Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Psychiatry
On-line version ISSN 2078-6786
Print version ISSN 1608-9685
S. Afr. j. psyc. vol.21 n.1 Pretoria Feb. 2015
http://dx.doi.org/10.7196/sajp.609
ARTICLE
Needs-based gap analysis for service transformation in the Eastern Cape
K SukeriI; O Alonso-BetancourtIII; R EmsleyII
IMB ChB FCPsych (SA); Department of Psychiatry, Faculty of Medicine and Health Sciences, Walter Sisulu University, Mthatha, South Africa
IIMB ChB DCH MMed (Psych) FCPsych (SA) DMed DSc; Department of Psychiatry, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg, Cape Town, South Africa
IIIMD PhD FCPsych (SA); Department of Psychiatry, Faculty of Medicine and Health Sciences, Walter Sisulu University, Mthatha, South Africa
ABSTRACT
OBJECTIVES: Part I of this research article presents a needs-based analysis for the management of schizophrenia, bipolar mood disorder and major depression for the Eastern Cape (EC) Province, South Africa. This part of the research paper focuses on quantifying human resources and bed needs for these three severe mental illnesses. Human resource expenditure is calculated for nursing staff at acute, ambulatory and medium-to-long-stay services. A further objective was to conduct a gap analysis for human resources and beds for the EC in order to assist mental health planners in the commissioning of services.
METHODS: Data from previous research conducted in the province, and international and national epidemiological studies were utilised to quantify the requirements for human resources (psychiatrists, medical officers/registrars, psychologists, nurses, occupational therapists and social workers) and beds for acute, medium-to-long-stay and ambulatory services at provincial and regional levels, to provide mental healthcare. The authors focused on three of the eight priority conditions set by the World Health Organization. A target coverage rate of 80% was used in all calculations. A gap analysis was conducted to demonstrate deficits and excesses, utilising available data on human resources and beds available in the province.
RESULTS: The results showed that the districts of Alfred Nzo and Ukhahlamba have no human resources or beds for the provision of mental health services. The province has a deficit of 23 psychiatrists and 243 nurses trained in psychiatry, and an oversupply of 486 other nurses. The results also clearly demonstrated an inequitable distribution of resources in the province.
CONCLUSIONS: This is the first study that has provided detailed estimates of human resource and bed deficits in the EC. The study demonstrates that the areas of greatest need in terms of bed and human resource requirements are in the eastern regions of the province, which includes the former homelands of the Transkei and Ciskei. This study will assist provincial mental health planners/commissioners in developing an equitable mental health delivery programme.
The central decision for [all organisations] is, what is thebest way to portion out available resources ...to meet all the demands - the needs - that compete for them ... the most effective way is to make needs assessment the first stage in planning. (Bella Ruth Witkin)[1]
In the development of a mental health plan, it is imperative to determine 'need', the nature and extent of the need, and how to measure and plan to meet this need. Kaufman and Stakenas[2] defined a needs assessment as 'a formal systematic attempt to determine and close the more important gaps between "what is" and "what should be".'
Needs assessments are conducted to assist planners to 'identify and select the right job before doing the job right.'[2] A needs-based approach is independent of past use and therefore allows for equitable and efficient resource allocation. Dreesch et al.[3]draw attention to the limitations of a needs-based approach, which include projection of unattainable staff requirements, extensive data collection and norms updating as technology advances.
The World Health Organization (WHO)[4] states that the needs of the population can be determined by utilising prevalence and incidence studies, and determining what communities identify as problems.
The first national epidemiological survey in South Africa (SA) was conducted between 2003 and 2004.[5] This study surveyed 619 house holds in the Eastern Cape (EC) and determined 12-month and life time prevalence estimates for certain classes of mental illnesses. These classes were anxiety disorders, mood disorders (major depressive disorder) and substance use disorders.
In 2008, the WHO launched the Mental Health Gap Action Programme (mhGAP).[6] This programme set eight priority conditions, which included epilepsy, schizophrenia and other psychotic disorders, depression, dementia, suicide, illicit substance use disorder and mental disorders in children. The SA study included two of these, viz. depression and substance use disorders.[5]
Risk factors provide a fertile substrate for the predisposition to mental illness and therefore affect prevalence rates. The EC has several high-risk factors, including an overall HIV prevalence rate of 16.8%, compared with 7.9% for the Western Cape.[7] The HIV prevalence rate in the EC among antenatal attendees was 29.9%.[8] In 2010, there were 781 713 and 62 029 new cases of HIV and TB, respectively, reported in the province.[8] The districts with the highest HIV prevalence rates are located in the eastern region of the province, with an average prevalence rate of 31.1%.[9]
Poverty is another risk factor, with the average household income of USD3 340/annum (7 June 2010), making the province a low-to-middle-income region according to the World Bank.[10] The further east a household is, the poorer it is (low-to-middle income: USD2 360/annum) and the further west a household is, the wealthier it is (upper-to-middle income: USD4 650/annum).[10] Westaway[11] observed that poverty in the EC is worse now than at the dawn of liberal democracy, and suggested that this is owing to a renewal of segregationist policies.
The province has higher than national murder and substance-related crime rates. The provincial murder rate stands at 39/100 000 (national figure 32/100 000) and has a drug-associated crime rate of 293/100 000 (national figure 232/100 000).[9]
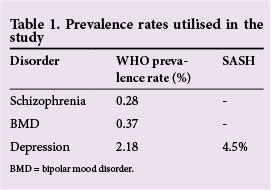
The effect of these factors is reflected in the prevalence rate for depression, where the SA Stress and Health (SASH) study rate is almost double that of the WHO figure.[5, 12]
This research article focuses on a needs analysis for the treatment of three severe psychiatric conditions, viz. schizophrenia, bipolar mood disorder and depression. Prevalence rates for these disorders are readily available from WHO studies and a national epidemiological study.[5,12] These disorders have been rated as having the highest disability from the eight priority conditions set by the WHO.[6]
Methods
The needs analysis was determined as per the norms manual of severe psychiatric conditions, and comprised the following steps.[13] The formula set out by Scheffler et al.,[12] albeit more recent than the norms manual for severe psychiatric conditions, was not utilised as it required substantial adjustment.
- Step 1: The population for which services are to be planned was determined. This article concerns the adult population of the EC, i.e. over the age of 18 years.[14]
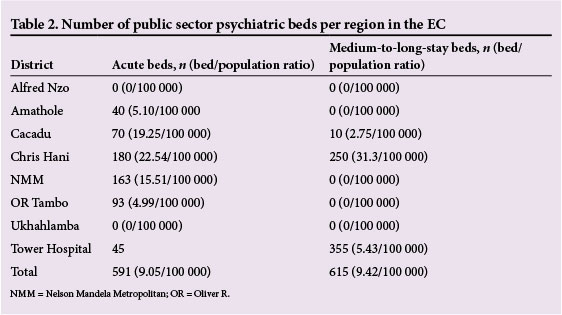
- Step 2: Current service provision in the province was determined. A detailed analysis was presented in previous research by the authors.[15] The results presented here are for staff and bed distribution at provincial and regional level. (Tower Hospital provides long-term care for the entire province.)
- Step 3: Prevalence rates for the three mental disorders were determined. Prevalence rates for schizophrenia and bipolar mood disorder were obtained from Scheffler et al. [12] The prevalence rate for depression was obtained from the SASH study (Table 1).[5] These prevalence rates were utilised to determine the expected number of cases in the entire population (prevalence rate x total population). The WHO has set a target coverage of 80% for schizophrenia and bipolar mood disorder for low-to-middle-income countries.[12] Although the target coverage for major depression was set at 33% by the WHO, the authors increased this to 80%, as the condition is easily managed at primary healthcare level. Utilising this target coverage, the expected number of severe cases was estimated.
- Step 4: Human resource requirements were based on this estimate. These requirements were calculated for ambulatory, acute, medium-to-long-stay service and management positions. The formula is set out in the norms manual for severe psychiatric conditions.[13]
- Step 5: Service delivery models were based on acute, medium-to-long-stay and ambulatory services. To determine outpatient needs or ambulatory services, the following formula was applied:
prevalence x target population coverage x number of visits per year
Utilisation rates were calculated as total visits/total population. Daily patient visits were determined as total outpatient visits/ total number of working days. In 2010 there were 257 working days. The above methodology was also applied to each region of the EC.
- Step 6: Human resource costing was calculated for nursing staff per service requirement. The category 'professional nurse grade 1 with a specialty in psychiatry' was utilised. This is a salary level 9 post, the annual cost of which is R320 730.[16]
- Step 7: Staff and bed deficits and excesses were calculated at provincial and district levels.
Results
The adult population of the EC (3 410 975)[14] was utilised in all calculations, except for public sector psychiatric beds where the entire population (6 527 747)[14] was used, as this sector provides services for adults, children and adolescents.
Bed and human resource distribution (2010) in the EC is demonstrated in Tables 2 and 3, respectively. Table 4 shows the target population at 80% coverage and Table 5 depicts the expected ambulatory service need.
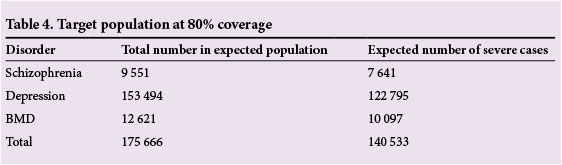
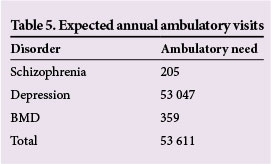
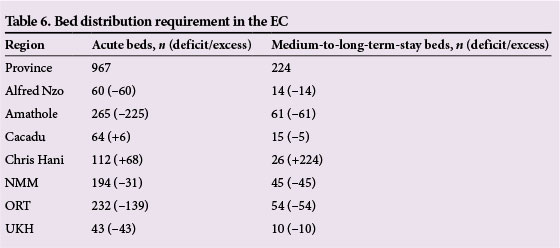
The EC had a utilisation rate of 0.02/ person/year and daily patient visits were estimated at 209 persons/day. Table 6 shows bed requirements for acute, medium- and long-stay beds provincially and per region.
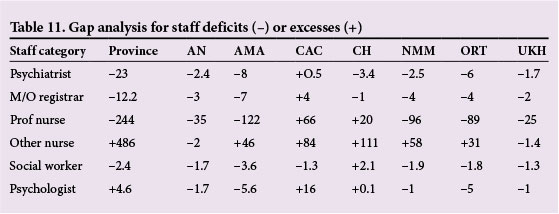
Human resource requirements are outlined per category of staff and service for each region and the province, for ambulatory, acute and medium-to-long-stay services (Tables 7 - 9). Human resource costs were calculated for nursing staff for the provision of acute, ambulatory and medium-to-long-stay services (Table 11). Table 11 shows the gap analysis for staff deficits (-) or excesses (+) at both provincial and district levels. Note that columns may not tally due to rounding of estimates.
Results from Table 6 depict a need for 967 acute beds for the management of three severe mental illnesses at 80% coverage. There are 591 acute beds in the province; a shortfall of 376 beds. The shortfall and requirement of beds is mainly in the eastern regions, including the Alfred Nzo, Amathole, OR Tambo and Ukhahlamba districts. The need for acute beds in these regions is ~48% of the total provincial acute bed requirement.
The results demonstrate an oversupply of medium-to-long-stay beds provincially, particularly in the Chris Hani district. This will significantly affect the redistribution of beds in the province.
A total staffrequirement of 705 (21/100 000 population) is required for service provision for three severe psychiatric conditions at 80% coverage for an adult population. This figure increases to 882 (26/100 000 population) at 100% coverage. The provincial staff number for the provision of mental healthcare for a wide spectrum of psychiatric illnesses at 100% coverage, for both adults and children, is 924 (14/100 000 population) (Table 3).
There is a province-wide need for psychiatrists, with the greatest need again in the eastern regions (~80% of the provincial need). The Alfred Nzo district requires the services of 2.4 psychiatrists (Table 11). The current psychiatrist/population ratio is 0.25/100 000 population.[15] An additional 23 psychiatrists increases this ratio to 0.6/100 000 population.
An analysis of the nursing category shows a need for an additional 244 nurses trained in psychiatry. The greatest need is in the provision of acute mental health services, hence the high salary costs for this service level (Table 10). This increased need may be met with the training of the general nursing category nurses. This is discussed further in a subsequent research article.
Discussion
Although the province has an oversupply of medium-to-long-stay beds, the formula prescribed by Flisher et al.[13] implies a move from institutional care to the development of community residential care. The public mental health sector in the province is dependent on institutional care, as community residential facilities are provided by non-governmental organisations and one public-private partnership.
It is evident that there is dire staff shortage in all categories except psychologists. In addition, there is inequitable distribution of staff to meet requirements in the provision of a minimal service at 80% coverage. The high number of psychologists could be owing to the fact that there are four training institutions for psychologists in the province.
Psychiatrists in the province do not only provide clinical services; they are involved in education, research, and outreach and inreach services. This increases the demand for this category of staff. Currently there are no psychiatrists in the Alfred Nzo district; this service is provided for by psychiatrists in the OR Thambo district, which at the time of the study had three psychiatrists.
An additional 23 psychiatrists increases the per population ratio to 0.6/100 000 in the province; however, this still falls short of the 1.2/100 000 population recommendation by the WHO.[17]
The calculated expenditure for human resource requirements appears astronomical for the treatment of three severe psychiatric conditions. However, it must be noted that nurses who provide acute psychiatric services would also provide ambulatory services in the regions where they work, for a wide spectrum of mental illnesses. This costing also includes commuted overtime, 25% pension contribution by the state, medical aid and bonus payments - incentives that are essential in staff retention. With the reduction in institutional care, the province would decrease costs incurred in salaries for this category of staff.
This research clearly demonstrates that the provincial mental health plan has to focus on the eastern regions; there are deficits in beds and human resources in these districts. The continued unmet need of the populations in these districts will increase the burden on services in other regions of the province. Strategies to improve this need will be discussed in a subsequent research article.
Study limitations
The authors focused only on three of the eight priority conditions set by the WHO. An inclusion of all eight conditions would certainly provide a detailed need and gap analysis. The results presented here may therefore be an underestimate of human resource and bed shortages. Nevertheless, this research provides a resource-limited province with an overview of needs that should be addressed.
A second limitation was the lack of province-specific prevalence data. This would affect the estimation of need within the general population. However, the lack of epidemiological data is not limited to the EC but applies nationally as well.
A third limitation was the exclusion of the child and adolescent population. The province does not have a child and adolescent psychiatric service, and a need and gap analysis would provide the basis for planning this service. However, there are no national epidemiological data in this population, which would impede a needs analysis.
Conclusion
This study provides the first detailed estimates of human resource and bed deficits and excesses in the EC. The analysis conducted here provides provincial policymakers with an understanding of the regions within the province with the greatest need for mental health services. This article allows for the planning and equitable redistribution of beds and human resources to meet the requirements for an efficient mental health service as set out in SA's national mental health policy framework and strategic plan.[18]
Acknowledgement. This study was sponsored by a Discovery Foundation Academic Fellowship Award.
Contributors. K Sukeri was the principal investigator, conducted the literature review, designed the study, collated the data, did the data analysis and wrote the draft manuscript. O Alonso-Betancourt and R Emsley supervised the study and contributed to the study design and the final drafting of the manuscript.
References
1. Witkin BR, Altschuld A. Planning and Conducting a Practical Needs Assessment: A Practical Guide. Newbury Park, CA: Sage Publications (Thousand Oaks), 1995. [ Links ]
2. Kaufman R, Stakenas RG. Needs assessment and holistic planning. Educational Leadership 1981:612-616. http://www. ascd.org/ASCD/pdf/journals/ed_lead/el_198105 (accessed October 2010). [ Links ]
3. Dreesch N, Dolea C, Dal Poz MR, et al. An approach to estimating human resource requirements to achieve the millennium development goals. Health Policy and Planning 2005;20(5):267-276. [http://dx.doi.org/10.1093/heapolczi036] [ Links ]
4. World Health Organization. Mental Health Policy, Plans and Programmes. Mental Health Policy and Services Guidance Package, 2005. http://who.int/mental_health/policy/services [ Links ]
5. Herman AA, Stein DJ, Seedat S, Heeringa SG, Moomal H, Williams DR. The South African Stress and Health Study: 12 month and life time prevalence of common mental disorders. S Afr Med J 2009;99(5):339-334. [ Links ]
6. World Health Organization. mhGAP: Mental Health Gap Action Programme: scaling up care for mental, neurological and substance use disorders, 2008. http://who.int/mental_health/evidence/ [ Links ]
7. HIV and AIDS in South Africa. http://avert.org/south-africa-hiv-aids-statistics.htm (accessed February 2011). [ Links ]
8. South African Department of Health. The National Antenatal Sentinel HIV and Syphilis Prevalence Survey in South Africa, 2010. Pretoria: Department of Health, Republic of South Africa, 2010. [ Links ]
9. Eastern Cape Socio-Economic Consultative Council (ECSECC). Eastern Cape Development Indicators, 2012. Bhisho: ECSECC, 2012. [ Links ]
10. The World Bank. How we classify countries. http://data.worldbank.org/about/country-classifications (accessed November 2010). [ Links ]
11. Westaway A. Rural poverty in the Eastern Cape Province: Legacy of apartheid or consequence of contemporary segregationism? Development South Africa 2012;29(1):115-125. [ Links ]
12. Scheffler RM, Bruckner TA, Fulton BD, et al. Human resources for mental health: Workforce shortages in low- and middle-income countries. Geneva: World Health Organization, 2011. [ Links ]
13. Flisher AJ, Lund C, Muller L, et al. Norms and Standards for Severe Psychiatric Conditions. A report submitted to the Department of Health, tender no. GES 105/96-97. Cape Town: Department of Psychiatry, University of Cape Town, 1998. [ Links ]
14. Statistics South Africa. Community Survey 2007. http://www.statssa.gov.za/publications/0301/p0301.pdf (accessed November 2010). [ Links ]
15. Sukeri K, Alonso-Betancourt O, Emsley R. Staff and bed distribution in public sector mental health services in the Eastern Cape, RSA. S Afr J Psychiatr 2014;20(4):160-165. [http://dx.doi.org/10.7196/SAJP.570] [ Links ]
16. South African Department of Public Service Administration. Salary scales for nurses. http://dpsa.gov.za (accessed May 2014). [ Links ]
17. Bruckner TA, Scheffler RM, Shen G, et al. The mental health workforce gap in low- and middle-income countries: A needs based approach. Bull World Health Organ 2011;89:184-194. [ Links ]
18. South African Department of Health. National Mental Health Policy Framework and Strategic Plan 2013 - 2020. Pretoria: Government Printer, 2012. [ Links ]
 Correspondence:
Correspondence:
K Sukeri (ksukeri@telkomsa.net)