Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Journal of Radiology
versión On-line ISSN 2078-6778
versión impresa ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.27 no.1 Johannesburg 2023
http://dx.doi.org/10.4102/sajr.v27i1.2707
PICTORIAL REVIEW
Superior labrum anterior to posterior lesions: Part 2 - Classification with arthroscopic correlation
Peter MercourisI; Matthew MercourisII
IDiagnotic Radiologist, Lake, Smit and Partners, Gateway Private Hospital, Durban, South Africa
IIDepartment of Orthopaedic, Mitchell's Plain District Hospital, Cape Town, South Africa
ABSTRACT
The glenoid labrum deepens the glenoid fossa and allows for the attachment of the long head of the biceps tendon and glenohumeral ligaments, contributing to the stability of the glenohumeral joint. The superior labrum is a common site of labral injury. The acronym SLAP (superior labrum anterior to posterior or anteroposterior) lesion was introduced by Snyder and colleagues in 1990 to describe superior labral tears based on arthroscopic evaluation. This original classification has since been expanded, and there are currently 10 types of SLAP lesions. The article will describe and illustrate the 10 types of SLAP lesions by means of colour illustrations, MRI images and correlative arthroscopy images. A practical approach to the assessment of SLAP lesions will be recommended.
CONTRIBUTION: The illustrated review functions as a crucial radiological guide for both radiologists and orthopaedic surgeons. The combination of illustrations, MR and correlative arthroscopic images enhances the comprehensive understanding of labral pathology. The value of the review lies in the presentation of imaging findings and classification, coupled with findings on arthroscopy. This understanding is vital in guiding orthopaedic management for patients, ensuring appropriate treatment strategies.
Keywords: shoulder; glenoid labrum; MRI; arthroscopy; anatomic variants; SLAP lesion or tear.
Introduction
In 1985, Andrews and colleagues described superior labral injuries in throwing athletes.1 This was followed by Snyder and colleagues in 1990, who introduced the term or acronym SLAP (superior labrum anterior to posterior or anteroposterior) to describe injuries of the superior labrum and, based on arthroscopic evaluation, classified SLAP lesions of the shoulder into four types.2 Following the identification of additional SLAP tears, the original classification has been revised, and there are presently 10 types of SLAP lesions.3,4 This review pictorially illustrates the spectrum of SLAP lesions by means of colour illustrations, MRI images and correlative arthroscopy images. The clinical presentation, diagnostic and management challenges are highlighted.
Diagnostic evaluation
The clinical diagnosis of a SLAP lesion is difficult, and patients often present with non-specific shoulder pain particularly with overhead or cross-body motion. The patient may also complain of popping, clicking, catching weakness, stiffness and instability. The presentation may be acute with the mechanism of injury involving a traction injury, direct trauma to the shoulder or commonly a fall on an outstretched arm, or it may be chronic because of repetitive microtrauma secondary to overhead activity.5,6 There is no single physical test or sign that is specific for a SLAP lesion,5 and clinical assessment is further complicated by the strong association with co-existent shoulder injuries such as rotator cuff tears, Bankart lesions and glenohumeral articular damage.7
Arthroscopy remains the gold standard for diagnosis of a SLAP lesion, but MRI, particularly direct MR arthrography that involves the intra-articular administration of gadolinium-based contrast medium, has been shown to be accurate in the evaluation of the glenoid labrum.5,8
Classification
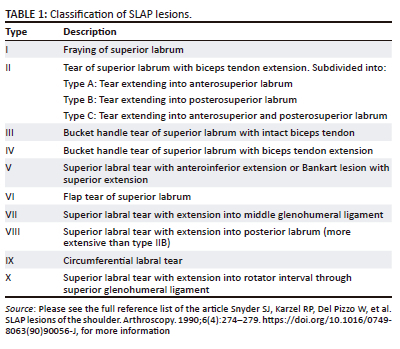
There are 10 different types of SLAP lesions, as outlined in Table 1.2,3,9,10 The arthroscopic prevalence of SLAP lesions in previous studies ranged from 3.9% to 11.8%2,9, but a more recent study has shown the prevalence to be as high as 26%.11 Snyder's original classification of SLAP lesions described the first four main types.2
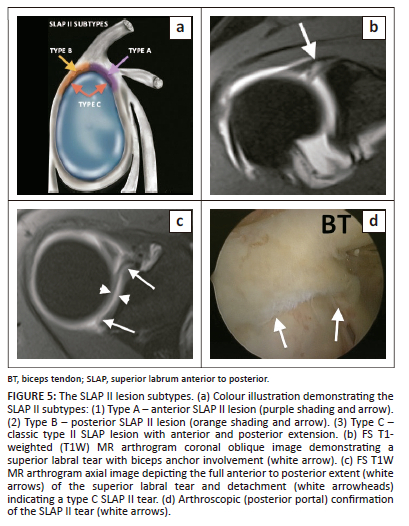
In 1991, Morgan and colleagues subdivided the type II lesion into subtypes A, B and C with the type A lesion being primarily anterior, the type B lesion primarily posterior and the type C lesion a combination of anterior and posterior tears.11 Maffett and colleagues subsequently identified a further three types of SLAP lesions, types V, VI and VII.9
Between 1997 and 2000, an additional three categories of SLAP lesions (VIII, IX and X) were introduced in informal talks, small meetings and conferences.3 There is another type of SLAP X lesion that exists in the literature, and this represents a superior labral tear with an associated reverse Bankart lesion.12
Imaging approach
The labrum, biceps tendon and glenohumeral ligaments should be considered as a single functional unit,8 highlighting the importance of a comprehensive evaluation of the labrum and adjacent structures. This concept arose primarily from the macroscopic and microscopic study by Huber and Putz13 that identified the periarticular fiber system, comprising bundles of parallel collagen fibers that run around the entire circumference of the glenoid and into the adjacent structures including the biceps tendon and glenohumeral ligaments. There is, however, individual variability of the periarticular fiber system because of the varied origin of the long head of the biceps tendon and the morphology of the glenohumeral ligaments. This patient variability most likely predisposes to certain patterns of injury, given an identical mechanism.8
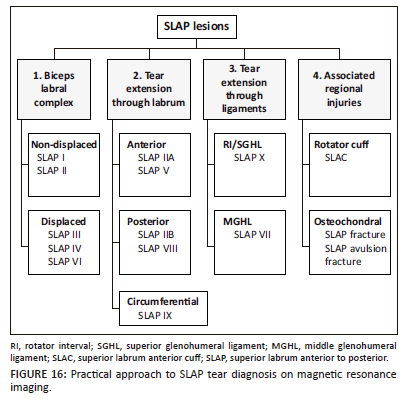
MR arthrography is a highly effective method for the detection of SLAP lesions but less so in the classification of the different types of SLAP lesions with 66% concurrence between MR arthrography and arthroscopy grading.14 A practical approach to the assessment of the labrum for a suspected SLAP lesion is therefore recommended, which also reinforces the concept of the periarticular fiber system and single functional unit and, should entail the evaluation of the following: (1) biceps labral complex for a tear, (2) the morphology of the tear (non-displaced or displaced), (3) the extension pattern of the tear to involve other parts of the labrum, (4) the glenohumeral ligaments and (5) the associated involvement of the regional structures that include the joint capsule, osteochondral elements and rotator cuff tendons.
The labrum should be assessed for its size, shape, signal intensity and attachment to the glenoid. The size is variable and of no practical diagnostic value.15,16 The shape is also variable and is most commonly triangular17 but can also be rounded, blunted, cleaved, notched, crescent-shaped and even absent.17,18 The labrum usually has regular margins and is of low signal on all MR pulse sequences. The labral attachment to the glenoid is extremely variable, particularly in the superior and anterosuperior quadrants, and this poses the greatest diagnostic challenge in differentiating developmental detachment from pathological detachment. There are five anatomic variants in this region, namely the sublabral recess or sulcus, sublabral foramen or hole, Buford complex, bicipital labral sulcus or pseudo-SLAP tear and the high attachment of the anterior band of the glenohumeral ligament. These may all be mistaken for labral tears, especially the sublabral recess.
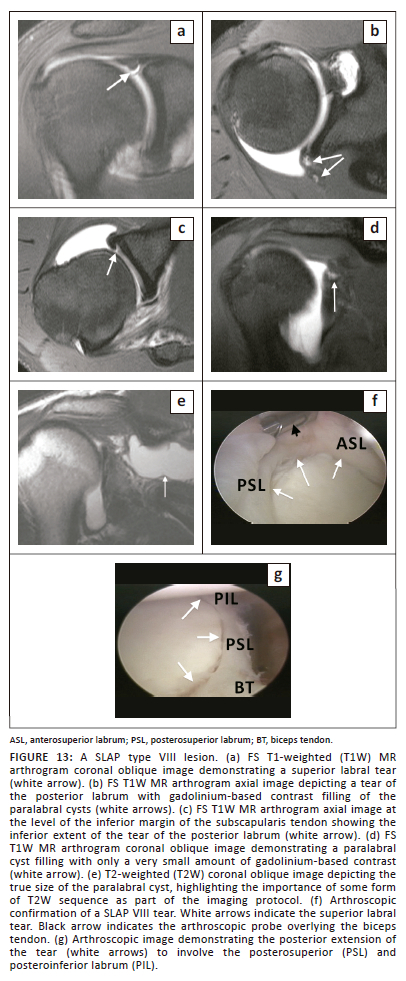
The diagnosis of SLAP lesions on MRI is based on the two primary signs of abnormal labral morphology and linear high signal intensity (fluid or contrast) in the labrum. A paralabral cyst is a secondary sign of a labral tear and is typically located in the spinoglenoid notch. These cysts may not fill during MR arthrography (MRA), as direct communication between the cyst and glenohumeral joint rarely occurs, emphasising the importance of obtaining a T2-weighted sequence as part of the routine MRA protocol (Figure 13d and Figure 13e).
It is important to assess whether the superior labral tear extends into the biceps tendon and to characterise the extent of biceps involvement as a compromise of the biceps anchor may determine the need for surgical treatment with biceps anchor stabilisation. The morphology of the labral tear should be evaluated as the labrum may remain in its normal location (non-displaced) or be displaced, having a fragment that has lost connection with the parent labrum and includes a bucket handle or flap tear.
Imaging diagnosis
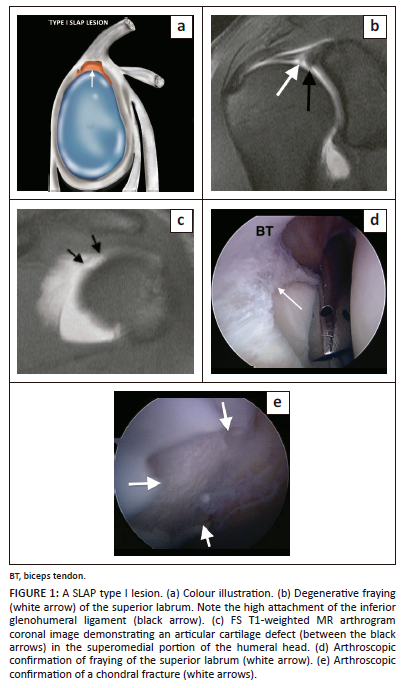
The type I SLAP lesion represents fraying of the superior labrum with an intact biceps anchor. This lesion is common in athletes with repetitive overhead shoulder activity but can also be seen incidentally as part of normal age-related labral degeneration.3 The fraying of the superior labrum may be difficult to appreciate, and the morphologic abnormality is probably best shown on direct MR arthrography (Figure 1).4
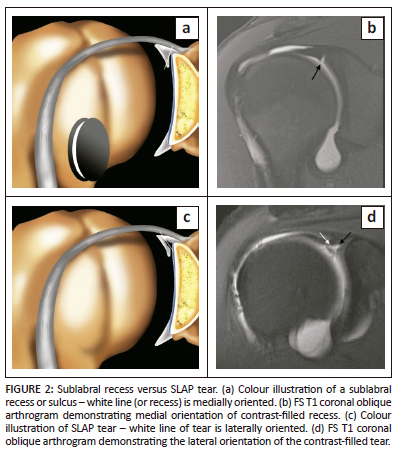
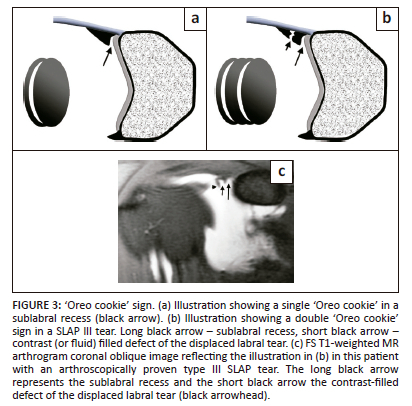
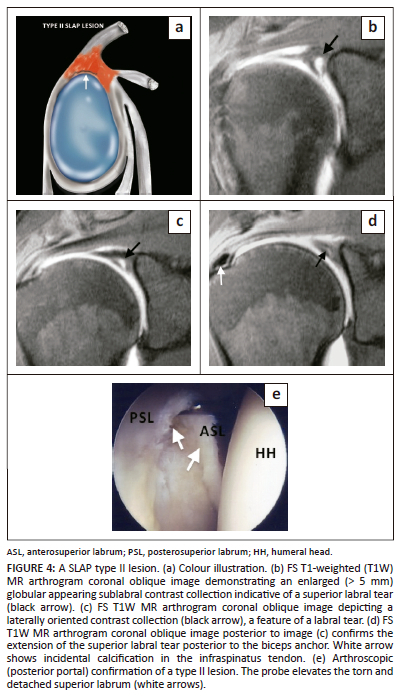
The type II SLAP lesion is a tear of the superior labrum with biceps anchor extension. The type II lesion is also common in athletic overhead activity and represents the most common type of SLAP lesion at arthroscopy and on MRI with a reported incidence of 41% - 55%.19 The sublabral recess variant may be mistaken for a type II SLAP lesion, and both entities can have the appearance of a single 'Oreo cookie' on coronal oblique images3 (Figure 2a and Figure 3a). Signs that are helpful in supporting the diagnosis of a tear rather than a normal recess include: a laterally oriented high signal intensity in the coronal oblique plane (Figure 2c and Figure 4c), extension of the high signal posterior to the biceps anchor in the coronal oblique plane (Figure 4d), a recess greater than 2 mm in size in its mediolateral dimension as measured in the coronal oblique plane (Figure 4b), anteroposterior extension of the high signal intensity in the axial plane (Figure 5c) and paralabral cyst formation.3,4,19,20 The anterior SLAP II lesion is associated with an anterior supraspinatus articular-sided partial thickness tendon tear in the SLAC (superior labrum anterior cuff) lesion and the posterior SLAP II lesion is the posterior peel-back lesion seen in the throwing athlete (Figure 5a).4
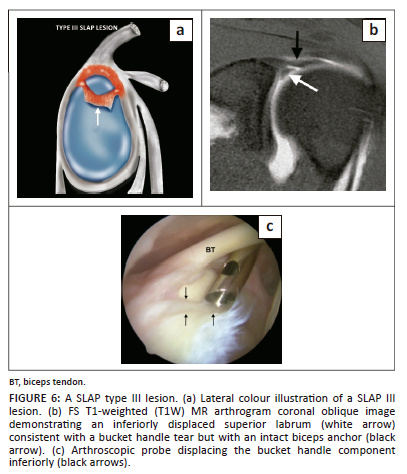
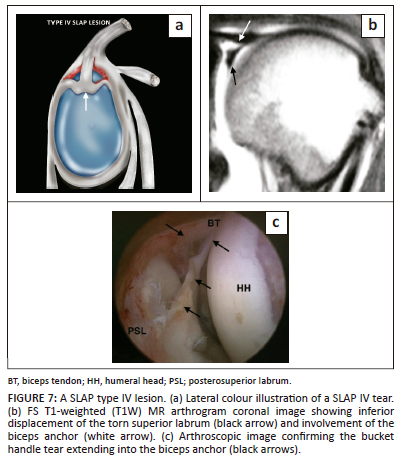
Type III SLAP lesion is a bucket handle tear of the superior labrum with an intact biceps anchor (Figure 6), whereas the type IV SLAP lesion represents a bucket handle tear of the superior labrum with biceps anchor extension (Figure 7), and both are usually the result of a fall on an outstretched arm.
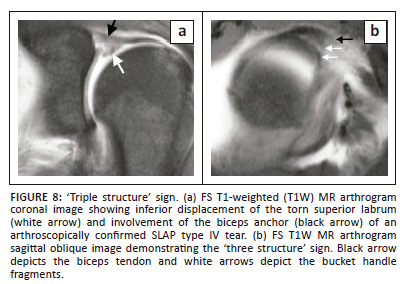
The type III and IV lesions are characterised by a bucket handle tear, and this is seen as displaced labral tissue on the coronal oblique and sagittal oblique images. Two useful diagnostic signs have been described: the double 'Oreo cookie' sign and the 'triple structure' sign. The double 'Oreo cookie' sign refers to the presence of a sublabral recess and a displaced labral fragment on a coronal oblique image (Figure 3).3 The 'triple structure' or 'three structure' sign refers to three separate and distinct structures that may be seen on sagittal or coronal oblique images. Contrast (or fluid) is seen between the biceps tendon and the superior labrum as well as between the two separated labral fragments (Figure 8).4
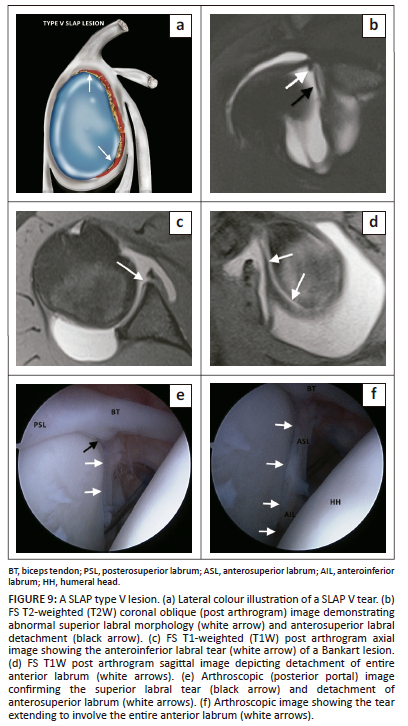
The type V SLAP lesion is a superior labral tear with anteroinferior extension or a Bankart lesion with superior extension and is usually associated with an anterior dislocation of the shoulder. The SLAP component of the tear is best visualised in the coronal oblique plane (Figure 9b), whereas the Bankart component is best seen in the axial plane (Figure 9c) and in the abduction and external rotation (ABER) position. A Hill-Sachs lesion may also be seen in the axial plane above the level of the coracoid process.
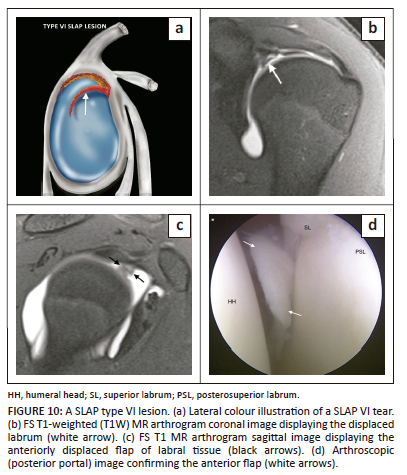
The type VI SLAP lesion represents a flap tear of the superior labrum and probably represents a tear of the bucket handle component of a type III or IV lesion.3 The flap tear can either be anterior (Figure 10) or posterior and is usually seen after a fall on an outstretched arm. This can be a very difficult diagnosis to make and is best identified on coronal images (Figure 10b) although sagittal images (Figure 10c) are required to appreciate the flap component.4
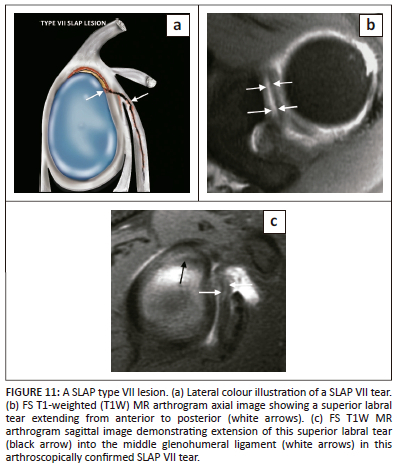
The type VII SLAP lesion is a superior labral tear with extension into the middle glenohumeral ligament (Figure 11) and, as with SLAP V lesions, is commonly associated with anterior shoulder dislocation.
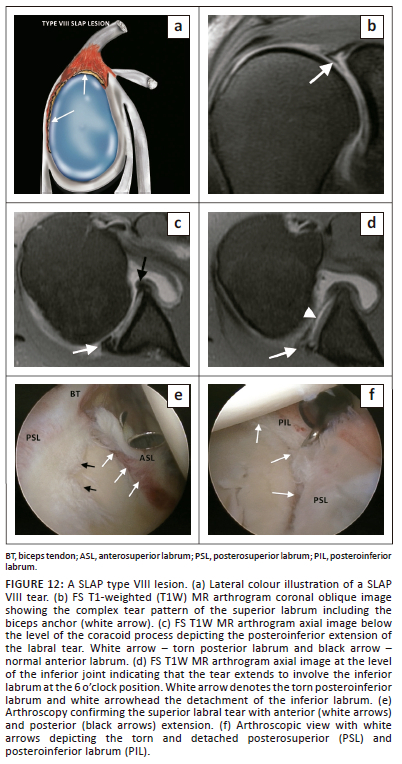
The SLAP VIII lesion represents a superior labral tear with extension into the posterior labrum (Figure 12 and Figure 13) but more extensively than that seen in a SLAP type IIB tear (Figure 5a). This tear usually follows a posterior dislocation of the shoulder. The coronal images confirm the superior labral tear and the axial and sagittal images demonstrate the posteroinferior extension of the tear.
Type IX SLAP lesion represents a circumferential labral tear (Figure 14) and is associated with severe acute trauma. The coronal images demonstrate the superior and inferior components of the labral tear, whereas the axial images display the anterior and posterior components of the tear.

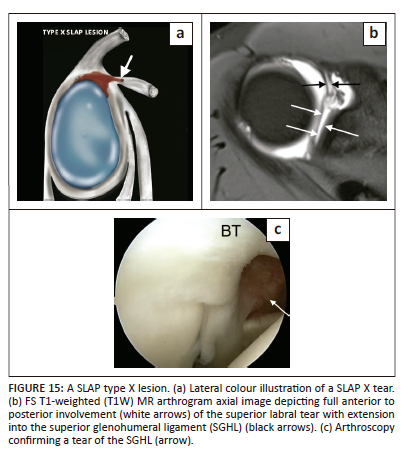
Type X SLAP lesion represents a superior labral tear with extension into the rotator interval involving the superior glenohumeral ligament (Figure 15) and usually follows acute severe trauma.
There are several miscellaneous SLAP lesions with the involvement of regional structures. A SLAP fracture represents a SLAP lesion with an associated humeral head chondral fracture, which is typically located superomedially (Figure 1c).4 While a rare injury, a SLAP avulsion fracture involves osseous avulsion of the labrum and biceps from the superior glenoid.4 A SLAC lesion represents a SLAP II lesion in association with a partial thickness tear of the articular surface of the anterior supraspinatus tendon.4 A practical approach to SLAP tear diagnosis on MRI is presented in Figure 16.
Management
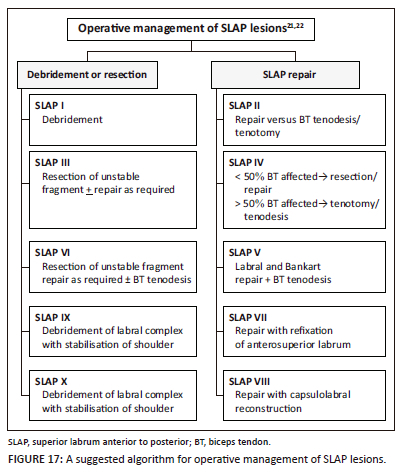
The management of SLAP lesions is controversial, and a detailed review is beyond the scope of this article. The main principle of operative intervention is to restore the stability of the superior labrum and the biceps labral complex. Several factors are taken into consideration including the type of tear, age of the patient, level of activity, stability of the superior labrum and integrity of the biceps anchor as well as associated injuries such as rotator cuff and capsular tears.21
Conservative management is usually reserved for type 1 lesions. Operative options include labral debridement, repair or resection of the unstable labral fragment. Biceps tendon procedures include debridement, tenotomy and tenodesis. Capsulolabral reconstruction and stabilisation are further options.21,22 A suggested management algorithm is highlighted in Figure 17.21,22 This underscores the value of MR arthrography as a means of accurate diagnosis and preoperative evaluation in patients with a SLAP lesion.
Conclusion
Superior labrum anterior to posterior lesions are a common cause of shoulder pain and instability. The clinical diagnosis is difficult and although arthroscopy remains the diagnostic gold standard, MRI, particularly direct MR arthrography, is the optimal imaging modality to evaluate glenoid labral anatomy and pathology and can reliably demonstrate the spectrum of SLAP lesions. A practical imaging approach is recommended that includes evaluation of the biceps labral complex, the morphology of the tear, the extension pattern of the tear to involve other parts of the labrum and glenohumeral ligaments and the associated involvement of the regional structures, which will assist in the management of patients with SLAP lesions.
Acknowledgements
The authors acknowledge Neil Northey, a graphic designer with Graphictricks, for the illustrations. They would like to thank their orthopaedic colleagues, particularly Dr S.A. Osman, Dr W. Haynes, Dr A. Baker, Dr L. Rajah and Dr B. Stathoulis whose cases appear in this pictorial review. The authors appreciate the great contribution of radiographic staff at Drs. Lake, Smit & Partners, particularly the MRI radiographers.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
P.M. serves as the primary author and was involved in the conceptualisation, methodology, formal analysis and writing of the article. M.M. contributed to the writing of the manuscript while aiding with the data curation, overseeing review and editing and managing project administration.
Ethical considerations
This article followed all ethical standards for research.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The data used in this pictorial review were obtained from a variety of sources, including published literature, imaging repositories and arthroscopic imaging. All data used in this review are either publicly available or permission to use the data was obtained from the original authors. Any data that are not publicly available will be made available upon request from the corresponding author, M.M., subject to any applicable confidentiality agreements or legal restrictions.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1.Andrews JR, Carson WG Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337-341. https://doi.org/10.1177/036354658501300508 [ Links ]
2.Snyder SJ, Karzel RP, Del Pizzo W, et al. SLAP lesions of the shoulder. Arthroscopy. 1990;6(4):274-279. https://doi.org/10.1016/0749-8063(90)90056-J [ Links ]
3.Mohana-Borges AV, Chung CB, Resnick D. Superior labral anteroposterior tear: Classification and diagnosis on MRI and MR arthrography. AJR Am J Roentgenol. 2003;181(6):1449-1462. https://doi.org/10.2214/ajr.181.6.1811449 [ Links ]
4.Stoller DW. The shoulder. Chapter 8. In: Stoller DW, editor. Magnetic resonance imaging in orthopaedics and sports medicine. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2007; p. 1131-1461. [ Links ]
5.Chung CB, Steinbach LS. Long bicipital tendon including superior labral anterior-posterior lesions, Chapter 6. In: Steinback LS, Tirman PFJ, Peterfy CG, Feller JF, editors. MRI of the upper extremity: Shoulder, elbow, wrist and hand. Chapter 6. Philadelphia, PA: Wolters Kluver Helath/Lippincott Williams & Wilkins, 2010; p. 337. [ Links ]
6.Rowbotham EL, Grainger AJ. Superior labrum anterior to posterior lesions and the superior labrum. Semin Musculoskelet Radiol. 2015;19(03):269-276. https://doi.org/10.1055/s-0035-1549320 [ Links ]
7.Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4(4):243-248. https://doi.org/10.1016/S1058-2746(05)80015-1 [ Links ]
8.Chang EY, Fliszar E, Chung CB. Superior labrum anterior and posterior lesions and microinstability. Magn Reson Imaging Clin N Am. 2012;20(2):277-294. https://doi.org/10.1016/j.mric.2012.01.002 [ Links ]
9.Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med. 1995;23(1):93-98. https://doi.org/10.1177/036354659502300116 [ Links ]
10.Morgan CD, Burkhart SS, Palmeri M, et al. Type II SLAP lesions: three subtypes and their relation- ships to superior instability and rotator cuff tears. Arthroscopy. 1998;14(6):553-565. https://doi.org/10.1016/S0749-8063(98)70049-0 [ Links ]
11.Kim TK, Queale WS, Cosgarea AJ, McFarland EG. Clinical features of the different types of SLAP lesions: An analysis of one hundred and thirty-nine cases. J Bone Joint Surg Am. 2003;85-A(1):66-71. https://doi.org/10.2106/00004623-200301000-00011 [ Links ]
12.Nord KD, Brady PC, Yazdani RS, et al. The anatomy and function of the low posterolateral portal in addressing posterior labral pathology. Arthroscopy. 2007;23(9):999-1005. https://doi.org/10.1016/j.arthro.2007.04.011 [ Links ]
13.Huber WP, Putz RV. Periarticular fiber system of the shoulder joint. Arthroscopy. 1997;13(6):680-691. https://doi.org/10.1016/S0749-8063(97)90001-3 [ Links ]
14.Waldt S, Burkart A, Lange P, Imhoff AB, Rummeny EJ, Woertler K. Diagnostic performance of MR arthrography in the assessment of superior labral anteroposterior lesions of the shoulder. AJR Am J Roentgenol. 2004;182(5):1271-1278. https://doi.org/10.2214/ajr.182.5.1821271 [ Links ]
15.Zanetti M, Carstensen T, Weishaupt D, et al. MR arthrographic variability of the arthroscopically normal glenoid labrum: Qualitative and quantitative assessment. Eur J Radiol. 2001;11:559-566. https://doi.org/10.1007/s003300000679 [ Links ]
16.Zlatkin MB, Saunders TG. Magnetic resonance imaging of the glenoid labrum. Radiol Clin North Am. 2013;51:279-297. https://doi.org/10.1016/j.rcl.2012.11.003 [ Links ]
17.Neumann CH, Tirman PFJ, Steinbach LS, Unger HR. Normal anatomy, Chapter 1. In: Steinbach LS, Tirman PFJ, Peterfy CG, Feller JF, editors. Shoulder magnetic resonance imaging. Philadelphia: Lippincott Williams & Wilkins, 1998; p. 27. [ Links ]
18.De Maeseneer M, Van Roy P, Shahabpour M. Normal MR imaging anatomy of the rotator cuff tendons, glenoid fossa, labrum and ligaments of the shoulder. Radiol Clin North Am. 2006;44(4):479-486. https://doi.org/10.1016/j.rcl.2006.04.002 [ Links ]
19.Jin W, Ryu KN, Kwon SH, Rhee YG, Yang DM. MR arthrography in the differential diagnosis of type II superior labral anteroposterior lesion and sublabral recess. AJR Am J Roentgenol. 2006;187(4):887-893. https://doi.org/10.2214/AJR.05.0955 [ Links ]
20.Beltran J, Bencardino J, Mellado JM, et al. MR arthrography of the shoulder: Variants and pitfalls. Radiographics. 1997;17(6):1403-1412. https://doi.org/10.1148/radiographics.17.6.9397454 [ Links ]
21.Jain A, Aniq H, Mistry A. SLAP injury and the superior labrum. Semin Musculoskelet Radiol. 2022;26(05):577-584. https://doi.org/10.1055/s-0042-1758840 [ Links ]
22.Brockmeyer M, Tompkins M, Kohn DM, Lorbach O. SLAP lesions: A treatment algorithm. Knee Surg Sports Traumatol Arthrosc. 2016;24(02):447-455. https://doi.org/10.1007/s00167-015-3966-0 [ Links ]
 Correspondence:
Correspondence:
Matthew Mercouris
mercouris@gmail.com
Received: 25 Apr. 2023
Accepted: 27 Aug. 2023
Published: 28 Nov. 2023














