Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Curationis
versão On-line ISSN 2223-6279
versão impressa ISSN 0379-8577
Curationis vol.36 no.1 Pretoria Jan. 2013
ORIGINAL RESEARCH
Compliance or non-compliance of hypertensive adults to hypertension management at three primary healthcare day clinics in Tshwane
Gloria N. Mafutha; Susana C.D. Wright
Adelaide Tambo School of Nursing Science, Tshwane University of Technology, South Africa
ABSTRACT
The objective of this article was to report on the rate of compliance to medication, sodium use and appointment keeping of hypertensive adults who are attending primary healthcare clinics in Tshwane. Despite the availability of effective management of hypertension globally, non-compliance to management still exists. This article reports on the hypertensive adult's compliance to medication, sodium use and appointment keeping. The design was a cross-sectional descriptive study. The sample was n =101 hypertensive patients from three primary healthcare clinics. Structured interviews were used to gather the data. The results indicated a variation in compliance rate depending on the question asked. When investigating whether the participants received enough medication on their last visit to the clinic, 98% said that they received enough medication to last them a month (Nkosi 2008:130). However, the appointment-keeping scale revealed that 23% of the participants reported that they left the clinic without prescribed medication or missed an appointment. When, using the Hill-Bone Compliance Scale, individuals were asked a question using the verb forgetting, 9 out of 10 would answer 'no', but when the verb decide was used to determine compliance, 6 out of 10 would admit to deciding not to take their medication sometimes. In terms of sodium use, 33% showed good compliance and 44% low compliance (Nkosi 2008:138). Compliance with regard to taking hypertension medication was 70%, which is good. This study recommends that compliance to hypertension management be assessed by asking questions specifically for sodium use, medication and appointment keeping as it was clear from the findings of this study that a person would comply with appointment keeping but not take medication daily as prescribed or not use sodium as recommended.
Introduction
Despite the availability of several guidelines for hypertension management globally, noncompliance still exist (Halpern et al. 2006:1039-1948; Patel & Davis 2006:439). Non-compliance to hypertension medication can lead to the development of chronic hypertension, which damages the walls of the blood vessels and can cause hypertrophy and hyperplasia associated with fibrosis of the tunica intimae (Nkosi 2008:69). The issue of non-compliance to therapy is not new; patients who are suffering from chronic diseases, particularly those with fluctuating or no symptoms such as hypertension, are likely to be non-compliant (Vlasnik, Aliotta & De Lor 2005:269).
Non-compliance is the fundamental cause of uncontrolled hypertension in South Africa (Seedat & Rayner 2011:79). A recent study conducted in a South African mine revealed poor control of hypertension in South Africa (Maepe & Outhoff 2012:32). The authors conducted a one year hypertension prevalence study in one of the gold mines in Gauteng, South Africa. They discovered that of the 4297 participants (where 99% were Black and 90% male with the mean age of 44) 39.5% had hypertension and only 42% were on antihypertensives. Only 13% of the total population (4297) had a blood pressure of < 140/90 mmHg. Such poor control of hypertension indicates that hypertension will continue to be the cause of disability-adjusted life years (DALYs).
Compliance is the extent to which a person's behaviour is in line with medical advice (Thrall, Lip & Lane 2004:595). Nunes et al. (2009:40) describes compliance as a behaviour change in accordance with a direct request without internal acceptance. The Standard Treatment Guideline and Essential Drug List (Department of Health 2003:61-67) states that if the first step fails to control the high blood pressure, the healthcare provider has to move to the next step, in which the patient's medication increases. This kind of practice might be a risk for non-compliance (Frishman 2007:257). The same guideline also outlines how adherence and non-adherence could be determined, with no specific questions set out for lifestyle modification compliance (Department of Health 2003:xxvii). Assessing compliance by asking questions regarding both medication and lifestyle modification regimen might be the best way to determine compliance and improving the level of hypertension control in South Africa.
Problem statement
In South Africa, approximately 6.3 million people are hypertensive, and the management of the condition is poor (Charlton, Steyn & Levitt 2007:1). The National Demographic Health Survey found that of the individuals living with hypertension, only 39% reported that they had the condition. Less than a third (29%) of the hypertensive participants was diagnosed and on medication, whilst only 14% was well controlled (Department of Health, MRC & OrcMacro 2007:217). The same survey reports that hypertension in South Africa was poorly controlled. Such poor levels of control might lead to hypertension being the cause DALYs if measures are not taken to improve the control of hypertension in South Africa.
It light of the poor control of hypertension in South Africa, this article aims to report on the contrast in compliance to sodium use, medication and appointment keeping. This article emerges from the study 'Management practices and nutrition related knowledge of hypertensive adults in Ga-Rankuwa' (Nkosi 2008).
Research question
The research question for the purpose of this article is: 'What is the compliance of hypertensive adults attending Ga-Rankuwa primary healthcare day clinics in Tshwane?'
Objective
The objective of the study by Nkosi (2008) was to explore the nutrition knowledge and management practices of hypertensive adults in three clinics at Ga-Rankuwa.
The objective of this article is to indicate the contrast in compliance to medication, sodium use and appointment keeping of hypertensive adults attending day clinics in Ga-Rankuwa.
Research method and design
Design
The design was quantitative, cross sectional and descriptive in nature. A cross sectional study differs from a longitudinal study in that it uses observation representing a single point in time (Babbie & Mouton 2004:641).
Context of the study
The study was contextual in nature and was conducted in Ga-Rankuwa, a township in Pretoria, Gauteng Province, South Africa. The population during the time of the study was 83 900 and households were 21 100 (Nkosi 2008:22).
In terms of socio-cultural groups, the majority (74%) were Setswana-speaking people. The educational level below Grade 10 was 56.8%, whereas 12.2% had post Grade 12 education. In addition, only 32.7% of the population were employed (Statistics South Africa 2001).
Population
The study participants were hypertensive, above 18 years old, living in Ga-Rankuwa and attending one of the three primary healthcare clinics in Ga-Rankuwa for hypertension management. The sampling method was convenient and the sample size was 101 (n = 101) participants. A consensus sampling method was used for the primary healthcare day clinics, thus three healthcare clinics were included in the study. At each clinic the researchers aimed to collect data for the first 30 participants that came for consultation at the clinic on the day of data collection. However, in one of the clinics data was collected from 41 participants (Nkosi 2008:124).
Data-collection methods
Self-report was used as data-collection method (Nkosi 2008:105). Trained fieldworkers conducted the structured interviews to prevent selection bias because of low literacy. The questionnaire had several sections focusing on nutrition related knowledge and management practices that a hypertensive person should have (see Box 1).
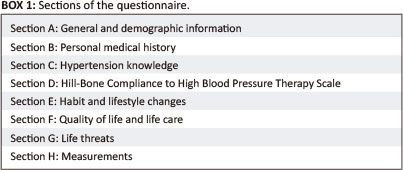
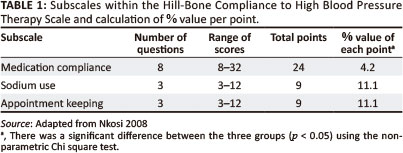
One of the components of the questionnaire, the Hill-Bone Compliance to High Blood Pressure Therapy Scale, was a 4 point Likert scale instrument focussing on compliance in terms of medication, salt use and appointment keeping (see Table 1) (Kim et al. 2000:90-96). As no validated cut off points existed for the scale (Kim et al. 2000:90-96), a decision was taken to label 80% and above as good compliance, between 70% and 79.9% as moderate compliance and 69.9% and below as poor compliance.
Data analysis
The Statistical Product and Service Solutions (SPSS) statistical software package (version 14) was used to analyse the data, descriptive statistics and inferential statistics (Nkosi 2008:134).
Results
General and demographic profile
The participants were represented by 78 women and 23 men aged from 20 to 80 (Nkosi 2008:124). The 51-60 year age group constituted the average of the sample at 29.7% of the group (Nkosi 2008:125). The majority of the sample (63.3%) had primary school education or less and in line with the advanced age, 65.3% were pensioners (Nkosi 2008:125). In terms of socio-cultural group, the majority (74%) was Setswana-speaking people.
Personal medical history
Regarding medical history, the most prevalent risk factors in the sample were high blood cholesterol (34.7%) and diabetes mellitus (19.8%) (Nkosi 2008:130). Regarding family history, the prevalence of obesity, hypertension and diabetes ranged from 30.7% to 34.7%.
In order to explore compliance questions varied. Almost all participants (98%) responded positively to the question 'At your last visit, did you receive enough medication to last you until your visit today?' (Nkosi 2008:135). In response to the question '[h]ow often do you take your blood pressure medication prescribed by the doctor?', 31.7% admitted that they occasionally forgot to take their medication (Nkosi 2008:135). Furthermore, only 18.8% of the participants responded that they did not drink their medication the morning before consultation at the clinic. When exploring missed appointments, 16.8% of the participants admitted to missing an appointment the past year (Nkosi 2008:135). An few reasons for missing the appointment were provided, including transport (7.9%) and other commitments or work-related obstacles (5%) (Nkosi 2008:130).
Hill-Bone Compliance to High Blood Pressure Therapy Scale
The Hill-Bone Compliance to High Blood Pressure Therapy Scale provides several insights into the participants' compliance with regard to their medication (see Table 2) (Nkosi 2008:155).
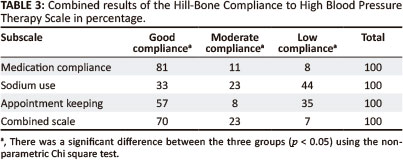
Three subscales are included in the Hill-Bone Compliance to High Blood Pressure Therapy Scale, namely reduced sodium use, appointment keeping and medication taking (Nkosi 2008:155). Table 3 outlines the results of the subscales in the Hill-Bone Compliance Scale.
An interesting result of the Hill-Bone Compliance Scale is the disparity in the answers depending on the way the question was structured. The questions and responses vary as follows:
When the question interrogated forgetting to take the medicine, nine out of every ten answered 'no'. When the question interrogated their decision not to take the medication, six out of every ten were willing to admit to such a decision. When the question interrogated supply, four out of every ten admitted to being without supplies at times. If the verb skip was used, for example 'skip your hypertension pills one to three days before you go to the clinic', three out of every ten participants admitted to it. Three questions were asked to investigate the influence of positive or negative emotions on the adherence to medication. Asking about adherence and feeling better or sick or caring less resulted in three out of ten participants admitting to non-compliance. When exploring whether they take someone else's hypertension pills, two out of ten participants admitted to this (Nkosi 2008:138).
The appointment keeping scale also shed some light on the dynamics of compliance to medication. Only 17.4% of the participants secured an appointment for the next visit, whilst 23% would leave without an appointment (Nkosi 2008:155).
The subscale investigating dietary intake of salty food also produced interesting results. When the question just focused on eating salty food, with no additional explanation, 4 out of every 10 would answer 'no', but when the question dealt with Aromat® or Fondor® (2 popular flavourants) only 2 to 3 out of every ten would say 'none of the time'. In addition, asking specifically about KFC® or MacDonald's® would cause 7 out of every 10 participants to say, 'Yes, that is part of my diet' (Nkosi 2008:138).
The evaluation of the participants' compliance (see Table 3) using the subscale and overall score provided evidence of non-compliance in terms of all three subscales. The worst compliance was with regard to sodium use: 33% good compliance and 44% low compliance (Nkosi 2008:138). Three out of 10 participants were not compliant in regularly taking medication, limited sodium use as well as keeping their appointments, which are all crucial in hypertension management and control.
Ethical consideration
Approval to conduct the study was obtained from the Ethics Committee of Tshwane University of Technology (#2006/07/007), the North West Department of Health and the management of the three primary healthcare clinics. Permission was granted by Becker et al. (2004) to conduct a similar study in Ga-Rankuwa. The principles of respect for persons, beneficence, justice and confidentiality were applied (Nkosi 2008:100-102).
Validity and reliability
The study was approved by the Faculty Research Committee of the Faculty of Health Science at the Tshwane University of Technology. A validated questionnaire (Becker et al. 2004: 63-69) was used to collect the data related to hypertension knowledge, habit and lifestyle changes, quality of life and care, life threats and clinical detail with personal medical history. Structured interviews ensured structural coherence through all the interviews. Face-to-face interviews were conducted, which allowed participants to ask for clarity even in their preferred language as the fieldworkers were fluent in the local languages (Nkosi 2008:107).
Theoretical framework
The Model for Health Promotion (Pender, Murdaugh & Parsons 2002:60) was used and it will guide the discussion.
Discussion
Based on the question asked, the results indicate a variation in compliance as most participants were non-compliant with their sodium use (33%) and follow-up appointments (57%) to collect medication, but more were compliant with taking the medication (81%). Non-compliance is common in individuals with asymptomatic conditions, for example those with hypertension may believe that they do not need take their medication regularly as they see no physical sign of being ill (Kagee & Le Roux 2007:444; Vlasnik et al. 2005:47-51,). The Health Promotion Model suggests that every person has their own unique personal experiences and characteristics that affect subsequent actions. The participants' actions of non-compliance can be attributed to their personal experiences or characteristics. Non-compliance to medication affects health promoting behaviour (compliance), which is the desired health promotion outcome. According to the theory of health promotion (Pender, Murdaugh & Parsons 2002:60), health professionals constitute a part of the interpersonal environment's interactive patterns which are essential in behaviour change, and have the responsibility to identify the factors that hinder compliance to treatment. Several factors affect compliance to medication and they need to be identified and addressed effectively by health professionals and clients (Van der Wal et al. 2006:434).
The Hill-Bone Compliance to High Blood Pressure Therapy Scale yielded different results depending on the questions that were asked using a dichotomous 'yes' or 'no' structure. Using various questions to determine compliance to medication therapy, the results clearly suggest non-compliance. When individuals were asked a question using the verb forgetting, 9 out of 10 answered 'no' but when the verb decide was used to determine compliance, 6 out of 10 admitted deciding not to take their medication sometimes. This indicates non-compliance to a plan of action of taking medication every day as prescribed and as required for effective management of hypertension. These findings are similar to those of Kripalani, Gatti and Jacobson (2010:180), who conducted a study in a primary healthcare clinic in Atlanta, Georgia. Amongst patients managed for coronary heart disease, the compliance varied when calculated from the prescription refill (43.4%) and when measured by self-report (50%) (Nkosi 2008:135). It is clear that to determine compliance, various methods should be used.
A study by Reiners and Nogueira (2009:1-8) discovered that despite health professionals' efforts to promote health, patients have their own way of managing their hypertension, for example they decide not to take treatment (Kagee & Le Roux 2007:453; Reiners & Nogueira 2009:1-8). The fact that patients manage their treatment their own way is not new in literature; patients adapt their treatment to their social habits. For the professional health worker to ensure compliance there is a need to understand the patient's immediate competing demands. This is confirmed by Pender, Murdaugh and Parsons (2002:60), who wrote that enquiring about clients' priorities, especially on the most crucial aspects of care that have high potential for low compliance, may be helpful in improving the quality of hypertensive patient care.
Using the various questions to determine compliance to medication therapy resulted in combined results (see Table 3) of the Hill-Bone Compliance Scale, indicating that 30% of the participants were not compliant to their prescribed medication (Nkosi 2008:138). Hypertension medication prevents the complications of hypertension, such as stroke. The Department of Health et al. (2007:217) emphasises the urgency of reminding clients to drink their pills even when they know they are coming for consultation at the clinics, it is the role of health professionals to interact with the client and identify non-compliance to be able to promote health and increase the client's well-being (Pender, Murdaugh & Parsons 2002:60).
Gascon et al. (2004:125) found that black people with hypertension are sensitive to sodium. In a study by Van der Wal et al. (2006:434-440), 13% (n = 25) of the participants reported that they had difficulties with their diet because the sodium-restricted diet was not palatable. Non-compliance to sodium usage is real and happening in patients with chronic diseases. According to Van der Wal et al. (2006:434), bland food due to low salt content does not taste good, which makes it difficult to adhere to a diet low in sodium.
To investigate compliance with low sodium usage, several questions were asked. When investigating eating salty food, four out of ten would say 'no', and concerning Aromat® or Fondor® 26.7% said 'no', they do not use it at all. However, regarding KFC® or MacDonald's® 7 out of 10 would say 'yes, that is part of my diet' (Nkosi 2008:135). Eating at a restaurant or having 'take-aways' was indicated to be a barrier to compliance with a low-sodium diet. Also, study participants in Schutte et al. (2003:339) reported a restriction to eat out at restaurants as a barrier to low-sodium compliance. In this study, compliance with low sodium usage was found to be low (see Table 3). The findings of this study indicate the importance of asking various questions to determine compliance if health promotion were to realise the objective of changing individuals' behaviour and increasing clients' well-being.
Limitations of the study
The results of the study cannot be generalised due to the convenience sample used in the study. Self-reporting, which was used as method of data collection, is subject to recall and social desirability bias. The instrument used did not offer a chance to gain deeper understanding because open-ended questions were not used.
Recommendations
The content and method of health education related to medication, diet and follow-up consultations should be investigated and improved. A hypertension health literacy evaluation tool should be developed to assess the effectiveness of the hypertension health education provided. Health professionals need to be familiarised with different methods that can be used to investigate compliance with hypertension management. A qualitative study using open-ended questions should be undertaken to shed more light on this health problem.
Conclusion
To improve the quality of life of hypertensive clients, hypertension as a life threatening condition needs to be managed and controlled well. This can be achieved through compliance and lifestyle adaptation by hypertensive individuals.
Acknowledgements
We acknowledge Becker et al. (2004) for granting us the opportunity to use their questionnaire, as well as the hypertensive clients and healthcare professionals in those three primary healthcare clinics, without whom this study would not have been possible.
Competing interests
The authors declare that they have no financial or personal relationship(s) which may have inappropriately influenced them in writing this article.
Authors' contributions
N.G.M. (Tshwane University of Technology) and S.C.D.W. (Tshwane University of Technology) made equal contributions to the article.
References
Babbie, E. & Mouton, J., 2004, The practice of social research, Oxford University Press, Cape Town. [ Links ]
Becker, H., Bester, M., Reyneke, N., Labadarios, D., Monyeki, K. & Steyn, N.P., 2004, 'Nutrition related knowledge and practices of hypertensive adults attending hypertensive clinics at day hospitals in the Cape Metropole', Curationis 27(2), 63-69. http://dx.doi.org/10.4102/curationis.v27i2.988, PMid:15974021 [ Links ]
Charlton, K.E., Steyn, K. & Levitt, D., 2007, Dietary intervention lowers blood pressure in South Africans with hypertension, viewed 17 July 2010, from http://www.mrc.ac.za/policybrief/saltpolicy.pdf [ Links ]
Department of Health, 2003, South African standard treatment guidelines and essential drug list for primary health care, 3rd edn, Department of Health, Pretoria. [ Links ]
Department of Health, Medical Research Council & OrcMacro, 2007, South Africa Demographic and Health Survey 2003, Department of Health, Pretoria, viewed 10 April 2011, from http://www.mrc.ac.za. [ Links ]
Frishman, W.H., 2007, Importance of medication adherence in cardiovascular disease and the value of once daily treatment regimens, Cardiology in Review 15(5), 257-263. [ Links ]
Halpern, M.T., Khan, Z.M., Schmier, J.K., Burnier, M., Caro, J.J., Cramer, J. et al. 2006, 'Recommendations for evaluating compliance and persistence with hypertension therapy using retrospectiv e data', American Heart Association 46, 1039-1948. [ Links ]
Kagee, A. & Le Roux, M., 2007, 'Treatment adherence among primary care patients in a historically disadvantaged community in South Africa: A qualitative study', Journal of Health Psychology 12(3), 444-460. http://dx.doi.org/10.1177/1359105307076232, PMid:17439995 [ Links ]
Kim, M.T., Hill, M.N., Bone, L.R. & Levine, D.M., 2000, 'Development and testing of the Hill-Bone compliance to high blood pressure therapy scale', Progress in Cardiovascular Nursing 15(3), 90-96. http://dx.doi.org/10.1111/j.1751-7117.2000.tb00211.x, PMid:10951950 [ Links ]
Kripalani, S., Gatti, M.E. & Jacobson, T.A., 2010, 'Association of age, health literacy and medication management strategies with cardiovascular medication adherence', Patient Education and Counselling 81, 177-181. http://dx.doi.org/10.1016/j.pec.2010.04.030, PMid:20684870 [ Links ]
Nkosi, N.G., 2008, 'Management practices and nutrition related knowledge of hypertensive adults in Ga-Rankuwa', Master's thesis, Deptartment of Nursing Science, Tshwane University of Technology, Pretoria. [ Links ]
Nunes, V., Neilson, J., O'Flynn, N., Calvert, N., Kuntze, S., Smithson, H. et al., 2009, 'Medicines adherence: Involving patients in decisions about prescribed medicines and supporting adherence', National Collaborating Centre for Primary Care and Royal College of General Practitioners, London, viewed July 2013, from http://www.sefap.it/servizi_lineeguida_200902/CG76FullGuidelineApp.pdf. [ Links ]
Maepe, L.M. & Outhoff, K., 2012, 'Hypertension in gold miners', South African Medical Journal 102(1), 30-33. [ Links ]
Patel, U.D. & Davis, M.M., 2006, 'Physicians' attitudes and practices regarding adherence to medical regimens by patients with chronic illnesses', Clinical Paediatrics 45(5), 439-495. http://dx.doi.org/10.1177/0009922806289619, PMid:16891277 [ Links ]
Pender, N., Murdaugh, C. & Parsons, A., 2002, Health promotion in nursing practice, Prentice Hall, Upper Saddle River. [ Links ]
Reiners, A.A.O. & Nogueira, M.S., 2009, 'Raising hypertensive patients' consciousness about treatment compliance', Revista Latino-Americana de Enfermagem 17(1), 1-8. http://dx.doi.org/10.1590/S0104-11692009000100010 [ Links ]
Schutte, A.E., Van Rooyen, J.M., Huisman, H.W., Kruger, H.S. & De Ridder, J.H., 2003, 'Factors analysis of possible risk for hypertension in a black South African population', Journal of Human Hypertension 17, 339-348. http://dx.doi.org/10.1038/sj.jhh.1001553, PMid:12756407 [ Links ]
Seedat, Y.K. & Rayner, B.L., 'South African hypertension guideline 2011', South African Medical Journal 102(1), 60-83. [ Links ]
Statistics South Africa, 2001, Extract from the Report of the Census Sub-Committee to the South African Statistics Council on Census 2001, viewed on 18 March 2006, from: http://www.statssa.gov.za/extract.html [ Links ]
Thrall, G., Lip, G. & Lane, D., 2004, 'Compliance with pharmacological therapy in hypertension: Can we do better, and how?', Journal of Human Hypertension 18, 594-597. http://dx.doi.org/10.1038/sj.jhh.1001722, PMid:15029219 [ Links ]
Van der Wal, M.H.L., Jaarsma, T., Morse, D.K., Veeger, N.J.G.M., Van Gilst, W.H. & Van Veldhuisen, D.J., 2006, 'Compliance in heart failure patients: The importance of knowledge and beliefs', European Heart Journal 27, 434-440. http://dx.doi.org/10.1093/eurheartj/ehi603, PMid:16230302 [ Links ]
Vlasnik, J.J., Aliotta, S.L., De Lor, B., 2005, 'Medication adherence: Factors influencing compliance with prescribed medication plans', Case Manager 16, 47-51. http://dx.doi.org/10.1016/j.casemgr.2005.01.009, PMid:15818344 [ Links ]
 Correspondence:
Correspondence:
Gloria Mafutha
Postnet Suite 49
Private Bag x927
Pretoria 0001, South Africa
Email: mafuthng@tut.ac.za
Received: 29 Aug. 2011
Accepted: 23 July 2013
Published: 06 Sept. 2013














