during the COVID-19 pandemic: Protecting scientific integrity. JAMA, 324(1), 33-34. https://doi.org/10.1001/jama.2020.9286 [ Links ]
Gallus, R., Melis, A., Rizzo, D., Piras, A., De Luca, L.M., Tramaloni, P., ... Bussu, F. (2021). Audiovestibular symptoms and sequelae in COVID-19 patients. Journal of Vestibular Research 31(5), 381-387. https://doi.org/10.3233/VES-201505 [ Links ]
Ghalibaf, A.N.A. (2017). Comprehensive overview of computer-based health information tailoring: A scoping review protocol. BMJ Open, 7(12), e019215. https://doi.org/10.1136/bmjopen-2017-019215 [ Links ]
Goderis, J., De Leenheer, E., Smets, K., Van Hoecke, H., Keymeulen, A., & Dhooge, I. (2014). Hearing loss and congenital CMV infection: A systematic review. Pediatrics, 134(5), 972-982. https://doi.org/10.1542/peds.2014-1173 [ Links ]
Goldin, A., Weinstein, B., & Shiman, N. (2020). Speech blocked by surgical masks becomes a more important issue in the era of COVID-19. Hearing Review, 27(5), 8-9. [ Links ]
Hansoti, B., Mwinnyaa, G., Hahn, E., Rao, A., Black, J., Chen, V., ... Quinn, T.C. (2019). Targeting the HIV epidemic in South Africa: The need for testing and linkage to care in emergency departments. EClinicalMedicine, 15, 14-22. https://doi.org/10.1016/j.eclinm.2019.08.007 [ Links ]
Homans, N.C., & Vroegop, J.L. (2021). The impact of face masks on the communication of adults with hearing loss during COVID-19 in a clinical setting. International Journal of Audiology, 61(5), 365-370. https://doi.org/10.1080/14992027.2021.1952490 [ Links ]
Hughes, G.D., Mbamalu, O.N., Okonji, C.O., & Puoane, T.R. (2021). The impact of health disparities on COVID-19 outcomes: Early findings from a high-income country and two middle-income countries. Journal of Racial and Ethnic Health Disparities, 9, 376-383. https://doi.org/10.1007/s40615-021-00999-5 [ Links ]
Hui, D.S., Azhar, E.I., Madani, T.A., Ntoumi, F., Kock, R., Dar, O., ... Zumla, A. (2020). The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - The latest 2019 novel coronavirus outbreak in Wuhan, China. International Journal of Infectious Diseases, 91, 264-266. https://doi.org/10.1016/j.ijid.2020.01.009 [ Links ]
Jacob, J., Flannery, W., & Mostert, C. (2020). Novel ENT triad of anosmia, ageusia and hearing impairment in COVID-19. Internal Medicine Journal, 50(9), 1155. https://doi.org/10.1111/imj.14880 [ Links ]
Jafari, Z., Kolb, B.E., & Mohajerani, M.H. (2021). Hearing loss, tinnitus, and dizziness in COVID-19: A systematic review and meta-analysis. Canadian Journal of Neurological Sciences, 49(2), 1-33. https://doi.org/10.1017/cjn.2021.63 [ Links ]
Jin, L., Fan, K., Tan, S., Liu, S., Wang, Y., & Yu, S. (2021). Analysis of the characteristics of outpatient and emergency diseases in the department of otolaryngology during the "COVID-19" pandemic. Science Progress, 104(3), 00368504211036319. https://doi.org/10.1177/00368504211036319 [ Links ]
Karimi-Galougahi, M., Naeini, A.S., Raad, N., Mikaniki, N., & Ghorbani, J. (2020). Vertigo and hearing loss during the COVID-19 pandemic - Is there an association? Acta Otorhinolaryngologica Italica, 40(6), 463. https://doi.org/10.14639/0392-100X-N0820 [ Links ]
Kataoka, Y., Maeda, Y., Sugaya, A., Omichi, R., & Kariya, S. (2021). Effects of protective measures against COVID-19 on auditory communication for people with hearing loss. Acta Medica Okayama, 75(4), 511-516. [ Links ]
Kaur, S., Bherwani, H., Gulia, S., Vijay, R., & Kumar, R. (2020). Understanding COVID-19 transmission, health impacts and mitigation: Timely social distancing is the key. Environment, Development and Sustainability, 23, 6681-6697. https://doi.org/10.1007/s10668-020-00884-x [ Links ]
Khoza-Shangase, K. (2010). HIV/AIDS and auditory function in adults: The need for intensified research in the developing world. African Journal of AIDS Research, 9(1), 1-9. https://doi.org/10.2989/16085906.2010.484531 [ Links ]
Khoza-Shangase, K. (2020). Pharmaco-audiology vigilance in the treatment of adult patients with HIV/AIDS: Ototoxicity monitoring protocol recommendation. Infectious Disorders-Drug Targets (Formerly Current Drug Targets-Infectious Disorders), 20(1), 33-42. https://doi.org/10.2174/1871526518666181016102102 [ Links ]
Khoza-Shangase, K. (2021). Confronting realities to early hearing detection in South Africa. In K. Khoza-Shangase & A. Kanji (eds), Early detection and intervention in audiology: An African perspective (pp. 66-68), Wits University Press, Johannesburg.
Khoza-Shangase, K. (2022). Preventive audiology: Ramping up efforts towards an ear and hearing healthy nation. In K. Khoza-Shangase (Ed.), Preventive audiology: An African perspective (pp. 1-44). AOSIS Press, Cape Town.
Khoza-Shangase, K., & Anastasiou, J. (2020). An exploration of recorded otological manifestations in South African children with HIV/AIDS: A pilot study. International Journal of Pediatric Otorhinolaryngology, 133, 109960. https://doi.org/10.1016/j.ijporl.2020.109960 [ Links ]
Khoza-Shangase, K., & Mophosho, M. (2021). Language and culture in speech-language and hearing professions in South Africa: Re-imagining practice. South African Journal of Communication Disorders, 68(1), 9. https://doi.org/10.4102/sajcd.v68i1.793 [ Links ]
Khoza-Shangase, K., Moroe, N., & Neille, J. (2021). Speech-language pathology and audiology: Clinical training and service in the era of COVID-19. International Journal of Telerehabilitation, 13(1), e6376. https://doi.org/10.5195/ijt.2021.6376 [ Links ]
Kilic, O., Kalcioglu, M.T., Cag, Y., Tuysuz, O., Pektas, E., Caskurlu, H., & Cetın, F. (2020). Could sudden sensorineural hearing loss be the sole manifestation of COVID-19? An investigation into SARS-COV-2 in the etiology of sudden sensorineural hearing loss. International Journal of Infectious Diseases, 97, 208-211. https://doi.org/10.1016/j.ijid.2020.06.023 [ Links ]
Kimura, Y., Nogami, K., Watanabe, K., Yoshimura, O., Asai, H., Fujioka, O., ... Fukuyo, K. (2021). COVID-19 findings revealed via otolaryngological examination: Findings of a Japan Otorhinolaryngologist Association questionnaire. Auris Nasus Larynx, 48(6), 1176-1180. https://doi.org/10.1016/j.anl.2021.05.010 [ Links ]
Koparal, M., & Yılmazer, C. (2021). Evaluation of postinfection hearing with audiological tests in patients with COVID-19: A case-control study. Journal of the American Academy of Audiology, 32(07), 464-468. https://doi.org/10.1055/s-0041-1730960 [ Links ]
Korkmaz, M.Ö., Eğilmez, O.K., Özçelik, M.A., & Güven, M. (2021). Otolaryngological manifestations of hospitalised patients with confirmed COVID-19 infection. European Archives of Oto-Rhino-Laryngology, 278(5), 1675-1685. https://doi.org/10.1007/s00405-020-06396-8 [ Links ]
Koumpa, F.S., Forde, C.T., & Manjaly, J.G. (2020). Sudden irreversible hearing loss post COVID-19. BMJ Case Reports CP, 13(11), e238419. https://doi.org/10.1136/bcr-2020-238419 [ Links ]
Lai, C.C., Shih, T.P., Ko, W.C., Tang, H.J., & Hsueh, P.R. (2020). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): The epidemic and the challenges. International Journal of Antimicrobial Agents, 55(3), 105924. https://doi.org/10.1016/j.ijantimicag.2020.105924 [ Links ]
Levac, D., Colquhoun, H., & O'Brien, K.K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5(1), 69. https://doi.org/10.1186/1748-5908-5-69 [ Links ]
Maru, D., Stancel-Lewis, J., Easton, G., & Leverton, W.E. (2021). Communicating with people with hearing loss: COVID-19 and beyond. BJGP Open, 5(1), BJGPO.2020.0174. https://doi.org/10.3399/BJGPO.2020.0174 [ Links ]
Mezue, K., Edwards, P., Nsofor, I., Goha, A., Anya, I., Madu, K., ... Madu, E. (2020). Sub-Saharan Africa tackles COVID-19: Challenges and opportunities. Ethnicity & Disease, 30(4), 693. https://doi.org/10.18865/ed.30.4.693 [ Links ]
Mukandavire, Z., Nyabadza, F., Malunguza, N.J., Cuadros, D.F., Shiri, T., & Musuka, G. (2020). Quantifying early COVID-19 outbreak transmission in South Africa and exploring vaccine efficacy scenarios. PLoS One, 15(7), e0236003. https://doi.org/10.1371/journal.pone.0236003 [ Links ]
Munro, K.J., Uus, K., Almufarrij, I., Chaudhuri, N., & Yioe, V. (2020). Persistent self-reported changes in hearing and tinnitus in post-hospitalisation COVID-19 cases. International Journal of Audiology, 59(2), 889-890. https://doi.org/10.1080/14992027.2020.1798519 [ Links ]
Mustafa, M.W.M. (2020). Audiological profile of asymptomatic Covid-19 PCR-positive cases. American Journal of Otolaryngology, 41(3), 102483. https://doi.org/10.1016/j.amjoto.2020.102483 [ Links ]
Naylor, G., Burke, L.A., & Holman, J.A. (2020). Covid-19 lockdown affects hearing disability and handicap in diverse ways: A rapid online survey study. Ear and Hearing, 41(6), 1442-1449. https://doi.org/10.1097/AUD.0000000000000948 [ Links ]
Ogbolosingha, A.J., & Singh, A. (2020). COVID-19 pandemic: Review of impediments to public health measures in Sub-Saharan Africa. American Journal of Preventative Medicine and Public Health, 6(3), 68-75. https://doi.org/10.5455/ajpmph.20200512020014 [ Links ]
Oskovi-Kaplan, Z.A., Ozgu-Erdinc, A.S., Buyuk, G.N., Sert-Dinc, U.Y., Ali-Algan, C., Demir, B., ... Moraloglu-Tekin, Ö. (2022). Newborn hearing screening results of infants born to mothers who had COVID-19 disease during pregnancy: A retrospective cohort study. Ear and Hearing, 43(1), 41-44. https://doi.org/10.1097/AUD.0000000000001167 [ Links ]
Park, J.J., Mogg, R., Smith, G.E., Nakimuli-Mpungu, E., Jehan, F., Rayner, C.R., ... Mills, E.J. (2021). How COVID-19 has fundamentally changed clinical research in global health. The Lancet Global Health, 9(5), e711-e720. https://doi.org/10.1016/S2214-109X(20)30542-8 [ Links ]
Parrino, D., Frosolini, A., Toninato, D., Matarazzo, A., Marioni, G., & De Filippis, C. (2022). Sudden hearing loss and vestibular disorders during and before COVID-19 pandemic: An audiology tertiary referral centre experience. American Journal of Otolaryngology, 43(1), 103241. https://doi.org/10.1016/j.amjoto.2021.103241 [ Links ]
Pepperrell, T., Rodgers, F., Tandon, P., Sarsfield, K., Pugh-Jones, M., Rashid, T., & Keestra, S. (2021). Making a COVID-19 vaccine that works for everyone: Ensuring equity and inclusivity in clinical trials. Global Health Action, 14(1), 1892309. https://doi.org/10.1080/16549716.2021.1892309 [ Links ]
Peters, M., Godfrey, C., McInerney, P., Soares, C.B., Khalil, H., & Parker, D. (Ed.). (2015). Methodology for JBI scoping reviews. In The Joanna Briggs Institute Reviewers Manual 2015 (pp. 3-24). The Joanna Briggs Institute, Adelaide.
Pillay, M., Tiwari, R., Kathard, H., & Chikte, U. (2020). Sustainable workforce: South African audiologists and speech therapists. Human Resources for Health, 18(1), 1-13. https://doi.org/10.1186/s12960-020-00488-6 [ Links ]
Pillay-Van Wyk, V., Bradshaw, D., Groenewald, P., Seocharan, I., Manda, S., Roomaney, R.A., ... Mkhize, Z.L. (2020). COVID-19 deaths in South Africa: 99 days since South Africa's first death. SAMJ: South African Medical Journal, 110(11), 1093-1099. https://doi.org/10.7196/SAMJ.2020.v110i11.15249 [ Links ]
Pokharel, S., Tamang, S., Pokharel, S., & Mahaseth, R.K. (2021). Sudden sensorineural hearing loss in a post-COVID-19 patient. Clinical Case Reports, 9(10), e04956. https://doi.org/10.1002/ccr3.4956 [ Links ]
Rhman, S.A., & Wahid, A.A. (2020). COVID-19 and sudden sensorineural hearing loss: A case report. Otolaryngology Case Reports, 16, 100198. https://doi.org/10.1016/j.xocr.2020.100198 [ Links ]
Ricciardiello, F., Pisani, D., Viola, P., Cristiano, E., Scarpa, A., Giannone, A., ... Chiarella, G. (2021). Sudden sensorineural hearing loss in mild COVID-19: Case series and analysis of the literature. Audiology Research, 11(3), 313-326. https://doi.org/10.3390/audiolres11030029 [ Links ]
Saniasiaya, J. (2021). Hearing loss in SARS-CoV-2: What do we know? Ear, Nose & Throat Journal, 100(2_suppl), 152S-154S. https://doi.org/10.1177/0145561320946902 [ Links ]
Saunders, G.H., Jackson, I.R., & Visram, A.S. (2021). Impacts of face coverings on communication: An indirect impact of COVID-19. International Journal of Audiology, 60(7), 495-506. https://doi.org/10.1080/14992027.2020.1851401 [ Links ]
Savtale, S., Hippargekar, P., Bhise, S., & Kothule, S. (2021). Prevalence of otorhinolaryngological symptoms in Covid 19 patients. Indian Journal of Otolaryngology and Head & Neck Surgery, 1-7. https://doi.org/10.1007/s12070-021-02410-5
Sriwijitalai, W., & Wiwanitkit, V. (2020). Hearing loss and COVID-19: A note. American Journal of Otolaryngology, 41(3), 102473. https://doi.org/10.1016/j.amjoto.2020.102473 [ Links ]
Ten Hulzen, R.D., & Fabry, D.A. (2020). Impact of hearing loss and universal face masking in the COVID-19 era. Mayo Clinic Proceedings, 95(10), 2069-2072. https://doi.org/10.1016/j.mayocp.2020.07.027 [ Links ]
Tian, S., Hu, N., Lou, J., Chen, K., Kang, X., Xiang, Z., ... Zhang, J. (2020). Characteristics of COVID-19 infection in Beijing. Journal of Infection, 80(4), 401-406. https://doi.org/10.1016/j.jinf.2020.02.018 [ Links ]
Vindrola-Padros, C., Chisnall, G., Cooper, S., Dowrick, A., Djellouli, N., Symmons, S.M., ... Johnson, G.A. (2020). Carrying out rapid qualitative research during a pandemic: Emerging lessons from COVID-19. Qualitative Health Research, 30(14), 2192-2204. https://doi.org/10.1177/1049732320951526 [ Links ]
Wang, D., Hu, B., Hu, C., Zhu, F., Liu, X., Zhang, J., ... Peng, Z. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA, 323(11), 1061-1069. https://doi.org/10.1001/jama.2020.1585 [ Links ]
Wieten, S., Burgart, A., & Cho, M. (2020). Resource allocation in COVID-19 research: Which trials? Which patients? The American Journal of Bioethics, 20(7), 86-88. https://doi.org/10.1080/15265161.2020.1779392 [ Links ]
World Health Organization (WHO). (2020a). High risk groups. Retrieved from https://www.who.int/westernpacific/emergencies/covid-19/information/high-risk-group
World Health Organization (WHO). (2020b). Global leaders unite to ensure everyone everywhere can access new vaccines, tests and treatments for COVID-19. Retrieved from https://www.who.int/news/item/24-04-2020-global-leaders-unite-to-ensure-everyone-everywhere-can-access-new-vaccines-tests-and-treatments-for-covid-19
World Health Organisation (WHO). (2022). Coronavirus (COVID-19) media briefings. Retrieved from https://www.bing.com/search?q=Coronavirus+(COVID-19)+%7C+WHO+%7C+Regional+Office+for+Africa&cvid=5037661c80b244b6bfda79f5e256c496&aqs=edge..69i57.397j0j4&FORM=ANAB01&PC=ASTS
Yıldız, G., Kurt, D., Mat, E., Yıldız, P., Başol, G., Gündogdu, E.C., ... Kale, A. (2021). Hearing test results of newborns born from the coronavirus disease 2019 (COVID-19) infected mothers: A tertiary center experience in Turkey. Journal of Obstetrics and Gynaecology Research, 48(1), 113-118. https://doi.org/10.1111/jog.15008 [ Links ]
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., ... Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. The Lancet, 395(10229), 1054-1062. https://doi.org/10.1016/S0140-6736(20)30566-3 [ Links ]
 Correspondence:
Correspondence:
Katijah Khoza-Shangase
katijah.khoza-shangase@wits.ac.za
Received: 26 Jan. 2022
Accepted: 30 June 2022
Published: 12 Aug. 2022














