Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Communication Disorders
On-line version ISSN 2225-4765
Print version ISSN 0379-8046
S. Afr. J. Commun. Disord. vol.69 n.2 Johannesburg 2022
http://dx.doi.org/10.4102/sajcd.v69i2.905
ORIGINAL RESEARCH
Simulations as a mode of clinical training in healthcare professions: A scoping review to guide planning in speech-language pathology and audiology during the COVID-19 pandemic and beyond
Nabeelah NagdeeI; Ben SebothomaI; Milka MadahanaII; Katijah Khoza-ShangaseI; Nomfundo MoroeI
IDepartment of Audiology, Faculty of Humanities, University of the Witwatersrand, Johannesburg, South Africa
IISchool of Engineering, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Simulation plays an important role as an alternative method for training of students, particularly in health education. As a result of coronavirus disease 2019 (COVID-19) restrictions of face-to-face interactions, traditional teaching methods have been disrupted, increasing the need for alternative methods to supplement modes of student clinical training in healthcare programmes
OBJECTIVES: The scoping review aimed to determine what has been documented about simulation as a mode of clinical training in healthcare professions (HCPs) in order to guide speech-language pathology and audiology (SLP&A) professions during the COVID-19 pandemic and beyond
METHOD: A scoping review was conducted. Electronic bibliographic databases including Science Direct, PubMed, Scopus MEDLINE, ProQuest, Google Scholar and WorldCat were searched to identify peer reviewed publications, published in English, between January 2011 and December 2021, and related to the use of simulation in HCPs clinical training programmes
RESULTS: A total of 32 articles met the inclusion criteria for this scoping review. Three themes emerged when reviewing the studies: (1) face-to-face simulations as a mode of clinical training, (2) virtual reality simulation and telesimulation as modes of clinical training and (3) simulation as a complementary mode of clinical training. Evidence suggests that whilst simulations are cost-effective, accessible and efficacious as clinical training modes, they need to be combined with other modes of training such as the traditional clinical training to yield better learning outcomes
CONCLUSIONS: Current findings highlight the role and value of simulation as a clinical training mode during COVID-19 and beyond. However, there are aspects that need to be considered to ensure that this mode of clinical training is effective, with endorsement and regulations by the SLP&A Professional Board of the Health Professions Council of South Africa (HPCSA). Simulations need to be complemented with traditional clinical training methods. In the context of SLP&A, particularly in low- and middle-income countries (LMICs), simulation can be used to better prepare students for their clinical placement where clinical training platforms are limited and where simulation combined with teletraining or telesupervision can be utilised to increase access to training
Keywords: audiology; healthcare professionals; clinical training; COVID-19; simulations; speech-language pathology.
Introduction
Simulations may be defined as scenarios that are artificially created to study or experience something that is possible in real life (Al-Elq, 2010; Datta et al., 2012). They have been used as a training strategy in high-risk professions like aviation, merchant marine, military and nuclear energy to enhance judgement and problem-solving skills, which lead to improved safety outcomes (Pham, 2019). Additionally, simulation has been found to be a cost-effective and less labour-intensive training method in these professions (Allerton, 2010).
To meet the growing demand for speech-language pathologists and audiologists, international and national universities that offer speech-language pathology and audiology (SLP&A) programmes were obliged to increase the intake of students into these programmes. However, this increased intake of students may have resulted in overburdening training platforms and university staff members who accommodate and facilitate SLP&A programmes (McAllister & Lincoln, 2004; O'Beirne, Kelly-Campbell, & Welch, 2020). This increase in student numbers may result in increased expenses to run SLP&A programmes as compared to non-clinical programmes, as a result of the demands of clinical training over and above the academic programme. Studies that have explored the effects of an increase in nursing student numbers on clinical placements have found that high student numbers place significant pressure on healthcare professional (HCP) clinical educators to teach, supervise and nurture the students towards clinical competency (Richardson & Claman, 2014; Roberts, Kaak, & Rolley, 2019). The same can be argued for the SLP&A programmes.
In addition to the high student-to-staff ratio, there is a clinical training platform challenge where there is a shortage of clinical placement sites, which may result in fewer learning opportunities and an increase in number of HCP students competing for supervision and access to the same patients (Feingold, Calaluce, & Kallen, 2004; Lambton, 2008). Because placing HCP students at appropriate clinical placements that support their learning is challenging, it may result in them feeling overwhelmed, less competent and demotivated to integrate and be involved in their clinical placements. This limitation in their training may hamper them from achieving the necessary core clinical competencies - knowledge, skills and attitudes - that are the intended learning outcomes at these placements (Griffin, McLeod, Francis, & Brown, 2016). These challenges and their effects may be exacerbated in HCP students' clinical training programmes in low- and middle-income countries (LMICs) such as South Africa, because of the documented resource constraints (Akhlaq, McKinstry, Muhammad, & Sheikh, 2016; Khoza-Shangase & Mophosho, 2021; Pillay, Tiwari, Kathard, & Chikte, 2020).
Furthermore, the American Speech-Language-Hearing Association (ASHA n.d.) has formulated guidelines pertaining to the use of simulations in clinical practical courses accredited by the Council for Academic Accreditation in Audiology and Speech-Language Pathology (CFCC) (2016). Simulations, in the context of clinical practicals, are viewed as an alternative means of clinical training whereby students are able to develop their clinical knowledge and skills (ASHA n.d.). Furthermore, because of resource constraints that negatively affect clinical training of SLP&A students, the Council for Clinical Certification (2016) in the United States of America has allowed SLP&A students to obtain 75 hours of direct clinical contact hours when they engage in simulations.
The coronavirus disease 2019 (COVID-19) pandemic has additionally undoubtedly added to the aforementioned challenges by disrupting the clinical training in HCPs, where clinical training activities had to either be cancelled, paused or postponed (Haridy, Abdalla, Kaisarly, & Gezawi, 2021), globally. Furthermore, because of the social distancing regulations, clinical environments such as hospitals, which are traditional clinical training sites, needed to make adjustments, including limiting the presence of hospital staff and students and cancelling services considered to be non-essential to reduce patient numbers - in order to adhere to the regulations (Giordano, Cipollaro, Migliorini, & Maffulli, 2021). In South Africa, speech-language pathology outpatient services were suspended, and speech-language therapists took on additional roles such as conducting COVID-19 screenings which were part of the public health emergency priority for the National Department of Health (Adams, Seedat, Coutts, & Kater, 2020). These changes in functioning and emergency extensions to the scopes of practice may have resulted in HCP students not receiving sufficient clinical practical experiences to develop the necessary knowledge, skills and attitudes for clinical practice in their scopes of practice. Additionally, the interruption in the clinical training of HCP students caused them to experience psychosocial effects of COVID-19 such as anxiety because of uncertainty about the world (Giordano et al., 2021), as well as fear of contracting the virus and/or infecting others at their clinical placement sites (Rainford, 2021).
All these challenges highlight the need for innovative modes of providing clinical training during public health emergencies, such as during the COVID-19 pandemic, as well as beyond. Technological advances embedded within telehealth have been documented to be valuable to overcome these challenges, even as part of hybrid approaches to clinical training (Khoza-Shangase, Moroe, & Neille, 2021). Technological advances including the fourth industrial revolution have significant potential to overcome the challenges faced by healthcare education, such as mitigating the risk of compromising patients' safety when HCP students learn about patient interactions and procedures on real patients (Guze, 2015). Furthermore, incorporating technology as a means of clinical training in healthcare education may support such a training shift towards competency-based education, as it facilitates basic knowledge acquisition, improves clinical skills and enhances decision-making. Simulation, specifically, allows for the fulfilment of educational goals such as the provision of feedback, repetitive practice, flexibility and the capturing of clinical variability (Guze, 2015).
Therefore, in light of the benefits of simulation training, the resource constraints that may affect HCP students' learning and achievement of the core clinical competencies and the impact that COVID-19 has had on traditional clinical training of student HCPs, this scoping review was aimed at exploring published evidence on simulations as a mode of clinical training in HCPs, to plan for SLP&A training during the COVID-19 pandemic and beyond.
Methodology
The researchers utilised the framework outlined by Arksey and O'Malley (2005) when conducting the scoping review, following five stages: (1) identifying the research question, (2) identifying relevant publications, (3) selecting studies to be included, (4) extracting and charting the data as well as (5) collating, summarising and reporting the results.
Additionally, the authors followed Levac, Colquhoun and O'Brien's (2010) recommendation of using a research team when conducting a scoping review. The research team comprised of five researchers with experience in planning and supervising SLP&A student clinical training. They agreed on the broad research question to be addressed by the scoping review and the overall study protocol including the search terms and the databases to be searched.
Research question
This scoping review sought to answer the following research question: 'what has been documented about simulation as a mode of clinical training in HCPs?' This research question was prompted by the need for alternative or supplemental modes of traditional clinical training to account for clinical training challenges encountered by SLP&A programmes during the COVID-19 pandemic. Findings from this scoping review will guide clinical training planning in SLP&A during the COVID-19 pandemic and beyond. These findings will also inform curriculum, policy formulation and future research.
Data sources and search strategy
The initial search was carried out in December 2021 by N.N. The following databases were searched: Science Direct, PubMed, Scopus, ProQuest, Google Scholar, WordCat and MEDLINE. An exhaustive search of these databases was conducted to obtain papers that pertain to simulation as a mode of clinical training in HCPs. The identified papers were included if they were published in English, because of the limited resources available for translation. The papers also needed to focus on simulation as a clinical training method in HCPs. The search terms were as follows: HCPs, simulation-based education, telesimulation, virtual simulation, clinical training, clinical education, continuous professional education, continuous professional development and COVID-19. The same search strategy was used to search Google Scholar and WorldCat to source grey literature such as research reports, dissertations and theses that discuss simulation as a method of clinical training in HCPs. However, no papers were generated through this search. Additionally, as a method of snowball sampling, the reference lists of the identified papers were screened to capture other papers that potentially met the inclusion criteria.
Citation management
Zotero referencing software was used to save the citations retrieved from the databases. This software allowed for any duplicate citations to be removed. Further duplicate citations, if found, were removed during the title and abstract relevance screening and data characterisation of full articles.
Eligibility criteria
A two-stage screening to assess the eligibility of the papers identified in the search was employed. Publications that contained the keywords and phrases and (if broadly described) simulation as a mode of clinical training in HCPs were included. To account for advancements in technology as well as to capture contemporary evidence, papers that were published between the years 2011-2021 were included in the review. Publications that described simulation without referring to clinical training and HCPs were excluded from the analysis.
Title, abstract and full-text relevance screening
For the first level of inspection, only the title citations were reviewed. Thereafter, the abstracts of those citations that were deemed to be eligible for inclusion at the title level were screened. Next, the full articles of those citations that passed the abstract screening were reviewed. If abstracts were not available, the citations were included for the review of the full article. This review was independently conducted by N.N. and B.S. N.N. created a title, abstract and full-text screening spreadsheet. The researchers discussed any discrepancies in the selected papers. Where consensus was not reached, K.K-S. performed the review to make a final decision. There was a high level of agreement between the researchers as the overall kappa was 0.81 (Dohoo, Martin, & Stryhn, 2012).
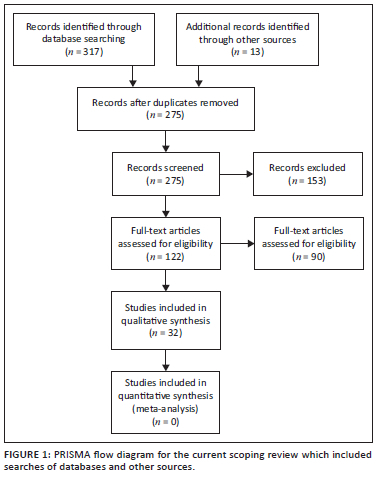
In total, the database search from all databases identified 330 publications. All identified database citations were exported to Zotero, a web-based referencing software. Through Zotero, duplicate studies were identified and removed. After the duplicates were removed, 275 records remained. The 275 records were screened, guided by the search question, and 153 were excluded as not being relevant to the study. One hundred twenty-two articles were then assessed for eligibility; of these, 32 were excluded because they did not meet the inclusion criteria. Consequently, a full-text screening of 90 articles resulted in 32 studies meeting the inclusion criteria and being included in this scoping review. Figure 1 shows a PRISMA flowchart for the literature search, retrieval and inclusion process of this scoping review.
Data characterisation
Relevant information from the publications that met the inclusion criteria was extracted and noted in the data chart. The data were extracted and charted by N.N., B.S. and M.M. The data charted included the author, year of publication, publication type, publication focus and aims, methodology (study design and sample and data sources, measurement of the outcomes post-simulation training), description of simulation training (preparation for the training, briefing, simulation activity and debriefing), context (country) and results (depicted in Table 1).
Data summary and synthesis
The data were compiled in a single spreadsheet and imported into Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA) for descriptive analysis, where thematic analysis was conducted by N.N., K.K-S. and N.M. to analyse the data extracted.
Results and discussion
As depicted in Table 1, 32 papers were included in the final analysis. Of these papers, 21 presented empirical data, whilst 11 were reviews. Of the total sample of studies reviewed, only four were conducted in LMICs, with the rest from high-income countries (HICs). Additionally, 28 of the studies were conducted prior to the COVID-19 pandemic, with only four conducted during COVID-19.
Nuanced analysis of the studies, as reflected in Table 1, revealed that the use of simulation has been investigated in basic medical (e.g. McGaghie et al., 2011; Zhang et al., 2015), surgery (Yang et al., 2020), nursing (e.g. Eide et al., 2020; Teles et al., 2020), radiography (Gunn et al., 2021), physiotherapy (Silberman et al., 2013; Wright et al., 2018) and pharmacy (Korayem & Alboghdadly, 2020) education. The review revealed an obvious gap in evidence regarding the utility of simulation in the clinical training of SLP&A professions, as none of the studies considered in this review explored the use of simulation in audiology, with only one study that explored the utility of simulation in speech-language pathology (Miles et al., 2016). However, this one study focused on simulation usage in teaching interprofessional clinical reasoning in speech-language therapy and dietetic students, and not on core clinical skills in SLP.
Of the studies reviewed, the use of simulation as a mode of clinical training has been explored mostly for undergraduate and postgraduate HCPs students. Very few studies have described its use as a method of continuous professional education in qualified HCPs (e.g. Boudiche et al., 2020; Rossler, Hardin, Hernandez-Leveille, & Wright, 2018), and this is an important area of training for SLP&A in South Africa as continued professional development, particularly with the rapid technological advancements in SLP&A, is a mandated regulation by the Health Professions Council of South Africa (HPCSA). This is despite Rossler et al. (2018) and Boudiche et al. (2020) indicating the effectiveness of simulation training as a continuous professional development tool and HCPs perceiving it to be a valuable clinical training method to enhance their clinical practice.
Thematic analysis of the papers reviewed revealed three themes. These themes that emerged from the data were as follows: (1) face-to-face simulations as a mode of clinical training, (2) virtual reality simulation (VRS) and telesimulation as modes of clinical training and (3) simulation as a complementary mode of clinical training. The rest of the scoping review findings will be presented under these three themes.
Face-to-face simulation as a mode of clinical training
Most of the studies included in this scoping review discussed face-to-face simulations, which comprised at least a simulation scenario and debriefing sessions (e.g. De Ponti et al., 2020; Hu et al., 2019; Shrestha et al., 2020). Although the purpose of conducting debriefing sessions has not been explicitly highlighted in the studies, a finding from one of the studies has alluded to the practice of debriefing as allowing students to reflect on their performance in the simulation scenario and thus improve on their weaker areas before they begin with their clinical placements (Shrestha et al., 2020). The scenarios involved interactions with a variety of simulators ranging from low-fidelity (part-task trainers and low-fidelity manikins) to high-fidelity simulators (high-fidelity manikins and simulated or standardised patients).
In LMICs, it seems that when simulation is used as a mode of clinical training, face-to-face simulations that incorporate low-fidelity simulators and students simulating patients are used (Boudiche et al., 2020; Shrestha et al., 2020; Teles et al., 2020). The authors of this scoping review query if this may be because of high-fidelity simulators being costly. The authors also found it interesting that virtual simulations were never used as a means of training in these countries, especially because virtual training platforms are thought to be feasible for HCPs who work in resource-constrained countries (Asangansi & Braa, 2010). Furthermore, the Medical Council of India (2019) is reforming medical education for it to be competency-based, so they have recommended the incorporation of face-to-face simulations in medical education. This recommendation motivated a review conducted by Kapoor et al. (2021) on the utility of simulated patients as a teaching tool.
The findings from the review revealed that incorporating simulated patients into medical education may allow medical students to achieve the core clinical competencies. Face-to-face simulations improved nurse-midwifery, nursing and physiotherapy students' self-efficacy and confidence (e.g. Silberman et al., 2013; Teles et al., 2020; Wright et al., 2018). It also enhanced nursing and physiotherapy students' knowledge in practically applying and integrating their knowledge in a safe environment (Eide et al., 2020; Offiah et al., 2019). It also enhanced their understanding of the need for collaboration with other HCPs (Eide et al., 2020). Face-to-face simulation also vastly improved nurses' and physiotherapists' clinical task and non-clinical task skills, particularly when high fidelity simulations were used (Kapoor et al., 2021; Silberman et al., 2013; Vermeulen et al., 2017). This may be a result of high-fidelity manikins being able to be programmed to produce physical responses and simulated or standardised patients being able to replicate patient encounters (Kapoor et al., 2021). Utilising high-fidelity simulations does not only allow for the consolidation of knowledge and skills but also seems to provide nursing students with the opportunity to practise providing holistic patient care (Teles et al., 2020). This mode of training may explain why nurses felt prepared to work with real patients and why simulation is considered to improve patient outcomes. Additionally, because face-to-face simulation training enhanced vascular residents' skills in performing surgery, they were able to perform cerebral vascular angiography procedures quicker, which meant that the potential radiation damage caused by this procedure is reduced in residents and patients (Yang et al., 2020).
Although face-to-face simulations have been shown to improve students' clinical competency, there are concerns that skill retention after solely face-to-face simulation training is short (Johnson et al., 2013; Offiah et al., 2019). One way to enhance medical and nursing students' skill retention is for them to repeat the simulation activities (Eide et al., 2020; Offiah et al., 2019). Additionally, studies by Zarifsanaiey et al. (2016), Offiah et al. (2019) and Korayem et al. (2020), as well as those incorporated in McGaghie et al.'s (2011) review, have shown that when face-to-face simulations are supplemented or integrated with other teaching or clinical training methods, pharmacy, medical and nursing students' knowledge and clinical task skills and retention thereof is further enhanced. Furthermore, to allow for the continuation of clinical training of HCPs in the COVID-19 era, some programmes, like anaesthesiology programmes, implemented face-to-face simulations as a mode of clinical training (Büyük et al., 2021).
Virtual reality simulation and telesimulation as modes of clinical training
Face-to-face simulation training was not always possible because of the social distancing regulations implemented during the COVID-19 pandemic. Therefore, medical programmes used telesimulation or VRS to train medical students (De Ponti et al., 2020; Mileder et al., 2012). However, VRS have been used prior to the pandemic. A review by Shorey and Ng (2021) found that VRS, namely, desktop virtual reality and immersive VRS were less costly and less time-intensive than face-to-face simulations that involve manikins. Virtual reality simulation is also not limited by time and space constraints, and students can practise any time. However, technical issues may be incurred when using VRS and telesimulation, which may frustrate students. Furthermore, these types of simulations may lack authentic realism (Gunn et al., 2021).
This lack of authentic realism may explain why HCP students' clinical tasks skills still need to be enhanced in traditional clinical training. This point may be reinforced by the findings of Gunn et al. (2021) and De Ponti et al. (2020), who found that medical imaging and radiation therapy students and medical students, respectively, preferred to learn procedures in traditional clinical placements. However, these students acknowledge that VRS may be used to prepare them for their clinical placements and can be an effective clinical training tool when supplemented with traditional clinical training. However when virtual patients are incorporated in VRS HCP, students' skills seem to be enhanced (Kononowicz et al., 2019). Similarly, telesimulation may allow students to gain knowledge and practise their clinical task skills, but face-to-face simulation is still a preferable means to acquire skills (Mileder et al., 2012). Therefore, although face-to-face simulation training may result in better learning outcomes compared to VRS and telesimulation, VRS and telesimulation have not shown to produce worse learning outcomes compared to face-to-face simulation (Mileder et al., 2021; Shorey & Ng, 2021).
Simulation as a complementary mode of clinical training
A review conducted by Roberts et al. (2019) documented that the clinical core competencies achieved by nursing students whose portion of traditional clinical training hours was replaced by face-to-face simulation were the same as those who only received traditional clinical training. Additionally, a study conducted by Korayem and Alboghdadly (2020) found that integrating face-to-face simulation with traditional clinical training and running these activities simultaneously allowed for the increase in student numbers to be accommodated because of the increase in clinical seats for students. In contexts where simulations have not been widely used as a mode of clinical training, such as South Africa, the current authors believe that the use of simulation as a complementary mode should be deliberated on for gradual and safe introduction of this mode of training in clinical training programmes. This would require more collaborative deliberations between training institutions and the regulating body, the HPCSA, so that such training can form part of the regulations as well as clinical hours for registration, as these changes have already begun during the 2020-2021 period where students were allowed to claim 20% of hours via simulation. Additionally, it is particularly important to consider simulations at least as a complementary mode of clinical training when planning clinical training for South African SLP&As, because ASHA (n.d.) recognises clinical simulation as an alternative means of traditional clinical training for American SLP&A students; meanwhile, the CFCC (2016) has allowed American SLP&A students to obtain 75 hours of direct clinical contact training through the use of simulations.
Conclusion
The current scoping review provides evidence that simulation is an effective method of clinical training in basic and specialised medical education, nursing, radiography, pharmacy and physiotherapy as it enhances the clinical competence of HCP students in these programmes. Therefore, it may equip students with knowledge, skills and attitudes required to interact with patients that they encounter in their clinical placements and independent practice. Simulation, particularly VRS and telesimulation, can be used as a mode of clinical training to allow for the continuation of clinical training of HCP students and practitioners despite the COVID-19 restrictions. However, simulation cannot replace traditional clinical training but may be combined with traditional clinical training in a hybrid mode - which may further enhance HCPs students' clinical competence.
As alluded to earlier, because of resource constraints, the large number of students enrolled in SLP&A programmes cannot be sufficiently accommodated for particularly in terms of clinical placements. Therefore, the current authors recommend deliberations around utilising simulations prior to traditional clinical placements, as a way of hastening acquisition of core clinical competencies, thus allowing students more opportunities to practise (both depth and breadth of the scope of the professions). The improved preparedness may also lessen the workload of clinical educators, whilst enhancing skills for independent safe practice (Cant & Cooper, 2017). Furthermore, if simulation is integrated within traditional clinical training and these modes of training run concurrently, clinical placements may be able to accommodate the increased numbers of students (Korayem & Alboghdadly, 2020). These suggestions, however, require regulatory approval as they have implications for the number of credits for courses as mandated by the South African Qualifications Authority (SAQA) as well as clinical hours required for registration of HCPs by the HPCSA. Furthermore, when considering the use of simulations as a mode of clinical training for South African SLP&A students, reference should be made to guidelines that have outlined the standards of using simulation as a mode of clinical training for SLP&A students, such as the ASHA (n.d.) guidelines.
The studies included in this scoping review have mostly provided insight into the use of simulations for clinical training in HCPs other than SLP&A. However, the studies may still support the consideration for using simulations in SLP&A clinical training, as clinical training in all HCPs is based on the same core clinical competencies (Medical and Dental Professions Board, 2016). When considering simulation as a mode of clinical training, clinical educators' competency in facilitating the activities needs to be considered. Inadequate skills in facilitating simulation activities will result in simulation training being ineffective (Krishnan, Keloth, & Ubedulla, 2017). Therefore, clinical educators facilitating these sessions need to receive training and mentoring regarding using simulators, creating and facilitating simulation activities and integrating simulations into the curriculum so that students can achieve the core clinical competencies (Koukourikos et al., 2019). Whilst simulation in HCP education aims to mimic real-life clinic scenarios, the degree of realism depends on the fidelity of the simulator, the setting and the simulation activity (Kapoor et al., 2021; Koukourikos et al., 2019). Therefore, the degree of realism needs to be accounted for when planning to use simulation as a mode of clinical training. Healthcare professions students seem to acknowledge the benefit of simulations being incorporated into their clinical training, but they still prefer that traditional clinical training be used at least in addition to simulations (e.g. Gunn et al., 2021; Mileder et al., 2021).
Therefore, research on the utility of simulation and how it can be incorporated in SLP&A is required. Specifically for LMICs, whilst simulation has proven to be cost-effective and a responsive mode of training HCPs during public health emergencies as evidenced during COVID-19 and beyond, there are contextual realities that cannot be ignored. These include resources that are not readily available because of finances and poor infrastructure (Khoza-Shangase, 2021), as well as a lag in the uptake of technological advances as part of clinical service provision and training (Khoza-Shangase et al., 2021). Furthermore, LMICs have a large rural population, limited health education and limited access to technology resources within poorly performing economies (Muttiah, McNaughton, & Drager, 2016). Therefore, whilst remote learning, and by extension, telesimulation is effective in HICs, its success in LMICs requires supportive measures such as supplements to poor internet bandwidth, strategies to address shortage of trained personnel (Pillay et al., 2020) and initiatives to improve limited computer skills for users (Khoza-Shangase et al., 2021).
Acknowledgements
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
N.N. was the lead researcher. She conducted the search, title, abstract and full-text screening and extracted the data from the relevant full-text papers. She also analysed the data and wrote the first draft of the paper. B.S. conducted the title, abstract and full-text screening and extracted the data from the relevant full-text papers. M.M. extracted the data from the full-text papers. K.K.-S. and N.M. conceptualised and supervised the project as well as analysed the data. All the other researchers reviewed the drafts of manuscript written and corrected by N.N.
Ethical considerations
This article followed all ethical standards for research without direct contact with human or animal subjects.
Funding information
The authors thank the National Research Foundation for providing financial assistance for the publication of the manuscript.
Data availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
Adams, S.N., Seedat, J., Coutts, K., & Kater, K.-A. (2021). 'We are in this together' voices of speech-language pathologists working in South African healthcare contexts during level 4 and level 5 lockdown of COVID-19. South African Journal of Communication Disorders, 68(1), a792. https://doi.org/10.4102/sajcd.v68i1.792 [ Links ]
Akhlaq, A., McKinstry, B., Muhammad, K.B., & Sheikh, A. (2016). Barriers and facilitators to health information exchange in low-and middle-income country settings: A systematic review. Health Policy and Planning, 31(9), 1310-1325. https://doi.org/10.1093/heapol/czw056 [ Links ]
Al-Elq, A.H. (2010). Simulation-based medical teaching and learning. Journal of Family and Community, 17(1), 35-40. https://doi.10.4103/1319-1683.68787 [ Links ]
Allerton, D.J. (2010). The impact of flight simulation in aerospace. The Aeronautical Journal, 114(1162), 747-756. https://doi.org/10.1017/S0001924000004231 [ Links ]
American-Speech-Language-Hearing Association. (n.d.). Certification standards for speech-language pathology frequently asked questions: Clinical simulation. Retrieved from https://www.asha.org/certification/certification-standards-for-slp-clinical-simulation/
Arksey, H., & O'Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice, 8(1), 19-32. https://doi.org/10.1080/1364557032000119616 [ Links ]
Asangansi, I., & Braa, K. (2010). The emergence of mobile-supported national health information systems in developing countries. Study Health Technology Information, 160(Pt 1), 540-545. [ Links ]
Boudiche, S., Zelfani, S., Hammamia, M.B., Mghaieth, F., Ouaghlani, K., Halima, M.B., ... Mourali, M.S. (2020). Simulation training for continuing professional development of nurses in cardiology and cardiovascular surgery. La Tunisie Medicale, 98(2), 116-122. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32395800/ [ Links ]
Büyük, S., Bermede, O., Erkoç, S., Alkış, N., Lilot, M., & Meço, B. (2021). Use of simulation to teach in the operating room: Don't let the COVID-19 pandemic to interrupt education: An observational clinical trial. Brazilian Journal of Anesthesiology (English Edition), 72(2), 185-188. https://doi.org/10.1016/j.bjane.2021.11.010 [ Links ]
Cant, R.P., & Cooper, S.J. (2017). The value of simulation-based learning in pre-licensure nurse education: A state-of-the-art review and meta-analysis. Nurse Education in Practice, 27, 45-62. https://doi.org/10.1016/j.nepr.2017.08.012 [ Links ]
Choong, J., & Tan, Z.Y. (2019). The role of simulation in burns education. British Journal of Hospital Medicine, 80(12), 716-719. https://doi.org/10.12968/hmed.2019.80.12.716 [ Links ]
Council for Clinical Certification in Audiology and Speech-Language Pathology of the American Speech-Language-Hearing Association (CFCC), 2016, Standards for the certificate of clinical competence in speech-language pathology. Retrieved from http://www.asha.org/Certification/2014-Speech-Language-Pathology-Certification-Standards
Datta, R., Upadhyay, K., & Jaideep, C. (2012). Simulation and its role in medical education. Medical Journal Armed Forces India, 68(2), 167-172. https://doi.org/10.1016/S03771237(12)60040-9 [ Links ]
De Ponti, R., Marazzato, J., Maresca, A.M., Rovera, F., Carcano, G., & Ferrario, M.M. (2020). Pre-graduation medical training including virtual reality during COVID-19 pandemic: A report on students' perception. BMC Medical Education, 20(1), 332. https://doi.org/10.1186/s12909-020-02245-8 [ Links ]
Dohoo, I.R., Martin, W., & Stryhn, H. (2012). Methods in epidemiologic research. Charlottetown: VER Inc. [ Links ]
Eide, W.M., Johansson, L., & Eide, L.S.P. (2020). First-year nursing students' experiences of simulation involving care of older patients. A descriptive and exploratory study. Nurse Education in Practice, 45, 102797. https://doi.org/10.1016/j.nepr.2020.102797 [ Links ]
Feingold, C.E., Calaluce, M., & Kallen, M.A. (2004). Computerized patient model and simulated clinical experiences: Evaluation with baccalaureate nursing students. Journal of Nursing Education, 43(4), 156-163. https://doi.org/10.3928/01484834-20040401-03 [ Links ]
Giordano, L., Cipollaro, L., Migliorini, F., & Maffulli, N. (2021). Impact of COVID-19 on undergraduate and residency training. The Surgeon, 19(5), e199-e206. https://doi.org/10.1016/j.surge.2020.09.014 [ Links ]
Grabowski, A., Chuisano, S.A., Strock, K., Zielinski, R., Anderson, O.S., & Sadovnikova, A. (2021). A pilot study to evaluate the effect of classroom-based high-fidelity simulation on midwifery students' self-efficacy in clinical lactation and perceived translation of skills to the care of the breastfeeding mother-infant dyad. Midwifery, 102, 103078. https://doi.org/10.1016/j.midw.2021.103078 [ Links ]
Griffin, K., McLeod, M., Francis, K., & Brown, A.-M. (2016). Do dummies make good teachers? A paradigm shift for clinical educators. Collegian, 23(3), 321-326. https://doi.org/10.1016/j.colegn.2015.06.005 [ Links ]
Gunn, T., Rowntree, P., Starkey, D., & Nissen, L. (2021). The use of virtual reality computed tomography simulation within a medical imaging and a radiation therapy undergraduate programme. Journal of Medical Radiation Sciences, 68(1), 28-36. https://doi.org/10.1002/jmrs.436 [ Links ]
Guze, P.A. (2015). Using technology to meet the challenges of medical education. Transactions of the American Clinical and Climatological Association, 126, 260-270. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4530721/pdf/tacca1260000260 [ Links ]
Haridy, R., Abdalla, M.A., Kaisarly, D., & Gezawi, M.E. (2021). A cross-sectional multicenter survey on the future of dental education in the era of COVID-19: Alternatives and implications. Journal of Dental Education, 85(4), 483-493. https://doi.org/10.1002/jdd.12498 [ Links ]
Hernández-Padilla, J.M., Granero-Molina, J., Márquez-Hernández, V.V., Cortés-Rodríguez, A.E., & Fernández-Sola, C. (2016). Effects of a simulation-based workshop on nursing students' competence in arterial puncture. Acta Paulista de Enfermagem, 29(6), 678-685. https://doi.org/10.1590/1982-0194201600095 [ Links ]
Hu, F., Yang, J., Yang, B.X., Zhang, F.-J., Yu, S.-H., Liu, Q., ... Chen, J. (2021). The impact of simulation-based triage education on nursing students' self-reported clinical reasoning ability: A quasi-experimental study. Nurse Education in Practice, 50, 102949. https://doi.org/10.1016/j.nepr.2020.102949 [ Links ]
Johnson, R.L., Cannon, E.K., Mantilla, C.B., & Cook, D.A. (2013). Cricoid pressure training using simulation: A systematic review and meta-analysis. British Journal of Anaesthesia, 111(3), 338-346. https://doi.org/10.1093/bja/aet121 [ Links ]
Kapoor, A., Kapoor, A., & Badyal, D.K. (2021). Simulated patients for competency-based undergraduate medical education post COVID-19: A new normal in India. Indian Pediatrics, 58(9), 881-887. https://doi.org/10.1007/s13312-021-2312-5 [ Links ]
Khoza-Shangase, K. (2021). Confronting realities to early hearing detection in South Africa. In K. Khoza-Shangase & A. Kanji (Eds.). Early detection and intervention in audiology: An African perspective (pp. 66-68). Johannesburg, South Africa: Wits University Press. [ Links ]
Khoza-Shangase, K., & Mophosho, M. (2021). Language and culture in speech-language and hearing professions in South Africa: Re-imagining practice. South African Journal of Communication Disorders, 68(1), 9. [ Links ]
Khoza-Shangase, K., Moroe, N., & Neille, J. (2021). Speech-language pathology and audiology in South Africa: Clinical training and service in the era of COVID-19. International Journal of Telerehabilitation, 13(1), 1-31. https://doi.org/10.5195/ijt.2021.6376 [ Links ]
Kononowicz, A.A., Woodham, L.A., Edelbring, S., Stathakarou, N., Davies, D., Saxena, N., ... Zary, N. (2019). Virtual patient simulations in health professions education: Systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research, 21(7), e14676. https://doi.org/10.2196/14676 [ Links ]
Korayem, G.B., & Alboghdadly, A.M. (2020). Integrating simulation into advanced pharmacy practice experience curriculum: An innovative approach to training. Saudi Pharmaceutical Journal, 28(7), 837-843. https://doi.org/10.1016/j.jsps.2020.06.004 [ Links ]
Koukourikos, K., Tsaloglidou, A., Kourkouta, L., Papathanasiou, I.V., Iliadis, C., Fratzana, A., ... Panagiotou, A. (2021). Simulation in clinical nursing education. Acta Informatica Medica, 29(1), 15-20. https://doi.org/10.5455/aim.2021.29.15-20 [ Links ]
Krishnan, D.G., Keloth, A.V., & Ubedulla, S. (2017). Pros and cons of simulation in medical education: A review. International Journal of Medical and Health Research, 3(6), 84-87. [ Links ]
Lambton, J. (2008). Integrating simulation into a pediatric nursing curriculum: A 25% solution. Journal of the Society for Simulation in Healthcare, 3(1), 53-57. https://doi.org/10.1097/SIH.0b013e31815e9964 [ Links ]
Levac, D., Colquhoun, H., & O'Brien, K.K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5(1), 69. [ Links ]
McAllister, L., & Lincoln, M. (2004), Clinical Education in Speech-Language Pathology. London: Wiley-Blackwell. [ Links ]
McGaghie, W.C., Issenberg, S.B., Cohen, E.R., Barsuk, J.H., & Wayne, D.B. (2011). Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Academic Medicine, 86(6), 706-711. https://doi.org/10.1097/ACM.0b013e318217e119 [ Links ]
Medical Council of India, 2019, Skills training module for undergraduate medical education, program. Retrieved from https://www.nmc.org.in/MCIRest/open/getDocument?path=/Documents/Public/Portal/LatestNews/Skill%20!Module_23.12.2019%20(1).pdf
Medical and Dental Professions Board. (2016). Core competencies* for undergraduate students in clinical associate, dentistry and medical teaching and learning programmes in South Africa. Retrieved from https://www.hpcsa-blogs.co.za/wp-content/uploads/2017/04/MDB-Core-Competencies-ENGLISH-FINAL-2014.pdf.
Mileder, L.P., Bereiter, M., & Wegscheider, T. (2021). Telesimulation as a modality for neonatal resuscitation training. Medical Education Online, 26(1), 1892017. https://doi.org/10.1080/10872981.2021.1892017 [ Links ]
Miles, A., Friary, P., Jackson, B., Sekula, J., & Braakhuis, A. (2016). Simulation-based dysphagia training: Teaching interprofessional clinical reasoning in a hospital environment. Dysphagia, 31(3), 407-415. https://doi.org/10.1007/s00455-016-9691-0 [ Links ]
Muttiah, N.A., McNaughton, D., & Drager, K.D. (2016). Providing instructional support for AAC service delivery in low-and middle-income (LAMI) countries. International Journal of Speech-Language Pathology, 18(4), 341353. https://doi.org/10.3109/17549507.2015.1101154 [ Links ]
O'Beirne, G.A., Kelly-Campbell, R.J., & Welch, D. (2020). Simulation in audiology training: Making the most of it. New Zealand Audiological Society Bulletin, 30(1), 24-29. https://hdl.handle.net/10092/101039 [ Links ]
Offiah, G., Ekpotu, L.P., Murphy, S., Kane, D., Gordon, A., O'Sullivan, M., ... Condron, C.M. (2019). Evaluation of medical student retention of clinical skills following simulation training. BMC Medical Education, 19(1), 263. https://doi.org/10.1186/s12909-019-1663-2 [ Links ]
Pham, D.C. (2019, Improving simulation-based training to better serve the maritime community: A comparative research between the aviation and maritime domains (Publication No. 1182). Master dissertation, World Maritime University, World Maritime University Dissertations. Retrieved from https://commons.wmu.se/all_dissertations [ Links ]
Pillay, M., Tiwari, R., Kathard, H., & Chikte, U. (2020). Sustainable workforce: South African audiologists and speech therapists. Human Resources for Health, 18(1), 1-13. http://doi.org/10.1186/s12960-020-00488-6 [ Links ]
Rainford, L.A., Zanardo, M., Buissink, C., Decoster, R., Hennessy, W., Knapp, K., ... McNulty, J.P. (2021). The impact of COVID-19 upon student radiographers and clinical training. Radiography (London, England: 1995), 27(2), 464-474. https://doi.org/10.1016/j.radi.2020.10.015 [ Links ]
Richardson, K.J., & Claman, F. (2014). High-fidelity simulation in nursing education: A change in clinical practice. Nursing Education Perspectives, 35(2), 125-127. https://doi.org/10.1097/00024776-201403000-00012 [ Links ]
Roberts, E., Kaak, V., & Rolley, J. (2019). Simulation to replace clinical hours in nursing: A meta-narrative review. Clinical Simulation in Nursing, 37, 5-13. https://doi.org/10.1016/j.ecns.2019.07.003 [ Links ]
Rossler, K.L., Hardin, K., Hernandez-Leveille, M., & Wright, K. (2018). Newly licensed nurses' perceptions on transitioning into hospital practice with simulation-based education. Nurse Education in Practice, 33, 154-158. https://doi.org/10.1016/j.nepr.2018.10.004 [ Links ]
Shorey, S., & Ng, E.D. (2021). The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse Education Today, 98, 104662. https://doi.org/10.1016/j.nedt.2020.104662 [ Links ]
Shrestha, R., Badyal, D., Shrestha, A.P., & Shrestha, A. (2020). In-situ simulation-based module to train interns in resuscitation skills during cardiac arrest. Advances in Medical Education and Practice, 2011(11), 271-285. https://doi.org/10.2147/AMEP.S246920 [ Links ]
Silberman, N.J., Panzarella, K.J., & Melzer, B.A. (2013). Using human simulation to prepare physical therapy students for acute care clinical practice. Journal of Allied Health, 42(1), 9. [ Links ]
Sun, Y., Pan, C., Li, T., & Gan, T.J. (2017). Airway management education: Simulation based training versus non-simulation based training - A systematic review and meta-analyses. BMC Anesthesiology, 17(1), 17. https://doi.org/10.1186/s12871-017-0313-7 [ Links ]
Teles, M.G., Mendes-Castillo, A.M.C., De Souza Oliveira-Kumakura, A.R., & Silva, J.L.G. (2020). Clinical simulation in teaching pediatric nursing: Students' perception. Revista Brasileira de Enfermagem, 73(2), e20180720. https://doi.org/10.1590/0034-7167-2018-0720 [ Links ]
Vermeulen, J., Beeckman, K., Turcksin, R., Van Winkel, L., Gucciardo, L., Laubach, M., ... Swinnen, E. (2017). The experiences of last-year student midwives with high-fidelity perinatal simulation training: A qualitative descriptive study. Women and Birth, 30(3), 253-261. https://doi.org/10.1016/j.wombi.2017.02.014 [ Links ]
Warren, J.N., Luctkar-Flude, M., Godfrey, C., & Lukewich, J. (2016). A systematic review of the effectiveness of simulation-based education on satisfaction and learning outcomes in nurse practitioner programs. Nurse Education Today, 46, 99-108. https://doi.org/10.1016/j.nedt.2016.08.023 [ Links ]
Wright, A., Moss, P., Dennis, D.M., Harrold, M., Levy, S., Furness, A.L., ... Reubenson, A. (2018). The influence of a full-time, immersive simulation-based clinical placement on physiotherapy student confidence during the transition to clinical practice. Advances in Simulation, 3(1), 3. https://doi.org/10.1186/s41077-018-0062-9 [ Links ]
Yang, L., Li, Y., Liu, J., & Liu, Y. (2020). Effect of vascular simulation training on practice performance in residents: A retrospective cohort study. BMJ Open, 10(9), e037338. https://doi.org/10.1136/bmjopen-2020-037338 [ Links ]
Zarifsanaiey, N., Amini, M., & Saadat, F. (2016). A comparison of educational strategies for the acquisition of nursing student's performance and critical thinking: Simulation-based training vs. integrated training (simulation and critical thinking strategies). BMC Medical Education, 16(1), 294. https://doi.org/10.1186/s12909-016-0812-0 [ Links ]
Zhang, M., Cheng, X., Xu, A., Luo, L., & Yang, X. (2015). Clinical simulation training improves the clinical performance of Chinese medical students. Medical Education Online, 20(1), 28796. https://doi.org/10.3402/meo.v20.28796 [ Links ]
 Correspondence:
Correspondence:
Nabeelah Nagdee
nabeelah.nagdee@wits.ac.za
Received: 31 Jan. 2022
Accepted: 25 Apr. 2022
Published: 02 Aug. 2022














