Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Journal of Radiology
On-line version ISSN 2078-6778
Print version ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.27 n.1 Johannesburg 2023
http://dx.doi.org/10.4102/sajr.v27i1.2730
CASE REPORT
Calcinosis circumscripta of the breasts: The deeper meaning
Tanusha SewchuranI; Joel M. KabeyaII
IDepartment of Radiology, Faculty of Health, Greys Hospital, University of KwaZulu-Natal, Pietermaritzburg, South Africa
IIDepartment of Radiology, Greys Hospital, Pietermaritzburg, South Africa
ABSTRACT
Calcinosis circumscripta involving the breasts usually hints at an underlying systemic cause, most commonly connective tissue disorders such as scleroderma or dermatomyositis. Localised scleroderma, also known as morphoea, is not usually associated with the systemic anomalies affecting the lungs and gastrointestinal system, but does manifest as calcified dermal and subdermal sclerotic plaques. Histological confirmation with skin biopsy is diagnostic.
CONTRIBUTION: Recognition of the atypical, bizarre, linear dystrophic calcifications on mammography should direct appropriate systemic investigations.
Keywords: calcinosis circumscripta; breast calcinosis; benign breasts calcification; mammography; HRCT.
Introduction
Calcinosis refers to the deposition of calcium in the skin and subcutaneous tissues and can either be localised in the form of calcinosis circumscripta or diffuse, calcinosis universalis.
Patient presentation
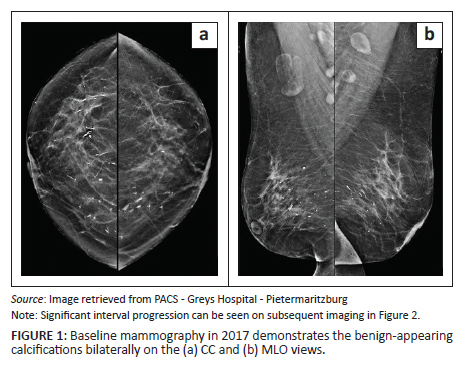
A 61-year-old female presented for mammography with a history of 'peau d'orange' and multiple 'lumps' translated as multiple suspected intraductal plaques palpable on clinical review. Baseline mammography in 2017 was evaluated as BIRADS 2, with several secretory type calcifications observed bilaterally (Figure 1). On further interrogation, the patient was known to dermatology with an undifferentiated connective tissue disorder, Raynaud syndrome and an anti-neutrophil cytoplasmic antibody (ANCA)-negative panniculitis or vasculitis. The diagnosis was confirmed with skin punch biopsy of an upper chest lesion, histologically proven as an old non-specific panniculitis, healing with fibrosis and focal calcification. No evidence of lupus was found. Biochemically, the patient's calcium and phosphate levels were within the normal range.
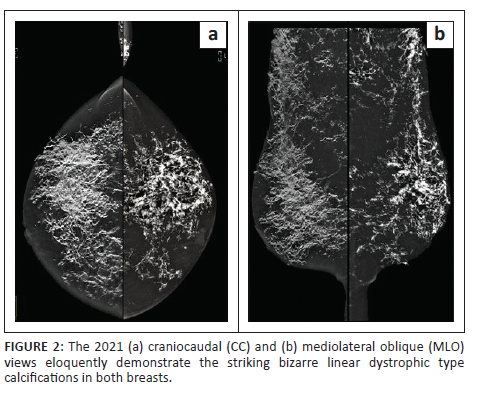
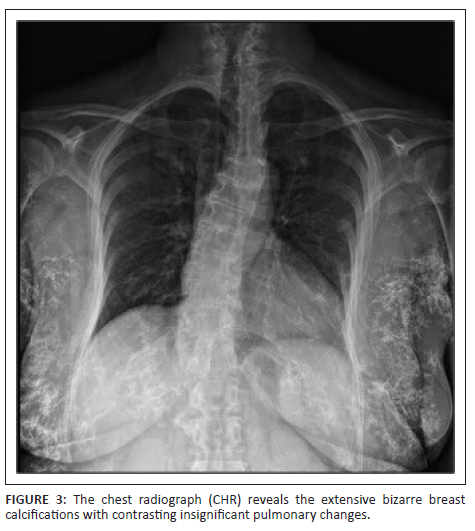
Imaging of the chest and breasts was performed subsequently. Mammography demonstrated marked interval progression in the previously observed benign calcifications, now seen to extensively involve the stromal tissue of both breasts and the subcutis (Figure 2). The calcifications appeared bizarre with a coarse linear morphology. The pectoralis muscles were relatively spared. No overt primary or secondary features of malignancy were identified. On further evaluation, scattered foci of mass-like calcifications were found to involve the subcutaneous tissues of the chest wall, axillae and abdomen (Figure 3). Ultrasound evaluation of the chest and abdominal wall revealed similar findings to that seen on breast ultrasound.
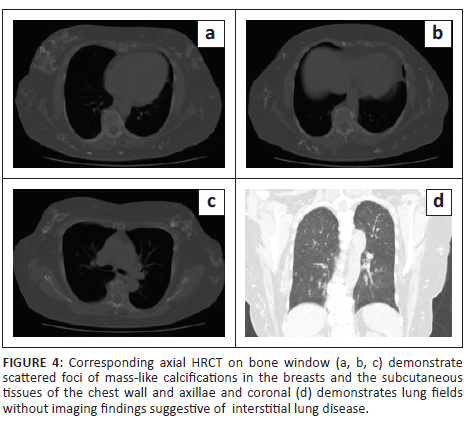
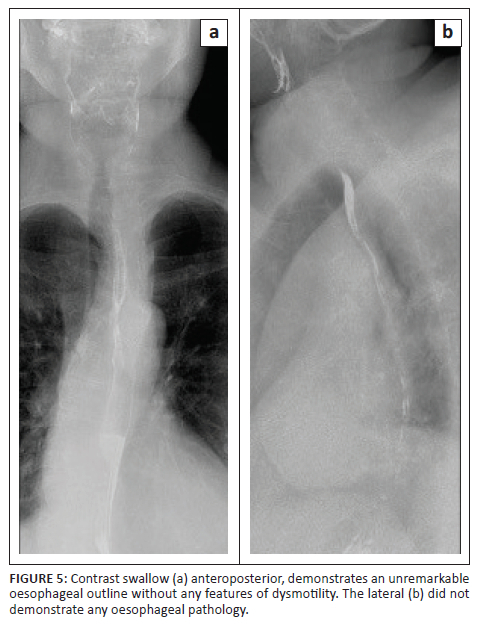
High resolution CT of the lungs performed thereafter, eloquently demonstrated the breast parenchymal changes with no interstitial lung changes (Figure 4). Similar appearing dystrophic calcifications were seen throughout the subcutis of the chest and abdomen. There were no discernible lung changes as compared with previous HRCT chest imaging from 2017. Contrast swallow was also normal at this stage, making CREST syndrome (calcinosis, Raynaud's, oesophageal dysmotility, sclerodactyly and telangiectasia) and dermatomyositis less likely differentials (Figure 5).
Discussion
The deposition of calcium in the skin and subcutaneous tissues, termed calcinosis, is generally attributed to either local or systemic causes.1,2 It can be differentiated as calcinosis circumscripta, which refers to more localised deposits in the cutis or subcutis, as compared to calcinosis universalis which includes muscle and tendon deposition.1,2 This calcinosis is a rare but documented cutaneous manifestation, first described in animals.1,3 It has also been established in patients with dermatomyositis and systemic lupus.3,4 Another recognised cause is localised scleroderma (LS) or morphoea, first described in 1878 by Weber.1 Localised scleroderma may be distinguished from systemic scleroderma by the lack of associated gastrointestinal, renal, cardiac and pulmonary anomalies.5 Localised scleroderma or morphoea can be broadly classified into plaque morphoea, generalised morphoea, linear morphoea or deep morphoea.6 Plaque morphoea represents the commonest variant of LS, presenting as dermal sclerosis or calcifications from excessive collagen production and deposition.1,6 This is manifested as indurated areas of skin, typically on the trunk and limbs, and calcifications.6
Clinically, patients may present with skin discolouration, nodularity, pain and limited mobility depending on the location, as well as ulceration and superimposed infection.1 The condition is generally self-limiting with morbidity depending on the site of involvement (e.g., joints and tendons) and/or superimposed infection. The disease entity is commonly seen in middle-aged females.1 Plain radiography identifies the calcifications as first line imaging.1 Imaging with CT and MRI can also be utilised to assess bones and joints in cases of associated morbidity.1 MRI depicts the accompanying inflammatory changes in the fascia, muscles, tendons and bones.5 Confirmation with biopsy and histopathology, with calcium deposits identified in the dermis and subcutaneous tissues, is usually diagnostic.1
While breast calcifications, both benign and malignant, are not novel imaging findings, these more bizarre dystrophic calcifications hint at a systemic cause and should prompt further investigation.
Acknowledgements
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
T.S. and J.M.K. contributed to the conception, design and drafting of the article. Both T.S. and J.M.K. contributed to the final version of the manuscript. T.S. supervised the project.
Ethical considerations
Ethical standards for research were followed during all the steps of this case report. Written informed consent was obtained directly from the patient. Confidentiality was maintained by anonymising the data at the point of collection.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The authors confirm that the data supporting the findings of this research are available within the article.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1.Yadav P, Thind SS. Imaging features in calcinosis circumscripta, a rare type of subcutaneous calcification in localized scleroderma. Med J DY Patil Univ. 2013;6(4):444-446. [ Links ]
2.Hwang ZA, Suh KJ, Chen D, Chan WP, Wu JS. Imaging features of soft-tissue calcifications and related diseases: A systematic approach. Korean J Radiol. 2018;19(6):1147-1160. https://doi.org/10.3348/kjr.2018.19.6.1147 [ Links ]
3.Magalhaes M, Costa Y, Goncalo M, Gomes P, Caseiro-Alves P. Breast calcinosis in a patient with dermatomyositis. Eurorad [serial online] 2013 [cited 2023 Jun 03]. Available from: https://www.eurorad.org/case/10899 [ Links ]
4.Prendergast M, Hopkinson N. Breast calcinosis, panniculitis and fat hypertrophy in a 35 year old woman with dermatomyositis. Rheumatology. 2007;46(8):1378-1379. https://doi.org/10.1093/rheumatology/kem144 [ Links ]
5.Schanz S, Fierlbeck G, Ulmer A, et al. Localised scleroderma: MR findings and clinical features. Radiology. 2011;260(3): 817-824. https://doi.org/10.1148/radiol.11102136 [ Links ]
6.Marsol IB. Update on the classification and treatment of localized scleroderma. Actas Dermosifiliogr. 2013;104(8):654-666. https://doi.org/10.1016/j.adengl.2012.10.012 [ Links ]
 Correspondence:
Correspondence:
Joel Kabeya
kabeyajoel@gmail.com
Received: 10 June 2023
Accepted: 31 July 2023
Published: 27 Sept. 2023














