Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Curationis
On-line version ISSN 2223-6279
Print version ISSN 0379-8577
Curationis vol.37 n.2 Pretoria 2014
http://dx.doi.org/10.4102/curationis.v37i1.1251
ORIGINAL RESEARCH
doi:10.4102/curationis.v37i1.1251
Improving the quality of nursing documentation: An action research project
Elisha M. OkaisuI; Florence KalikwaniI; Grace WanyanaI; Minette CoetzeeII
ICURE Children's Hospital of Uganda, Mbale, Uganda
IIThe Child Nurse Practice Development Initiative, School of Child and Adolescent Health, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: Documentation is an important function of professional nursing practise. In spite of numerous improvement efforts globally, inadequate documentation continues to be reported as nurse authors investigate barriers and challenges.
OBJECTIVES: The project aimed to improve nurses' documentation of their patient assessments at the CURE Children's Hospital of Uganda in order to enhance the quality of nursing practise.
METHOD: An action research methodology, using repeated cycles of planning, intervention, reflection and modification, was used to establish best practise approaches in this context for improving nurses' efficacy in documenting assessments in the patient record. The researchers gathered data from chart audits, literature reviews and key informant interviews. Through analysis and critical reflection, these data informed three cycles of systems and practise modifications to improve the quality of documentation.
RESULTS: The initial cycle revealed that staff training alone was insufficient to achieve the project goal. To achieve improved documentation, broader changes were necessary, including building a critical mass of competent staff, redesigned orientation and continuing education, documentation form redesign, changes in nurse skill mix, and continuous leadership support.
CONCLUSION: Improving nursing documentation involved complex challenges in this setting and demanded multiple approaches. Evidence-based practise was the foundation of changes in systems required to produce visible improvement in practise. The involved role of leadership in these efforts was very important.
Introduction
Assessment is the first standard of nursing practise (American Nurses Association 2010). Adequate assessment is essential in guiding interventions and evaluating the effect of care. Assessment includes gathering, validating and analysing subjective (symptoms) and objective (signs) information about a patient's health status. Assessment directly influences the nurses' plan of care, (Taylor et al.2011:559) and is necessary for continuous provision of quality care. It is therefore important that nursing assessment is communicated accurately and stored effectively in the patient record.
In a British study, Rothman et al. (2012) found that substandard documentation of nursing assessments was associated with increased in-hospital and post-discharge mortality. Initial chart audits of documentation at the CURE Children's Hospital of Uganda (CCHU) revealed that the quality of the documentation of nurses' assessments was poor. Nursing leadership therefore undertook to work with nurses to improve the standard of documentation.
Problem statement
CCHU uses paper-based documentation, with the scientific nursing process as the documentation guiding framework. However, audits of patient records for quality assurance purposes and morbidity and mortality reviews revealed poor documentation of nursing assessments and other pertinent patient care information. Since the majority of nurses employed at the hospital were enrolled nurses with limited experience and little formal training in nursing assessment.
Aim
This project aimed to improve the documentation of nursing assessments in the patient record as a step toward improving nursing practise at the hospital.
Background
CCHU: CCHU is a specialist paediatric neurosurgical teaching hospital, located in Mbale, Eastern Uganda. The hospital's focus is treatment of children with hydrocephalus, neural tube defects (including spina bifida), and epilepsy and brain tumours.
During the study period (2008-2012), the hospital had 40 beds (30 ward beds and 10 Intensive Care Unit [ICU] beds). There were, on average, 1230 admissions each year; 1180 of these children were being seen for the first time.
At CCHU the nursing service is led by a nurse manager and an assistant-nurse manager. A charge nurse on each shift is responsible the day-to-day running of each of the ward, ICU and operating room or theatre. The nursing care activities are organised under a total patient care delivery model in which the primary care nurse is responsible for all the care of a group of patients throughout the shift. The hospital employed 34 primary care nurses, the majority of whom were enrolled nurses. Enrolled nurses are registered with the Uganda Nurses and Midwives Council after a three year training programme in general nursing science or comprehensive (nursing & midwifery) nursing science. This level of training requires an Ordinary-level certificate (11 years of schooling) for entry into the training programme. Diploma and baccalaureate nursing training programmes require an Advanced-level certificate (13 years) and graduates are registered nurses.
Uganda: The economic cost of treating children with neurosurgical disease is substantial in developed and low resource countries alike (Rabiu & Adeleye 2013). Location in the developing world makes achieving quality health care delivery a difficult goal for a variety of reasons, not least of which is the limited availability of resources. Competent nursing as a resource is fundamental if quality outcomes for patients and hospitals are to be realised. In the authors' experiences of teaching in nursing colleges in Uganda (i.e. non-baccalaureate training institutions), critical thinking (including models like the scientific nursing process), clinical reasoning and evidence-based practise are infrequently emphasised in nursing education. The principle approach to teaching and in clinical settings seems to be task-based rather than patient-centred. Recent evidence shows that task-based care is associated with increased risk for adverse events (Dubois et al. 2013:113).
Baccalaureate nurse training in Uganda started in 1993 (Klopper & Uys 2013). Both nursing service leaders were bachelor-prepared nurses who had a sound knowledge base in scientific processes and patient-centred care. The nursing leadership was able to identify the first step in changing established practise (from a task-based model to patient-centred practise) as the need to improve the nurses' knowledge and skills in assessment and documentation. The long-term goal was to achieve professional nursing practise that met the needs of the high acuity, neurosurgical paediatric patients and their families.
Literature review
Documentation is reported to take up to 50% of nurses' time per shift (Gugerty et al. 2007:6). It serves a number of important functions, including communication amongst healthcare workers for continuity of care. Poor communication, in a broader sense, is known to contribute significantly to the occurrence of adverse events in healthcare (The Joint Commission 2012) and is therefore an important target of initiatives to improve patient safety. Additionally, documentation is important for education, research, quality assurance and for reimbursement by third party claimants (DeLaune & Ladner 2011:216). According to Wilson et al. (2012), nursing documentation can serve as an indicator of quality nursing practise. Additionally Collins et al. (2013) demonstrated that nursing documentation could be used to predict mortality.
According to Jefferies, Johnson and Griffiths (2010:119), quality nursing documentation meets seven criteria: (1) patient-centred, (2) contains the actual work of nursing, (3) reflects the nurses' clinical judgment, (4) is presented in a logical sequence, (5) is written in real time, (6) records variances in care and (7) fulfils legal requirements. Prideaux (2011) argues that the quality of nursing documentation in many countries remains poor due to numerous reasons which different authors articulated. A Dutch study found inadequate documentation of important aspects of assessment and other related nursing care, including inaccuracy of documentation (Paans et al.2010). A Swedish study reported incongruence between what is documented and actual physical patient status (Gunningberg & Ehrenberg 2004), and limited documentation of the work of nurses in an Australian study was documented by Jefferies, Johnson and Nicholls (2011). These inadequacies could be related to challenges in two areas: the nurses' individual characteristics and work environments (Cheevakasemsook et al. 2006; Taylor 2003).
Nurses' perceptions and attitudes towards documentation impact the quality of how and what they document. Studies in various settings found that whilst nurses consider documentation important for nursing professionalisation, they consider it a burdensome secondary task that takes nurses away from direct patient care (Blair & Smith 2012; Björvell, Wredling & Thorell-Ekstrand 2003b). Also, as nurses consider increasing liability for their practise, their documentation may be negatively affected (Brown 2013; Cartwright-Vanzant 2010). Furthermore, knowledge of the nursing process, which forms the basis for nursing documentation, has been found to be inadequate (Ofi & Sowunmi 2012; Allen 1998).
The workplace environment can contribute to poor documentation. Heavy workloads, laborious documentation forms, fragmentary language (i.e. documentation language that is not understood beyond the local context), inadequate resources and hospital culture all impact the quality of nurses' documentation (Prideaux 2011; Jefferies, Johnson & Nicholls 2011; Taylor 2003; Björvell, Wredling & Thorell-Ekstrand 2003b).
Given the significance of nursing documentation and the reality of poor documentation practises, it is not surprising that there have been resolute calls and subsequent efforts to improve its quality (Whitcomb et al. 2013).
Training nurses to improve knowledge, skills and documentation practises has been a widely used strategy. For example, Jefferies et al. (2012) used a writing coach programme to improve documentation quality. Training has been augmented by using written practise standards (Considine, Potter & Jenkins 2006); standardised nursing records, or a nursing model (Tornvall, Wahren & Wilhelmsson 2009; Björvell, Wredling & Thorell-Ekstrand 2003a).
Research method and design
This project utilised action research and action learning methods. Revans (1982) first described action learning as the process in which groups of people that carry real responsibility in real conditions work together on real issues or problems. When this process has the added element of rigorous tracking to gain understanding and knowledge, action research takes place. Dick (2002) states that reflection that is critical, regular and systematic allows more confidence in the research outcomes. In this study, the flexible spiral process of action research, involving stages of planning, implementation, evaluation and modification allowed action (change and improvement) and research (understanding and knowledge) to be achieved at the same time. The reflective cycles utilised in this study are the 'tight cycles' described by Dick (2002) of action and critical reflection before the next action. Figure 1 shows the action research process applied in three phases of this effort to improve nursing documentation. In Phase 1, action (training) and critical reflection on the training, informed Phase 2, resulting in change in practise and systems. In Phase 3 these were further refined to achieve the project goal - improved documentation of nursing assessments.

Phase 1
Training workshop
Methods
Data from patient records revealed poor documentation of nursing assessments. Informal interviews of nursing leadership (key informants) identified inadequate training as a likely explanation for substandard documentation.
In October 2008 a five-day training workshop for all nurses employed at the hospital was planned and conducted by a multi-disciplinary team involving the hospital anaesthesiologist, medical officers, nurse managers and human resources staff (see Figure 1, Phase 1). The training comprised topics on assessment and professional nursing practise. Trainees had access to preceptor and mentorship support post-training.
One month following the training, the researchers compared all records of patients admitted and discharged during a one week period.
Results
Whilst training participants displayed improved assessment techniques, the chart audit showed no observable change in documentation practises. Comparison of the 2008 post-training documentation practises and content showed they were very similar to records made by different nursing personnel in 2001-2003. Therefore, training alone was insufficient to change practise.
Reflection on these findings pointed to a cultural component of documentation practise that would need to be addressed to achieve observable change in documentation of nursing assessments. The culture was defined in relation to the values, attitudes, competencies and patterns of behaviour (Feng, Bobay & Weiss 2008) of the nurses at the hospital.
Phase 2
Modification of orientation programme and developing a documentation template
Methods
In Phase 1, the researchers identified a cultural component of nursing documentation practise that was a barrier to change and conducted a literature review to gain further understanding of the concept of culture in healthcare. Interviews with nursing staff, and visiting nursing students and professors from the United States provided additional perspective.
Findings guided modifications to the content and organisation of the hospital's traditional two-month orientation programme for newly hired nursing staff (Table 1). The modifications aimed to teach a new patient-centred way of thinking and doing, to consolidate the new preferred knowledge and documentation practises, and to create a critical mass of staff that would help drive the efforts to change the culture and sustain the practise change and improvement process.
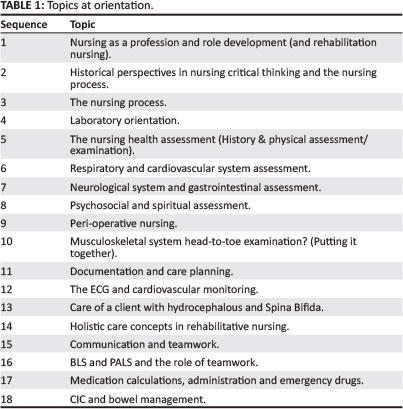
Topics from the 5-day workshop on documentation were incorporated into the orientation to address identified gaps. The first month of orientation was changed to exclusively classroom-based training with only limited ward time so that the new nurses learned the preferred knowledge and practises prior to exposure to the targeted undesirable practises and cultural norms. The second month of orientation included a mentorship period that socialised the new nurses to the ward, operating room or theatre and ICU environments. During this second month of orientation, the new nurses shadowed full-time employees and were oriented to other hospital departments (e.g. radiology, laboratory and physiotherapy).
Further, the researchers developed a new form to facilitate complete documentation of nursing assessments on admission and discharge. The form prompted documentation of a comprehensive nursing history and physical examination aligned with processes taught during orientation.
Charge nurses on the wards reviewed and commented on the redesigned assessment documentation form.
Results
This second cycle of action research focused on initiating the process of culture change in two areas: professional nursing development - orientation, and systems changes - the redesign of the assessment documentation forms.
The charge nurses indicated that the first draft of the revised documentation form - a ruled paper with headings for complete health assessment - was unduly laborious. The form required much writing and relied on nurses' recall of what to document. Therefore, the form needed modification before it could be introduced to the wards.
After implementation of the modified orientation programme, but before implementation of the new documentation forms, chart audits revealed improvement in newly hired nurses' documentation at admission, and on a shift-by-shift basis. However, this change was not sustained; in spite of continual feedback and training, the documentation content and practise of new nursing staff reverted to the established inadequate documentation style.
Reflecting on this, the researchers concluded that the power of the culture was too strong to sustain improvement with new nurses quickly taking on the prevalent practises. It was concluded that the form would need to be easier to use in order to support adoption of the new form and documentation practises.
Phase 3
System changes towards professionalisation
Methods
Phase 2 initiated the process of culture change. The purpose of Phase 3 was to build on the changes that, though not sustained, had been visible. A literature review on culture, quality improvement and change management focused reflection on systems changes as drivers of changes in practise. Necessary systems changes included: (1) redesign testing and implementation of the admission assessment form, (2) change in employment policy, and (3) new focus on creating a healthy working environment based on the American Association of Critical-Care Nurses' (AACCN) standards (2005);
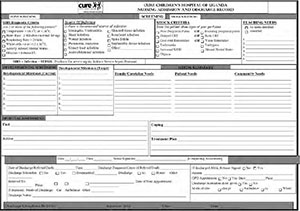
- Form redesign: Beginning in June 2010, the corresponding author and a group of nurses in orientation training redesigned the admission assessment form with review and commentary by charge nurses. The modified form was pilot tested with the ward nursing staff during August 2010. Results from the pilot guided further modification and retesting during October 2010. Nurses began using the new Nursing Admission and Discharge Record form in January 2011 (see Appendix 1).
- Employment policy: In 2010, in an attempt to professionalise nursing at the hospital and change the culture, nursing and hospital leadership changed policy to employ only registered nurses (RNs) with a diploma, rather than enrolled nurses. The charge nurse positions were to be filled by baccalaureate-prepared nurses. Efforts to reach appropriate staffing levels were guided by the development of a staffing policy, including stipulating the education levels of the nurses employed.
- Healthy work environment: Efforts to transform the working conditions at CCHU were initiated in January 2010. Nursing leadership prioritised four areas most likely to produce change: authentic leadership, meaningful recognition, skilled communication and appropriate staffing. The former two areas required a change in leadership style, increased efforts to develop and grow nursing leadership through training, nurses' personal development and continual reflection, and recognition of nurses' work. Nurses were trained in skilled communication through monthly continuing education sessions and enhanced mentorship.
Results
Learning from the previous phase, the researchers planned to refine the documentation form(s) and modify other systems factors (appropriate staffing and healthy work environment), to achieve sustainable change in documentation practise:
- The nursing admission and discharge record: This form was redesigned to make it simple to use, requiring standardised content, limited need for recall and minimal writing, whilst still enabling the capture of all information needed for the comprehensive nursing assessment. The form is a 3-page admission and discharge record requiring check off of items needed for a comprehensive assessment of a child with neurological disability in the local context (Appendix 1). It requires documentation in a standardised format that reflects a deliberate thinking process and problem-solving approach, based on the American Heart Association's Paediatric Advanced Life Support assessment (Kleinman et al. 2010). New nurses were trained, audited and supervised using this assessment approach and it formed the basis for continuing education efforts.
The CCHU nurses' experiences of providing care to children with neurological illness informed content revisions along with new evidence regarding the follow-up of children with neurological disability. According to Warf, Wright and Kulkarni (2011), mortality of children with spina bifida is more strongly related to their home and/or community situation than in-hospital factors. Consequently, a section to gather information about the child's and family's home and community environments, especially healthcare services and social support systems, was incorporated into the admissions form. The form includes a focus on family composition and the parents' relationships with in-laws who, according to information gathered from the parents, seemed to have a significant influence on how family decisions are made, including decisions on healthcare seeking behaviour and follow-up. The researchers anticipated that collecting this data would alert the nurses to child and family needs and inform an individualised plan that would facilitate adherence to the follow-up schedule and positively influence patient outcomes. Further, the revised documentation form assesses spirituality and belief systems. Furthermore, screening on admission for sepsis and shock was included based on anecdotal evidence in this setting that suggested that these conditions were prevalent and often missed:
- Skill mix of nurses: Up to 2010, the nursing skill mix at the hospital comprised both enrolled and RNs, with a predominance of enrolled nurses (see Table 2). Considering the limited resources, along with the need for sustained improved outcomes, nursing leadership decided to employ only RNs. This decision was supported by research evidence showing that increasing the proportion of staff nurses with higher levels of education ultimately led to improved outcomes (Aiken et al. 2003). Further, the model of total patient care delivery used at the hospital requires a widened scope of practise, strong critical thinking and clinical reasoning skills (Tiedeman & Lookinland 2004) more characteristic of RNs. Retention of RNs was also better than the retention of enrolled nurses. Consequently, in 2013 there was a higher proportion of RNs providing direct care at the hospital: 88% compared to 31% in 2008 (Table 2).
- Healthy work environment: Efforts to improve the work environment focused on authentic leadership, meaningful recognition, skilled communication and appropriate staffing. The intent was to enhance nurses' feelings of self-worth, confidence and respect by meaningfully recognising their contributions.
- Authentic leadership: The nurse managers implemented transformational leadership theory as the core strategy to create authentic leadership (Cummings et al. 2010; Mcfadden, Henagan & Gowen 2009; Krause & Hidley 2009). Mentorship activities focused on: (1) challenging the prevailing work processes, (2) inspiring shared vision, (3) empowerment, (4) modelling the way and (5) encouraging the heart through attention to personal things (Evans 2007). The continuous education team led by a charge nurse and supervised by the nurse manager's office set monthly objectives for knowledge and skills building. Nursing leadership and the nurses evaluated progress immediately post-training and at monthly meetings.
- Meaningful recognition: Leadership fostered recognition of the work of nurses through intentional affirmation during daily interactions and monthly meetings. Letters of recognition of exceptional work were written to individual nurses from the executive director and human resource manager.
- Skilled communication: Training in communication skills is ongoing and is a core of the continuous education efforts, especially during monthly simulated resuscitation trainings.
- Appropriate staffing: Policies on staffing were developed and are still being modified in light of other issues affecting nursing including staff turnover and resource availability.

Ethical considerations
The nursing department leadership initiated this practise improvement project and the hospital administration was aware of it. Participation by nurses was voluntary. Data was gathered and reported whilst ensuring anonymity and confidentiality.
Discussion
To achieve sustained improvement in the quality of nurses' documentation of their assessments required a change in the culture of nursing at CCHU along with modification of systems, continual training, mentorship and strong innovative nursing leadership.
Culture
Culture, in relation to patient safety and quality improvement in healthcare, comprises the values, attitudes, competencies and patterns of behaviour of employees (Feng et al. 2008). Organisational culture is complex, stable, invisible and difficult to describe, yet is known to be powerful in determining how the organisation will function (Krause & Hidley 2009; Schein 2004).
Organisational culture seems to drive and sustain change in quality improvement efforts by creating a new norm of practise. At the hospital, culture change was achieved through recruiting and socialising new nurses into new ways of thinking, thereby building a critical mass of staff with similar values, beliefs, attitudes and competencies in relation to professional nursing practise (Oliver, Marwell & Teixeira 1985). This strategy was successful in changing the nurses' documentation practises, thus creating a new documentation practise norm.
Early in the project new nurses adopted improved practises, but quickly reverted to the established norm reinforced by the culture. This failure to sustain improvements elucidated a need for 'systems thinking' to consolidate the change in documentation practise. According to Waldman and Schargel (2006):
Systems thinking suggests that one can only understand (and subsequently improve) a system by looking at how all the parts interact; focusing on, even optimising, parts in isolation will not optimise final (rather than in process) outcomes. (p. 118)
Therefore, sustained change was made possible when multiple interventions were implemented in concert. These were: (a) redesigned orientation and continual training, (b) standardised documentation forms, (c) recruitment of highly educated nurses and (d) improvement of the work environment.
The nursing admission and discharge record
The creation of a new documentation practise norm required redesigned forms to facilitate efficient comprehensive assessment and documentation. In addition, the form established a new way of thinking and practicing, and demonstrates the significant system changes made at the hospital over a four-year period. The revised documentation form also represents progress towards professionalisation and increasing visibility of nursing through quality documentation (Pearson 2003). The use of evidence (Warf, Wright & Kulkarni 2011) to focus on patients' and families' social circumstances enabled planning of care and follow-up that is cognisant of the obstacles to adherence to this plan.
Skill mix of nurses
Nursing leadership focused on improving nurses' skills in care planning and clinical reasoning, as well as documentation. The hospital faced a challenge of high nurse turnover, mostly due to nurses going back to school to upgrade from enrolled nursing (EN) to registered nursing (RN, Diploma). This phenomenon is not unique to this setting; it is common to nursing globally with various consequences (Hayes et al. 2012; Waldman et al. 2004). The high turnover rate presented an opportunity to adopt a policy of employing nurses with higher levels of education. This policy change was supported by evidence that higher education levels of nurses are related to improved outcomes for patients and nurses (Kutney-Lee, Sloane & Aiken 2013; Dubois et al. 2013; Twigg et al. 2012; Aiken et al. 2011; Aiken et al. 2003). It is important to note that these authors refer mainly to the proportion of nurses with a baccalaureate degree. However, due to feasibility and resource limitations, this principle was used to employ nurses with the highest possible educational level.
Nursing professional practise environment
A nursing practise environment refers to 'the work settings' organisational characteristics that either facilitate or constrain professional nursing practice' (Dubois et al. 2012:6). That the environment in which nurses practise impacts both patient and nursing outcomes (including, job satisfaction, turnover and burn out) is well documented (Aiken et al. 2011; Aiken et al. 2003). Therefore, improving the work environment in order to improve quality of care and reduce turnover was an essential component of this project. Nursing leadership adopted transformational leadership practises to improve patient, nurse and hospital outcomes.
Conclusion
The purpose of this project was to improve the documentation of nursing assessments in the patient record, initially through training. However, three cycles of action research revealed that training alone was insufficient. Sustainable practise change required multi-pronged efforts to change organisational culture and modify systems to support rather than hinder, practise change. Successful efforts were based on the best available evidence, including nurses' experiences in providing care and patients' experiences of receiving care.
Acknowledgements
The authors would like to thank and acknowledge the CURE Children's Hospital of Uganda and especially the nursing staff for their willing and enthusiastic participation in the project to improve their practise.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
E.M.O. (CURE Children's Hospital of Uganda) was responsible for project planning, design and implementation and preparation of the manuscript. F.K. (CURE Children's Hospital of Uganda) was responsible for project design and policy and decision making during this period. G.W. (CURE Children's Hospital of Uganda) was involved in Phase 3 implementation. M.C. (University of Cape Town) was responsible for manuscript preparation.
References
Aiken, L.H., Clarke, S.P., Cheung, R.B., Sloane, D.M. & Silber, J.H., 2003, 'Educational levels of hospital nurses and surgical patient mortality', Journal of the American Medical Association 290(12), 1617-1623. http://dx.doi.org/10.1001/jama.290.12.1617 [ Links ]
Aiken, L.H., Cimiotti, J. P., Sloane, D. M., Smith, H. L., Flynn, L. & Neff, D. F., 2011, 'The effects of nurse staffing and nurse education on patient deaths in hospitals with different work environments', Medical Care 49(12), 1047-1053. http://dx.doi.org/10.1097/MLR.0b013e3182330b6e [ Links ]
Allen, D., 1998, 'Record-keeping and routine nursing practice: The view from the wards' Journal of advanced nursing 27, 1223-1230. http://dx.doi.org/10.1046/j.1365-2648.1998.00645.x [ Links ]
American Association of Critical-Care Nurses, 2005, 'AACN standards for establishing and sustaining healthy work environments: A journey to excellence', viewed 18 September 2013, from http://www.aacn.org/WD/HWE/Docs/HWEStandards.pdf [ Links ]
American Nurses Association, 2010, 'Nursing: Scope and standards of practice, 2nd edn., Silver Spring, MD, Nursesbooks.org, n.p. [ Links ]
Björvell, C., Wredling, R. & Thorell-Ekstrand, I., 2003a, 'Improving documentation using a nursing model', Journal of advanced nursing34(4), 402-410. http://dx.doi.org/10.1046/j.1365-2648.2003.02751.x [ Links ]
Björvell, C., Wredling, R. & Thorell-Ekstrand, I., 2003b, 'Prerequisites and consequences of nursing documentation in patient records as perceived by a group of registered nurses', Journal of clinical nursing 12, 206-214. http://dx.doi.org/10.1046/j.1365-2702.2003.00723.x [ Links ]
Blair, W. & Smith, B., 2012, 'Nursing documentation: Frameworks and barriers', Contemporary nurse 41(2), 160-168. http://dx.doi.org/10.5172/conu.2012.41.2.160 [ Links ]
Brown, A., 2013, 'Nursing: Frequently in the bull's eye for noncompliance', Nurse Leader 11(1), 46-47, 51. http://dx.doi.org/10.1016/j.mnl.2012.08.006 [ Links ]
Cartwright-Vanzant, R., 2010, 'Medical record documentation: Legal aspects in neonatal nursing', Newborn & infant nursing reviews10(3), 134-137. http://dx.doi.org/10.1053/j.nainr.2010.06.008 [ Links ]
Cheevakasemsook, A., Chapman, Y., Francis, K. & Davies, C., 2006, 'The study of nursing documentation complexities', International Journal of Nursing Practice, 12, 366-374. http://dx.doi.org/10.1111/j.1440-172X.2006.00596.x [ Links ]
Collins, S.A., Cato, K., Albers, D., Scott, K., Stetson, P.D., Bakken, S. et al., 2013, 'Relationship between nursing documentation and patients' mortality', American Journal of Critical Care 22(4), 306-313. http://dx.doi.org/10.4037/ajcc2013426 [ Links ]
Considine, J., Potter, R. & Jenkins, J., 2006, 'Can written nursing practice standards improve documentation of initial assessment of ED patients?', Australasian Emergency Nursing Journal 9, 11-18. http://dx.doi.org/10.1016/j.aenj.2006.03.004 [ Links ]
Cummings, G.G., MacGregor, T., Davey, M., Lee, H., Wong, C. A., Lo, E., Muise, M. et al. 2010, 'Leadership styles and outcome patterns for the nursing workforce and environment: A systematic review', International Journal of Nursing Studies 47, 363-385. http://dx.doi.org/10.1016/j.ijnurstu.2009.08.006 [ Links ]
DeLaune, C.S. & Ladner, K.P., 2011, Fundamentals of nursing standards & practice, 4th edn., Cengage Learning, New York. [ Links ]
Dick, B., 2002, 'Action Research: Action and research', viewed 21 October 2013, from http://www.aral.com.au/resources/aandr.html [ Links ]
Dubois, C-A., D'Amour, D., Tchouaket, E., Rivard, M., Clarke, S. & Blais, R., 2012, 'A taxonomy of nursing care organization models in hospitals', BMC Health Services Research, 12:n.p. [ Links ]
Dubois, C-A., D'Amour, D., Tchouaket, E., Clarke, S., Rivard, M. & Blais, R., 2013, 'Associations of patient safety outcomes with models of nursing care organizations at unit level in hospitals', International Journal for Quality in Health Care 25(2), 110-117. http://dx.doi.org/10.1093/intqhc/mzt019 [ Links ]
Evans, L.M., 2007, 'Developing the role of leader', in P.S. Yoder-Wise, Leading and managing in nursing, 4th edn., pp. 27-43, Elsevier, St. Louis. [ Links ]
Feng, X., Bobay, K. & Weiss, M., 2008, 'Patient safety culture in nursing: A dimensional concept analysis', Journal of advanced nursing63(3), 310-319. http://dx.doi.org/10.1111/j.1365-2648.2008.04728.x [ Links ]
Gugerty, B., Maranda, M.J., Beachley, M., Navarro, V.B., Newbold, S., Hawk, W. et al., 2007, 'Challenges and Opportunities in Documentation of the Nursing Care of Patients', Baltimore, Documentation Work Group, Maryland Nursing Workforce Commission, viewed 21 July 2013, from http://www.mbon.org/commission2/documenation_challenges.pdf [ Links ]
Gunningberg, L. & Ehrenberg, A., 2004, 'Accuracy and quality in the nursing documentation of pressure ulcers: a comparison of record content and patient examination', Journal of Wound Ostomy & Continence Nursing 31(6), 328-335. http://dx.doi.org/10.1097/00152192-200411000-00004 [ Links ]
Hayes, L.J., O'Brien-Pallas, L., Duffield, C., Shamian, J., Buchan, J., Hughes et al., 2012, 'Nurse turnover: A literature review - an update', International Journal of Nursing Studies 49, 887-905. http://dx.doi.org/10.1016/j.ijnurstu.2011.10.001 [ Links ]
Jefferies, D., Johnson, M. & Griffiths, R., 2010, 'A meta-study of the essentials of quality nursing documentation', International Journal of Nursing Practice 16, 112-124. http://dx.doi.org/10.1111/j.1440-172X.2009.01815.x [ Links ]
Jefferies, D., Johnson, M. & Nicholls, D., 2011, 'Nursing documentation: How meaning is obscured by fragmentary language' Nurse outlook 59, E6-E12. [ Links ]
Jefferies, D., Johnson, M., Nicholls, D. & Lad, S., 2012, 'A ward-based writing coach program to improve the quality of nursing documentation', Nurse education today 32, 647-651. http://dx.doi.org/10.1016/j.nedt.2011.08.017 [ Links ]
The Joint Commission, 2012, 'Sentinel Event Data: Root causes by event type 2004-2012', viewed 11 August 2013, from http://www.jointcommission.org/assets/1/18/Root_Causes_Event_Type_04_4Q2012.pdf [ Links ]
Kelly, T.F., Brandon, D.H. & Docherty, S.L., 2011, 'Electronic nursing documentation as a strategy to improve quality of patient care',Journal of nursing scholarship 43(2), 154-162. http://dx.doi.org/10.1111/j.1547-5069.2011.01397.x [ Links ]
Kleinman, M.E., Chameides, L., Schexnayder S.M., Samson, R.A., Hazinski M.F., Atkins, D.L. et al., 2010, 'Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care', Pediatrics126(5), e1361-e1399, viewed July 2014, from http://www.ncbi.nlm.nih.gov/pubmed/20956434 [ Links ]
Klopper, H. & Uys, L., 2013, The State of Nursing and Nursing Education in Africa: A Country-by-Country Review, Sigma Theta Tau International, Indianapolis. [ Links ]
Krause, T.R. & Hidley, J. H., 2009, 'Taking the lead in patient safety: How healthcare leaders influence behavior and create culture', John Wiley & Sons, Inc., Hoboken, NJ. [ Links ]
Kutney-Lee, A., Sloane, D.M. & Aiken, L.H., 2013, 'An increase in the number of nurses with baccalaureate degrees is linked to lower rates of postsurgery mortality', Health Affairs 32(3), 579-586. http://dx.doi.org/10.1377/hlthaff.2012.0504 [ Links ]
McFadden, K.L., Henagan, S.C. & Gowen, C.R., 2009, 'The patient safety chain: Transformational leadership's effect on patient safety culture, initiatives, and outcomes', Journal of Operations Management 27(5), 390-404. http://dx.doi.org/10.1016/j.jom.2009.01.001 [ Links ]
Ofi, B. & Sowunmi, O., 2012, 'Nursing documentation: Experience of the use of the nursing process model in selected hospitals in Ibadan, Oyo state, Nigeria', International Journal of Nursing Practice 18, 354-362. http://dx.doi.org/10.1111/j.1440-172X.2012.02044.x [ Links ]
Oliver, P., Marwell, G. & Teixeira, R., 1985, 'A theory of the critical mass. I. interdependence, group heterogeneity, and the production of collective action', American Journal of Sociology 91(3), 522-556. http://dx.doi.org/10.1086/228313 [ Links ]
Paans, W., Sermeus, W., Niewag R.M.B. & Van der Schans, C.P., 2010, 'Prevalence of accurate nursing documentation in patient records', Journal of Advanced Nursing 66(11), 2481-2489. http://dx.doi.org/10.1111/j.1365-2648.2010.05433.x [ Links ]
Pearson, A., 2003, 'The role of documentation in making nursing work visible', International Journal of Nursing Practice 9, 271. http://dx.doi.org/10.1046/j.1440-172X.2003.00442.x [ Links ]
Prideaux, A., 2011, 'Issues in nursing documentation and record-keeping practice', British Journal of Nursing 20(22), 1450-1454. http://dx.doi.org/10.12968/bjon.2011.20.22.1450 [ Links ]
Rabiu, T.B. & Adeleye, A.O., 2013, 'Prevention of myelomeningocele: African perspectives', Child's Nervous System 29, 1533-1540. http://dx.doi.org/10.1007/s00381-013-2126-4 [ Links ]
Revans, R.W., 1982, 'The origins and growth of Action Learning', Chartwell-Bratt Ltd, Bromley. [ Links ]
Rothman, M.J., Solinger, A.B., Rothman, S.I. & Finlay, G.D., 2012, 'Clinical implications and validity of nursing assessments: A longitudinal measure of patient condition from analysis of the electronic medical record', British Medical Journal Open 2(4), 1-6. [ Links ].
Schein, E. H., 2004, Organizational culture and leadership, 3rd edn., Jossey-Bass, San Francisco. [ Links ]
Taylor, C.R., Lillis, C., LeMone, P. & Lynn, P., 2011, Fundamentals of nursing: The art and science of nursing, 7th edn., Lippincott Williams & Wilkins, Philadelphia. [ Links ]
Taylor, H., 2003, 'An exploration of the factors that affect nurses' record keeping', British Journal of Nursing 12(12), 751-758. http://dx.doi.org/10.12968/bjon.2003.12.12.11338 [ Links ]
Tiedeman, M.E. & Lookinland, S., 2004, 'Traditional models of care delivery: What have we learned?', Journal of Nursing Administration34(6), 291-297. http://dx.doi.org/10.1097/00005110-200406000-00008 [ Links ]
Tornvall, E., Wahren, L.K. & Wilhelmsson, S., 2009, 'Advancing documentation - an intervention study using patients with leg ulcer as an example', International journal of medical informatics 78, 605-617. http://dx.doi.org/10.1016/j.ijmedinf.2009.04.002 [ Links ]
Twigg, D., Duffield, C., Bremner, A., Rapley, P. & Finn, J., 2012, 'Impact of skill mix variations on patient outcomes following implementation of nursing hours per patient day staffing: A retrospective study', Journal of Advanced Nursing 68(12), 2710-2718. http://dx.doi.org/10.1111/j.1365-2648.2012.05971.x [ Links ]
Waldman, J.D. & Schargel, F.P., 2006, 'Twins in trouble (II): Systems thinking in healthcare and education', Total Quality Management17(1), 117-130. http://dx.doi.org/10.1080/14783360500250040 [ Links ]
Waldman, J.D., Kelly, F., Arora, S. & Smith, H.L., 2004, 'The shocking cost of turnover in healthcare', Health Care Management Review29(1), 2-7. http://dx.doi.org/10.1097/00004010-200401000-00002 [ Links ]
Warf B.C., Wright, E.J. & Kulkarni, A.V., 2011, 'Factors affecting survival of infants with myelomeningocele in southeastern Uganda',Journal of Neurosurgical Pediatrics 7, 127-133. http://dx.doi.org/10.3171/2010.11.PEDS10428 [ Links ]
Whitcomb, J.J., Seawright, J., Flehan, A. & Echols L., 2013, 'A retrospective study evaluating responses time and survival from cardiopulmonary arrest: A creative inquiry project with undergraduate nursing students', Dimensions of critical care nursing 32(1), 50-53. http://dx.doi.org/10.1097/DCC.0b013e3182768399 [ Links ]
Wilson, S., Hauck, Y., Bremner, A. & Finn, J., 2012, 'Quality nursing care in Australian paediatric hospitals: A Delphi approach to identifying indicators', Journal of Clinical Nursing 21, 1594-1605. http://dx.doi.org/10.1111/j.1365-2702.2011.04004.x [ Links ]
 Correspondence:
Correspondence:
Elisha Okaisu
The Child Nurse Practice Development Initiative
5th Floor, ICH Building
Klipfontein Road
Rondebosch 7700
South Africa
Email: elisha.okaisu@gmail.com
Received: 15 Jan. 2014
Accepted: 18 Aug. 2014
Published: 03 Dec. 2014
Appendix 1
Appendix 1: Nursing admission and discharge record: page 1.
Appendix 1: Nursing admission and discharge record: page 2.
Appendix 1: Nursing admission and discharge record: page 3.