Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Psychiatry
versão On-line ISSN 2078-6786
versão impressa ISSN 1608-9685
S. Afr. j. psyc. vol.21 no.2 Pretoria Mai. 2015
http://dx.doi.org/10.7196/SAJP.661
ARTICLE
What patients with bipolar disorder and major depressive disorder perceive as adverse life events precipitating a current major depressive episode
R A van Schoor; P M Joubert
MB ChB, MMed (Psych), FCPsych (SA); Department of Psychiatry, Faculty of Health Sciences, University of Pretoria, South Africa
ABSTRACT
BACKGROUND: Adverse life events (ALEs) as precipitants of a major depressive episode (MDE) have been the subject of many studies. These studies indicate an increase in ALEs in the 6 months preceding an MDE.
OBJECTIVES: The study examined what participants, suffering from major depressive disorder (MDD) or bipolar disorder (BD), perceived as the precipitating ALE of a current MDE. The severity and categories of ALEs were compared between these two patient groups.
METHODS: Consenting, adult inpatients were sourced from Weskoppies Hospital, Steve Biko Academic Hospital, Tshwane District Hospital, Denmar Psychiatric Hospital and Vista Clinic in the Pretoria area. A semi-structured questionnaire was used to obtain demographic data and the diagnosis. Information regarding the course of the disorder, including the number of previous MDEs and the age at which the first MDE occurred, was also obtained. The perceived precipitating ALE was detailed for each participant. A severity value referred to as a Life Change Unit Score (LCU score), based on the Recent Life Changes Questionnaire (RLCQ) by Miller and Rahe, was then assigned to each participant's perceived precipitant.
RESULTS: Of the 64 participants, 12.7 % were experiencing a first MDE. In those participants who had experienced prior episodes the average number (standard deviation (SD)) of previous episodes was 3.86 (2.46). The mean approximate age (SD) at first onset of an MDE was 24.81 (10.9) years. The BD group had significantly more previous MDEs than the MDD group. Although the average LCU scores were higher in the BD group than the MDD group this did not reach statistical significance. Therefore, this study could not find a difference in the severity ofthe perceived precipitants between the BD group and MDD group. However, when the LCU scores were analysed within subcategories of the RLCQ, it was found that participants with BD perceived significantly more problems associated with the workplace as precipitants of a current MDE than individuals with MDD.
CONCLUSION: Most participants could link an ALE to the onset of a current MDE. The study did not find a differential response to ALEs between patients with BD and MDD. The severity of the social precipitants did not differ significantly between the two groups. The notion of a 'kindling effect' could not be supported by the outcome of this study. Because some study participants experienced ALEs not accounted for by the RLCQ, a more comprehensive assessment instrument may be more appropriate for similar studies.
Adverse life events (ALEs) as precipitants of a major depressive episode (MDE) have been the subject of many studies.[1-7] Such studies indicate that there tends to be an increase in ALEs in the 6 months preceding an MDE.[1,4,5] In line with the 'kindling effect' hypothesis more stressful ALEs are needed for the first MDE, with progressively less stressful ALEs needed for subsequent episodes.[8] The kindling effect hypothesis holds that major life stressors are required to trigger the initial onset of a mood episode, but that subsequent episodes become progressively less tied to stressors, so that they eventually occur spontaneously, or at least seemingly spontaneously.[8-10] Since this original idea was postulated by Post[8] several studies have supported the hypothesis[6,7,11-13] while others have not.[14-16]
Apart from a study examining the differences in ALEs between patients with dysthymic disorder and major depressive disorder (MDD)[17] to the best of the authors' knowledge, no study has yet compared the severity of ALEs before an MDE in relation to bipolar disorder (BD) and MDD. This study aims to make that comparison. The study examines participants who suffer from MDD or BD who recently suffered a first MDE or a recurrence of an MDE, specifically regarding what these participants perceive as the precipitating ALE of their current MDE. The study also compares the severity and categories of ALEs between participants suffering from MDD and BD.
Method
The study was approved by the Research Ethics Committee of the Faculty of Health Sciences, University of Pretoria. Consenting adult psychiatric inpatients were sourced from five hospitals in the Pretoria area: Weskoppies Hospital, Steve Biko Academic Hospital, Tshwane District Hospital, Denmar Psychiatric Hospital and Vista Clinic. To qualify for the study, participants had to be 18 years or older, be able to give informed consent, and be suffering from either MDD or BD (bipolar I disorder or bipolar II disorder). Participants had to be suffering from an MDE irrespective of whether it was a first or subsequent episode. A subsequent episode was defined as the recurrence of an MDE after a period of full or partial remission for at least 3 months. At least 30 participants were needed for each group for the purposes of statistical comparison. The study made use of convenience sampling based on the availability of suitable subjects for the study's purposes. Consequently the numbers of the subjects in each group are not representative of the incidence and prevalence of MDD and BD in the general population. Participants were excluded if they suffered from a non-mood psychotic disorder, a substance-induced mood disorder, mood disorder due to a general medical condition or a mixed episode.
All interviews were semi-structured and performed by the first author. The structured part of the interview consisted of a questionnaire assessing participants' demographic data, diagnosis, course of the disorder including the number of previous MDEs, and age at which the first MDE had occurred. The unstructured part of the interview allowed participants to elaborate on what they perceived as stressful life events that had precipitated their current MDE. When needed, the interviewer sought clarity about the perceived stressful life events reported by participants during the interview. The results were recorded in writing.
Using the results of the interview, as set out above, the researchers allocated a severity score to participants' perceived ALEs by mutual agreement. The severity score was based on the Recent Life Changes Questionnaire (RLCQ) by Miller and Rahe[18] However, the researchers found that some of the participants' perceived ALEs did not exactly fit into any of the categories and subcategories provided by the RLCQ. That challenge was addressed by discussing the issue and agreeing on a category in the RLCQ that best reflected the stressful life event in question. This was done in five instances: (i) a participant reported struggling to find employment for the first time; the score of investment and/or credit difficulties was given; (ii) a friend's baby died while in the care of a participant; the score of a major change in health or behaviour of a family member was assigned; (iii) being charged with manslaughter was assigned as double the score of a minor violation of the law; (iv) inability to perform parenting obligations to a 3-year-old child as a result of mental illness was assigned the score of experiencing illness or injury; (v) experiencing a reaction on the anniversary of death of a sibling was assigned half the score of the death of a close family member.
Having completed the scoring of participants' individual ALEs, the individual scores of each participant's stressful life events were added up to provide a total Life Change Unit Score (LCU score) in accordance with Miller and Rahe.[18] These scores were later used for statistical analysis. This consisted of basic descriptive statistics, cross-tabulations, the x2-test, Fisher's exact test and the Mann-Whitney (7-test. The x2-test was used to assess associations between the demographic variables and comparisons between the two clinical groups. The Fisher's exact test was used to assess the demographic variable: race. All other demographic variables were assessed using the x2-test. A non-parametric test, the Mann-Whitney (7-test, was used to analyse the course of the disorder (i.e. the number of previous episodes) and the differences in the LCU scores between the 2 groups of participants (MDD and BD). A p-value of <0.05 was considered statistically significant.
Results
A total of70 patients were interviewed, of whom 6 were excluded. The reasons for exclusion were as follows: 2 patients denied feeling depressed despite being admitted and treated for an MDE, 1 was too cognitively impaired, 1 patient's diagnosis was not an MDD, bipolar I disorder, or bipolar II disorder, 1 because the questionnaires lacked the necessary information to rate stressor severity, and 1 because the perceived stressor was a delusion. Thus, 64 participants entered the study. Thirty participants suffered from BD, thereby constituting the BD group, while 34 participants suffered from MDD, thereby constituting the MDD group. In the BD group, 20 participants had bipolar I disorder and 10 had bipolar II disorder.
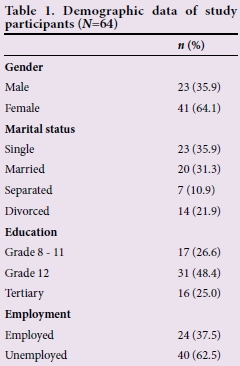
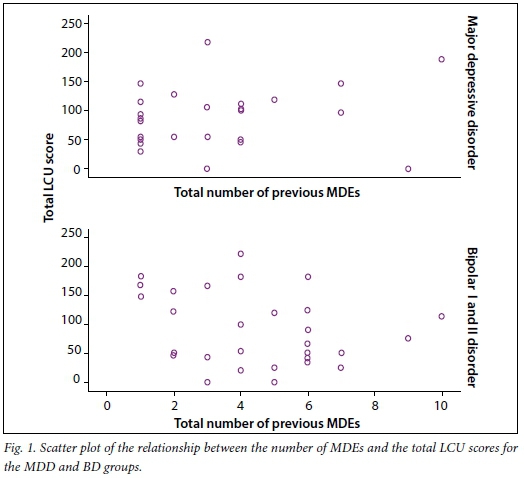
Table 1 summarises the demographic data of the sample. The mean age of participants (standard deviation (SD) was 38.97 (10.3) years. There were no significant demographic differences between the MDD group and BD group. Table 2 presents the main results of the study. Fig. 1 displays a scatter plot of the relationship between the number of MDEs and the total LCU scores for the MDD and BD groups.
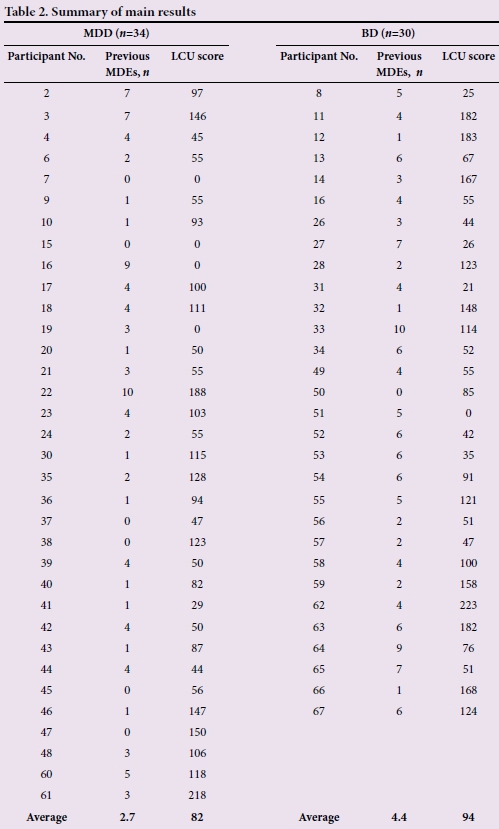
Ofthe 64 participants, 12.7% were experiencing a first MDE. In those participants who had experienced prior episodes the average number (SD) of previous episodes was 3.86 (2.46). The mean approximate age at first onset of an MDE was 24.81 (10.9) years and this did not differ significantly between the two patient groups (p=0.200). The BD group did however have significantly more previous MDEs than the MDD group (p=0.013).
Although the average LCU scores were higher in the BD group than the MDD group this did not reach statistical significance (p=0.499). This disconfirms the null hypothesis that there may be a difference in the severity of the perceived precipitant between the two groups of patients based on clinical diagnosis.
The LCU scores were analysed within subcategories of the RLCQ. The mean LCU scores for the subcategories 'Health, 'Home and family, 'Personal and social' and 'Financial' did not differ significantly across the two groups based on clinical diagnosis. The mean LCU subscores for 'Work' did however differ significantly between the two groups. In the MDD group, the average LCU score for the subcategory of work was 7.17% of the total LCU score, while the average for the bipolar group was 25.4% of the total LCU score. In this sample of patients, individuals with BD experienced significantly more problems associated with the workplace as precipitants of a current MDE than individuals with MDD.
Discussion
The results of this study are in keeping with previous studies in that most participants reported ALEs, which they think precipitated a current MDE. As reported by the participants of this study, other studies reported that one of the variables that are most consistently associated with the onset of MDEs is an ALE. These studies reported that there is a significant increase in stressful life events in the 6 months preceding the onset of an MDE.[1-7] It seems that the tendency of an ALE to result in an MDE is related to an individual's ability to cope with a stressor.[2] Consequently, on the one hand seemingly uncontrollable ALEs are more likely to cause a sense of hopelessness, which may precipitate an MDE, while on the other hand ALEs perceived as controllable along with adequate coping methods lead to less hopelessness, which may be protective against an MDE.[2] Furthermore, depressed individuals seem to have an emotion-based coping style rather than a problem-focused coping style.[17]
While this study compared perceived ALEs related to the onset of MDEs between BD and MDD, Moerk and Klein[4] examined ALEs related to depressive episodes in MDD and in people who had dysthymic disorder and subsequently experienced an MDE. They found that in dysthymic disorder a first MDE was associated with a new ALE in the context of a chronic stressor. However, in MDD relapse was associated with the occurrence of a new ALE irrespective of the presence of a chronic stressor. [4] They found no support for the notion of a differential response to the severity of ALEs when dysthymic disorder and MDD were compared.[4] When ALEs between BD and MDD were compared in the present study, a differential response to ALEs was also not detected. Yet, the present study found that when the categories of ALEs were compared, participants suffering from BD more frequently reported problems in the workplace as an ALE precipitating an MDE than participants suffering from MDD.
Previous studies have identified that stressors at work play a significant role in precipitating MDEs. Wang[19] analysed a large representative community-based sample to assess the effects of work stress on individuals. High levels of work stress (identified as measuring above the 75th percentile on the work stress scale) were associated with an elevated risk of MDEs during the follow-up period. The results showed that work stress was an independent risk factor for the development of an MDE.[19]
Another important aspect to consider when looking at ALEs as precipitants of an MDE is the so-called 'kindling effect'. The kindling effect as described by Post[8] in 1992 hypothesises that major life stress is required to trigger initial onsets and recurrences of affective episodes but successive episodes become progressively less tied to stressors and may eventually occur autonomously. Lewinsohn et al.[11]found that stressful life events predicted the first onset of MDD and the amount of stress preceding the first episode was significantly greater than the magnitude of stressors associated with a recurrence of MDD. The kindling effect includes two hypotheses. One concept is that of stress autonomy, where a progressive decoupling between stressors and MDEs occurs and an endogenous neurobiological mechanism takes over as the determinant for future episode timing. The other concept is that of stress sensitisation. The idea is that psychosocial stressors that previously were insufficient to initiate an episode of depression seem to acquire the ability to initiate recurrent episodes. There is progressive sensitisation to less severe forms of stress.[9,10] Since the original idea was postulated by Post,[8] many studies have confirmed this hypothesis[6,7,11-13] while others have not.[14-16]
Evidence of a kindling effect was not found in this study. Despite the BD group's having presented with significantly more MDEs than the MDD group, the LCU scores between the two groups did not differ statistically significantly. If a kindling effect were evidenced by this study's results, the LCU scores of the BD group would have been expected to be statistically significantly lower. A scatter plot was performed to look for any inverse relationship between the number of previous MDEs and the severity of the LCU score but no clear correlations were seen (Fig. 1).
Despite limitations, this study contributes to other studies about ALEs as precipitants for MDEs. It further contributes by comparing two mood disorders in this regard, namely MDD and BD. The limitations are that the sample size is relatively small and that the RLCQ did not capture all participants' perceived ALEs accurately. The latter issue lead to the researchers' assigning a score, as set out in the method, which may differ from a score another investigator would assign. The fact that the researchers had to do this indicates an inadequacy in the RLCQ.
Conclusions
This study, in keeping with many previous studies, has found that ALEs are common in the 6 months before an MDE, and this is so for both MDD and BD. This study did not find a differential response to ALEs between participants suffering from MDD and BD. Nevertheless, in this study population, individuals with BD were more likely than participants with MDD to experience work-related ALEs as a precipitating factor for a current MDE. The notion of a kindling effect could not be supported by the outcome of this study. Finally, because some study participants experienced ALEs not accounted for by the RLCQ, a more comprehensive assessment instrument may be more appropriate for similar studies.
Acknowledgements. We are grateful to the following people for their assistance during this project: Ms J Jordaan and Dr M Graham from the Department of Statistics, University of Pretoria, Mrs M A Mabena (Weskoppies Hospital), Dr N Soe, (Tshwane District Hospital), Dr H Tanna (Steve Biko Academic Hospital), Dr G Grobler (Steve Biko Academic Hospital), Dr S H Mansoor (Tshwane District Hospital), Dr L P Steenkamp (Denmar Psychiatric Hospital), Dr J Bezuidenhout (Vista Clinic), and Dr M Henning (Denmar Psychiatric Hospital).
References
1. Horesh N, Klomek AB, Apter A. Stressful life events and major depressive disorders. Psychiatry Res 2008;160(2):192-199. [http://dx.doi.org/10.1016/j.psychres.2007.06.008] [ Links ]
2. Agid O, Kohn Y, Lerer B. Environmental stress and psychiatric illness. Biomed Pharmacother 2000;54:135-141. [http://dx.doi.org/10.1016/S0753-3322(00)89046-0] [ Links ]
3. Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol 1997;48:191-214. [http://dx.doi.org/10.1146/annurev.psych.48.1.191] [ Links ]
4. Moerk KC, Klein DN. The development of major depressive episodes during the course of dysthymic and episodic major depressive disorders: A retrospective examination of life events. J Affect Disord 2000; 58:117-123 [ Links ]
5. Kendler KS, Krakowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry 1999;156:837-841. [http://dx.doi.org/10.1176/ajp.156.6.837] [ Links ]
6. Mitchell PB, Parker GB, Gladstone GL, et al. Severity of stressful life events in first and subsequent episodes of depression: The relevance of depressive subtype. J Affect Disord 2003;73:245-252. [ Links ]
7. Corruble E, Falissard B, Gorwood P. Life events exposure before a treated major depressive episode depends on the number of past episodes. Eur Psychiatry 2006;21:364-366. [http://dx.doi.org/10.1016/j.eurpsy.2006.03.006] [ Links ]
8. Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry 1992;149(8):999-1010. [http://dx.doi.org/10.1176/ajp.149.8.999] [ Links ]
9. Bender RE, Alloy LB. Life stress and kindling in bipolar disorder: Review of the evidence and integration with emerging biopsychosocial theories. Clin Psychol Rev 2011;31(3):383-398. [http://dx.doi.org/10.1016/j.cpr.2011.01.004] [ Links ]
10. Monroe SM, Harkness KL. Life stress, the 'kindling' hypothesis and the recurrence of depression: Considerations from a life stress perspective. Psychol Rev 2005;112:417-445. [http://dx.doi.org/10.1037/0033-295X.112.2.417] [ Links ]
11. Lewinsohn PM, Allen NB, Seeley JR, Gotlib IH. First onset versus recurrence of depression: Differential processes of psychosocial risk. J Abnorm Psychol 1999;108:483-489. [http://dx.doi.org/10.1037/0021-843X.1083.483] [ Links ]
12. Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: An evaluation of the 'kindling' hypothesis. Am J Psychiatry 2000;157:1243-1251. [http://dx.doi.org/10.1176/appi.ajp.157.8.1243] [ Links ]
13. Ormel J, Oderhinkel AJ, Brilman EI. The interplay and etiological continuity of neuroticism, difficulties, and life events in the etiology of major and subsyndromal, first and recurrent depressive episodes in later life. Am J Psychiatry 2001;158:885-891. [http://dx.doi.org/10.1176/appi.ajp.158.6.885] [ Links ]
14. Hlastala SA, Frank E, Kowalski J, et al. Stressful life events, bipolar disorder and the 'kindling model'. J Abnorm Psychol 2000;109:777-786. [http://dx.doi.org/10.1037/0021-843X.109.4.777] [ Links ]
15. Swendson J, Hammen C, Heller T, et al. Correlates of stress reactivity in patients with bipolar disorder. Am J Psychiatry 1995;152:795-797. [http://dx.doi.org/10.1176/ajp.152.5.795] [ Links ]
16. Dienes KA, Hammen C, Henry RM, et al. The stress sensitization hypothesis: Understanding the course of bipolar disorder. J Affect Disord 2006;95:43-49. [http://dx.doi.org/10.1016/j.jad.2006.04.009] [ Links ]
17. Ravindran AV, Griffiths J, Waddell C, Anisman H. Stressful life events and coping styles in relation to dysthymia and major depressive disorder: Variation associated with alleviation of symptoms following pharmacotherapy. Prog Neuro-Psychopharmacol Biol Psychiatry 1995;19:637-653. [ Links ]
18. Miller MA, Rahe RH. Life changes scaling for the 1990s. J Psychosom Res 1997;43(3):279-292. [http://dx.doi.org/10.1016/S0022-3999(97)00118-9] [ Links ]
19. Wang J. Work stress as a risk factor for major depressive episode(s). Psychol Med 2005;35:865-871. [http://dx.doi.org/10.2105/AJPH.2006.104406] [ Links ]
 Correspondence:
Correspondence:
R A van Schoor
robyn.vanschoor@up.ac.za














