Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Journal of Radiology
On-line version ISSN 2078-6778
Print version ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.21 n.1 Johannesburg 2017
http://dx.doi.org/10.4102/sajr.v21i1.1183
CASE REPORT
Extraosseous Ewing's sarcoma, a case report on a rare diagnosis in an 80-year-old woman with a large abdominal mass
Charlotte de WildeI; Alain BolsII; Ivo van den BergheIII; Kenneth CoenegrachtsIV
IDepartment of Radiology, Ghent University, Belgium
IIDepartment of Oncology, AZ St.-Jan Brugge-Oostende, Belgium
IIIDepartment of Pathology, AZ St.-Jan Brugge-Oostende, Belgium
IVDepartment of Radiology, AZ St.-Jan Brugge-Oostende, Belgium
ABSTRACT
Extraosseous or extraskeletal Ewing's sarcoma is a very rare mesenchymal soft tissue malignancy. We report on a case of abdominal swelling in an 80-year-old woman caused by a large intra-abdominal EES. This case report illustrates that Ewing's sarcoma can occur in adults and elderly, and highlights the importance of early diagnosis because of poor prognosis.
Introduction
This case report demonstrates the rare diagnosis of an extraskeletal Ewing sarcoma (EES) in an elderly woman with a large abdominal mass. EES is commonly diagnosed in a younger population, which makes our case very unusual. This article discusses the presentation and typical radiological appearance of extraskeletal Ewing sarcoma and the differential diagnoses with their radiological appearances.
Case report
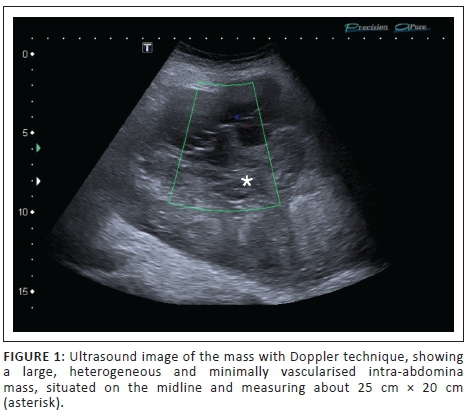
An 80-year-old female patient was referred by her general practitioner and presented at the radiology department for an abdominal ultrasound. She complained about painless abdominal swelling for several weeks. A firm intra-abdominal mass was palpable during clinical examination. The abdominal ultrasound showed a large, heterogeneous and minimally vascularised intra-abdominal midline mass, measuring about 25 cm × 20 cm (Figure 1).
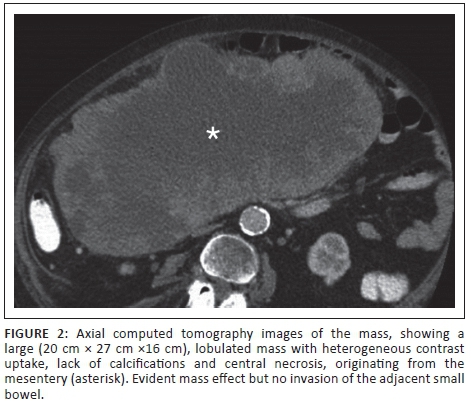
The ultrasound was followed by a computed tomography (CT) scan of the abdomen with oral and intravenous contrast agent. CT showed a large (20 cm × 27 cm ×16 cm) (Figure 2), lobulated mass with heterogeneous contrast uptake, lack of calcifications and central necrosis, probably originating from the mesentery. There was no evidence of invasion of the adjacent small bowel. No metastatic lesions were seen. An ultrasound-guided core biopsy was performed (Figure 3).

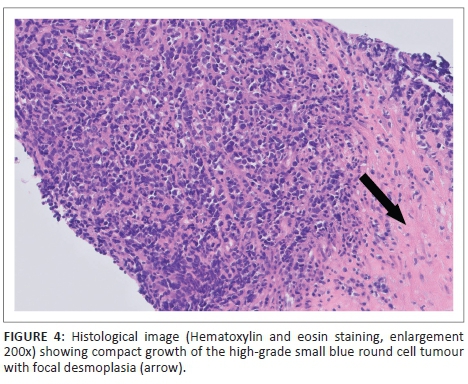
Microscopic examination of the biopsy sample revealed a high-grade small blue round cell tumour, immunohistochemically compatible with an extraskeletal Ewing's sarcoma (Figure 4). The diagnosis was confirmed with fluorescence in situ hybridisation (FISH) cytogenetic evaluation and immunohistochemistry staining, the latter showing positive CD 99 and synaptofysine staining (Figure 5).
Discussion
Ewing's sarcoma is a high-grade rounded cell sarcoma, which arises from both skeletal and extraskeletal mesenchymal cells with a t(11;22) chromosomal translocation. However, there are important differences between the extraosseous and the osseous type of Ewing's sarcoma. These differences mainly comprise age distribution, clinical presentation, prognosis, treatment and survival. EES is more common in adults, although usually in young adults in contrast to our case. Adults tend to have a worse prognosis than children with this presentation of Ewing's sarcoma. A possible explanation for the worse outcome in adults is the inability to tolerate the aggressive chemotherapy.1,2
It is important to recognise that approximately 20% of all cases of Ewing's sarcomas occur in patients older than 18 years and at least 50% of these patients have an extraskeletal presentation. The most prevalent extraskeletal sites are the chest (most common), the abdomen (both intra- and retroperitoneal), the soft tissues of the extremities (the gluteal region and the lower extremities are relatively common sites) and the head and neck region (most rare location).2,3,4
On CT, abdominal EESs show heterogeneous contrast enhancement with hypoattenuating areas corresponding to necrosis and high-density foci in cases of haemorrhage. Calcification is atypical, occurring in approximately 10% of tumours at presentation. When present, it appears faint and amorphous.2,4 Most abdominal EESs are unilateral and do not cross the midline, in contrast to our case.3
The radiological differential diagnosis for abdominal EES includes:
-
other peritoneal tumours such as lymphoma, peritoneal metastasis and lymph node metastases (often with associated retroperitoneal lymph node enlargement)
-
gastrointestinal stromal tumours (GIST) (gastric or small bowel GIST, extends exophytically from the gastrointestinal tract)
-
desmoid tumour (arising at the site of scarring from prior surgery)
-
other soft tissue sarcomas (like synovial sarcoma and rhabdomyosarcoma).4,5
Extraskeletal Ewing's sarcomas in adults are large tumours that metastasise to the lung and can invade adjacent organs, although they tend to displace adjacent structures rather than invade them. They are aggressive tumours, often with distant metastases and local recurrence and a 5-year survival rate of less than 50%.3
Patients with localised EES are treated aggressively with neoadjuvant chemotherapy, followed by surgery and in the event of inadequate surgical margins, post-operative radiotherapy. Molecular-targeted treatments are in development.2,3 The case discussed above was treated with neoadjuvant carboplatin-etoposide, followed by excision of the tumour and radiotherapy.
Conclusion
Extraskeletal Ewing's sarcomas are rare tumours and even more rare in the abdomen. They occur in an older age group compared to osseous Ewing's sarcoma, but are rare in the elderly. They should, however, be considered in the differential as this will help guide pathologists and clinicians in making the final diagnosis.
Ethical considerations
There were no ethical conflicts. This article does not contain any studies with human or animal subjects.
Acknowledgements
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
C.D.W. and K.C. performed the ultrasound and computed tomography scan on the patient. They followed up the histology results and the oncological treatment with I.V.d.B. and the oncological treatment with A.B., respectively.
References
1. Applebaum MA, Worch J, Matthay KK, et al. Clinical features and outcomes in patients with extraskeletal Ewing sarcoma. Cancer. 2011;117(13):3027-3032. https://doi.org/10.1002/cncr.25840 [ Links ]
2. Javery O, Krajewski K, O'Regan K, et al. A to Z of extraskeletal Ewing sarcoma family of tumors in adults: Imaging features of primary disease, metastatic patterns, and treatment responses. AJR Am J Roentgenol. 2011;197:W1015-W1022. https://doi.org/10.2214/AJR.11.6667 [ Links ]
3. Somarouthu BS, Shinagare AB, Rosenthal MH, et al. Multimodality imaging features, metastatic pattern and clinical outcome in adult extraskeletal Ewing sarcoma: Experience in 26 patients. Br J Radiol. 2014;87:20140123. https://doi.org/10.1259/bjr.20140123 [ Links ]
4. Huh J, Kim KW, Park SJ, et al. Imaging features of primary tumors and metastatic patterns of the extraskeletal Ewing sarcoma family of tumors in adults: A 17-year experience at a single institution. Korean J Radiol. 2015;16(4):783-790. https://doi.org/10.3348/kjr.2015.16.4.783 [ Links ]
5. Ulusan S, Koc Z, Kayaselcuk F. Gastrointestinal stromal tumours: CT findings. Br J Radiol. 2008;81(968):618-623. https://doi.org/10.1259/bjr/90134736 [ Links ]
 Correspondence:
Correspondence:
Charlotte de Wilde
charlotte.dewilde@hotmail.com
Received: 26 Jan. 2017
Accepted: 14 Mar. 2017
Published: 29 May 2017














