Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Psychiatry
versão On-line ISSN 2078-6786
versão impressa ISSN 1608-9685
S. Afr. j. psyc. vol.27 no.1 Pretoria 2021
http://dx.doi.org/10.4102/sajpsychiatry.v27i0.1617
ORIGINAL RESEARCH
Prevalence and correlates of psychological distress amongst healthcare workers during the COVID-19 pandemic: An online survey
Olamiji A. BadruI; Kehinde O. OlokoII; Abdulwasiu O. HassanIII; Oyindamola B. YusufIV; Umar A. Abdur-RazaqV; Saheed YakubVI
IDepartment of Mental Health and Behavioural Medicine, Federal Medical Center, Abeokuta, Nigeria
IIDepartment of Haematology, Haematology Mavens Specialist Center, Lagos, Nigeria
IIIDepartment of Medical Laboratory Science, Achievers University, Owo, Nigeria
IVDepartment of Epidemiology and Medical Statistics, Faculty of Public Health, College of Medicine, University of Ibadan, Ibadan, Nigeria
VDepartment of Nursing Science, Faculty of Clinical sciences, College of Medicine, University of Lagos, Lagos, Nigeria
VIDepartment of Surgery, Osun State University (UNIOSUN) Teaching Hospital, Osun, Nigeria
ABSTRACT
BACKGROUND: Understanding the mental health needs of healthcare workers during coronavirus disease 2019 (COVID-19) pandemic with a view of mitigating its impact on occupational functioning is vital
AIM: To determine the prevalence and correlates of psychological distress amongst healthcare workers
SETTING: The study was carried out in Nigeria during COVID-19 pandemic
METHODS: A cross-sectional quantitative study using a convenience sample was conducted amongst healthcare workers. The survey comprised of two Google formatted self-report questionnaires, a 12-item General Health Questionnaire and a questionnaire containing socio-demographic, work related and knowledge of COVID-19 variables. Questionnaires were distributed via closed professional WhatsApp platforms. Data were analysed using descriptive statistics, chi-square test and logistic regression
RESULTS: There were 313 respondents and prevalence of psychological distress was 47.0%. Females were almost twice as likely to have psychological distress as males (OR = 1.92, 95% CI: 1.21-3.04, p = 0.006). Healthcare workers who had no contact with COVID-19 positive patients had an 87% reduced risk of psychological distress (OR = 0.13, 95%CI: 0.23-0.25, p = 0.018) compared with those who had contact with COVID-19 positive patients. Healthcare workers with poor knowledge of COVID-19 had a 44% reduced risk of psychological distress compared with those with good knowledge (OR = 0.56, 95% CI: 0.34-0.93, p = 0.025
CONCLUSION: Findings revealed that healthcare workers in Nigeria reported psychological distress during COVID-19 pandemic. Greater risk was amongst females and those who had contact with COVID-19 positive patients whilst poor knowledge was protective
Keywords: COVID-19; psychological distress; healthcare workers; Nigeria; general health questionnaire-12 (GHQ-12), pandemic.
Introduction
The pandemic of 2019 novel coronavirus disease (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first reported in Wuhan, China, before becoming global.1 The index case in Nigeria was reported on 27 February 2020, thereafter, 10 162 cases were confirmed by 31 May 2020.2,3 Considering the novelty of COVID-19, the possibility of adverse effects on psychological well-being as a result of unpredictability of its outbreak cannot be overemphasised, especially amongst healthcare workers.4
The workplace is an environment that may generate demands and pressures such as excessive workload. Studies suggest that healthcare workers develop increased levels of psychological distress during outbreak of infectious diseases, especially when work conditions are not favourable.4,5 Thus, compromise of effective healthcare service delivery may be an aftermath of mental imbalance experienced by healthcare workers during COVID-19 pandemic. Contrary to the general population, healthcare workers can neither afford to stay safe at home nor practice physical distancing in view of their professional calling. In addition, scarcity of personal protective equipment exposes healthcare workers, especially clinical staff at increased risk of getting infected, which may lead to increased anxiety.6
A cross-sectional survey assessing psychological distress in the community and amongst medical students, medical staff and patients with COVID-19, in Iran with the Depression, Anxiety and Stress Scale (DASS) revealed lower scores amongst medical students compared with medical staff. Professionalism amongst medical staff perhaps served as a protective factor, which made them less prone to psychological distress.7
In addition, the emotional consequence of COVID-19 pandemic on healthcare workers in Singapore revealed that 14.5% participants had anxiety, 8.9% had depression, 6.6% were positive for stress and clinical concern of post-traumatic stress disorder (PTSD) was reported amongst 7.7%.8 Another cross-sectional on-line survey using the Insomnia Severity Index (ISI), the Symptom Check List-revised (SCL-90-R), and the Patient Health Questionnaire-4 (PHQ-4 to assess mental health variables amongst both medical and non-medical staff in China revealed increased morbidity amongst medical staff.9
Therefore, it is vital to determine the mental health impact of COVID-19 on healthcare workers, more so that healthcare workers have been reported to get infected in their line of duty.10 This study aimed to determine the prevalence of psychological distress amongst healthcare workers during the COVID-19 pandemic and to assess the associated, socio-demographic, level of knowledge and work-related correlates.
Methods
A cross-sectional quantitative study, using a convenience sample, was conducted amongst healthcare workers between 01 April 2020 and 30 June 2020. The survey comprised of two Google formatted self-report questionnaires: A 12-item General Health Questionnaire (GHQ) to assess psychological distress and a questionnaire containing socio-demographic, work related and knowledge of COVID-19 variables. Questionnaires were sent through broadcast messages with a brief description of the study via series of network of healthcare workers' WhatsApp groups in Nigeria. Questionnaires were then filled and submitted via the attached questionnaire link.
Settings
The study was conducted in Nigeria from 01 April to 30 June 2020, during the COVID-19 pandemic.
Study population
Our study population included healthcare workers residing in Nigeria who could be contacted via WhatsApp during the pandemic irrespective of the type of healthcare worker or type of health facility. Healthcare workers not residing in Nigeria were excluded.
Sample size calculation
The sample size was estimated using the formula for determining the sample size for single proportions, which is as follows:

where  = standard normal deviate at α set at 0.05 = 1.96
= standard normal deviate at α set at 0.05 = 1.96
α = level of significance
p = proportion of the population with the variable of interest, that is, psychological distress
This was estimated as 35% from a previous study.1
q = 1-p
d = margin of error = 0.06
n = minimum sample size = 243
~ 316
Although the estimated sample size was 243, the sample size was increased by 30% (72.9) to accommodate for non-response.
Instruments
Socio-demographic questionnaire
A structured questionnaire was composed to obtain information on socio-demographic and work-related variables and level of knowledge regarding the COVID-19 pandemic. The socio-demographic variables included, gender, age, type of religion, frequency of participation in religious activities and marital status. The work-related variables included, type of healthcare worker, years of service, coming into contact with COVID-19 positive patients (confirmed or suspected cases), recovery or death of COVID-19 positive patients, being a routine frontline healthcare worker (working at the first point of call in health facilities, for example, accident and emergency units) and provision of incentives as a frontline healthcare worker.
Variables to test the level of knowledge of healthcare workers towards the pandemic were: their understanding on availability of vaccine, whether it could be cured, how contagious the virus was; its prevention through: frequent hand washing, use of face masks, staying at home and social distancing. Each correct response was scored as 1 whilst a wrong response was scored as 0. The responses were added and the mean was calculated as 5.96 ± 1.05. Respondents with scores above the mean were regarded as those with good knowledge whilst those with scores below the mean were regarded as those with poor knowledge.
General Health Questionnaire-12
General Health Questionnaire-12 (GHQ-12) designed by David Goldberg in 1978 was used in this study.11 It is a 12-item easy to use screening instrument for general psychiatric morbidity such as psychological distress. Questions in the instrument were: ability to concentrate, loss of sleep over worry, playing useful part in things, ability to make decisions, being under strain, inability to overcome difficulties, ability to enjoy day to day activities, being able to face up to problems, feeling unhappy or depressed, losing self-confidence, thinking of self as worthless and feeling reasonably happy, all things considered. The instrument can be scored either on the Likert scale or on the bimodal scale. The bimodal scale was used in this study.
On the bimodal scale, the two least symptomatic answers score 0 and the two most symptomatic answers score 1 (i.e. 0-0-1-1), the score range is 0-12 with a score of 3 or more indicative of psychological distress.
The GHQ-12 has been reported to have inter-rater reliability and internal consistency with Cronbach's alpha of 0.76.12 It has equally been validated for use in Nigeria13 and has been used in several studies to identify psychiatric distress in other settings.14,15,16
Procedure
Google formatted forms containing both self-administered questionnaires were posted on-line via several healthcare workers' WhatsApp platforms of various health facilities. The two questionnaires were formatted in such a way that all questions were required to be answered for submission to be possible. The completely filled questionnaires were submitted via Google to the attached e-mail address.
Data analysis
All the data received via Google within the specified period of data collection were cleaned and analysed with SPSS version 23 software. Data were summarised with descriptive statistics such as mean, standard deviation and percentage. The chi-square test was used to investigate associations between psychological distress and socio-demographic, level of knowledge of COVID-19 and work-related variables. Variables that were significant in the chi-square analysis were entered into a binary logistic regression model to further explore the association between psychological distress and level of knowledge whilst controlling for the effect of other confounding variables such as gender and contact with COVID-19 positive patients. All analyses were carried out at 5% level of significance.
Ethical considerations
Informed consent and confidentiality were ensured. Ethical approval was given by Ethics and Research Committee, Ladoke Akintola University of Technology Teaching Hospital Osogbo, Osun State, protocol number: LTH/EC/2020/07/465.
Results
A total of 313 completed questionnaires were received and analysed. Of the 313 respondents, 147 (47%) had a GHQ-12 score of 3 and above indicating psychological distress, whilst 166 (53.0%) scored less than 3.
Association between psychological distress and socio-demographic variables
Being female was the only socio-demographic variable (χ2 = 7.07, p = 0.008) that was found to be significantly associated with psychological distress (Table 1).
Association between psychological distress and work-related variables
Of the work-related variables, only having contact with COVID-19 positive patients was significantly associated with psychological distress (χ2 = 5.57, p = 0.018) (Table 2).
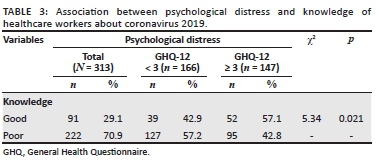
Association between psychological distress and knowledge
Psychological distress was more frequent amongst healthcare workers with a good knowledge of COVID-19 (n = 52; 57.1%) than those with a poor level of knowledge (95; 42.8%), χ2= 5.34, p = 0.021 (Table 3).
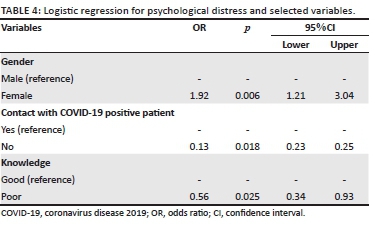
Logistic regression analysis for psychological distress
Female healthcare workers were about twice as likely to have psychological distress as their male counterparts (OR = 1.92, 95% CI: 1.21-3.04, p = 0.006). Healthcare workers who had no contact with COVID-19 positive patients had an 87% reduced risk of psychological distress (OR = 0.13, 95% CI: 0.23-0.25, p = 0.018) compared with those who had contact with COVID-19 positive patients. Healthcare workers with poor knowledge of COVID-19 had a 44% reduced risk of psychological distress (OR = 0.56, 95% CI: 0.34-0.93, p = 0.025) compared with those with good knowledge (Table 4).
Discussion
The prevalence of psychological distress amongst respondent healthcare workers was 47.0%. Female gender was a risk factor whilst poor knowledge of the pandemic and lack of contact with of COVID-19 positive patients were protective factors.
Prevalence of psychological distress amongst healthcare workers in Nigeria
Nearly half of the participants reported psychological distress in this study. This is comparable with a study in Pakistan where a prevalence of 42% for moderate psychological distress was reported amongst healthcare workers.17
However, in China, 71.5% of healthcare workers reported distress compared with the 47% in our study. The lower prevalence in our study may be related to differences in the study population, as only healthcare workers attending to patients with fever or COVID-19 clinic participated in the Chinese study. The difference in the instruments used may also have a bearing on the results. Psychological distress in our study was measured with GHQ-12 whilst distress in the Chinese study was assessed with the 22-item Impact of Event Scale-Revised. Although both are self-report questionnaires, the 22-item Impact of Event Scale-Revised is more specific to traumatic events whilst GHQ-12 measures general psychiatric morbidity. Another reason for the lower prevalence in our study may be because of previous knowledge of the pandemic before it found its way into the country. Coronavirus disease 2019 was reported in China at the end of 2019, whilst the first case ever reported in Nigeria was on 27 February 2020.1,2,18
Religion has been shown to influence behaviour through the control of emotional response to stressors or through the modification of the social milieu of the stressor itself.19 Given the high number of respondents who participated in religious activities in our study, religion may be a good coping mechanism ameliorating the effect of the pandemic on healthcare workers. However, there was no significant difference between those who participated frequently in religious activities and those who did not.
Prior to COVID-19 pandemic in Nigeria, studies carried out amongst healthcare workers with GHQ-12 in 2012 and 2018 reported prevalence of 10% and 17.2%, respectively. Therefore, the higher prevalence in our study may not be unconnected with COVID-19 pandemic. The 2012 study was conducted amongst 30 doctors and nurses working at a university medical centre whilst the 2018 survey was carried out amongst 256 doctors, nurses, pharmacists and medical laboratory scientists working in a teaching hospital.20,15
Psychological distress and socio-demographic variables
Psychological distress was more in females compared with males. In keeping with our study, women reported more severe symptoms in China.9,18,21 Similarly, in Saudi Arabia, the level of distress was higher amongst females.22 Women suffer more from psychological distress than men, especially when confronted with clashes between their jobs and family lives.23,24 The novelty of the pandemic might have disrupted the hitherto equilibrium between work and family life achieved amongst females.
Another explanation could be that men may not be too willing to admit to some of the symptoms elicited by GHQ-12 that are not in keeping with their conventional role in the society.25 Given the non-availability of data base of all healthcare workers, the possibility of having a higher ratio of women to men amongst all healthcare workers in Nigeria amongst those who participated in the study cannot be verified. Otherwise, the probability of a higher ratio of women compared with men would have been said to be the reason why more women were distressed. However, it is good to note that, the probability of having a higher proportion of women with psychological distress out of those who actually participated in our study could not have been related to their higher number given that the number of male and female respondents in this study were close.
Psychological distress and work-related variables in Nigeria
No significant association was found between psychological distress and different categories of healthcare workers, including nurses. This is contrary to other literature findings where nurses were reported to be at increased risk of mental health challenges during outbreak of infectious diseases.26 Studies have shown that the female gender and being nurses who invariably are females are risk factors for psychological distress.9,18,27 It is, however, noteworthy that in our study, female gender is a risk factor, whilst being a nurse is not.
It is not surprising that psychological distress was more amongst healthcare workers who had contact with COVID-19 positive patients. Coming into proximity with people infected by the virus may increase the fear of contracting the disease, which may lead to distress. This risk may be compounded by pre-existing poor healthcare system, poor funding and scarcity of personal protective equipment, which has been a cause for concern in some healthcare delivery systems.18,28,29
Psychological distress and knowledge of coronavirus 2019
The number of participants with good knowledge of COVID-19 who developed psychological distress was higher compared with those with poor knowledge. This is a paradoxical finding. Good knowledge is assumed to be protective, however, those with good knowledge were the ones more affected. Alternative explanation may be that knowledge about the cause and prevention of COVID-19 may stimulate negative emotional responses more, especially when it is seemingly impossible to achieve the preventive measures in a poor resource setting.
In addition, El Hage et al. in a narrative review of literature on mental health risks of COVID-19 amongst healthcare workers identified lack of specific drugs as contributory to the mental health problems amongst healthcare workers.30 Furthermore, the absence of a vaccine for the containment of the virus reported by Cascella et al. in a review of the features, evaluation and treatment of COVID-19 maybe a source of distress.31 It may therefore not be out of place when healthcare workers who have a good knowledge of COVID-19 are more distressed.
Limitations and strength
Causality cannot be determined because of the cross-sectional nature of the study. Data were a convenient sample, which may impact its representativeness. In addition, use of self-report questionnaires may give room to report bias from respondents. There is, therefore, a need to exercise caution in the interpretation of our findings in the light of these limitations. This is the first on-line study on psychological distress amongst healthcare workers in Nigeria during COVID-19 pandemic to the best of our understanding.
Conclusion
Our findings revealed that healthcare workers in Nigeria reported psychological distress during COVID-19, with greater risk amongst females compared with males and amongst those who had contact with COVID-19 positive patients. Unexpectedly, poor knowledge was found to be protective. There is a need for more research to evaluate the role of the pandemic in the reported distress, as well as risk and protective factors.
Acknowledgements
The authors would like to thank Mr Olanrewaju Eniade for assisting with the statistical analysis.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
O.A.B. conceptualised, designed and was responsible for the intellectual discucussion, K.O.O., A.O.H. and S.Y. contributed to reviewing and editing the manuscript, U.A.A. contributed in the data analysis and design of questionnaire, O.B.Y. was responsible for the critical appraisal of the methodology and statistical analysis. All authors read and approved the final manuscript.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The data are unsuitable for sharing because of confidentiality as a result of stigmatisation of mental disorders.
Disclaimer
The views and opinion expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psych. 2020;33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213 [ Links ]
2. Nigeria Center for Disease Control. Public health advisory to Nigerians on novel coronavirus [homepage on the Internet]. 2020 Feb 29 [cited 2020 Jun 17]. Available from: https://ncdc.gov.ng/news/234/29th-february-2020%7C-public-health-advisory-to-nigerians-on-novel-coronavirus-%28%234%29 [ Links ]
3. Nigeria Center for Disease Control [homepage on the Internet]. 2020 [cited 2020 Jun 17]. Available from: https://t.co/YKOiX7aMA5 [ Links ]
4. Robertson LJ, Maposa I, Somaroo HO, Johnson O. Mental health of healthcare workers during the COVID-19 outbreak: A rapid scoping review to inform provincial guidelines in South Africa. S Afr Med J. 2020;110(10):1010-1019. https://doi.org/10.7196/SAMJ.2020.v110i10.15022 [ Links ]
5. Gray P, Senabe S, Naicker N, Kgalamono S, Yassi A, Spiegel JM. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. Int J Environ Res Public Health. 2019;16(22):4396. https://doi.org/10.3390/ijerph16224396 [ Links ]
6. Boškoski I, Gallo C, Wallace MB, Costagmana G. COVID-19 pandemic and personal protective equipment shortage: Protective efficacy comparing masks and scientific methods for respirator reuse. Gastrointest Endosc. 2020;92(3):519-523. https://doi.org/10.1016/j.gie.2020.04.048 [ Links ]
7. Vahedian-Azimi A, Moayed MS, Rahimibashar F, Shojaei S, Ashtari S, Pourhoseingholi MA. Compare the severity of psychological distress among four groups of Iranian society in COVID-19 pandemic. BMC Psychiatry. 2020;20(1):402. https://doi.org/10.1186/s12888-020-02804-9 [ Links ]
8. Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173 (4):317-320; M20-1083. https://doi.org/10.7326/M20-1083 [ Links ]
9. Zhang W, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89(4):242-250. https://doi.org/10.1159/000507639 [ Links ]
10. Oludare I. Abeokuta: FMC nurse discharged from COVID-19 isolation centre. Daily post Nigeria [homepage on the Internet]. [cited 2020 May 16]. Available from https://dailypost.ng/2020/05/16/abeokuta-fmc-nurse-discharged-from-covid-19-isolation-centre [ Links ]
11. Goldberg DP, Williams P. A user guide to the General Health Questionnaire. Windsor: NFER-Nelson Publisher; 1978. [ Links ]
12. Sanchez-Lopez MP, Dresch V. The 12-item General Health Questionnaire (GHQ-12): Reliability, external validity and factor structure in the Spanish population. Psicothema. 2008;20(4):839-843. [ Links ]
13. Gureje O, Obikoya B. The GHQ-12 as a screening tool in a primary care setting. Soc Psychiatr Epidemiol. 1990;25(5):276-280. https://doi.org/10.1007/BF00788650 [ Links ]
14. Esan O, Adeoye B, Onakoya P, et al. Features of residency training and psychological distress among residents in a Nigerian teaching hospital. S Afr J Psychiatry. 2014;20(2):46-50. https://doi.org/10.4102/sajpsychiatry.v20i2.426 [ Links ]
15. Obadeji A, Oluwole LO, Dada MU, Oshatimi MA. Alcohol use and psychological wellbeing of health workers in a Nigerian Hospital: An exploratory study. Malawi Med J. 2018;30(1):31-36. https://doi.org/10.4314/mmj.v30i1.7 [ Links ]
16. Mohammed A, Sheikh TL, Gidado S, et al. An evaluation of psychological distress and social support of survivors and contacts of Ebola virus disease infection and their relatives in Lagos, Nigeria: A cross sectional study. BMC Public Health. 2015;15(1):824. https://doi.org/10.1186/s12889-015-2167-6 [ Links ]
17. United Nations. Policy brief: COVID-19 and the need for action on mental health: Specific populations [homepae on the Internet]. 2020; p. 11 [cited 2020 Aug 26]. Available from: https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf [ Links ]
18. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 [ Links ]
19. Krägeloh CU. A systematic review of studies using the brief COPE: Religious coping in factor analyses. Religions. 2011;2(3):216-246. https://doi.org/10.3390/rel2030216 [ Links ]
20. Coker OO, Coker, Ayodele AO, Apampa RA. An assessment of emotional pain and psychological distress among health workers in a university medical centre in Lagos, Med Rev. 2012;18(7):5-8. [ Links ]
21. Si MY, Su XY, Jiang Y, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. 2020;9(113):2020. https://doi.org/10.1186/s40249-020-00724-0 [ Links ]
22. Al-Hanawi MK, Mwale ML, Alshareef N, et al. Psychological distress amongst health workers and the general public during the COVID-19 pandemic in Saudi Arabia. Risk Manag Healthc Policy. 2020;2020(13):733-742. https://doi.org/10.2147/RMHP.S264037P [ Links ]
23. Honda A, Abe Y, Date Y, Honda S. The impact of multiple roles on psychological distress among Japanese workers. Saf Health Work. 2015;6(2):114-119. https://doi.org/10.1016/j.shaw.2014.12.004 [ Links ]
24. Viertiö S, Kiviruusu O, Piirtola M. Gender and psychological distress: Contribution of work-family balance. Eur J Public Health. 2019;29(4):ckz187.116. https://doi.org/10.1093/eurpub/ckz187.116 [ Links ]
25. Smith DT, Mouzon DM, Elliott M. Reviewing the assumptions about men's mental health: An exploration of the gender binary. Am J Mens Health. 2018;12(1):78-89. https://doi.org/10.1177/1557988316630953 [ Links ]
26. Park JS, Lee EH, Park NR, Choi YH. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: A cross-sectional study. Arch Psychiatr Nurs. 2018;32(1):2-6. https://doi.org/10.1016/j.apnu.2017.09.00635 [ Links ]
27. Mo Y, Deng L, Zhang L, et al. Work stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic. J Nurs Manag. 2020;28(5):1002-1009. https://doi.org/10.1111/jonm.13014 [ Links ]
28. Jaffery R. Pakistan struggles to fight COVID-19. The diplomat [homepage on the Internet]. 2020 [cited 2020 Dec 25]. Available from: https://thediplomat.com/2020/04/pakistan-struggles-to-fight-covid-19/ [ Links ]
29. Khalid A, Ali S. COVID-19 and its challenges for the healthcare system in Pakistan. ABR. 2020;12(4):551-564. https://doi.org/10.1007/s41649-020-00139-x [ Links ]
30. El-Hage W, Hingray C, Lemogne C, et al. Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: What are the mental health risks? Encephale. 2020;46(3 Suppl):S73-S80. https://doi.org/10.1016/j.encep.2020.04.008 [ Links ]
31. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment of coronavirus (COVID-19) [homepage on the Internet]. StatPearls. 2021 [cited 2020 Apr 25]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554776/ [ Links ]
 Correspondence:
Correspondence:
Olamiji Badru
biodunbadru2008@yahoo.com
Received: 28 Aug. 2020
Accepted: 03 May 2021
Published: 29 July 2021














