Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Journal of Radiology
On-line version ISSN 2078-6778
Print version ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.22 n.1 Johannesburg 2018
http://dx.doi.org/10.4102/sajr.v22i1.1259
REVIEW ARTICLE
Magnetic resonance imaging of classified and unclassified Müllerian duct anomalies: Comparison of the American Society for Reproductive Medicine and the European Society of Human Reproduction and Embryology classifications
Devimeenal JegannathanI; Venkatraman IndiranII
IDepartment of Radiology, Government Kilpauk Medical College, India
IIDepartment of Radiodiagnosis, Sree Balaji Medical College and Hospital, India
ABSTRACT
Magnetic resonance imaging (MRI), due to its optimal delineation of anatomy, has become the mainstay in imaging for diagnosing Müllerian duct anomalies (MDA). Pelvic MRI is requested for various conditions such as primary amenorrhoea, infertility or poor obstetric history with regard to MDA, as identifying the exact aetiology for these conditions is vital. Knowledge regarding the classification of MDA is important, as the treatment varies with respect to the different classes. As all the lesions do not fit within the classification of the American Society for Reproductive Medicine, a new anatomy-based classification was established by the European Society of Human Reproduction and Embryology and the European Society for Gynecological Endoscopy, to fulfil the needs of experts. We aim to discuss various classes of classified and unclassified MDA with regard to both the above-mentioned classifications and illustrate some of them using various cases based on pelvic MRI studies.
Introduction
Embryologically, the two-paired Müllerian ducts fuse in the midline in the lower part by the 6th to the 11th week of gestation. Lateral fusion forms the uterus and upper two-thirds of the vagina and the cephalad parts of the separated ducts form the fallopian tubes. Resorption of the midline septum results in a single uterine cavity. The sinovaginal bulb forms the lower third of the vagina, which fuses with the lower part of the fused Müllerian ducts.1
Any deviation from the above process leads to Müllerian duct anomalies (MDA). Three-dimensional transvaginal ultrasound is almost as sensitive as magnetic resonance imaging (MRI) in diagnosing congenital uterine anomalies.2 However, MRI is preferred, as the T2 sequences enable clear delineation of the uterine zonal anatomy, ovaries, follicles, vaginal continuity to the uterus and vaginal septum.3 Though MDA are classified by the American Society for Reproductive Medicine (ASRM) into seven classes, there are some anomalies that are not included in the classification. In order to rectify the deficiencies, a new anatomy-based classification was established by the European Society of Human Reproduction and Embryology (ESHRE) and the European Society for Gynaecological Endoscopy (ESGE),4 classifying the anomalies according to the morphology of the uterus, cervix and vagina, independently.4
Clinical presentation of the MDA is variable, where patients with obstructive anomalies present earlier. In these young women, the goals of therapy are to relieve the obstruction immediately, restore normal menstruation and sexual function and preserve reproductive potential.5 Proper description and classification of the MDA on imaging is vital for planning and instituting appropriate treatment.
Magnetic resonance imaging sequences
T2-weighted sequences in all three planes (axial, coronal and sagittal) are adequate. Firstly, a sagittal T2-weighted image is obtained (TR/TE-4860/86, slice thickness [ST] 5mm and NEX-2), following which oblique coronal (Figure 1) and oblique axial sections are obtained along and perpendicular to the long axis of the uterus. A true coronal section along the long axis of the uterus allows for proper visualisation of the fundal contour. Volume sequences such as T2 CUBE (TR/TE-2000/102, ST2.8 mm and gap 1.4 mm) are very useful in this regard. With this sequence (Figure 2a), reformats in all the planes, including oblique sections, can be determined after image acquisition (Figure 2b). When complex anomalies such as accessory uterus-like structures are seen or in the case of didelphys with a divergent fundus, it is usually necessary to repeat the sequences for each component separately to get the exact coronal and axial sections of uterine cavities. T2 CUBE (GE Medical Corporation) is very beneficial in these circumstances (Figure 2c and d).
T1-weighted sequences are used to define any haemorrhagic component in the obstructed anomaly such as haematometra, adenomyosis, ovarian chocolate cyst and benign teratoma. It is also useful for uterine cysts with mucinous components and paravaginal Gartner's duct cysts (Figure 3b).
Coronal screening of the upper abdomen is mandatory in all cases of MDA to evaluate for associated renal abnormalities (Figure 3e). Instillation of vaginal gel (Figure 3b) is useful in cases of a blind vagina or transverse or longitudinal vaginal septum. Near-field artefacts can be reduced by placing saturation bands at both the anterior and posterior body walls.
Classifications
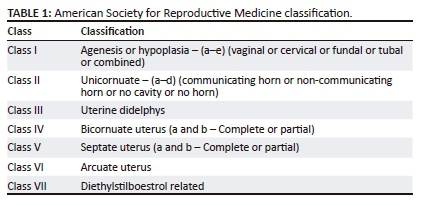
American Society for Reproductive Medicine (Table 1 and Figure 4) and ESHRE and ESGE classifications are used to illustrate the cases here.
The European Society of Human Reproduction and Embryology and the European Society for Gynecological Endoscopy classification
Uterine anatomical deviations are classified as normal uterus U0, dysmorphic uterus U1, septate uterus U2, bicorporeal uterus U3, hemi-uterus U4, aplastic uterus U5 and still unclassified cases U6.4 Each main class is further divided into sub-classes (Figure 5 and Figure 6).4

The main diagnostic features used in the American Society for Reproductive Medicine classification
1. An external fundal contour with dipping of more than 10% or 1 cm,6 indicates a possible diagnosis of uterine didelphys or a bicornuate uterus. Two separate uteri with preserved myo-endometrium zonal widths, two cervices and two vaginas are in keeping with didelphys.7 The uterine horns are widely splayed in uterine didelphys. Some degree of fusion in the lower uterine segment points more towards a bicornuate uterus than uterine didelphys.
2. To differentiate bicornuate and septate uterus: an intercornual distance of more than 4 cm, an intercornual angle of more than 105° and external fundal dipping favours a bicornuate uterus.7,8
3. Flat or subtle fundal dipping (less than 1 cm), an intercornual distance of less than 4 cm and an acute intercornual angle of less than 75° suggests a septate uterus.9 The septum can be muscular or fibrous. A muscular septum is thick and appears similar to myometrial intensity. A fibrous component is hypointense, thin and sharp.
4. In an arcuate uterus, myometrial dipping in the inner aspect of less than 10% is seen with a convex or flat outer fundal contour. The inner dipping edge is not sharp and saddle shaped,10 differentiating arcuate from a partial septate uterus.
5. The unicornuate uterus does not have the usual rounded fundal contour and oblong shape. Zonal anatomy and endometrial-myometrial differentiation is maintained.10,11
6. Absence of myometrial-endometrial differentiation or fundus, body and cervix differentiation represent a hypoplastic uterus.8
Salient points of the European Society of Human Reproduction and Embryology and the European Society for Gynecological Endoscopy classification
1. Bicornuate and didelphys uterus of the previous ASRM classification incorporate under bicorporeal uterus U3, subcategories 3a and 3b, respectively. A dysfused septate uterus is 3c.
2. Unicornuate uterus is classified under hemi-uterus U4.
3. A clear description of the septate uterus is provided as a fundal midline indentation of >50% of the uterine wall thickness. Anything less is included in the subcategory of U1, a dysmorphic uterus.4 The reference for myometrial thickness is obtained on the sagittal image of the uterus by calculating the mean of the measured anterior and posterior wall thicknesses.12
4. Arcuate uterus (type VI of ASRM) is not included in the ESHRE-ESGE classification system, avoiding unnecessary apprehension created by this almost normal variant as an anomaly. In the ESHRE-ESGE classification, these patients are classified as normal or septate, depending on the degree of midline indentation.13
5. The ESHRE and ESGE classification classifies 38 of the 39 congenital anomalies of the female genital tract, whereas the ASRM classification is not as comprehensive.13
6. Independent classification of uterine, cervical and vaginal anomalies is made. It is very useful, especially in cases of obstructive cervical or vaginal malformations with a normal uterus, which constitutes about 22 out of the 39 types of anomalies.13 The ASRM classification does not provide specific classes for these anomalies and groups them all under Class I.
7. The ESHRE and ESGE classification uses common terms for describing anomalies and the exact anatomical status of the female genital tract, rather than the liberal non-specific terminologies used in the ASRM classification.
8. The ESHRE and ESGE classification includes associated anomalies of non-Müllerian origin as part of its system to accommodate the renal tract malformations which are common with MDA.
9. The embryological origin of the anomalies can be easily identified on the basis of the ESHRE and ESGE classification.
10. The ESHRE and ESGE classification places less severe anomalies at the beginning with the more deformed anomalies placed as the later classes and sub-classes.4
11. The ESHRE and ESGE classification defines uterine deformities based on the proportions of uterine anatomical landmarks, such as uterine wall, rather than using definite objective numerical values, keeping in consideration the variability of uterine dimensions in different patients.4
Ethical consideration
Written informed consent was obtained from all the patients for publication of this review article, including all the images.
Case reviews
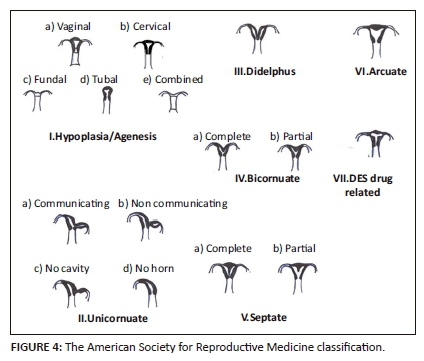
Normal uterus U0
A uterus having an interostial straight or curved line with less than 50% of the uterine wall thickness, internal indentation in the midline fundus and a flat external contour on coronal MRI section is considered a normal uterus U0 (Figure 7).
Dysmorphic uterus U1
A dysmorphic uterus is sub-classified by the shape of the uterine cavity as T-shaped, infantile and others. The other category is used to differentiate minor deformities.
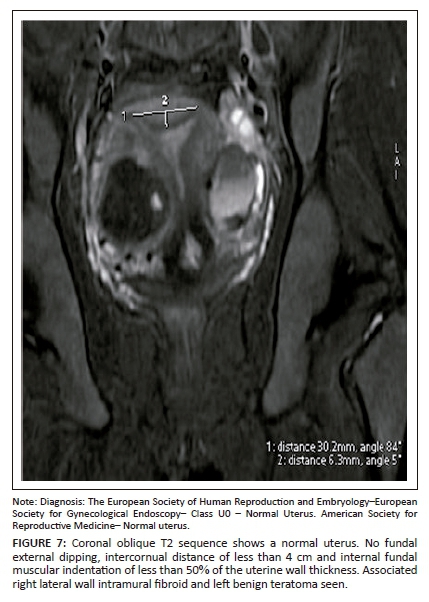
Septate uterus U2
This is due to an absorption defect. A uterus having a flat external contour and more than 50% internal fundal midline indentation is classified as a septate uterus. It is divided into subtypes a and b (partial [Figures 8 and 9] and complete [Figure 10] septate) by the extension of the septum above or below the internal cervical os, respectively. When two cervices are identified at clinical examination, it should not be interpreted as uterine didelphys, where no treatment is required. Imaging is mandatory.6 Septate uteri with two cervices (Figure 10) have been documented in the literature.14,15,16,17 The optimum treatment is resection of the septum.18
An arcuate uterus may be classified as a partial septate uterus in the ESHRE-ESGE classification (Figure 8). Somayya et al. state that the diagnosis of septate uterus is made frequently by following the ESHRE-ESGE classification, resulting in increased hysteroscopic metroplasty.19 This could be considered as one of the limitations of the study.
Ludwin et al.20 identified the median length of septum as 10.7 mm by the ESHRE-ESGE classification and as 21.1 mm by the ASRM criteria. In 36.4% of cases of septate uterus, internal fundal indentation was <1 cm by ESHRE-ESGE criteria and is usually considered as a normal uterus by ASRM. Their study further stated that the septate uterus was overdiagnosed and needed to be redefined for determining the treatment option of hysteroscopic metroplasty.20 Ludwin et al. stated that using three-dimensional ultrasonography and the ASRM classification with morphometric criteria is preferable and that further study with a larger sample size should be evaluated for reliability.21
Patients with a complete septate uterus may have multiple associated findings. Myomas were seen in the septum and left broad ligament in one of our patients (not shown). There was an associated Gartner's duct cyst that appeared hyperintense on the T1 sequence, extending from the fornix to the anterior vaginal wall. This patient also had a left ureterocoele with a short ureter ending blindly. She had a normal right kidney and an absent left kidney with an incidental left adrenal adenoma (Figures 3a-f). A blind-ending ureteral bud in association with renal agenesis and a ureterocoele are rarely reported.22,23,24 Magnetic resonance imaging is the modality of choice for diagnosing an atretic ureterocele; other cross-sectional imaging modalities have limited value.23
Bicorporeal uterus U3
A bicorporeal uterus is caused by fusion defects, characterised by external indentation of more than 50% of the uterine wall thickness. This is subdivided into partial and complete (Figure 11) by the extension of the division above or up to the level of the cervix. A bicorporeal septate uterus (Class U3c) has a coexistent absorption defect in addition to the fusion defect and shows fundal indentation exceeding 150%.
Increased risk of placental abnormalities has been reported with uterine anomalies,25 especially with uterus didelphys (Figure 12) and bicornuate, unicornuate and septate uteri. Uterine didelphys (bicorporeal U3b) with a vaginal septum and obstructed hemivagina resulting in haematometra along with ipsilateral renal agenesis is known as Herlyn-Werner-Wunderlich syndrome (Figure 13). The treatment for class U2 and U3c is metroplasty. It is also recommended in cases of arcuate uterus with repeated pregnancy loss.26,27
Hemi-uterus U4
A unilaterally formed uterus, which occurs as a result of a formation defect with an absent or incompletely formed contralateral part, is usually laterally deviated. It is sub-classified into subtypes a and b by the presence or absence (Figure 14) of a functional cavity in the contralateral component (rudimentary horn communicating or non-communicating). Laparoscopic removal of the rudimentary horn is advised if there is a functional cavity. Forty percent of hemi-uteri have associated renal anomalies.28
Aplastic uterus U5
An aplastic uterus is a formation defect with bilateral (Figure 15) or unilateral, complete or partially absent uterine cavity or rudimentary horn, with or without a cavity or uterine remnants. Presence (Figure 15) or absence of a functional cavity sub-classifies an aplastic uterus into subtypes a and b.
Fundal, body and cervix differentiation as well as endometrial-myometrial differentiation are not seen (Figure 2).
Failure of the Müllerian duct to develop leads to Müllerian agenesis. Parikh et al. state that the most common cause of primary amenorrhea is Müllerian agenesis.5 Uterovaginal aplasia or hypoplasia is referred to as Mayer-Rokitansky-Küster-Hauser syndrome. In type I or the typical form, there is isolated uterovaginal aplasia. Laparoscopy can identify Müllerian remnants as symmetric muscular buds and normal Fallopian tubes.29 In type II (Figure 16) or the atypical form, other upper urinary tract, vertebral, cardiac and otologic malformations are seen.29
Still unclassified cases U6
Rare anomalies or combined pathologies that do not comply correctly with one of the above six groups are categorised into unclassified (Figure 17). Ectopic Müllerian tissue anomalies such as an accessory-cavitating uterine mass30 and tricavitated uterus13 belong to this category.
Conclusion
The ESHRE and ESGE classification is an anatomical and embryological-based classification and includes cervical and vaginal anomalies. A volumetric T2-weighted MRI sequence such as T2 CUBE is the sequence of choice. Although the ESHRE classification is more accommodative than the ASRM classification, there are still a few unclassified anomalies. Magnetic resonance imaging acquired after the instillation of vaginal gel helps to clearly delineate the transverse and longitudinal vaginal septum. Knowledge of the various classifications, differentiating points, imaging characteristics, associated anomalies, syndromes and various available treatment options is vital for the radiologist to guide the treating experts to achieve the best patient outcome.
Acknowledgements
We thank Dr Prabu Dhanasingh and Dr Sunil Kumar for their contribution in figure and artwork preparation.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
D.J. was the project leader. D.J. and V.I. were responsible for experimental and project design. Both authors collected and reported the cases and wrote the manuscript.
References
1. Duncan SLB. Embryology of the female genital tract: Its genetic defects and congenital anomalies. In: Shaw RW, Soutter WP, Stanton SL, editors. Gynecology. Edinburgh: Churchill Livingstone, 1992; p. 3-21. [ Links ]
2. Graupera B, Pascual MA, Hereter L, et al. Accuracy of three-dimensional ultrasound compared with magnetic resonance imaging in diagnosis of Mullerian duct anomalies using ESHRE-ESGE consensus on the classification of congenital anomalies of the female genital tract. Ultrasound Obstet Gynecol. 2015;46(5):616-622. https://doi.org/10.1002/uog.14825 [ Links ]
3. Troiano RN, McCarthy SM. Mullerian duct anomalies: Imaging and clinical issues. Radiology. 2004;233(1):19-34. https://doi.org/10.1148/radiol.2331020777 [ Links ]
4. Grimbizis GF, Gordts S, Di Spiezio Sardo A, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013;28(8):2032-2044. https://doi.org/10.1093/humrep/det098 [ Links ]
5. Parikh RM, Nakum K, Kadikar GK, Gokhle AV. Mullerian anomalies: A cause of primary amenorrhea. Int J Reprod Contracept Obstet Gynecol. 2013;2:393-397. https://doi.org/10.5455/2320-1770.ijrcog20130926 [ Links ]
6. Mueller GC, Hussain HK, Smith YR, et al. Mullerian duct anomalies: Comparison of MRI diagnosis and clinical diagnosis. AJR Am J Roentgenol. 2007;189:1294-1302. https://doi.org/10.2214/AJR.07.2494 [ Links ]
7. Behr SC, Courtier JL, Qayyum A. Congenital pelvic abnormalities; imaging of Müllerian Duct Anomalies. Radiographics. 2012;32(6):E233-E250. https://doi.org/10.1148/rg.326125515 [ Links ]
8. Saleem SN. MR Imaging diagnosis of uterovaginal anomalies: Current state of the art. Radiographics. 2003;23(5):e13. https://doi.org/10.1148/rg.e13 [ Links ]
9. Reuter KL, Daly DC, Cohen SM. Septate versus bicornuate uteri: Errors in imaging diagnosis. Radiology. 1989;172(3):749-752. https://doi.org/10.1148/radiology.172.3.2528160 [ Links ]
10. Pellerito JS, McCarthy SM, Doyle MB, Glickman MG, DeCherney AH. Diagnosis of uterine anomalies: Relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology. 1992;183(3):795-800. https://doi.org/10.1148/radiology.183.3.1584936 [ Links ]
11. Carrington BM, Hricak H, Nuruddin RN, Secaf E, Laros RK, Hill EC. Mullerian duct anomalies: MR imaging evaluation. Radiology. 1990;176(3):715-720. https://doi.org/10.1148/radiology.176.3.2202012 [ Links ]
12. Grimbizis GF, Gordts S, Sardo A, et al. Reply: Are the ESHRE/ESGE criteria of female genital anomalies for diagnosis of septate uterus appropriate? Hum Reprod. 2014;29:868-869. https://doi.org/10.1093/humrep/deu002 [ Links ]
13. Di Spiezio Sardo A, Campo R, Gordts S, et al. The comprehensiveness of the ESHRE/ESGE classification of female genital tract congenital anomalies: A systematic review of cases not classified by the AFS system. Hum Reprod. 2015;30(5):1046-1058. https://doi.org/10.1093/humrep/dev061 [ Links ]
14. Lev-Toaff AS, Kim SS, Toaff ME. Communicating septate uterus with double cervix: A rare malformation. Obstet Gynecol. 1992;79:828-830. [ Links ]
15. Wai CY, Zekam N, Sanz LE. Septate uterus with double cervix and longitudinal vaginal septum: A case report. J Reprod Med. 2001;46:613-617. [ Links ]
16. Hundley AF, Fielding JR, Hoyte L. Double cervix and vagina with septate uterus: An uncommon Müllerian malformation. Obstet Gynecol. 2001;98:982-985. https://doi.org/10.1016/S0029-7844(01)01559-9 [ Links ]
17. Saygili-Yilmaz ES, Erman-Akar M, Bayar D, Yuksel B, Yilmaz Z. Septate uterus with a double cervix and longitudinal vaginal septum. J Reprod Med. 2004;49:833-836. [ Links ]
18. Patton PE, Novy MJ, Lee DM, Hickok LR. The diagnosis and reproductive outcome after surgical treatment of the complete septate uterus, duplicated cervix and vaginal septum. Am J Obstet Gynecol. 2004;190:1669-1675. https://doi.org/10.1016/j.ajog.2004.02.046 [ Links ]
19. Sadek SM, Ahmad RA, Atia H. Performance of the ESHRE/ESGE classification in differentiating anomalies of double uterine cavity in comparison with the ASRM classification. Middle East Fertil Soc J. 2016;21(2):75-81. https://doi.org/10.1016/j.mefs.2015.09.001 [ Links ]
20. Ludwin A, Ludwin I. Comparison of the ESHRE-ESGE and ASRM classifications of Mullerian duct anomalies in everyday practice. Hum Reprod. 2015;30(3):569-580. https://doi.org/10.1093/humrep/deu344 [ Links ]
21. Ludwin A, Ludwin I, Kudla M, Kottner J. Reliability of the European Society of Human Reproduction and Embryology/European Society for Gynaecological Endoscopy and American Society for Reproductive Medicine classification systems for congenital uterine anomalies detected using three-dimensional ultrasonography. Fertil Steril. 2015;104 (3):688-697. https://doi.org/10.1016/j.fertnstert.2015.06.019 [ Links ]
22. Mohseni MG, Hosseini SR, Salavati A, Dadgari S. Ureterocele associated with renal agenesia presented as a pelvic mass in an adult. Iran J Radiol. 2013;10(1):45-47. https://doi.org/10.5812/iranjradiol.10262 [ Links ]
23. Maas KL, Lipson SA, Hricak H. Ureteric bud remnant in two patients with renal agenesis: Diagnosis by MRI. J Comput Assist Tomogr. 1997;21(5):745-747. https://doi.org/10.1097/00004728-199709000-00016 [ Links ]
24. Calleja Escudero J, Amo Garcia A, Garrido Redondo M, Rodriguez Toves A, del Rio Dominguez F, Martinez Sagarra JM. Renal agenesis, cranial blind ureter and ureterocele. Report of a case. Arch Esp Urol. 1995;48(1):89-91. [ Links ]
25. Tuştaş Haberal E, Çekmez Y, Ulu İ, Divlek R, Göçmen A. Placenta percreta with concomitant uterine didelphys at 18 weeks of pregnancy: A case report and review of the literature. J Matern Fetal Neonatal Med. 2016;29(21):3445-3448. https://doi.org/10.3109/14767058.2015.1130819 [ Links ]
26. Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update. 2001;7(2):161-174. https://doi.org/10.1093/humupd/7.2.161 [ Links ]
27. Homer HA, Li TC, Cooke ID. The septate uterus: A review of management and reproductive outcome. Fertil Steril. 2000;73(1):1-14. https://doi.org/10.1016/S0015-0282(99)00480-X [ Links ]
28. Li S, Qayyum A, Coakley FV, Hricak H. Association of renal agenesis and Mullerian duct anomalies. J Comput Assist Tomogr. 2000;24(6):829-834. https://doi.org/10.1097/00004728-200011000-00001 [ Links ]
29. Strübbe EH, Willemsen WN, Lemmens JA, Thijn CJ, Rolland R. Mayer-Rokitansky-Küster-Hauser syndrome: Distinction between two forms based onexcretory urographic, sonographic, and laparoscopic findings. AJR Am J Roentgenol. 1993;160(2):331-334. https://doi.org/10.2214/ajr.160.2.8424345 [ Links ]
30. Jain N, Verma R. Imaging diagnosis of accessory and cavitated uterine mass, a rare Mullerian anomaly. Indian J Radiol Imaging. 2014;24(2):178-181. https://doi.org/10.4103/0971-3026.134411 [ Links ]
 Correspondence:
Correspondence:
Venkatraman Indiran
ivraman31@gmail.com
Received: 01 Aug. 2017
Accepted: 05 Feb. 2018
Published: 23 Apr. 2018














