Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Journal of Radiology
versão On-line ISSN 2078-6778
versão impressa ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.25 no.1 Johannesburg 2021
http://dx.doi.org/10.4102/sajr.v25i1.1964
PICTORIAL REVIEW
A kaleidoscopic view of male urethral pathologies on 64-slice multidetector computed tomographic urethrography: A novel technique
Shuchi BhattI; Avinaba BanerjeeI; Anupama TandonI; Saumya DangwalI; Arun GuptaII
IDepartment of Radiology, University College of Medical Sciences and GTB Hospital, Delhi, India
IIDepartment of Surgery, University College of Medical Sciences and GTB Hospital, Delhi, India
ABSTRACT
Pathologies of the male urethra are mostly obstructive in nature and require imaging to delineate the lesion type, site, extent and associated abnormality of the urinary bladder. Contrast urethrography (CU) is the gold standard investigation for urethral assessment but has many limitations. Cross-sectional imaging is infrequently used for the evaluation of the urethra but has been gaining importance recently. Multidetector computed tomographic urethrography (MDCTU) has the capability of evaluating the entire length of a male urethra in a single setting and overcomes many technical and patient limitations of CU. Being a novel technique, most radiologists are not familiar with MDCTU and the imaging spectrum of various urethral and bladder pathologies. This pictorial review attempts to present the imaging appearance of the normal male urethra and spectrum of pathological findings, with highlights on its advantages over the CU technique.
Keywords: male urethra; urethrography; computed tomography; stricture; 3D imaging.
Background
Contrast urethrography (CU) - retrograde urethrography and micturating cystourethrography - evaluates the anterior and posterior male urethra, respectively, and is the gold standard for urethral assessment.1 Cross-sectional techniques - sonourethrography, transrectal voiding sonourethrography and magnetic resonance urethrography - delineate the urethral pathologies but have inherent limitations. Sonourethrography has a small field of view, assesses only the anterior urethra and is operator dependent.2 Transrectal voiding sonourethrography3 evaluates the posterior urethra with much patient discomfort. Magnetic resonance imaging is not frequently used because of its cost and complexity.
Multidetector computed tomographic urethrography (MDCTU) is obtained using a multidetector computed tomographic scanner to acquire fast, thin slices of a distended urethra as the patient voids4 a contrast-filled urinary bladder. Better sensitivity to the contrast and post-processing of iso-volumetric axial images to obtain reformatted two-dimensional (2D) and 3D images explicitly demonstrate a plethora of urethral pathologies. Comprehensive evaluation of the entire length of the urethral lumen, periurethral, pelvic soft tissues and bones is possible with MDCTU.4
The possibility of post-processing in MDCTU allows the patient to micturate in a comfortable position with representation of non-distorted urethral anatomy, leading to better patient compliance. Therefore, MDCTU proves useful in uncooperative patients or in the following clinical situations:
•when procedural failure is expected because of technical difficulties: unsuccessful catheterisation, inadequate bladder filling and inability to assume an oblique position during micturition because of a pelvic fracture
•following suboptimal examination on CU resulting in inadequate urethral evaluation: failure to delineate the pathology, especially of the posterior urethra because of obscuration from the pelvic bones; faint contrast density in the urethra and contrast extravasation into periurethral tissues, hindering urethral visualisation
•if surgical intervention is planned: improved surgical planning can be done in cases such as pelvic trauma with suspected posterior urethral distraction defects; accurate measurement of the stricture length ensures optimal treatment decisions, especially when associated periurethral diseases such as fistula and false passages are present.
Technique
Initially, bladder filling is achieved either directly by instillation of contrast (250 millilitres [mL] - 400 mL of 10% diluted ionic or non-ionic contrast media) through a supra-pubic catheter or a Foley's catheter or indirectly by intravenous contrast administration. Thin axial computed tomography (CT) sections (e.g. 64 × 0.6 with a 64-slice CT) are obtained as the patient voids into a condom catheter in a comfortable position (supine, prone, oblique or lateral).
Multiplanar reformatting (MPR), maximum intensity projection (MIP) and volume rendering technique (VRT) images are used for vivid representation of the urethra and its pathology. Multiplanar reformatting images depict the urethra and periurethral soft tissues, enabling visualisation of normal anatomy and pathology simultaneously. Curved MPR images show the entire length of the curved urethra and thus delineates a stricture, if present. Thick MIP reconstructions clearly depict the capacity, outline of the contrast-filled bladder, vesico-ureteric reflux into the lower ureters as well as the urethral outline and calibre. The volume rendering technique is used to provide a 3D external view of the bladder and urethra. Bone removal algorithms help in the optimal visualisation of the posterior urethra.
A 64-slice multidetector computed tomography scanner, Somatom Definition AS (M/s Siemens AG Healthcare Sector, Germany), was used to acquire all the scans presented in this review. The various types of images present exquisite details of the common urethral pathologies encountered in a male patient.
Normal imaging appearance
The urethra can be visualised on VRT (Figure 1a), MIP (Figure 1b) and curved MPR (Figure 1c) images as a contrast-filled tubular structure, arising from the neck of the bladder and opening into the external urethral meatus. The bulbar urethra is the widest portion, having a normal coned appearance at the bulbomembranous junction. The membranous urethra is the narrowest part with near-parallel walls, at the level of the external urethral sphincter (Figures 1a, b and c). Distally, the bulbar urethra continues as the penile urethra with a normal 'kink' or 'bend' at the penoscrotal junction, which should not be confused with a stricture (Figures 1a, b and c).
The VRT and MIP images can be represented with bone subtraction for depicting a clear 3D volumetric view (VRT) of the urethra, whilst the MIP image shows the contrast-filled urethra and bladder as a composite CU image without the overlapping pelvic bones. This provides a clear understanding of any abnormal morphology of the urethra.
Urethral pathologies
Stricture
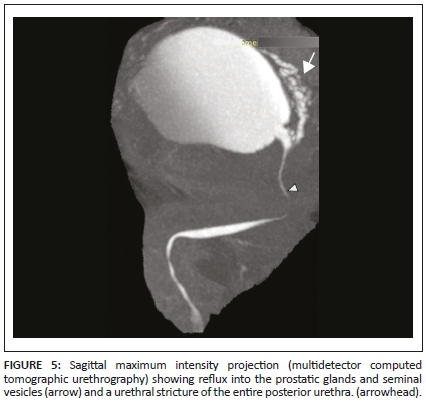
A urethral stricture is the commonest obstructive lesion, appearing as narrowing or abrupt change in calibre of the contrast-filled urethral lumen. A short- or long-segment stricture is less than or more than 2 cm, respectively1 (Figures 2 and 3). The definitive treatment is urethroplasty, and surgical planning requires accurate demonstration of the stricture length.5,6,7 The mean stricture length can be more accurately measured on MDCTU than on CU.1 Greater sensitivity for contrast in an antegrade urethrographic study on MDCTU1,4 allows for posterior urethral evaluation as well, unlike in micturating cystourethrography. Partial urethral strictures (Figures 2-4) and multiple urethral strictures (Figure 4) can be delineated on MDCTU. A posterior urethral stricture, its length, extent and the associated reflux of contrast into the prostatic glands and seminal vesicles is also well demonstrated on MDCTU (Figure 5).
Urethritis
Urethral inflammation on MDCTU is seen as irregularity in the urethral wall (Figure 6). It is often associated with contrast extravasation into the periurethral soft tissues or Littre's glands. Cystitis is commonly seen with urethritis and urethral strictures (Figure 7).
False tract
A false tract may result from an attempt to dilate the urethral stricture. False tracts are seen as contrast-filled linear tracts, separate from the main urethra but communicating with the main urethral lumen (Figures 6 and 8). Multidetector computed tomographic urethrography accurately helps to differentiate it from reflux into any normal anatomical structures (Figure 6).
Posterior urethral distraction defects
These defects are difficult to evaluate on CU as associated pelvic fractures result in suboptimal radiographs.8 Soft tissues are well demonstrated by selective removal of overlapping bones on MDCTU, thus enhancing visualisation of the posterior urethra. Posterior urethral distraction defects are best seen on 3D-VRT images8 (Figures 9 and 10).
Urethral diverticulum
A urethral diverticulum is uncommon and classified as congenital or acquired or as primary or secondary.9 Recurrent infections, instrumentation or surgery, inflammation and trauma of the periurethral glands or ducts result in secondary diverticula formation.10 It appears as a focal contrast-filled outpouching from the urethra (Figure 10) and is continuous with the urethral lumen. Associated complications such as calculi are also well demonstrated on MDCTU.
Urethral calculi
Primary urethral stones may occur in the urethra proximal to an obstruction, related to chronic infective strictures and meatal stenosis in young boys.11 An isolated stone is often a migrated stone from the upper urinary tract.12 A calculus is a well-defined, sharply marginated hyperdensity within the urethral lumen. Occasionally the high density of contrast may obscure a calculus on CU unless supplemented by a control plain radiograph (Figure 11). In MDCTU, alteration of the window levels and width enables detection of the calculus within the contrast column.
Urethral foreign bodies
A urethral foreign body is demonstrated on MDCTU due to the inherent high-contrast resolution of CT (Figure 12).
Bladder pathologies
Cystitis
Bladder outlet obstruction and bladder calculus are common causes of secondary cystitis and are mostly seen as generalised and uniform bladder wall thickening. Extravasation of contrast may be identified from the inflamed bladder wall. Chronic cystitis appears as a small capacity bladder (Figure 7).
Other bladder pathologies observed are sacculations, diverticula and calculi. A focal outpouching within the bladder wall is a sacculation, and when it extends outside the wall, it is a diverticulum (Figure 13). Associated urinary stasis may lead to calculus formation within the diverticulum (Figure 13).
Bladder rupture
Bladder rupture is seen in the context of significant trauma13,14 and may be of two types:
•Extra-peritoneal (80% - 90%) is the result of pelvic fractures or penetrating trauma. Multidetector computed tomographic urethrography reveals a variable path of extravasated contrast material.
•Intra-peritoneal (10% - 20%) typically results from a direct blow to a distended bladder and demonstrates intra-peritoneal contrast material around the bowel loops, between mesenteric folds and in the paracolic gutters (Figure 14).
Vesical fistula
A fistulous communication between the bladder and an adjacent structure, such as the rectum (rectovesical), colon (colovesical) or small bowel (enterovesical), is better seen on MDCTU as an irregular contrast-filled tract from the bladder to the adjacent organ. Sometimes, only a nipple-like projection outside the bladder lumen may suggest the presence of a fistulous tract (Figure 11c).
Miscellaneous pathologies
Additional findings in the periurethral, vesical and pelvic soft tissues and bones may also be observed on MDCTU, including vesico-ureteric reflux (Figure 15), prostatomegaly (Figure 16), prostatic and soft-tissue calcifications, bone abnormalities and hydrocele.
Radiation issues
The effective radiation dose on MDCTU varies between 5 millisievert (mSv) and 6 mSv,14 whereas in CU, it is less than 1 mSv. Radiation exposure can be further reduced on MDCTU by using a low-dose protocol, single acquisition, mA tube modulation and iterative reconstruction techniques. Although the radiation dose is higher with MDCTU, radiation exposure to the operator can be avoided, unlike in CU.
Conclusion
This pictorial assay apprises radiologists and clinicians about the novel technique of MDCTU, its advantages over CU and appropriate patient selection to justify the increased radiation exposure, a shortcoming associated with it.
Multidetector computed tomographic urethrography is capable of comprehensive evaluation of both the anterior and posterior male urethra, periurethral tissues, urinary bladder, pelvic soft tissues and bones in a single scan, thus rendering it an effective diagnostic tool.
Acknowledgements
Competing interests
The authors have declared that no competing interests exist.
Authors' contributions
All authors contributed equally to this work.
Ethical consideration
Due institutional ethical clearance was obtained (IEC-HR 126) and written informed consent was taken from all patients. The ethical standards of the Declaration of Helsinki were followed.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability statement
Data sharing is not applicable to this article as no new data was created or analysed in this study.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1.Zhang XM, Hu WL, He HX, et al. Diagnosis of male posterior urethral stricture: Comparison of 64-MDCT urethrography vs. standard urethrography. Abdom Imaging. 2011;36(6):771-775. https://doi.org/10.1007/s00261-010-9676-7 [ Links ]
2.Chou CP, Huang JS, Wu MT, et al. CT voiding urethrography and virtual urethroscopy: Preliminary study with 16-MDCT. Am J Roentgenol. 2005;184(6):1882-1888. https://doi.org/10.2214/ajr.184.6.01841882 [ Links ]
3.Mandal SK, Bhattacharyya SK, Mandal A, Deoghuria D, Mandal PK. Sonourethrography in the evaluation of anterior urethral stricture: Correlation with retrograde urethrography in male. Int J Pharm Biomed Res. 2012;3(2):77-80. https://doi.org/10.1002/jcu.1870210404 [ Links ]
4.Mihmanli I, Kantarci F, Gulsen F, Kadioglu A. Transrectal voiding sonourethrography for diagnosis of a prostatic urethral calculus. J Ultrasound Med. 2006;25(11):1455-1457. https://doi.org/10.7863/jum.2006.25.11.1455 [ Links ]
5.Heyns CF, Steenkamp JW, De Kock MLS, Whitaker P. Treatment of male urethral strictures: Is repeated dilation or internal urethrotomy useful? J Urol. 1998;160(2):356-368. https://doi.org/10.1016/s0022-5347(01)62894-5 [ Links ]
6.Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: Long-term followup. J Urol. 1996;156(1):73-75. https://doi.org/10.1016/s0022-5347(01)65942-1 [ Links ]
7.Greenwell TJ, Castle C, Andrich DE, MacDonald JT, Nicol DL, Mundy AR. Repeat urethrotomy and dilation for the treatment of urethral stricture are neither clinically effective nor cost-effective. J Urol. 2004;172(1):275-277. https://doi.org/10.1097/01.ju.0000132156.76403.8f [ Links ]
8.El-Kassaby AW, Osman T, Abdel-Aal A, Sadek M, Nayef N. Dynamic three-dimensional spiral computed tomographic cysto-urethrography: A novel technique for evaluating post-traumatic posterior urethral defects. BJU Int. 2003;92(9):993-996. https://doi.org/10.1111/j.1464-410x.2004.4949a.x [ Links ]
9.Lee JWS, Fynes MM. Female urethral diverticula. Best Pract Res Clin Obstet Gynaecol. 2005;19(6):875-993. https://doi.org/10.1016/j.bpobgyn.2005.08.008 [ Links ]
10.Venkatanarasimha N, Freeman SJ, Dubbins PA. Posterior urethral diverticulum on transrectal sonography. J Ultrasound Med. 2009;28(6):827-829. https://doi.org/10.7863/jum.2009.28.6.827 [ Links ]
11.Frick J, Kunit G. Operations on previously operated patients with hypospadias. Prog Pediatr Surg. 1984;17:57-63. https://doi.org/10.1016/s0022-3468(85)80353-5 [ Links ]
12.Vashishtha S, Sureka SK, Agarwal S, et al. Urethral stricture and stone: Their coexistence and management. Urol J. 2014;11(1):1204-1210. https://doi.org/10.22037/uj.v11i1.1645 [ Links ]
13.Vaccaro JP, Brody JM. CT cystography in the evaluation of major bladder trauma. Radiographics. 2000;20(5):1373-1381. https://doi.org/10.1148/radiographics.20.5.g00se111373 [ Links ]
14.Avery LL, Scheinfeld MH. Imaging of male pelvic trauma. Radiol Clin North Am. 2012;50(6):1201-1217. https://doi.org/10.1016/j.rcl.2012.08.010 [ Links ]
 Correspondence:
Correspondence:
Shuchi Bhatt
drshuchi@hotmail.com
Received: 07 Aug. 2020
Accepted: 29 Sep. 2020
Published: 29 Jan. 2021














