Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Psychiatry
versão On-line ISSN 2078-6786
versão impressa ISSN 1608-9685
S. Afr. j. psyc. vol.20 no.1 Pretoria Jan./Mar. 2014
ARTICLE
Designing an educational programme in mental health for general practitioners in South Africa
R J NicholI; B de KlerkII; M M NelIII; G J Van ZylIV; J F HayV
IMB ChB, DTM&H, DPH, MMed (Psych), PhD (HPE). Department of Psychiatry, School of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIMB ChB, DTM&H, DPH, DOH, PhD (HPE). Department of Community Health, School of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIPhD. Department of Health Science Education, School of Health Sciences, University of the Free State, Bloemfontein, South Africa
IVMB ChB, MFamMed, DHA, DPH, MBA, PhD (HPE). Dean, School of Health Sciences, University of the Free State, Bloemfontein, South Africa
VHDE (Guidance), PhD. Programme Director, Department of Initial Teacher Education, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: With the new Mental Health Care Act in use, additional demands will be placed on general practitioners to provide adequate care for mental health patients. The College of Psychiatry of the Colleges of Medicine of South Africa awards a Postgraduate Diploma in Mental Health (PGDipMH) to medical doctors, but there is no standardised formal tuition or curriculum available to potential candidates.
OBJECTIVES: A study was undertaken to design a postgraduate programme using a six-step process to assist medical practitioners in preparing for the PGDipMH.
METHODS: The Delphi research method, a nominal group technique for developing forecasts and trends based on the collective opinion of knowledgeable experts, was used. Data, obtained by means of closed items in a questionnaire, were analysed, and the opinions and ideas of the expert respondents were used to adapt the formulated set of criteria for each subsequent round of Delphi. This process was repeated until 80% consensus or stability had been reached. After the last round, a framework and final set of criteria were compiled.
RESULTS: The preferred mode of teaching was online distance learning utilising electronic learning and limited formal learning. The content of the curriculum was based on the findings of the Delphi study experts. The programme as a complete entity contains six steps.
CONCLUSIONS: Using the recommendations and findings of the Delphi panel, a comprehensive programme was developed, which shows an appreciation for the interfaces between the different role-players (the patient/so-called mental healthcare user and the doctor as learner), outcomes-based education and distance learning.
Historically, madness has always been associated with institutionalisation. Since the Middle Ages, people who were mentally ill were removed from society, often up until they died.[1] Generally, psychiatric patients were regarded as extremely dangerous, with society in need of protection from them. In South Africa (SA), the first hospital to cater specifically for mentally deranged persons was established in 1711.[2] This stigma is still prevalent today, although perhaps to a lesser degree.
Since the middle of the last century, psychotropic drugs have been developed, which have allowed for the effective management (but not cure) of some of the most disabling psychiatric conditions.[3] As a result, patients can not only be sedated effectively when necessary, but also helped to cope with mental illness.[4] Deinstitutionalisation has become the order of the day and long-term institutionalisation is only utilised in chronic patients who are unable to function in the community.[5]
SA is known to have a particularly high lifetime prevalence of common psychiatric disorders and substance abuse disorders.[6] Utilising the 'Free State Model',[7] psychiatric patients in the Free State Province are treated as outpatients in clinics close to their homes, rather than being confined to the Free State Psychiatric Complex (formerly Oranje Hospital) for weeks or months on end. Although many acutely psychotic patients are admitted to hospital, they are discharged into the community as soon as their condition starts to enter remission - a far more humane approach for psychiatric disease. The onus to care for these patients in the community, to ensure that they do not relapse and need subsequent admission to hospital, rests with medical practitioners,[8] who should also be able to diagnose and treat (or refer) new cases of psychiatric conditions.
Postgraduate training in psychiatry has been available at SA medical schools for many years. Despite this, there are only 676 psychiatrists registered in SA,[9] many of whom work and live in other countries. Our current population is estimated to be ~50.59 million (2010 mid-year estimate), equating to less than one psychiatrist per 75 000 people. If these statistics are evaluated according to access to service, 208 000 people have access to one of the 91 state psychiatrists, while there is one private psychiatrist for every 12 000 people able to afford private care (there are 234 private psychiatrists in SA). This demonstrates the great need for other medical doctors to be involved in the field of mental health.
The new Mental Health Care Act passed in 2004 placed additional demands on mental healthcare workers, including general practitioners (GPs), to provide adequate care to patients.[10] In the developing world, primary healthcare is needed to meet the medical needs of the community, but GPs have fewer consultants to advise them, as there is a trend of many specialists leaving Africa to work in 'the apparent safety of the West.[11] Medical schools are forced to opt for localised practical courses rather than internationally acceptable scientific training in the discipline (e.g. in Malawi[12]).
Judging by the nature or quality of referrals to tertiary centres, many medical practitioners in SA have insufficient knowledge in the field of psychiatry. Some would like to increase their expertise, but do not wish to specialise in the area (evident from personal dialogue with doctors at workshops and conferences). The College of Psychiatry (Colleges of Medicine of South Africa) offers a Postgraduate Diploma in Mental Health (PGDipMH). There is, however, no standardised formal tuition or curriculum (other than a list of topics) available to potential candidates who wish to sit the examination for this diploma. Non-specialist doctors are required to have spent at least 3 months working in a given academic psychiatric hospital, or at least 6 months working in the psychiatric ward of nine selected general hospitals in southern Africa, under the supervision of a psychiatrist. Doctors who have been formally mentored by a registered psychiatrist on at least ten cases may also be eligible to sit the examination. Medical doctors who do not have direct access to a registered psychiatrist are therefore automatically disqualified from applying to the PGDipMH, even though they may frequently manage psychiatric patients at a primary healthcare level.
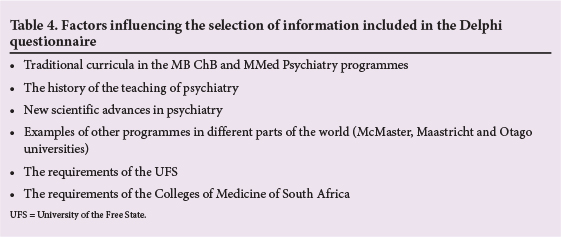
Over a 14-year period (1997 - 2011), 360 candidates wrote the PGDipMH examination, and only 279 (78%) were successful (Table 1). From two different perspectives, the College obtained excellent results in certain examination centres, such as in May 1997 and October 1998, but less than satisfactory results in May 2004 and October 2005. Considering the statistics presented in Table 1, there is a need for certain candidates to receive more thorough tuition; however, this need is not catered for in the PGDipMH.
Here we report on a study undertaken to design a postgraduate programme to assist medical practitioners in preparing for the PGDipMH. A framework was established to allow practitioners requiring additional tuition to embark on formal postgraduate training on a part-time basis. The programme was designed to support the requirements of the National Qualifications Network (NQF), the Colleges of Medicine of South Africa and the Professional Boards, utilising a mode of blended learning, including face-to-face contact sessions, directed learning and electronic (e-) learning.
Methods
The study was approved by the ethics committee, Faculty of Health Sciences, University of the Free State (UFS) (ETOVS 89/06).
A Delphi process was used - a nominal group technique for developing forecasts and trends based on the collective opinion of knowledgeable experts. Experts were individuals possessing specific levels of knowledge and expertise related to the core content. Their academic fields included psychiatry, family medicine, medical education, e-learning and government legislature.
Closed items in the Delphi study, dealing with curriculum content, were derived from multiple sources. Open-ended questions were used to obtain opinions and ideas put forward by the panellists.[13] Recommendations made were incorporated into the questionnaire for successive rounds and hence submitted to other respondents for further comment. This process was repeated until 80% consensus or stability had been reached. After the final round, a set of criteria was compiled, which served to develop a framework for the programme.
Since the PGDipMH is also intended to cater for medical doctors in primary healthcare settings in rural regions, the consensus of the Delphi process was that the most appropriate mode of teaching was online distance learning (ODL) utilising e- and mobile (m-) learning.[14] An advantage of e- and distance learning is these modes of tuition make it possible for doctors to learn in their own environment, without the disruption of having to spend too much time away from their practices.
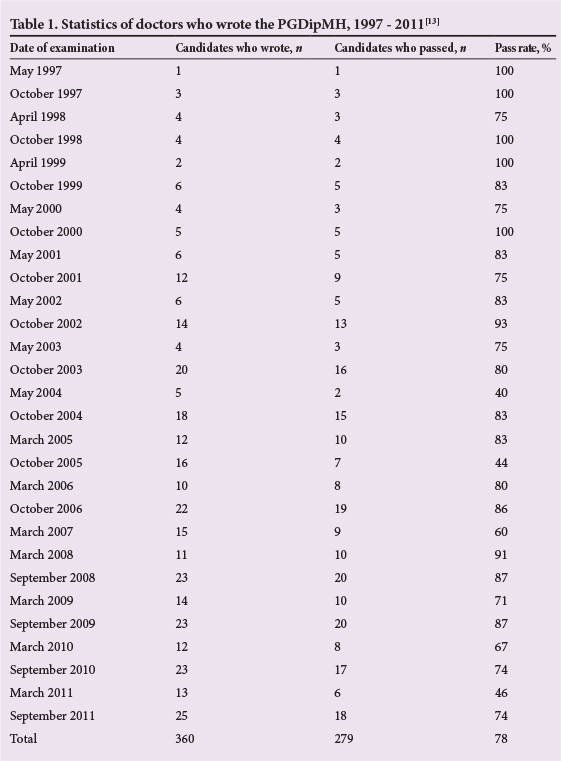
The programme was designed in six steps (Table 2), similar to the six-step approach to curriculum development described by Kern et al.[15]
Programme design
Step I: Identification of individual needs of the doctor as learner and the mental healthcare user (patient)
It was identified that the study of mental healthcare, including psychiatry, should fixate around the needs of the patient (also known as the mental healthcare user, although this term may include the person's next of kin, a person authorised to act on their behalf, an appointed administrator or an executor of the person's estate in the event that they are deceased). Further, it should include comprehensive knowledge on psychiatry and psychiatric illness, the management of psychiatric conditions in primary healthcare, and methods relating to the primary prevention of mental illness in psychiatric patients (which also affect their families).
Patient-centred learning
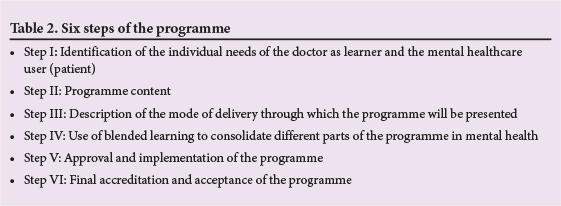
It was identified that learners (doctors) need to be encour aged to make use of patient-centred learning and link conditions under discussion with patients in their practices or the hospitals in which they serve their communities. Refer to Table 3 for a summary of the identified mental health needs of the community. Using consenting patients as 'study material, learners would have to detect certain sympt oms and discuss these with their tutors or the group, and describe the efficacy and side-effect profile of the medications that patients receive. Thus, patients who are difficult to manage would benefit from 'tertiary-level consultations', and the learners would gain more knowledge on the topic. Students would write case reports concerning patients with certain conditions and include this in their portfolios, which would be assessed at predetermined dates. Students would have to appreciate the effect of the physical and cultural environment on patients' conditions.
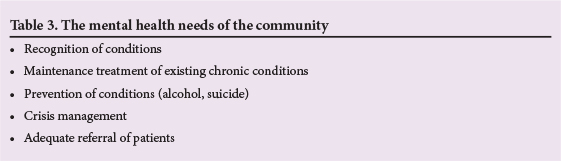
Step II: Programme content Various information sources (Table 4) were used to structure the Delphi questionnaire. After the final round of the Delphi process, the curriculum was structured into ten modules as such:
• Module 1: Introduction to psychiatry. In this 2-day seminar, students would receive face-to-face tuition from lecturers of the Department of Psychiatry, UFS, which would be intense and articulate with the learners' undergraduate knowledge. Additional material for a more indepth study of neuro-anatomy and -physiology would be made available. Clinical evaluation methods of common psychiatric conditions would be demonstrated. Students would work through specific case reports before emailing their answers to the Department of Psychiatry within 7 working days of receipt of the tutorials.
• Module 2: Chronic common psychiatric conditions (part 1) - schizophrenia. Tuition for this and all other modules (except module 1) would be presented using ODL.
• Module 3: Chronic common psychiatric conditions (Part 2) - mood disorders
• Module 4: Chronic common psychiatric conditions (part 3) - anxiety disorders
• Module 5: Child psychiatry (part 1)
• Module 6: Child psychiatry (part 2)
• Module 7: Forensic psychiatry
• Module 8: Addiction disorders
• Module 9: Geriatric psychiatry
• Module 10: Introduction to cognitive behaviour therapy.
The didactic content of modules 1 - 10 would be presented as lectures using Powerpoint presentations, video-clips, illustrations, handouts and podcasting as appropriate to enhance the lecture; after which time, these would be made available on a dedicated website. With the exception of module 1, all other modules would be presented using ODL, complemented by the use of chat rooms. Students would be encouraged to use iPods and personal digital assistants (PDAs) as part of the m-learning, and blogs which would be monitored by those presenting the programme.
Step III: Description of the mode of delivery of the programme
The programme would not only cover the scope of mental healthcare required for the PGDipMH, but would also be comprehensive enough to accommodate the logistics required to present a modern curriculum harnessing modern technology for ODL.
Step IV: Use of blended learning to consolidate different parts of the programme
According to Welch,[16] a blended learning model incorporates a variety of delivery styles and accommodates different organisational needs to achieve the most effective knowledge transfer. Accordingly, as for step III, the programme would not only provide the syllabus needed to cover the scope of mental healthcare, but would also be comprehensive enough to accommodate a modern curriculum harnessing modern technology for ODL.
Programme format and time frame
An essential part of constructing a programme is to ensure that blended learning can be facilitated. Using the statements of the respondents in the Delphi process, the consensus was to adhere to the following principles:
• The time frame for the programme would be 2 years.
• The first academic year would contain four (compulsory) modules.
• In the second academic year, students would have to select three modules from a list of six to be presented in that year.
• Students would be required to pass the first academic year before proceeding to the second year.
• Students who wish to exit the course after one year would have to pass an oral examination in order to receive a short learning course certificate.
• Students would be assessed using tutorials and worksheets.
• There should be a restriction on the number of students who would be allowed to enrol for the course per academic year.
• Only medical practitioners registered with the Health Professions Council of South Africa would be accepted for enrolment in the programme.
• After receiving each formal lecture, learners would also receive an online tutorial relating to the subject matter. Learners would have 7 working days in which to return their 'homework' online. If the tutorial was successfully completed (>70% of answers correct), the student would be asked to form part of the chat room session; otherwise, students would have 3 working days in which to make corrections (then, if >70% of the homework was correct, the student would be allowed to partake in the chat room session on the topic). The rationale for the 70% boundary would be to ensure that students have a working knowledge of the topic, and do not participate in the chat room session unprepared.
Steps V and VI (Table 4) will not be discussed in this article, as they remain to be implemented. The theoretical programme as a complete entity, containing all six steps, is demonstrated in Fig. S1 (supplementary material, available in the online version of this article).
Conclusion
Using the recommendations and findings of the Delphi panel and other sources (literature and personal experience), a comprehensive programme was designed (in theory) to train doctors at generalist level to provide a high quality of care. Appreciation was given for the interfaces between the different role-players, the central role of outcomes-based education and the dynamics relating to psychiatric patients and their care. The characteristics of this programme would allow adult learners to study further in the fields of mental health and psychiatry, in order to enhance service delivery to their patients.
The process of obtaining approval and accreditation for this programme still needs to be undertaken. The process of taking a concept and transforming it into a framework for a fully accredited diploma programme (the PGDipMH) has been described here using the aforementioned six steps. Once implemented, it is hoped that doctors who complete the programme will be more knowledgeable in the field of psychiatry and in a better position to serve the mental healthcare needs of their communities.
References
1. Porter R. Madness - a briefhistory. Oxford: Oxford University Press, 2002. [ Links ]
2. Emsley R. Focus on psychiatry in South Africa. Br J Psychiatry 2001;178:382-386. [ Links ]
3. Ketter TA, Wang PW, Nowakowska C, Marsh WK New treatment options for bipolar disorders. Acta Psychiatrica Scandinavica 2004;110(Supp1 42):18-33. [ Links ]
4. Shorter E. A History of Psychiatry - From the Era of the Asylum to the Age of Prozac. New York: John Wiley and Sons, 1997. [ Links ]
5. Kaplan H, Sadock B. Synopsis of Psychiatry: Behavioral Sciences, Clinical Psychiatry. 8th ed. Baltimore: Lippincott, Williams & Wilkins, 1998. [ Links ]
6. Stein D, Seedat S, Herman A, et al. Lifelong prevalence of psychiatric disorders in South Africa. Br J Psychiatry 2008;192:112-117. [ Links ]
7. Gagiano CA, Venter JC. Psychiatric nursing: The ideal and the practice. Nursing RSA 1992;7(8):34-35. [ Links ]
8. Van't Hoff E, Stein D, Marks I, et al. The effectiveness of problem solving therapy in deprived South African communities. BMC Psychiatry 2011;11:156. [ Links ]
9. Janse van Rensburg B. SESIG Report 2008 - 2010. Johannesburg: SASOP, 2011. [ Links ]
10. Republic of South Africa. Mental Health Care Act 2002. Government Gazette, Vol. 449, No. 17. Cape Town: Government Printer, 2002. [ Links ]
11. Kigozi FN. Challenges to the current provision of mental health services and development of psychiatry in Africa. South African Journal of Psychiatry 2003;9(2):27. [ Links ]
12. Herzig H. Teaching psychiatry in poor countries: Priorities and needs. A description of how mental health is taught to medical students in Malawi, central Africa. Education for Health: Change in Learning & Practice 2003;16(1):32-39. [ Links ]
13. College of Psychiatry of South Africa. Statistics of Doctors who Wrote the Diploma in Mental Health 1997 - 2007. Johannesburg: College of Psychiatry of South Africa, 2011. [ Links ]
14. Bezuidenhout MJ. National Standards for the Accreditation of Undergraduate Medical Students and Training in South Africa. Unpublished MHPE thesis, Division of Educational Development, Faculty of Health Sciences, University of the Free State, Bloemfontein, 2002. [ Links ]
15. Kern DE, Thomas PA, Hughes MT, eds. Curriculum Development for Medical Education: A Six Step Approach. 2nd ed. Baltimore: Johns Hopkins University Press, 2009. [ Links ]
16. Welch J. Training: A Critical Success Factor in Implementing a Technology Solution. New Jersey: Radiant Systems Inc., 2003. [ Links ]
Corresponding author: B de Klerk (gngmbdk@ufs.ac.za)