Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Psychiatry
versão On-line ISSN 2078-6786
versão impressa ISSN 1608-9685
S. Afr. j. psyc. vol.28 no.1 Pretoria 2022
http://dx.doi.org/10.4102/sajpsychiatry.v28i0.1661
ORIGINAL RESEARCH
Community mental health literacy in Tshwane region 1: A quantitative study
Dumisile MadlalaI; Pierre M. JoubertII; Andries MasengeIII
IDepartment of Health, Faculty of Health Sciences, Tshwane Mental Health District Services, Tshwane, South Africa
IIDepartment of Psychiatry, Faculty of Health Science, University of Pretoria, Pretoria, South Africa
IIIDepartment of Statistics, Natural and Agricultural Science, University of Pretoria, Pretoria, South Africa
ABSTRACT
BACKGROUND: Although mental health literacy is a major determining factor of mental health outcomes and functional capacity of individuals, there is dearth of research on the issue in South Africa
AIM: To assess the literacy of three mental disorders, namely major depressive disorder (MDD), schizophrenia and generalised anxiety disorder (GAD) and to compare the resultant assumed literacy level between urban and townships participants
SETTING: Five clinics of region 1 in Tshwane, South Africa
METHOD: A cross-sectional descriptive study was performed between November 2019 and January 2020. A total of 385 questionnaires were distributed equally in all five clinics. By means of questions about three fictive cases with clinical pictures indicative of MDD, schizophrenia and GAD the following were assessed: recognising a mental disorder, identifying the cause and knowledge about what would help best
RESULTS: The majority of participants (67.3%) recognised the clinical picture indicative of schizophrenia as a mental disorder, almost half of the participants (49.9%) recognised the clinical picture indicative of MDD as a mental disorder, whilst just more than one third (36.3%) of participants recognised the clinical picture GAD as a mental disorder. Concerning the causes for the clinical pictures, most participants indicated that stress was the cause for MDD and GAD (77.4% and 68.1%, respectively), whilst indicating that biological or psychological (59.5%) causes are relevant to the clinical picture indicative of schizophrenia symptoms. Fewer participants indicated supernatural causes for any of the clinical case (MDD: 2.6%; schizophrenia 15.3%; GAD 4.2%). Most participants chose professional help as the best option for all three cases (MDD 81.3%, schizophrenia 82.2%, GAD 66.1%). The indicators for health literacy in this study show that urban participants had better knowledge than township participants across all questions about the cases
CONCLUSION: Overall, the study indicated a variable knowledge regarding the three mental disorders in region 1 of Tshwane and variable literacy levels in townships compared with urban settings. The results indicate that awareness campaigns should focus on the deficient areas
Keywords: community; mental health literacy; mental health; depression; schizophrenia; GAD.
Introduction
Mental health is more than just lack of a mental illness. It is defined as mental functioning that enables one to recognise one's abilities, cope with the normal stresses of life, work productively and make a positive contribution to one's community.1 Mental health literacy is defined as knowledge and beliefs about mental disorders that aid in the recognition, management and prevention of mental disorders.2 It includes seven components: (1) the ability to recognise specific disorders, (2) knowing how to seek mental health-related information, (3) knowledge on causes, (4) knowledge of risks factors for mental disorders, (5) knowledge on self-treatments available, (6) knowledge on professional help available and (7) attitudes that promote recognition and appropriate help seeking.2 Lack of knowledge in the different aspects of mental health literacy has a major impact in the total outcome of mental health status of individuals and their communities.3 Patients' responses are motivated not only by the availability of services but also by their knowledge about the services and how to access the services.4 The ability to recognise specific disorders and knowledge on how to seek mental health information prompt early help-seeking behaviours and early attendance with a relevant mental health team.5 This in turn promotes the early identification of mental disorders and the treatment thereof, which in turn promotes the mental health of that particular community.
As there is a correlation between mental health literacy and mental health outcomes,4,5 it is not surprising that this construct has been a subject of extensive research in many countries.
Studies have shown variable outcomes depending on the region researched. For example, Australian surveys indicate a steady improvement of mental health literacy over the years,6,7 while studies in some parts of Europe and Asia found lower levels of literacy than those of Australia.8,9,10,11,12,13
African studies revealed poor mental health literacy regarding the recognition, causes and professional treatment of mental disorders and consequently, negative attitudes towards mentally ill individuals.14 Studies in Ethiopia and Nigeria,15,16 for example, determined that respondents could only identify overt psychotic symptoms as signs of mental disorders. This means that common psychiatric disorders such as depressive disorders and anxiety disorders were not recognised. Furthermore, mental disorders were mainly attributed to supernatural causes rather than biological causes.17
South Africa is a middle-income country in Africa with an estimated population of 57 million.18 The country is fraught with many societal problems posing risk factors for mental disorders (e.g. violence and racial discrimination).19 Nonetheless, little has been published on mental health literacy in South Africa. The available studies indicate a lack of mental health literacy. One study reports that respondents mostly attributed the symptoms of mental disorders to stress, while ignoring biogenetic factors.20 A study involving families with relatives suffering from schizophrenia, reports that mental illness was often attributed to supernatural causes such as bewitchment.21 Furthermore, South African studies also indicate high prevalence rates of stigmatising mental disorders.22,23,24 Regarding stigma, Kakuma et al.25 reported on awareness campaigns to improve mental health literacy, but the impact of such campaigns remain unclear. Reports on the state of mental health systems in South Africa indicate the following: variation in service provision between the different provinces,26 treatment gaps, about 70% of mentally ill people do not receive treatment,27 a limited scope of decentralised community-based care,28 poor mental health policy implementation,28 a lack of uniform indicators for mental health information systems,28 a lack of involvement of mental healthcare users in mental health policy development.28
Considering all these facts, one questions how much South Africans know about mental disorders. Consequently, this study aimed to describe the mental health literacy of three common psychiatric disorders, namely generalised anxiety disorder, schizophrenia and major depressive disorder (MDD) in a region in South Africa. According to the South African health and stress study (SASH), anxiety disorders were found to be the most common with a prevalence of 13%. Mood disorders were found to have a prevalence of 9%.27 The prevalence of schizophrenia, a psychotic disorder, was not assessed in the SASH study but has a prevalence of about 1% worldwide.29
Methods
The study was performed in region 1 of Tshwane, in the Gauteng province of South Africa. Gauteng is one of nine provinces in South Africa. Tshwane is one of five metropolitan municipalities in Gauteng province. Tshwane is divided into seven demographic regions, namely Regions 1-7. Tshwane has about 2.2 million people, with region 1 having about 811 570 people.30
Tshwane has 61 clinics that serve about 250 people daily in each clinic. This study was performed in five of these clinics, namely Tlamelong Clinic, Kgabo Clinic, Phedesong 4 Clinic, Soshanguve Clinic 3 and Pretoria North Clinic. The latter is the only urban clinic. The others are township clinics. The clinics were randomly selected.
Study design and sampling
This quantitative, cross-sectional, descriptive study was carried out between November 2019 and January 2020. A total of 385 participants were recruited by convenience sampling. This amounted to 77 participants per clinic.
The sample size was informed by statistics: A sample of at least 384 is needed for a 95% confidence and 5% margin of error for a population of more than 1 000 000.31 The inclusion criteria to participate were: men or women from all race and ethnic groups aged 18 years and older and exclusion criteria were: people under 18 years of age and people unable to read or write.
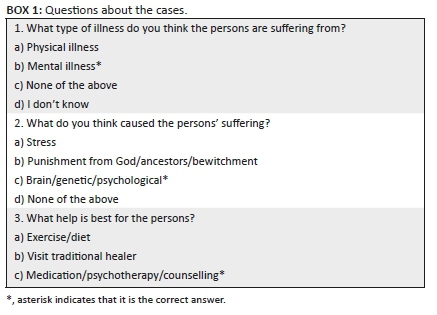
Service users waiting to see health practitioners, as well as their accompanying family members were approached to take part in the study and briefed about it. This was done in English, isiZulu or Setswana, as needed, by the first researcher, who can speak all three languages. The fictive cases, questions about the cases (see Box 1), were also translated into isiZulu and Setswana. In the experience of the first researcher, these three languages are commonly used in the clinics where the study was performed. Participants signed the consent form and after that were given the research cases (Appendix 1) and questionnaire.
The questionnaire
The questionnaire was divided into two sections, namely sections A and B. Section A contained the demographic data and section B contained the questions to assess the mental health literacy. In order to assess mental health literacy, respondents were presented with three case studies that, respectively, meet the DSM-529 criteria for MDD ('Betty'), schizophrenia ('Muzzy') and generalised anxiety disorder ('Lucy'). These disorders were selected because anxiety and mood disorders are common in South Africa.27
Although the global prevalence of schizophrenia is less, it is nonetheless relatively common.29 Although this is the case, symptoms of schizophrenia seem to be more likely to be identified as belonging to a mental disorder, especially in African countries.14,15 Hence, schizophrenia was included.
This study asked participants to choose one answer amongst various options for three questions about the fictive cases: (1) What type of illness do you think the persons are suffering from? (2) What do you think caused the persons' suffering? (3) What help is best for the persons? (See Box 1: Questions about the Cases and Appendix 1). Thus, three specific aspects of mental health literacy were targeted, based on the work of Jorm et al.2 Like the fictive cases, the questions were also translated in Setswana and isiZulu.
Ethical considerations
The study was approved by the Tshwane District Research Committee and Research Ethics Committee of the Faculty of Health Sciences, University of Pretoria. Ethics Reference No.: 543/2019.
Statistical analysis
Frequency tables (counts and percentages) were performed for demographic variables (gender, employment status, marital status and level of education) and participants chosen answer for the type of problem, cause of the problem and best help for the problem. Cross tabulation was performed between the township clinics and the urban clinic where participants were enrolled and evaluated. Finally, the z test of proportion was conducted to test if the clinics' participants differed proportionally in their response. The statistical significance was set at p < 0.05.
Results
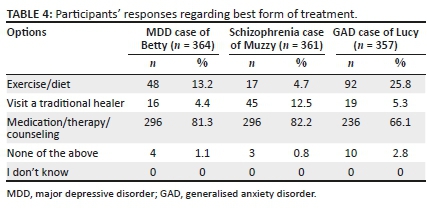
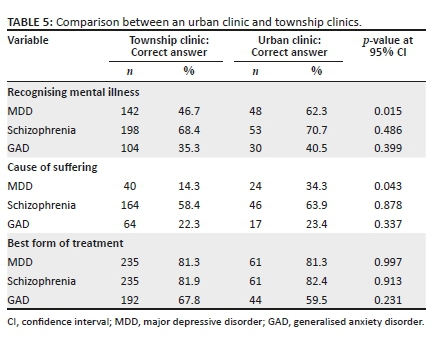
The demographic results are displayed in Table 1. A total of 77 questionnaires were distributed in each of the five clinics. The sum total of all questionnaires for all the clinics was 385. Each of the respondents was required to give responses to all three cases, namely depression, schizophrenia and generalised anxiety disorder (GAD). The descriptive statistical results obtained from participants' chosen answers are displayed in Tables 2-4. From these tables it is evident that not all participants responded to all cases and all questions about the cases. The descriptive statistics comparing urban and rural outcomes are displayed in Table 5.
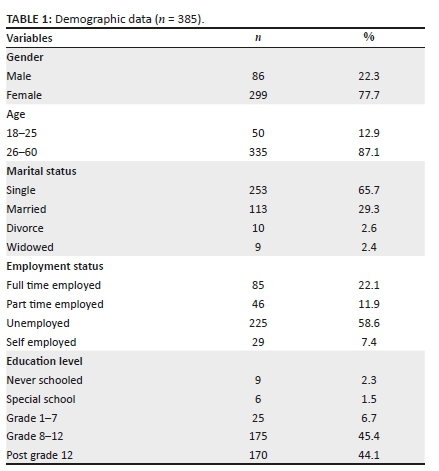
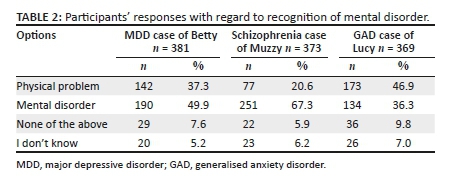
On recognising a mental disorder
See Table 2 for the results of participants' chosen answers to questions regarding the ability to identify a mental disorder. In all cases the correct choice is mental illness. Out of 381 participants who responded, the chosen answer for the case about MDD was a physical illness by 142 (37.3%), a mental illness by 190 (49.9%), neither a physical nor a mental illness by 29 (7.6%), while 20 (5.2%) did not know. Out of 373 participants who responded, the chosen answer for the case about schizophrenia was a physical illness by 77 (20.6%), a mental illness by 251 (67.3%), neither physical nor mental illness by 22 (5.9%), while 23 (6.2%) did not know. Out of 369 participants who responded, the chosen answer for the case of GAD was a physical illness by 173 (46.9%), a mental illness by 134 (36.3%), neither a physical nor a mental illness by 36 (9.8%), while 26 (7.0%) did not know.
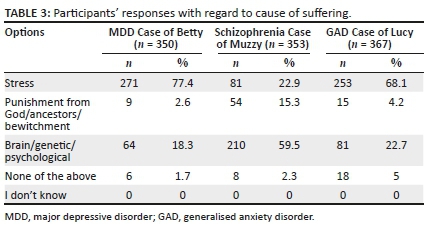
On the cause of suffering
See Table 3 for the results of participants' chosen answers to the question regarding the ability to identify the cause of the suffering in the cases. In all cases the correct choice is either brain or genetic or psychological. Out of 350 participants who responded, the chosen answer about the cause of suffering in the case about MDD was stress by 271 (77.4%), punishment from God, ancestors or bewitchment by 9 (2.6%), brain, genetic or psychological by 64 (18.3%), none of the given options by 6 (1.7%), while no one chose, 'I don't know'. Out of 353 participants who responded, the chosen answer for the cause of suffering in the case about schizophrenia was stress by 81 (22.9%), punishment from God, ancestors or bewitchment by 54 (15.3%), brain, genetic or psychological by 210 (59.5%), none of the given options by 8 (2.3%), while no one chose, 'I don't know'. Out of 367 participants who responded, the chosen answer about the cause of suffering in the case about GAD was 'stress' by 253 (68.1%), 'punishment from God/ancestors/bewitchment' by 15 (4.2%), 'brain/genetic/psychological' by 81 (22.7%), none of the given options by 18 (5%), while no one chose, 'I don't know'.
On the best form of treatment
Out of 364 participants who responded (see Table 4), the chosen answer for the best form of treatment in the case about MDD was exercise/diet by 48 (13.2%), a visit to a traditional healer by 16 (4.4%), medication/therapy by 296 (81.3%), none of the options by 4 (1.1%), whilst no one chose, 'I don't know'. Out of 361 participants who responded, the chosen answer for the best form of treatment in the case about schizophrenia was 'exercise/diet' by 17 (4.7%), 'a visit to a traditional healer' by 45 (12.5%), 'medication/therapy' by 296 (82.2%), none of the options by 3 (0.8%), whilst no one chose, 'I don't know'. Out of 357 participants who responded, the chosen answer for the best form of treatment in the case about GAD was 'exercise/diet' by 92 (25.8%), a visit to a traditional healer by 19 (5.3%), 'medication/therapy' by 236 (66.1%), none of the options by 10 (2.8%), whilst no one chose, 'I don't know'.
On comparing the results between an urban clinic and township clinics
Referring to Table 5, here follow the comparisons between the descriptive statistics of township and an urban clinic regarding the correct chosen answers for the different case-related questions. Firstly, correctly choosing 'mental illness' as answers to the question about the kind of illness the fictive cases portrayed; for township clinics versus urban clinic: MDD, 142 (46.7%):48 (62.3%) (p = 0.015 at 95% CI [confidence interval]); schizophrenia, 198 (68.4%): 53 (70.7%) (p = 0.486 at 95% CI); GAD, 104 (35.3):30 (40.5%) (p = 0.399 at 95% CI). Secondly, correctly choosing 'brain/genetic/psychological' as answer to the question about the cause of suffering; township clinics versus urban clinic: MDD, 40 (14.3%):24 (34.3%) (p = 0.043 at 95% CI); schizophrenia, 164 (58.4%):46 (63.9%) (p = 0.878 at 95% CI); GAD, 64 (22.3%):17 (23.4%) (p = 0.337 at 95% CI). Thirdly, correctly choosing 'medication/psychotherapy/counselling' as the answer to the question about the best form of treatment; township clinics versus urban clinic: MDD, 235 (81.3%):61 (81.3%) (p = 0.997 at 95% CI); schizophrenia, 235 (81.9%):61 (82.4%) (p = 0.913 at 95% CI); GAD, 192 (67.8%):44 (59.5%) (p = 0.231 at 95% CI). Thus, there are only two parameters where there is a significant difference between the urban clinic and township clinics regarding the correct choice of answer: Choosing MDD as a mental illness and choosing the cause of suffering to be 'brain/genetic/psychological'; in both cases the urban clinic did better.
Discussion
This study investigated the mental health literacy of participants from clinics in region 1 of the Tshwane District. Mental health literacy was assessed by using Jorm's2 definition, namely recognition of a mental illness, knowledge of causation and knowledge of the best help available. Participants were requested to complete a questionnaire after having read three fictive cases that, respectively, indicated MDD, schizophrenia and GAD. Based on the answers chosen by about half of the participants, the mental illness, MDD, was readily recognised as a mental illness after reading the fictive case. Participants from the urban clinic chose mental illness significantly more frequently than those from the township clinics. That being so, the overall results are encouraging, because recognising mental illness is associated with appropriate help seeking.31,32,33,34 Nonetheless, about half of all the participants did not recognise the mental illness. The latter group included those who chose physical illness as the answer (more than one third) or (much fewer) neither a mental nor physical illness, or chose that they did not know. Two implications are immediately apparent: (1) clinicians should be aware that MDD (perhaps especially in township areas) may present as a physical illness (2) more community-based psychoeducation is needed.
For the MDD case, only a minority (18.3%) chose the correct answer to the question about the cause of suffering, namely 'brain/genetic/psychological', whilst an overwhelming majority (77.4%) chose 'stress'. Since so many participants chose physical illness as the explanation for the symptoms of the MDD case, one wonders whether participants might have considered stress as a cause of physical illness (and mental illness), which would not be incorrect. Nonetheless, urban participants did significantly better than the township participants and this finding is consistent with other studies.35,36,37 It also indicates that people consider stress to be the cause of MDD and GAD.38,39,40 Identifying stress as the cause, is associated with seeking lay help rather than professional help.39 Unfortunately, a very small portion (2.6%), chose 'punishment from God/ancestor/bewitchment'. This finding also supports continued community-based psychoeducation.
When it comes to the best treatment, the overwhelming majority chose 'medication/therapy'. As most participants chose either mental illness or physical illness and since for both the choice 'medication/therapy' would be the correct choice, the outcome is to be expected. For this last question, urban and township participants faired equally well, perhaps further indicating that 'medication/therapy' was chosen for mental and physical illnesses. Thus, this answer too needs revision for future use, so as to clearly distinguish between the management of mental and physical illness. A sizable minority (13.2%) choose 'diet/exercise' and, much fewer, traditional healing as the best treatment option. Taken together, the findings about the MDD case calls for more community-based education.
Whilst about half of participants recognised the MDD case as a mental illness, most (67.3%) recognised the schizophrenia case a mental illness. with little difference between urban and township participants. Participants in this study did better than in a previous study.21
Nonetheless, a sizable portion (20.6%) chose physical illness, with much fewer choosing the case being neither a mental nor physical illness (5.9%) or that they don't know (6.2%). The findings are in line with previous studies indicating that schizophrenia is more readily recognisable as a mental illness than MDD,24,41,42 and, by extension, GAD (which will be discussed here). Thus, it seems less likely that people will confuse schizophrenia with a physical illness and thus, seek appropriate help. It is possible that community-based education and lay publications give more attention to schizophrenia than MDD and GAD. However, it is also possible that the dramatic nature of psychotic symptoms readily alert community members to a mental illness.
Contrary to the MDD case (and the following GAD case) most participants (59.5%) chose the correct answer about the cause of suffering, with urban participants doing somewhat better. It is possible that most participants considered 'brain/genetic/psychological' to be the (obvious) cause, thereby simply excluding 'stress' from the picture, but yet, a sizable minority (22.9%) chose 'stress'. A sizable minority (15.3%) also chose 'punishment from God/ancestor/bewitchment' as the cause of suffering is worrying. This answer was chosen with greater frequency than for the MDD (2.6%) and GAD (4.2%) cases. Despite that, fewer participants in this study chose the supernatural as cause for MDD and GAD43 and schizophrenia44 than in other studies. The implications are that, although schizophrenia is readily recognised as mental disorder, a sizable minority may consider the cause of suffering to be supernatural. That in turn may have an effect on seeking appropriate help and the way a psychotically ill person is viewed and handled by the community, for example, searching out spiritualists and traditional healers.38,39,40 The need for community-based psychoeducation is again indicated.
Whilst participants recognised mental illness regarding the MDD and schizophrenia cases, they had, by inference, difficulty doing so for GAD: physical illness (46.9%) was more frequently chosen than mental illness (36.3%), whilst a few chose neither (9.8%) or did not know (7.0%).
Participants from both urban and township clinics did poorly with GAD. Possible reasons for this are lack of community-based education, fears (if one should recognise oneself in the case) of being seen as weak or stigmatisation.33 This outcome may indicate that few people with GAD will seek appropriate help.
Participants mostly chose stress as the cause of suffering (68.1%), with a sizable minority choosing 'brain/genetic/psychological' (22.7%) and a smaller minority (5.0%) choosing neither. As for MDD and schizophrenia, participants again chose 'medication/therapy' as best treatment. However, many participants (25.8%) chose 'exercise/diet' as the best treatment, more frequently than for MDD and schizophrenia, perhaps reflecting the perceptions of stress as the cause. Like for MDD, this may be because many chose the GAD case to reflect physical illness, and thus, medication would be a logical treatment choice.
Limitations
The study used only three mental illnesses, targeted very specific aspects of mental health literacy and sourced participants from very specific areas in Gauteng. Furthermore, doing the study at clinics may have selected participants with biases that may be different from people who never use or need to use medical clinics. Thus, the outcomes of the study should not readily be generalised. Nonetheless, the study gives a glimpse into a poorly researched area. In retrospect it is possible that at least some participants found the difference between the options, 'stress' and 'brain/genetic/psychological' confusing because stress and psychological are closely related. As pointed out here, medication would be the treatment choice for both mental illness and physical illness. Consequently, the study cannot claim that when participants chose the treatment option, 'medication', it was for a mental illness. The study mostly used descriptive statistics, rather than analyses of significance when comparing outcomes related to the three mental illnesses. Nonetheless, at face value, the descriptive statistics are informative.
Conclusion
Participants in this study correctly recognised and identified causation and the best treatment for schizophrenia, followed by MDD, and then GAD. Participants from an urban area did somewhat better than those from township areas. The study indicates that, especially for MDD and GAD, mental illness is confused with physical illness. Furthermore, a minority attributed clinical features of a mental illness as punishment from God. Altogether, there is a reason to be optimistic and concerned.
Acknowledgements
The authors acknowledge the Tshwane district mental health team including the office of the director and the deputy director, the region mental health coordinators who assisted in the identifications of the clinics where the research was conducted, all the clinic managers who allowed for the research to be conducted at their clinics and all the participants.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
D.M. was responsible for inception of ideas regarding the research, methodology, investigations, visualisation, administration, resources, writing, review and editing. P.J. was involved in methodology, conceptualisation, writing-review and editing, supervision. A.M. was responsible for software, formal analysis and writing.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
All data that support the findings of this study are available online.
Disclaimer
Views and opinions expressed in the article are those of the authors and do not reflect the official policy or position of any affiliated agency of the authors.
References
1.World Health Organization. Investing in mental health. Geneva: World Health Organization; 2003. [ Links ]
2.Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollit P. Mental health literacy: A survey of the public's ability to recognise mental disorders and their beliefs about effectiveness of treatment. MJA, 1997;166(4):182-186. https://doi.org/10.5694/j.1326-5377.1997.tb140071.x [ Links ]
3.Coles ME, Ravid A, Gibb B, et al. Adolescent mental health literacy: Young people's knowledge of depression and social anxiety disorder. J Adolesc Health. 2016;58:57-62. https://doi.org/10.1016/j.jadohealth.2015.09.017 [ Links ]
4.Rusch N, Evans-Lacko S, Henderson C, Flach C, Thornicroft G. Knowledge and attitudes as predictors of intentions to seek help for and disclose mental illness. Psychiatr Serv. 2011;62(6):675-678. https://doi.org/10.1176/ps.62.6.pss6206_0675 [ Links ]
5.Henderson C, Evans-lacko S, Thornicroft G. Mental illness stigma, help seeking, and public help programmes. Am J Public Health. 2013;103(5):777-780. https://doi.org/10.2105/AJPH.2012.301056 [ Links ]
6.Jorm AF, Christensen H, Griffiths MK. The public's ability to recognize mental disorders and their beliefs about treatment: Changes in Australia over 8 years. Australian New Zealand J Psychiatr. 2006;40(1):36-41. https://doi.org/10.1080/j.1440-1614.2006.01738.x [ Links ]
7.Raevely N J, Too T, Zhao MJ. National survey of mental health literacy and stigma. A report for mental Health Commission of NSW. Sydney: Mental Health Commission of NSW; 2015. [ Links ]
8.Melas PA, Tartani E, Forsner T, Forsell Y. Mental literacy about depression and schizophrenia among adolescent in Sweden. Eur Psychiatr. 2013;28(7):404-411. https://doi.org/10.1016/j.eurpsy.2013.02.002 [ Links ]
9.Waldman T, Stagier T, Oexle N, Rusch N. Mental health literacy and help seeking among the unemployed people with mental health problems. J Mental Health. 2019;29(3):270-276. https://doi.org/10.1080/09638237.2019.1581342 [ Links ]
10.Loureiro L, Jorm F, Padreiro A, et al. Mental health literacy about depression: A survey of Portuguese youth. BMC Psychiatr. 2013;13:129-138. https://doi.org/10.1186/1471-244X-13-129 [ Links ]
11.Wong FKD, Xuesong H, Poon A, et al. Depression literacy among the Chinese in Shanghai, China: A comparison with Chinese speaking Australians in Melbourne and Chinese in Hong Kong. Social Psychiatr Psychiatr Epidemiol. 2012;47(8):1235-1242. https://doi.org/10.1007/s00127-011-0430-4 [ Links ]
12.Kermode M, Bowen K, Arole S, et al. Community beliefs and treatments and outcomes of mental disorders: A mental health literacy survey in a rural area of Maharashtra, India. Public Health. 2009;123(7):476-483. https://doi.org/10.1016/j.puhe.2009.06.004 [ Links ]
13.Okumura Y, Sakomoto S. depression treatment among Japanese undergraduate using conjoint analysis. Int J Soc Psychiatr 2012;58(2):195-203. https://doi.org/10.1177/0020764010390437 [ Links ]
14.Atiola O. Level of community mental health literacy in sub Saharan Africa: Current studies are limited in number, scope, spread and cognizance of cultural nuances. Nord J Psychiatr. 2015;69(2):93-101. https://doi.org/10.3109/08039488.2014.947319 [ Links ]
15.Deribew A, Yonas S. How mental problems are perceived by a community in Agaro town. Ethiop J Health Dev. 2005;19(2):153-159. https://doi.org/10.4314/ejhd.v19i2.9985 [ Links ]
16.Kabir M, Iliyasu Z, Abubakar S, et al. Perception and beliefs about mental illness among adults in Karfi village, northern Nigeria. BMC Int Health Human Rights. 2004;4:3. https://doi.org/10.1186/1472-698X-4-3 [ Links ]
17.Mubbshar MH, Farooq S. Mental health literacy in developing countries. Br J Psychiatr. 2001;179(1):75. https://doi.org/10.1192/bjp.179.1.75-a [ Links ]
18.Statistic South Africa. Mid-year population estimates. Pretoria: StatsSA; 2018. [ Links ]
19.Van der Westhuizen M, Swart I. The struggle against poverty, unemployment and social injustice in the present-day South Africa: Exploring of the ditch reformed Church at congregational level. Stellenbosch Theol J. 2015(1):731-759. https://doi.org/10.17570/stj.2015.v1n2.a35 [ Links ]
20.Hugo CJ, Boshoff EL, Traut A, et al. Community attitudes towards knowledge of mental illness in South Africa. Socio Psychiatr Epidemol. 2003;38(12):715-719. https://doi.org/10.1007/s00127-003-0695-3 [ Links ]
21.Mbanga NI, Niehaus DJ, Mzamo NC, et al. Attitudes towards and beliefs about schizophrenia in Xhosa families with affected probands. Curationis. 2002;25(1):a718. https://doi.org/10.4102/curationis.v25i1.718 [ Links ]
22.Egbe C, Brooke-Summer C, Kathree T. Psychiatric stigma and discrimination in South Africa: A perspective from key stakeholders. BMC Psychiatr. 2014;14:191-212. https://doi.org/10.1186/1471-244X-14-191 [ Links ]
23.Hugo CJ, Matelo-Liquito J, Stein DJ. A critical look at stigma and its impact in psychiatry. 12th National psychiatry congress of the South African Society of Psychiatrists, Somerset West. Sept. 2002. [ Links ]
24.Sorsdahl K, Stein DJ. Knowledge of and stigma associated with mental disorders in a South African community sample. J Nerv Ment Dis. 2010;198(10):742-747. https://doi.org/10.1097/NMD.0b013e3181f4b2d7 [ Links ]
25.Kakuma R, Kleintjies S, Lund C, et al. Mental health stigma: What is being done to raise awareness to reduce stigma in South Africa. Afr J Psychiatr. 2010;13(2):116-124. https://doi.org/10.4314/ajpsy.v13i2.54357 [ Links ]
26.WHO. AIMS report on mental health systems in South Africa. Cape Town: WHO; 2007. [ Links ]
27.Herman A, Stein DJ, Williams DR. The South African stress and health study: 12 month and life time prevalence of common mental disorders. Afr Med J. 2009;99(2):339-344. [ Links ]
28.Department of Health Republic of South Africa. National mental health policy framework and strategic plan. Cape town: Department of Health; 2013. [ Links ]
29.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: APA; 2013. [ Links ]
30.Tshwane. Department of Health Republic of South Africa. Gauteng Tshwane district profile. Tshwane: Department of Healthcity; 2011. [ Links ]
31.Firky A, Mohamed practises in sample size determination and variance estimation-implications on data analysis. Proceeding of regional conference on statistical science 2010; p. 147-162. [ Links ]
32.Amarasuya S, Jorm F, Reavley N. Depression literacy of undergraduates in a non-western developing context: The case of Sri Lanka. BMC. 2015;8:593. https://doi.org/10.1186/s13104-015-1589-7 [ Links ]
33.Bonabi H, Muller M, Ajdac-Gross V, et al. Mental health literacy, Attitudes to help seeking, and perceived need as predictors of mental health Service use: A longitudinal study. J Nerv Ment Dis. 2016;204(4):321-324. https://doi.org/10.1097/NMD.0000000000000488 [ Links ]
34.Ibrahim N, Amit N, Shahar S. Do depression literacy, mental illness beliefs and stigma influence mental health help seeking attitude? A cross sectional study of secondary school and university students from B40 household in Malaysia. BMC Public Health. 2019;19:544. https://doi.org/10.1186/s12889-019-6862-6 [ Links ]
35.Ghadirian L, Sarayifard A. Depression literacy in urban and suburban Residents of Tehran, The capital of Iran; recognition, help seeking and stigmatizing attitude and Predicting factors. Int J Med. 2019;10:134. https://doi.org/10.4103/ijpvm.IJPVM_166_18 [ Links ]
36.Yu Y, Ziwei L, Mi H, et al. Assessment of mental health literacy using a multifaceted measure among Chinese rural population. BMJ Open. 2015;5(10):e009054. https://doi.org/10.1136/bmjopen-2015-009054 [ Links ]
37.Swami V, Loo P, Furnham A. Public knowledge and beliefs about depression among urban and rural Malays in Malaysia. J Soc Psychiatr. 2010;56(5):480-496. https://doi.org/10.1177/0020764008101639 [ Links ]
38.Van der ham L, Wright P, Doan D, Broerse JE. Perceptions of mental health and help seeking behaviours in an urban community in Vietnam: An explorative study. Community Ment Health J. 2011;47(5):574-582. https://doi.org/10.1007/s10597-011-9393-x [ Links ]
39.Naeem F, Ayub M, Kingdon D, Gobbi M. Views of depressed patients in Pakistan concerning their illness, its causes, and treatments. Qual Health Res. 2012;22(8):1083-1093. https://doi.org/10.1177/1049732312450212 [ Links ]
40.Khan T, Suliman S, Hassai M. Mental health literacy towards depression among non-medical students at a Malaysian university. Ment Health Fam Med. 2010;7:27-35. [ Links ]
41.Angemeyer M, Millier A, Remuzat C, et al. Attitudes and beliefs of French public about schizophrenia and major depression: Results from a vignette-based population survey. BMC Psychiatr. 2013;13:313. https://doi.org/10.1186/1471-244X-13-313 [ Links ]
42.Harsh E. Mental health literacy among Sri Lankan Cares of patients with schizophrenia and depression. Asian J Psychiatr. 2012;5(3):246-250. https://doi.org/10.1016/j.ajp.2012.02.016 [ Links ]
43.Teferra S, Shibre T. Perceived causes of severe mental disturbance and preferred interventions by Borana semi-nomadic population in southern Ethiopia: A qualitative study. BMC Psychiatr. 2012;12:79. https://doi.org/10.1186/1471-244X-12-79 [ Links ]
44.Kate, Grover S, Nehra R. Supernatural beliefs, aetiological models and help seeking behaviours in patients with schizophrenia. Ind Psychiatr J. 2012;21(1):49-54. https://doi.org/10.4103/0972-6748.110951 [ Links ]
 Correspondence:
Correspondence:
Dumisile Madlala
dumipsm@gmail.com
Received: 18 Nov. 2020
Accepted: 11 Aug. 2021
Published: 24 Mar. 2022
The Cases
Betty
Betty is a 34 year old married female with two children, she presents with 4 weeks history of the following symptoms:
1.She has low mood every day and most of the day.
2.She lacks interest and does not enjoy things anymore most of the time, nearly every day.
3.She feels sad, empty and hopeless.
4.She is not sleeping well.
5.She is very slow.
6.She is always tired.
7.She feels small, has low self-esteem and feels worthless and guilty about a lot of things.
8.She cannot think clearly and concentrate.
9.She thinks it is better to die.
As a result she is no longer able to take care of her family
She is physically health and does not use drugs.
Tick what you think is correct
Muzzy
Muzzy is 25 years of age. He is not married. He dropped out of university in his first year about 3 years ago. Since then he has often been hearing a voice that tells him what to do. He then also started talking in a way that does not make sense. He became very aggressive towards his uncle, and accused his uncle of planting wires inside his stomach. He still believes that his uncle did it. At present he does not like to mix with others and prefers to do nothing.
He is physically healthy and does not use drugs.
Lucy
Lucy is a 37 year old female. She experiences excessive worry and she is always anxious. She finds it difficult to control the worries and it affects her ability to do her chores. She also experiences the following symptoms:
1.She is restless.
2.She becomes tired easily.
3.She cannot concentrate.
4.She is irritable.
5.She has muscle tension.
6.She has problems with sleeping.
She physically healthy and does not use drugs.














