Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Scientia Militaria: South African Journal of Military Studies
versão On-line ISSN 2224-0020
versão impressa ISSN 1022-8136
SM vol.51 no.1 Cape Town 2023
http://dx.doi.org/10.5787/51-1-1406
ARTICLES
Perceived Barriers Affecting Adherence to Healthy Eating and Exercise Guidelines among Obese Active-Duty Military Personnel of the South African National Defence Force
Magdeline AlcockI; Jacqueline E WolvaardtII
ISouth African National Defence Force School of Health Systems and Public Health University of Pretoria240
IISchool of Health Systems and Public Health University of Pretoria241
ABSTRACT
The World Health Organization defines overweight and obesity as an excessive or a disproportionate accumulation of body fat that impairs health. The South African military community is a subset of the general population, and is not exempt from the effects of overweight and obesity. Military recruitment and operational preparedness are directly affected by obesity as it affects members' physical fitness, overall health, and capacity to perform duties optimally. The South African Military Health Services uses a multidisciplinary approach for the treatment and prevention of obesity and related conditions. Assessing perceived barriers to physical activity and healthy eating within the military environment could contribute to the development of effective and relevant programmes to address weight management and mitigate the health consequences of obesity. The current cross-sectional study was conducted in Bloemfontein, and comprised 58 randomly selected active-duty military personnel diagnosed with obesity, who completed a self-administered questionnaire. Correlation analysis was used to investigate the association between continuous data by calculating the Pearson's correlation coefficient. Analytical statistics, namely the independent T-test or analysis of the variance, was used to compare mean values among groups. The five items identified as barriers to healthy eating habits were liking food too much, difficulty controlling cravings, staying motivated, perceiving healthy food to be expensive, and a lack of will power. The five items identified as barriers to physical activity were a lack of will power to get started, social activities that do not include physical activity, a lack of physical training centres and shower facilities at work, no motivation to stick to a plan for healthy eating, and being too busy. Factors related to the military environment did not affect perceived barriers. A multidisciplinary and coordinated approach might enable the target population to attain better health outcomes, as the identified barriers were related to social and environmental factors and perceptions of self-efficacy. Further investigation into the enablers and motivators of behaviour change in this population would shed more light on addressing the apparent lack of motivation that persists among active-duty military personnel.
Keywords: Obesity, Adherence, Lifestyle, Military, Barriers, Motivation, Behaviour.
Background
Healthy eating and increased physical activity are lifestyle changes that have been shown to be the most affordable and most cost-effective factors in the control and management of non-communicable diseases (NCDs).242 However, individuals who report more perceived barriers to behaviour change have poorer motivation and self-efficacy to change than those who report fewer perceived barriers, according to health behaviour theories, such as social cognitive theory (SCT) and the health belief model (HBM).243 SCT proposes a multidimensional causal framework in which self-efficacy beliefs combine with objectives, outcome expectancies, and perceived environmental barriers and facilitators in the control of human motivation, behaviour and wellbeing. Among the components of the HBM, perceived barriers have been cited as the most significant predictor of behaviour change.244,245 Common examples of these perceived barriers to regular physical activity and practicing healthy eating habits are the absence of exercise facilities, finding time to exercise, willpower, and the cost of healthy food.246,247 Various studies have reported on the barriers to healthy lifestyles experienced by workers as reported in a systematic review by Mazzola.248 Barriers may differ across subgroups of the population. Moreover, the role that the working environment plays in daily health decisions has not been explored sufficiently in the South African National Defence Force, which is one such subgroup. "Barriers" in the context of this study, were defined as elements that active-duty military personnel (ADMP) describe as making it difficult to make healthy food choices or engage in physical activity. For this reason, we wanted to explore associations between perceived barriers to healthy eating and participating in physical activity, and sociodemographic variables of the overweight and obese ADMP, as well as the military-specific aspects, such as rank group, deployment, course attendance, and physical training opportunities.
Overweight and Obesity Globally and in the South African Context
Excessive body weight or the disproportionate accumulation of fat may impair health, and is a known important risk factor for the development of NCDs and higher mortality worldwide.249,250 Known negative effects of overweight and obesity are the higher prevalence of chronic diseases (such as Type 2 diabetes and hypertension) among the obese population when compared to those with a normal body mass index (BMI).9,251,252The World Health Organization (WHO) has reported a substantial global increase in the prevalence of overweight and obesity amongst adults.253 BMI is a measurement of weight in relation to height (reported as weight in kilograms divided by the square of the height in metres or kg/m2), and is used as a screening tool for risk of developing lifestyle diseases. The WHO considers a BMI of > 25 kg/m2 as overweight, and a BMI of > 30 kg/m2 as obese. Findings show that globally 39 per cent of adults (18 years and older) are overweight, while 13 per cent are obese. Furthermore, between 1980 and 2014, the prevalence of obesity nearly doubled worldwide.254
According to the 2014 South African Health and Nutrition Examination Survey (SANHANES-1), obesity levels have increased in South Africa and with them, there was an increased risk of metabolic complications associated with chronic diseases.255 Data from the SANHANES-1 indicate that the BMI, waist circumference, and waist-hip ratio all show an increasing trend among South Africans aged 15 years and older.256 When compared to the 2003 South African Demographic and Health Survey, the SANHANES-1 shows that the greatest increase in mean BMI was in the age group 55 to 64 years of age (28,5 kg/m2 to 31,3 kg/m2), and in people living in the Free State (26,4 kg/m2 to 29,6 kg/ m2).257,258 The 2017 South African Demographic and Health Survey reported a combined prevalence of overweight and obesity of 68 per cent for females and 31 per cent for males.259The same survey reported a 20 per cent prevalence of severe obesity (BMI more or equal to 35 kg/m2) for females and 3 per cent for males.260
The role of diet and physical activity in health and weight management is well known. Healthy eating and increased physical activity are lifestyle changes that have been shown to be the most affordable and cost-effective factors in the control and management of NCDs.261,262 Furthermore, diet and exercise have been identified as major components of the strategy to prevent and control obesity in South Africa.263
Barriers to Healthy Eating and Exercise among South Africans
Various barriers influence participation in exercise and/or physical activity, and practicing healthy eating habits among the South African (SA) general population. Many of the studies conducted focused on specific subgroups of the population, such as female caregivers,264 adolescent girls in rural populations,265 healthcare workers,266 physiotherapy students,267 and first-year university students.268
These studies commonly cited preferences of family members for unhealthy food,269budget restrictions,270 and the cost of healthy food.271,272 The availability of healthy food is not perceived as a barrier in urban settings, but the cost of such food is.273 The availability of healthy options is viewed as a barrier in some,274 but not all, rural settings.275 The convenience and taste of fast food was emphasised in urban settings,276 while peer pressure and aspirations to buy more socially acceptable fast foods were cited in a rural setting.277A lack of motivation for physical activity278 and not enough free time279 are commonly perceived barriers to physical activity.
Overweight and Obesity in the Military Community
The global pattern in overweight and obesity has been noticed in several military communities around the world.280,281,282,283 Obesity in the military community directly affects the readiness to deploy, as well as the performance of duties in the deployment areas. In a 2010 report from the United States, the impact of obesity on military readiness, recruitment, and retention was highlighted. In the 17-24-year-old group, 27 per cent did not meet the BMI standard, and was the primary reason why this group could not enlist.284 In 2015, a longitudinal study done over 13 years showed a high prevalence of overweight and obesity amongst active armed forces personnel in the United States. The most significant increase in the prevalence of obesity was among female soldiers.285
Obesity threatens the overall health as well as the recruitment ability of the military. Bin Horaib et al. report a 40,9 per cent prevalence of overweight and a 29 per cent prevalence of obesity among the Kingdom of Saudi Arabia Military.286 Data from the British Army in 2011 revealed that, of the 50 635 study participants, 56,7 per cent were overweight, and among these, 12 per cent were obese.287 Predictors associated with the prevalence of overweight in military personnel were found to be age, gender, marital status, and military rank.288,289
Obesity in the South African National Defence Force
Although data exist for the prevalence of obesity in the SA context, there is a paucity of data for the military community despite the fact that obesity could affect recruitment for military service, military readiness to deploy and/or be operational, as well as retention of military personnel. In a recent study, Haasbroek et al. found a prevalence of overweight and obesity of 38,6 per cent and 36.1 per cent respectively at an Air Force Base in South Africa.290 A study done in an Army Support Base in Gauteng found a prevalence of overweight (26,3 per cent) and obesity (42,1 per cent) in women and 31 per cent and 35,7 per cent in men respectively.291
The South African Military Health Services (SAMHS) offer comprehensive health care and uses a multidisciplinary approach for the treatment and prevention of obesity and related conditions through its own health centres and three military hospitals.292 The South African National Defence Force (SANDF) also makes provision for regular participation in sport and recreation as well as fitness testing in its Physical Training, Sport and Recreation Policy.293 Despite the provisions made for exercise, not all members comply, and Ngoepe found that fewer women (44 per cent) than men (71,2 per cent) met the requirement of the recommended weekly physical activity.294
The health status of ADMP has been identified by the Department of Defence (DoD) as a strategic issue, as combat readiness of DoD members is directly affected. As part of performing standard physical examination, the BMI and waist-to-hip ratio are measured.295The BMI is used as an appropriate and simple indicator to relate weight-for-height to health outcomes. Apart from athletes and the elderly, the BMI has been shown to be a relatively dependable indicator of adult body fat.296 The maximum cut-off BMI for ADMP in the SANDF of < 30 kg/m2 is considered acceptable, and a BMI of > 30 kg/m2 is used as a cut-off point for referral for intervention.297
All uniformed members of the SANDF are required to do a Concurrent Health Assessment (CHA), which comprises social, psychological, dental, audiology, and medical screening. The CHA focuses on identifying potential health risk factors in ADMP. A comprehensive range of healthcare services (e.g. dietitians, biokineticists, nurses, social workers, psychologists, etc.) is available via the SAMHS, should any of the screening processes indicate a need for intervention.298 Even though lifestyle interventions - which commonly involve combining diet, physical activity and behaviour change - are efficacious strategies, these programmes are often plagued by poor attendance and poor adherence.299 Perceived barriers, which refer to an individual's evaluation of the potential obstacles to adherence, may lessen the likelihood of engaging in a health behaviour. There are numerous studies that have explored predictors of behaviour change in the general population.300,301,302Despite the availability of healthcare practitioners (HCPs) to provide education and guidelines in terms of nutrition, advice about exercise, and policies to promote physical training in the SANDF, ADMP appear to face particular barriers that prevent adherence to recommendations regarding healthy eating and exercise. Factors affecting adherence to dietary and exercise advice and the influence of the unique environment of the SANDF have not been explored sufficiently. The current study examined which factors may be affecting non-adherence of ADMP to diet and exercise guidelines as experienced in the SANDF.
Methods
A cross-sectional descriptive study was conducted.
Participants
Computerised records were used to identify ADMP with a BMI > 30 kg/m2. Participants were randomly selected from these health records, and BMI assessments were performed over the period January 2017 to December 2018. A sample size of 100 was considered adequate for a population of 1 168 members from the 12 participating units. Using a Microsoft Excel®-generated random number selection, 115 members were invited to participate.
Measures
A thorough review of the literature of perceived barriers to following healthy eating and exercise guidelines was completed as part of the design of the questionnaire.303,304,305,306Participants were asked to indicate the likelihood of barriers prohibiting them from following healthy eating habits on a 17-item survey from the work of Sun et al. (2019) who used a four-point Likert-type scale (where very unlikely = 1, somewhat unlikely = 2, somewhat likely = 3, and very likely = 4).307 Barriers to physical activity were assessed by using the Barriers to Being Active Quiz, a 21-item questionnaire developed by the Centers for Disease Control.308 Socio-demographic information and information on participants' working environment were included.
Procedures
Participants were selected based on previous anthropometry measurements, which indicated that they are obese. After recruitment, participants were invited to the health facilities to complete the surveys. Informed consent was signed by all participants, and they received instructions on the completion of the surveys. Anthropometric measurements were performed by the principal investigator to ascertain whether the participants were indeed still obese. Weight measurements were taken twice on the day of assessment for accuracy using a calibrated Seca 876 scale. Participants were weighed without shoes and in minimal clothing. Weight was recorded in kilograms to two decimal places. Height was measurement using a Seca 217 stadiometer, and recorded in meters to two decimal places.
The BMI was calculated in Excel® using the formula weight divided by height in meters squared (kg/m2). The average of two weight readings was used for BMI calculations. Only two participants had a BMI of < 30 kg/m2 and were subsequently excluded from the study.
Data Analysis
The SAS statistical software suite was used for data analysis. According to the Shapiro-Wilk test for normality, the distribution of age of the participants did not follow a normal distribution (W=0.947, p=0.0136). Consequently, the median and inter-quartile range was reported. Sample characteristics were described by means of descriptive statistics.
In the current study, Cronbach's alpha (α) was used to calculate the internal consistency of items in the two barrier subscales, namely barriers to healthy eating and barriers to physical activity. The barriers to healthy eating subscale consisted of 17 items, and the reliability analysis resulted in a Cronbach's alpha (α) of 0.864. The subscale had a good internal consistency (α > 0.80). The barriers to physical activity subscale consisted of 21 items, and the reliability analysis resulted in a Cronbach's alpha (α) of0.895. This subscale also had a good internal consistency (α > 0.80). Each of the items in the subscales was scored by allocating a numerical value to each category of the Likert-type scale (very unlikely = 1, somewhat unlikely = 2, somewhat likely = 3, and very likely = 4). Barriers with a high likelihood consequently also had a high score. For each participant, a total healthy eating barrier score was calculated by adding the scores of all 17 items. The same was done for the physical activity for all 21 items. Correlation analysis was used to investigate the association between continuous data and categorical data by calculating the Pearson's correlation coefficient. Analytical statistics, namely the independent T-test or analysis of the variance (ANOVA), were used to compare mean values among groups. A significance level (α) of 0.05 was used.
Ethical Considerations
Ethical approval was granted by the University of Pretoria, Faculty of Health Sciences Research Ethics Committee (182/2019). Defence Intelligence and 1 Military Hospital Research Ethics Committee gave approval for the study to be conducted on military personnel and premises prior to the commencement of the study. Permission was also granted by the Area Military Health Unit Free State and the Directorate Ancillary Health. Participation was voluntary and anonymous. Each participant received an information sheet about the study, and could withdraw at any time.
Results
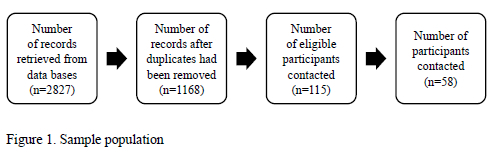
Fifty-eight members agreed to participate (response rate was 50 per cent). Figure 1 represents the process of participant selection. Duplicate records were identified through a search in Excel®.
The majority of the participants were black (African) (64 per cent) with a median age of 43 years and median BMI of 35,7 kg/m2 (Table 1).
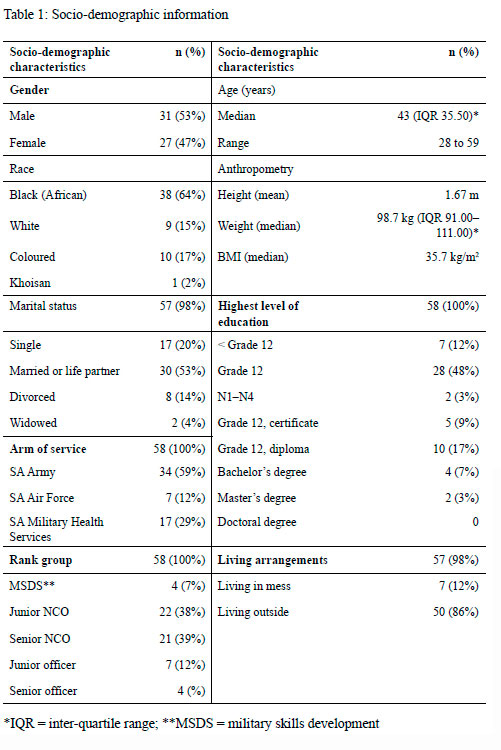
Of the 58 participants, 31 (53 per cent) were male. The sample included mostly noncommissioned officers (NCOs) (n=47), which included military skills development members (MSDS) to Warrant Officers while the officers included ranks from lieutenant to lieutenant colonel (Table 1).
Most of the households consisted of three members (n=15), or four members (n=12); though it ranged from 1 to 8 members. Twenty six per cent of participants were deployed, while 19 per cent were on course for six months or longer in the two years preceding the study. One participant did not respond to the question.
Except for one participant who did not respond, only 12 other participants (21 per cent) had never been referred for diet and/or exercise advice for weight management during their military career. The remaining 45 participants (77 per cent) had received referrals at least once for weight management. Close to two-thirds (64 per cent) of the participants had received structured diet plans to achieve weight loss (Figure 2).

Fifty-nine per cent of the participants (n=34) reported that they had received diet and exercise advice from other HCPs, such as doctors, nurses, or occupational therapists.
The most common barriers to healthy eating were factors related to motivation and/or self-control. The mean and standard deviation (SD) of the 17 items in the barriers to healthy eating subscale are reported in Table 2.

George and Mallery's rule of thumb for the Cronbach's alpha score is when α > 0.9 (excellent), > 0.8 (good), > 0.7 (acceptable), > 0.6 (questionable), > 0.5 (poor), and < 0.5 (unacceptable). The Cronbach's alpha score of α=0.864 for the healthy eating subscale can therefore be considered as good.
For each participant, a total healthy eating barrier score was calculated by adding the scores of all 17 items. The mean for this group was 38.00 (SD=± 10.66).
A lack of motivation and social support and resources (facilities), and being too tired or too busy were the top perceived barriers to physical activity (PBPA) cited by participants (Table 3). There was a lack of any significant relationship between any of the socio-demographic variables and the perceived barriers to healthy eating and physical activity. The Cronbach's alpha for barriers to physical activity was 0.895, which could be considered good.

For each participant, a total physical activity barrier score was calculated by adding the scores of all 21 items. The mean for this group was 44.64 (SD=+/- 12.51).
Factors related to the military environment and application of the Physical Training, Sport and Recreation Policy were explored (Table 4).

Participants answered the open-ended question: "What is the most important thing that stops you from exercising?" Of the 58 participants, 15 participants (26 per cent) indicated that they had no reason for being physically inactive. The remaining 43 participants gave 51 reasons why they were not physically active. Since the participants gave more than one reason, the total is more than 100 per cent (Table 5).

Most participants (86 per cent) stayed outside of the mess (thus not consuming meals provided by the mess). The information on the home food environment was only reported by those living outside of the mess (n=50). Thirty-three participants (66 per cent) indicated that they prepared meals themselves, whereas 21 (42 per cent) reported that their spouse or partners prepared the meals. Others indicated that a child (n=8) or helper (n=2) prepared meals. There were several participants (n=13) who indicated a combination. Twenty-seven participants (54 per cent) ate at least three meals per day. The median budget spent on food and/or groceries was ZAR2 500.00 per household (IQR 2000 to 3000).
The following findings reflect a correlation between participants' budget for food and groceries and PBHE and PBPA scores as reported by those living outside of the mess (n=50). The correlation between the grocery budget and the PBHE mean score was weak (r=0.03) and not significant (p=0.8578). This finding implies that the grocery budget did not have a significant association with the total score for PBHE. There was a weak positive correlation between budget and PBPA mean score (r=0.16). This correlation was however also not significant (p=0.2689). This finding implies that the grocery budget did not have a significant association with PBPA scores.
Pearson's correlation coefficient test was performed to determine any linear correlation between the PBHE data and the demographic data, and between the PBPA data and the demographic sets of data. There was a weak negative correlation between age and the mean total score for PBHEs (r=-0.23), and between age and the mean total score for PBPAs (r=-0.08). Neither correlation was significant (p=0.0822 and p=0.5644 respectively).
The mean scores for PBHE and for PBPA were compared to each of the socio-demographic variables (Table 6), using a one-way ANOVA test. The results for one participant were excluded due to missing information.

Discussion
The current study identified the main barriers to healthy eating and exercise as perceived by active-duty military personnel (ADMP) at one location in South Africa. The sample had a good representation of the different races considering the geographic location. The SA Army had the highest representation in the sample group, which reflected the location - which was land locked - and the number of army units in the area. The majority of the participants were NCOs, and did not have a tertiary qualification (which is not a requirement for NCOs).
Participants indicated individual factors: food taste preference, controlling cravings, motivation, cost of healthy food, and a lack of willpower as the five top barriers to healthy eating. This finding is similar to those reported internationally and locally for the general population. Reported barriers related to price,309,310,311,312,313,314,315time constraints,316,317,318 and daily habits,319 such as a lack of discipline.320 Individual factors were: fondness of good food,321 the preference for fast food or preferred food,322,323 a lack of willpower324,325and peer pressure.326
Studies in military populations consistently found the lack of time as a key PBHE.327,328,329The relative unimportance of time in the current study could be because of different settings, as many SA households include extended family members and/or staff and operational activities. Another barrier on which the current participants did not report was "lack of knowledge" as a key PBHE, although other studies in other settings have reported on this barrier.330,331,332 Similarly, Sigrist et al. did not find a lack of knowledge as a major barrier among senior military officers.333 In the current study, the participants - of whom the majority were not senior military officers - did not view a lack of knowledge as a barrier to either healthy eating or physical activity. This was expected as ADMP have access to various sources of health information, including contact with an HCP and/or a dietitian. The results from the HCP contact and nutrition intervention activities support this notion. In this study, the majority of the study population had been referred to an HCP for weight management at least once, and close to two thirds of participants had received structured diet plans for weight loss. ADMP have access to various sources of health information through regular HCP contact, awareness newsletters on the intranet, and nutrition education presentations and campaigns. The study by Ngoepe on another SA military community found that the median frequency of healthy and unhealthy food intake was the same for men and women in terms of the four food groups,334 which might explain the lack of any difference between the genders in the current study. Literature reports that personal taste and food preference determine food choices in the general population despite the awareness of health issues.335,336,337,338 The current study echoed this finding. In our study, the availability of healthy food options and preparation scored the lowest as a barrier.
The main PBPA identified by participants were related to a lack of motivation, social support, a lack of resources (facilities), and being too tired or too busy. Our findings on physical activity are in line with the literature, with barriers to physical activity identified at both individual and socioeconomic level. Shuval et al. found fatigue, a lack of motivation and time at individual level, as well as a lack of exercise facilities for urban residents, as major barriers.339 The perceived barriers of lack of motivation340 and time341 have similarly been cited in SA studies in the general population. Sigrist et al. found that, in addition to time constraints, a dislike of exercise and the unavailability of exercise facilities were the most common PBPA among US army officers.342 The PBPA with the highest mean score in the current study reflects the lack of willpower or motivation. Factors related to willpower (not able to start, unable to stick to anything, finding excuses) have high mean scores and these could be attributed to self-efficacy. Self-efficacy, as described by Bandura, is a person's conviction in his or her ability to manage his or her own functioning and events that affect his or her life. Motivation, wellbeing, and personal accomplishment can all be affected by a strong sense of self-efficacy or a lack thereof.343 Agazio et al. found perceived self-efficacy and interpersonal influences to be significant predictors of health-promoting behaviours, including physical activity, in active-duty women.344 In the current study, the main reasons for not exercising were confirmed in the responses to the open-ended question.
The current study found routine social activities that do not include physical activity to be a key barrier. McDowell et al. report that engagement in leisure-time physical activity was less likely among older service members.345 Addressing leisure-time activities could be an opportunity to empower members and enhance self-efficacy. Interestingly, the lack of facilities at work had a high mean score, even though 43 per cent of the participants indicated that their individual units had a gymnasium or exercise facility. Nineteen per cent indicated that they had access to these facilities, but only 16 per cent were given the opportunity to exercise during working hours. This unexpected poor access to exercise facilities for a workforce that has to be deployment ready could have been due to the Covid-19 pandemic and subsequent restrictions during the study period. Prohibition on all sport and physical training activities in the SANDF were only lifted in October 2021, which could explain these low percentages.
There were no significant differences in the independent variables (gender, marital status, age, race, rank or educational level) between the groups in the scores for PBHE and PBPA. The weak negative correlation between age and PBHE and PBPA implies that the older members had lower scores, although this association was not significant. De Mestral found a gradual decrease in barriers to healthy eating with age in women in the general population.346 In contrast, McDowell et al. found older ADMP had less adherence to nutrition and physical activity recommendations than young service members.347 This finding could be attributed to more structured meal and activity patterns of younger ADMP who dine in messes or who are based on unit duties and mustering.
There was a lack of a significant relationship between the socio-demographic variables and the PBHE and PBPA. Findings by Kullen et al. reflected the same results for age and gender in PBHE in a military population; however, they found differences between occupational groups in terms of PBHE.348 In the current study, the rank group with the highest mean score for PBHE was junior NCOs, and the lowest score was the MSDS group. Junior officers and junior NCOs scored the highest PBPA, however. These rank groups are considered the workforce that executes most of the daily tasks. Senior NCOs and senior officers are found in leadership and management positions and might have more flexibility in their work schedules than their junior ranks. In this case, the higher PBPA could reflect this military hierarchy, where ADMP are given the opportunity to exercise at work, but cannot do so due to work responsibilities. Only seven participants were living in catered military accommodation, i.e. in a mess, at the time of the study. The living-in members however reported higher PBHE and PBPA, although this finding was not significant. There are various factors that could have influenced their meal patterns and food choices, such as availability and accessibility to healthier food options, not having control over food that they do not prepare, and the timing of meals in dining rooms.349
The relationship between being on course or deployment was insignificant. The results show that members who were deployed (n=15) or on course (n=11) had lower scores for both PBHE and PBPA than members who were not deployed or attending courses. Courses often include physical activity and fitness as a component and could therefore contribute to a reduction in the perceived barriers, particularly in relation to time, access to training equipment, opportunity to exercise, and group support. There are different types of courses with varying levels of activity and academic focus, which might have a different outcome in terms of perceived barriers.
We wanted to understand the extent to which members had access to HCPs, and how this affected perceived barriers. Our results show that a large proportion of the sample had either been referred to and had received nutrition and exercise information or a structured meal plan during the course of their military career. Literature shows previous exposure to nutrition education leads to increased knowledge. This explains why a lack of knowledge was not a key barrier in this study.350 However, increased knowledge does not necessarily translate into behaviour change. Neither access to HCPs nor knowledge had a significant association with perceived barriers. This finding is important, and warrants further investigation. The participants were diagnosed with obesity between 2017 and 2018 and had still not reached their target BMI of < 30 kg/m2 at the time of the current study in 2020 in spite of knowledge and available healthcare services. The number of study participants who had been on a structured meal plan indicated that members were seeking treatment but this had not translated into reduction of their BMI.
The organisational environment could affect physical activity. Having available exercise facilities does not automatically mean that these facilities are accessible. Similarly, having permission to exercise does not translate into having the time to do so during a working day. The results show that, while 43 per cent indicated the unit had access to exercise facilities, only a small fraction of the study participants was given the opportunity to exercise due to Covid-19 restrictions. It has been proved that physical exercise is strongly linked to accessibility and opportunity. Even if exercise choices are available at work, the fact that employees might become sweaty when exercising might function as a further deterrent, especially if there is a lack of shower facilities (making it difficult to turn their intentions into actual healthy exercise behaviours).351 The results of the current study do not necessarily reflect normal circumstances, as no PTSR activities were allowed during the study period due to the Covid-19 pandemic. The Covid-19 pandemic however did not explain the prior lack of success to reduce weight.
Sigrist et al. found that, despite the fact that exercise is an important element of military culture, one-fifth of the participants in their study said they disliked it. Military fitness and weight standards might be the driving forces behind these officers' frequent exercise, outweighing any motivational elements, such as personal medical history, counsel from a healthcare professional or support from family, friends or co-workers.352 Self-control issues have been examined in various studies, and appear to have a significant effect on whether people make good decisions and engage in healthy habits.353 Self-efficacy has also been studied by Agazio et al., as a predictor of healthy habits among military personnel. While requirements are specified by military regulation, self-efficacy on an individual level is required to make the commitment to achieve targets.354
Health promotion and the concurrent health assessments are implemented in the military to ensure a healthy deployable workforce. For these health promotion activities, intervention, and initiatives to be successful, they must recognise that there are barriers to people adopting and engaging in healthy eating and physical activity habits. HCPs could strengthen self-efficacy by empowering ADMP with skills to overcome perceived barriers. One example could be to guide members to set goals that are achievable yet challenging enough to facilitate a sense of accomplishment. The PTSR policy might not be implemented consistently, as not all units have a designated sports officer, and work requirements may not allow time for a training programme to be implemented effectively, especially where members are deployed or tasked outside of their usual work environment or attending courses. Having on-site physical training programmes might be beneficial to encourage physical activity and better adherence.
By identifying these common barriers, specific elements could be targeted to attain good employee health.
Limitations
Due to the outbreak of the Covid-19 pandemic and the mobilisation of SANDF personnel during disaster management, many members were deployed internally making the process of finding available participants difficult. Moreover, some of the members who were contacted were transferred out of the region at the time. The sample size was thus smaller than desired limiting generalisation of the results to the obese military population in South Africa.
The current study did not explore body image perceptions, as this might contribute to the perceived need or desire to lose weight. When presented with body image silhouettes, 87,9 per cent of South Africans indicated that their ideal body image was "fat", which can be attributed to culturally acceptable norms.355 Exploring body image perception could shed further light on the motivational aspect to adhere to eating and exercise guidelines and personal factors in this regard. The current study did not explore participants' views of the potential consequences of continued overweight or obesity for continued employment in the armed forces. The single study site, the cross-sectional study design, the absence of a pilot study, and the use of self-reported data were further limitations in this study. The exploration of an under-researched topic was a strength of the study.
Conclusion
Military regulations governing fitness and weight standards do not appear to be enough of a driving force to motivate ADMP to exercise or eat a healthy diet. As alluded to by the social cognitive theory and the health belief model, individuals who report multiple perceived barriers have poor motivation and self-efficacy to change. From this study, it is evident that a lack of motivation plays a vital role in healthy eating and physical activity among ADMP. Although physical activity is an essential part of military culture, it cannot be assumed that ADMP enjoy exercise. Efforts should be made to include and promote leisure-time activity with family and friends to incorporate physical activity into their lifestyles, which was identified as an important barrier. HCPs could intervene more effectively by implementing strategies that strengthen self-efficacy and motivation to overcome barriers.
Acknowledgements
The author would like to thank the participants for their time, and Maryn Viljoen (University of Free State) for her assistance with the statistical analysis.
240 Magdeline Alcock completed an undergraduate B.Sc Dietetics at the University of the Western Cape in 2000 and her Master of Public Health degree at the University of Pretoria in 2022. She joined the South African National Defence Force (SAMHS) in 2002 at Air Force Base Langebaanweg. Since then she has gained 10 years' experience in the clinical dietetic environment at 1- and 2-Military Hospital. She is currently based in Bloemfontein in a community nutrition capacity. She is passionate about keeping our soldiers as healthy as possible for as long as possible and has focussed her master's research on this topic.
241 Jacqueline Elizabeth Wolvaardt completed an undergraduate degree in nursing (BCur), a Master of Public Health, a Postgraduate Certificate in Higher Education and PhD in Curriculum Development and Instructional Design at the University of Pretoria. She is an Associate Professor at the School of Health Systems and Public Health at the University of Public Health. Her research areas of interest are strengthening health and health systems and undergraduate health professions education. She is an associate editor on two journals and serves on a board of an international journal.
242 BH Goodpaster et al., 'Effects of Diet and Physical Activity Interventions on Weight Loss and Cardiometabolic Risk Factors in Severely Obese Adults: A Randomized Trial', JAMA, 304, 16 (2010), 795-802.
243 A Bandura, 'Health Promotion by Social Cognitive Means", Health Education & Behavior, 32, 2 (2004), 143-164.
244 P Rahman, E Gholamreza, K Seyede Somayeh & T Mahmoud, 'Health Literacy: An Effective Component to Overcome Perceived Barriers to Adoption of Preventive Behaviours in the Health Belief Model', Journal of Education and Community Health, 5, 3 (2018), 1-3.
245 EJ Henshaw & CR Freedman-Doan, 'Conceptualizing Mental Health Care Utilization Using the Health Belief Model', Clinical Psychology: Science and Practice, 16, 4 (2009), 420-439.
246 N Eikenberry & C Smith, 'Healthful Eating: Perceptions, Motivations, Barriers, and Promoters in Low-income Minnesota Communities', Journal of the American Dietetic Association, 104, 7 (2004), 1158-1161.
247 K Silliman, K Rodas-Fortier & M Neyman, 'A Survey of Dietary and Exercise Habits and Perceived Barriers to Following a Healthy Lifestyle in a College Population', Californian Journal of Health Promotion, 18 (2004), 281.
248 JJ Mazzola, AT Jackson & A Thiele, 'Obesity in the Workplace: A Systematic Review of Barriers and Facilitators to Healthy Lifestyles', Occupational Health Science, 3, 3 (2019), 239-264.
249 WPT James, 'WHO Recognition of the Global Obesity Epidemic', International Journal of Obesity, 32, S7 (2008), S120-S6.
250 WPT James, 'Obesity: A Global Public Health Challenge', Clinical Chemistry, 64, 1 (2018), 24-29.
251 WPT James, 'Obesity: A Global Public Health Challenge', Clinical Chemistry, 64, 1 (2018), 24-29.
252 B Adeboye, G Bermano & C Rolland, 'Obesity and its Health Impact in Africa: A Systematic Review', Cardiovascular Journal of Africa, 23, 1 (2012), 512-521. [ Links ]
253 World Health Organization, Obesity and Overweight Factsheet, 2021. <https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight> [Accessed on 27 September 2021].
254 B Adeboye, G Bermano & C Rolland, 'Obesity and its Health Impact in Africa: A Systematic Review', Cardiovascular Journal of Africa, 23, 1 (2012), 512-521.
255 O Shisana et al., South African National Health and Nutrition Examination Survey: SANHANES-1 (Cape Town: HSRC Press, 2013). [ Links ]
256 O Shisana et al., South African National Health and Nutrition Examination Survey: SANHANES-1 (Cape Town: HSRC Press, 2013). [ Links ]
257 South African Medical Research Council, South Africa Demographic and Health Survey 2003, 2007. <https://www.samrc.ac.za/sites/default/files/files/2017-07-03/sadhs2003coverpg.pdf> [Accessed on 21 October 2021].
258 O Shisana et al., South African National Health and Nutrition Examination Survey: SANHANES-1 (Cape Town: HSRC Press, 2013).
259 Stats SA, Statistical Release P0318. General Household Survey 2017 (Pretoria, 2018).
260 Stats SA, Statistical Release P0318. General Household Survey 2017 (Pretoria, 2018).
261 BH Goodpaster et al., 'Effects of Diet and Physical Activity Interventions on Weight Loss and Cardiometabolic Risk Factors in Severely Obese Adults: A Randomized Trial', JAMA, 304, 16 (2010), 795-802. [ Links ]
262 GA Bray, G Frühbeck, DH Ryan & JP Wilding, 'Management of Obesity', Lancet, 387, 10031 (2016), 1947-1956. [ Links ]
263 Department of Health, Strategy for the Prevention and Control of Obesity in South Africa 2015-2020, 2016. <https://extranet.who.int/ncdccs/Data/ZAF_B10_National%20Strategy%20for%20prevention%20and%20Control%20of%20Obesity%204%20August.pdf> [Accessed on 31 July 2018].
264 D Besselink, H Brandt, S Klingberg & CE Draper, 'Perceptions of Healthy Food, and Perceived Facilitators and Barriers to Buying and Consuming Healthy Food, among Female Caregivers in Soweto, South Africa', SAJCH, 16, 3 (2022), 172-177.
265 HM Sedibe, K Khan, K Edin, T Gitau, A Ivarsson & S Norris, 'A Qualitative Study Exploring Healthy Eating Practices and Physical Activity among Adolescent Girls in Rural South Africa', BMC Pediatrics, 14, 211 (2014), 1-9.
266 L Skaal, 'Factors Influencing Healthcare Workers' Participation in Physical Activity in One Public Hospital in South Africa: Do Healthcare Workers Have Barriers to Exercise?', African AJPHERD, 17, 4 (2011), 813-823.
267 D Kgokong & R Parker, 'Physical Activity in Physiotherapy Students: Levels of Physical Activity and Perceived Benefits and Barriers to Exercise', South African Journal of Physiotherapy, 76, 1 (2020), a1399. doi: 10.4102/sajp. v76i1.1399
268 VT Nolan, M Sandada & J Surujlal, 'Perceived Benefits and Barriers to Physical Exercise Participation of First Year University Students', AJPHERD, September Supplement (2011), 56-69.
269 D Besselink, H Brandt, S Klingberg & CE Draper, 'Perceptions of Healthy Food, and Perceived Facilitators and Barriers to Buying and Consuming Healthy Food, among Female Caregivers in Soweto, South Africa', SAJCH, 16, 3 (2022), 172-177.
270 D Besselink, H Brandt, S Klingberg & CE Draper, 'Perceptions of Healthy Food, and Perceived Facilitators and Barriers to Buying and Consuming Healthy Food, among Female Caregivers in Soweto, South Africa', SAJCH, 16, 3 (2022), 172-177.
271 HM Sedibe, K Khan, K Edin, T Gitau, A Ivarsson & S Norris, 'A Qualitative Study Exploring Healthy Eating Practices and Physical Activity among Adolescent Girls in Rural South Africa', BMC Pediatrics, 14, 211 (2014), 1-9.
272 C Vogel, Contribution of the Local Food Environment to the Food Choices of Black Urban Adults in Mamelodi (Master in Consumer Science [Food Management] thesis, University of Pretoria, Pretoria, 2018).
273 NJ Temple, NP Steyn, J Fourie & A de Villiers, 'Price and Availability of Healthy Food: A Study in Rural South Africa', Nutrition, 27, 1 (2011), 55-58.
274 HM Sedibe, K Khan, K Edin, T Gitau, A Ivarsson & S Norris, 'A Qualitative Study Exploring Healthy Eating Practices and Physical Activity among Adolescent Girls in Rural South Africa', BMC Pediatrics, 14, 211 (2014), 1-9.
275 NJ Temple, NP Steyn, J Fourie & A de Villiers, 'Price and Availability of Healthy Food: A Study in Rural South Africa', Nutrition, 27, 1 (2011), 55-58.
276 MK van Zyl, NP Steyn & ML Marais, 'Characteristics and Factors Influencing Fast Food Intake of Young Adult Consumers in Johannesburg, South Africa', South African Journal of Clinical Nutrition, 23, 3 (2010), 24-130.
277 HM Sedibe, K Khan, K Edin, T Gitau, A Ivarsson & S Norris, 'A Qualitative Study Exploring Healthy Eating Practices and Physical Activity among Adolescent Girls in Rural South Africa', BMC Pediatrics, 14, 211 (2014), 1-9.
278 L Skaal, 'Factors Influencing Healthcare Workers' Participation in Physical Activity in One Public Hospital in South Africa: Do Healthcare Workers Have Barriers to Exercise?', African AJPHERD, 17, 4 (2011), 813-823.
279 D Kgokong & R Parker, 'Physical Activity in Physiotherapy Students: Levels of Physical Activity and Perceived Benefits and Barriers to Exercise', South African Journal of Physiotherapy, 76, 1 (2020), a1399. doi: 10.4102/sajp.v76i1.1399.
280 CM Reyes-Guzman, RM Bray, VL Forman-Hoffman & J Williams, 'Overweight and Obesity Trends among Active Duty Military Personnel: A 13-year Perspective', American Journal of Preventative Medicine, 48, 2 (2015), 145-153.
281 G Bin Horaib et al., 'Prevalence of Obesity among Military Personnel in Saudi Arabia and Associated Risk Factors', Saudi Medical Journal, 34, 4 (2013), 401-407.
282 J Peake et al., 'The Health and Cost Implications of High Body Mass Index in Australian Defence Force Personnel', BMC Public Health, 12, 451 (2021), 1-10.
283 PW Sanderson, SA Clemes & SJ Biddle, 'Prevalence and Socio-demographic Correlates of Obesity in the British Army', Annals of Human Biology, 41, 3 (2014), 193-200.
284 Council for a Strong America, Mission Readiness Report: Too Fat to Fight Report, 2010. <https:www.strongnation.org/articles/23-too-fat-to-fight> [Accessed on 21 October 2021].
285 CM Reyes-Guzman, RM Bray, VL Forman-Hoffman & J Williams, 'Overweight and Obesity Trends among Active Duty Military Personnel: A 13-year Perspective', American Journal of Preventative Medicine, 48, 2 (2015), 145-153.
286 G Bin Horaib et al., 'Prevalence of Obesity among Military Personnel in Saudi Arabia and Associated Risk Factors', Saudi Medical Journal, 34, 4 (2013), 401-407.
287 PW Sanderson, SA Clemes & SJ Biddle, 'Prevalence and Socio-demographic Correlates of Obesity in the British Army', Annals of Human Biology, 41, 3 (2014), 193-200.
288 PW Sanderson, SA Clemes & SJ Biddle, 'Prevalence and Socio-demographic Correlates of Obesity in the British Army', Annals of Human Biology, 41, 3 (2014), 193-200.
289 TJ Smit et al., 'Overweight and Obesity in Military Personnel: Sociodemographic Predictors', Obesity, 20, 7 (2012), 1534-1538.
290 C Haasbroek, R Lategan-Potgieter, C van Rooyen & M Jordaan, 'Do Lifestyle Choices Influence the Development of Overweight and Obesity in the South African Air Force, Bloemfontein?', South African Journal of Clinical Nutrition, 35, 2 (2021), 1-10.
291 MM Ngoepe, Meaning in Life in Relation to Healthy Eating, Weight Status and Physical Activity among South African National Defence Force Members at Lenz Military Base (Master of Science in Dietetics thesis, North West University, 2019).
292 Department of Defence, 'Process and Procedures on South African Military Health Service's Health Care Delivery', in Services SAMHS (2013).
293 Department of Defence, Joint Defence Publication: Physical Training, Sport and Recreation, SG00006/2000 (2000).
294 MM Ngoepe, Meaning in Life in Relation to Healthy Eating, Weight Status and Physical Activity among South African National Defence Force Members at Lenz Military Base (Master of Science in Dietetics thesis, North West University, 2019).
295 Department of Defence, 'Process and Procedures on South African Military Health Service's Health Care Delivery', in Services SAMHS (2013).
296 O Shisana et al., South African National Health and Nutrition Examination Survey: SANHANES-1 (Cape Town: HSRC Press, 2013).
297 Department of Defence, 'Process and Procedures on South African Military Health Service's Health Care Delivery', in Services SAMHS (2013).
298 Department of Defence, 'Process and Procedures on South African Military Health Service's Health Care Delivery', in Services SAMHS (2013).
299 E Burgess, P Hassmén & KL Pumpa, 'Determinants of Adherence to Lifestyle Intervention in Adults with Obesity: A Systematic Review', Clinical Obesity, 7, 3 (2017), 123-135.
300 E Burgess, P Hassmén & KL Pumpa, 'Determinants of Adherence to Lifestyle Intervention in Adults with Obesity: A Systematic Review', Clinical Obesity, 7, 3 (2017), 123-135.
301 J Wang, L Ye, Y Zheng & LE Burke, 'Impact of Perceived Barriers to Healthy Eating on Diet and Weight in a 24-month Behavioural Weight Loss Trial', Journal of Nutrition Education and Behavior, 47, 5 (2015), 432-436.
302 JJ Mazzola, JT Moore & K Alexander, 'Is Work Keeping Us from Acting Healthy? How Workplace Barriers and Facilitators Impact Nutrition and Exercise Behaviours', Stress and Health, 33, 5 (2017), 479-89.
303 JJ Mazzola, JT Moore & K Alexander, 'Is Work Keeping Us from Acting Healthy? How Workplace Barriers and Facilitators Impact Nutrition and Exercise Behaviours', Stress and Health, 33, 5 (2017), 479-89.
304 M Baruth, PA Sharpe, D Parra-Medina & S Wilcox, 'Perceived Barriers to Exercise and Healthy Eating among Women from Disadvantaged Neighbourhoods: Results from a Focus Groups Assessment', Women & Health, 54, 4 (2014), 336-353.
305 C de Mestral, S Stringhini & P Marques-Vidal, 'Barriers to Healthy Eating in Switzerland: A Nationwide Study', Clinical Nutrition, 35, 6 (2016), 1490-1498.
306 LD Sigrist, JE Anderson & GW Auld, 'Senior Military Officers' Educational Concerns, Motivators and Barriers for Healthful Eating and Regular Exercise', Military Medicine, 170, 10 (2005), 841-845.
307 R Sun, M Rohay, M Sereika, Y Zheng & E Burke, 'Psychometric Evaluation of the Barriers to Healthy Eating Scale: Results from Four Independent Weight Loss Studies', Obesity, 27, 5 (2019), 700-706.
308 The Centers for Disease Control and Prevention, Barriers to Being Active Quiz. <https://www.cdc.gov/diabetes/ndep/pdfs/8-road-to-health-barriers-quiz-508.pdf> [Accessed on 27 September 2021].
309 N Eikenberry & C Smith, 'Healthful Eating: Perceptions, Motivations, Barriers, and Promoters in Low-income Minnesota Communities', Journal of the American Dietetic Association, 104, 7 (2004), 1158-1161.
310 HM Sedibe, K Khan, K Edin, T Gitau, A Ivarsson & S Norris, 'A Qualitative Study Exploring Healthy Eating Practices and Physical Activity among Adolescent Girls in Rural South Africa', BMC Pediatrics, 14, 211 (2014), 1-9.
311 C Vogel, Contribution of the Local Food Environment to the Food Choices of Black Urban Adults in Mamelodi (Master in Consumer Science [Food Management] thesis, University of Pretoria, Pretoria, 2018).
312 NJ Temple, NP Steyn, J Fourie & A de Villiers, 'Price and Availability of Healthy Food: A Study in Rural South Africa', Nutrition, 27, 1 (2011), 55-58.
313 MK van Zyl, NP Steyn & ML Marais, 'Characteristics and Factors Influencing Fast Food Intake of Young Adult Consumers in Johannesburg, South Africa', South African Journal of Clinical Nutrition, 23, 3 (2010), 24-130.
314 JJ Mazzola, JT Moore & K Alexander, 'Is Work Keeping Us from Acting Healthy? How Workplace Barriers and Facilitators Impact Nutrition and Exercise Behaviours', Stress and Health, 33, 5 (2017), 479-89.
315 M Rao, A Afshin, G Singh & D Mozaffarian, 'Do Healthier Foods and Diet Patterns Cost More than Less Healthy Options? A Systematic Review and Meta-analysis', BMJ Open, 3, 12 (2013), e004277.
316 N Eikenberry & C Smith, 'Healthful Eating: Perceptions, Motivations, Barriers, and Promoters in Low-income Minnesota Communities', Journal of the American Dietetic Association, 104, 7 (2004), 1158-1161.
317 K Silliman, K Rodas-Fortier & M Neyman, 'A Survey of Dietary and Exercise Habits and Perceived Barriers to Following a Healthy Lifestyle in a College Population', Californian Journal of Health Promotion, 18 (2004), 281.
318 JJ Mazzola, JT Moore & K Alexander, 'Is Work Keeping Us from Acting Healthy? How Workplace Barriers and Facilitators Impact Nutrition and Exercise Behaviours', Stress and Health, 33, 5 (2017), 479-89.
319 JJ Mazzola, JT Moore & K Alexander, 'Is Work Keeping Us from Acting Healthy? How Workplace Barriers and Facilitators Impact Nutrition and Exercise Behaviours', Stress and Health, 33, 5 (2017), 479-89.
320 N Eikenberry & C Smith, 'Healthful Eating: Perceptions, Motivations, Barriers, and Promoters in Low-income Minnesota Communities', Journal of the American Dietetic Association, 104, 7 (2004), 1158-1161.
321 C de Mestral, S Stringhini & P Marques-Vidal, 'Barriers to Healthy Eating in Switzerland: A Nationwide Study', Clinical Nutrition, 35, 6 (2016), 1490-1498.
322 D Besselink, H Brandt, S Klingberg & CE Draper, 'Perceptions of Healthy Food, and Perceived Facilitators and Barriers to Buying and Consuming Healthy Food, among Female Caregivers in Soweto, South Africa', SAJCH, 16, 3 (2022), 172-177.
323 MK van Zyl, NP Steyn & ML Marais, 'Characteristics and Factors Influencing Fast Food Intake of Young Adult Consumers in Johannesburg, South Africa', South African Journal of Clinical Nutrition, 23, 3 (2010), 24-130.
324 N Eikenberry & C Smith, 'Healthful Eating: Perceptions, Motivations, Barriers, and Promoters in Low-income Minnesota Communities', Journal of the American Dietetic Association, 104, 7 (2004), 1158-1161.
325 K Silliman, K Rodas-Fortier & M Neyman, 'A Survey of Dietary and Exercise Habits and Perceived Barriers to Following a Healthy Lifestyle in a College Population', Californian Journal of Health Promotion, 18 (2004), 281.
326 HM Sedibe, K Khan, K Edin, T Gitau, A Ivarsson & S Norris, 'A Qualitative Study Exploring Healthy Eating Practices and Physical Activity among Adolescent Girls in Rural South Africa', BMC Pediatrics, 14, 211 (2014), 1-9.
327 LD Sigrist, JE Anderson & GW Auld, 'Senior Military Officers' Educational Concerns, Motivators and Barriers for Healthful Eating and Regular Exercise', Military Medicine, 170, 10 (2005), 841-845.
328 C Kullen, H O'Connor & T Prvan, 'Barriers and Enablers Influencing Dietary Practices in Australian Army Personnel', Military Medicine, 184, 1/2 (2019), E213-E221.
329 CL Chukwura, TJ Santo, CN Waters & A Andrews, '"Nutrition is out of Our Control": Soldiers' Perceptions of Their Local Food Environment', Public Health Nutrition, 22, 5 (2019), 2766-2776.
330 M Baruth, PA Sharpe, D Parra-Medina & S Wilcox, 'Perceived Barriers to Exercise and Healthy Eating among Women from Disadvantaged Neighbourhoods: Results from a Focus Groups Assessment', Women & Health, 54, 4 (2014), 336-353.
331 M Farahmand, FR Tehrani, P Amiri & F Azizi, 'Barriers to Healthy Nutrition: Perceptions and Experiences of Iranian Women', BMC Public Health, 12, 1 (2012), 1-7.
332 M Farahmand, P Amiri, F Ramezani Tehrani, AA Momenan, P Mirmiran & F Azizi, 'What are the Main Barriers to Healthy Eating among Families? A Qualitative Exploration of Perceptions and Experiences of Tehranian Men', Appetite, 89 (2015), 291-297.
333 LD Sigrist, JE Anderson & GW Auld, 'Senior Military Officers' Educational Concerns, Motivators and Barriers for Healthful Eating and Regular Exercise', Military Medicine, 170, 10 (2005), 841-845.
334 MM Ngoepe, Meaning in Life in Relation to Healthy Eating, Weight Status and Physical Activity among South African National Defence Force Members at Lenz Military Base (Master of Science in Dietetics thesis, North West University, 2019).
335 D Besselink, H Brandt, S Klingberg & CE Draper, 'Perceptions of Healthy Food, and Perceived Facilitators and Barriers to Buying and Consuming Healthy Food, among Female Caregivers in Soweto, South Africa', SAJCH, 16, 3 (2022), 172-177.
336 MK van Zyl, NP Steyn & ML Marais, 'Characteristics and Factors Influencing Fast Food Intake of Young Adult Consumers in Johannesburg, South Africa', South African Journal of Clinical Nutrition, 23, 3 (2010), 24-130.
337 M Farahmand, FR Tehrani, P Amiri & F Azizi, 'Barriers to Healthy Nutrition: Perceptions and Experiences of Iranian Women', BMC Public Health, 12, 1 (2012), 1-7.
338 M Farahmand, P Amiri, F Ramezani Tehrani, AA Momenan, P Mirmiran & F Azizi, 'What are the Main Barriers to Healthy Eating among Families? A Qualitative Exploration of Perceptions and Experiences of Tehranian Men', Appetite, 89 (2015), 291-297.
339 K Shuval et al., 'Impediments and Facilitators to Physical Activity and Perceptions of Sedentary Behavior among Urban Community Residents: The Fair Park Study', Preventing Chronic Disease, 10 (2013), E177.
340 L Skaal, 'Factors Influencing Healthcare Workers' Participation in Physical Activity in One Public Hospital in South Africa: Do Healthcare Workers Have Barriers to Exercise?', African AJPHERD, 17, 4 (2011), 813-823.
341 D Kgokong & R Parker, 'Physical Activity in Physiotherapy Students: Levels of Physical Activity and Perceived Benefits and Barriers to Exercise', South African Journal of Physiotherapy, 76, 1 (2020), a1399. doi: 10.4102/sajp.v76i1.1399.
342 LD Sigrist, JE Anderson & GW Auld, 'Senior Military Officers' Educational Concerns, Motivators and Barriers for Healthful Eating and Regular Exercise', Military Medicine, 170, 10 (2005), 841-845.
343 A Bandura, 'Health Promotion by Social Cognitive Means", Health Education & Behavior, 32, 2 (2004), 143-164.
344 JG Agazio & K Buckley, 'Finding a Balance: Health Promotion Challenges of Military Women', Health Care for Women International, 31, 9 (2010), 848-868.
345 MA McDowell & VS Hubbard, 'Adherence to National Diet and Physical Activity Objectives among Active Duty Military Personnel: What are the Implications?', Journal of the Academy of Nutrition and Dietetics, 113, 7 (2013), 903-906.
346 C de Mestral, S Stringhini & P Marques-Vidal, 'Barriers to Healthy Eating in Switzerland: A Nationwide Study', Clinical Nutrition, 35, 6 (2016), 1490-1498.
347 MA McDowell & VS Hubbard, 'Adherence to National Diet and Physical Activity Objectives among Active Duty Military Personnel: What are the Implications?', Journal of the Academy of Nutrition and Dietetics, 113, 7 (2013), 903-906.
348 CJ Kullen, J-L Farrugia, T Prvan & H O'Connor, 'Relationship between General Nutrition Knowledge and Diet Quality in Australian Military Personnel', British Journal of Nutrition, 115, 8 (2016), 1489-1497.
349 MA McDowell & VS Hubbard, 'Adherence to National Diet and Physical Activity Objectives among Active Duty Military Personnel: What are the Implications?', Journal of the Academy of Nutrition and Dietetics, 113, 7 (2013), 903-906.
350 CJ Kullen, J-L Farrugia, T Prvan & H O'Connor, 'Relationship between General Nutrition Knowledge and Diet Quality in Australian Military Personnel', British Journal of Nutrition, 115, 8 (2016), 1489-1497.
351 JJ Mazzola, AT Jackson & A Thiele, 'Obesity in the Workplace: A Systematic Review of Barriers and Facilitators to Healthy Lifestyles', Occupational Health Science, 3, 3 (2019), 239-264.
352 LD Sigrist, JE Anderson & GW Auld, 'Senior Military Officers' Educational Concerns, Motivators and Barriers for Healthful Eating and Regular Exercise', Military Medicine, 170, 10 (2005), 841-845.
353 JJ Mazzola, AT Jackson & A Thiele, 'Obesity in the Workplace: A Systematic Review of Barriers and Facilitators to Healthy Lifestyles', Occupational Health Science, 3, 3 (2019), 239-264.
354 JG Agazio & K Buckley, 'Finding a Balance: Health Promotion Challenges of Military Women', Health Care for Women International, 31, 9 (2010), 848-868.
355 B Adeboye, G Bermano & C Rolland, 'Obesity and its Health Impact in Africa: A Systematic Review', Cardiovascular Journal of Africa, 23, 1 (2012), 512-521.














