Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Journal of Radiology
versão On-line ISSN 2078-6778
versão impressa ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.20 no.1 Johannesburg 2016
http://dx.doi.org/10.4102/sajr.v20i1.1034
ORIGINAL RESEARCH
Adequacy of ultrasound reports in patients presenting with obstructive jaundice at a tertiary hospital radiology department
Nondumiso Dlamini; Matthew Goodier
Department of Radiology, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: Patients with obstructive jaundice require a stepwise approach to investigation and management. Ultrasound (US) is the initial screening modality of choice and has been shown to be accurate in demonstrating the presence of dilated bile ducts, as well as the level and cause of obstruction. For adequate radiological communication to the clinician, degree of bile duct dilatation, level of obstruction, appearance of the transition zone and cause of obstruction must be reported. However, without a structured reporting method, much of this information may be omitted.
OBJECTIVES: The aim of the study was to investigate the adequacy of US findings in patients with obstructive jaundice, as documented, without standardised reporting.
METHODS: A retrospective chart review of 130 US reports of adult patients presenting at Grey's Hospital US Department with a clinical assessment of obstructive jaundice was conducted. Data for the period January to December 2013, were analysed. US reports of patients with dilated bile ducts were assessed for report adequacy by looking at four important clinical factors, that is, the degree of bile duct dilatation, the level of obstruction, the appearance of the transition zone and the cause of the obstruction.
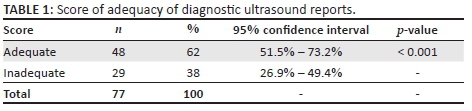
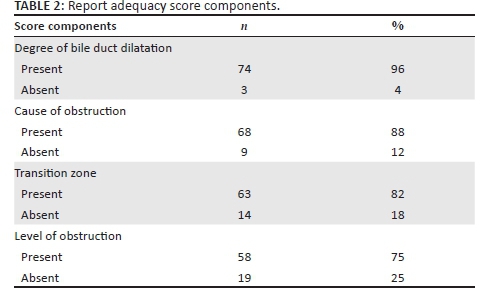
RESULTS: A report adequacy score was assessed in 79 patients with dilated bile ducts; however, two reports were excluded because of obscuration by gas. There was a high level of report inadequacy (38%) without the use of a structured reporting template. The level of obstruction was the most common component missing from the reports (25%), followed by the appearance of the transition zone (18%) and cause of obstruction (12%).
CONCLUSION: We propose the use of an US report template for obstructive jaundice patients in order to ensure comprehensive reporting. Structured radiological reporting will improve the method of communication between clinicians and radiologists, thus improving the quality of patient care.
Introduction
Jaundice is a commonly encountered condition in clinical practice.1,2 Differentiating between obstructive (surgical) and non-obstructive (medical) jaundice can be achieved clinically by using a combination of clinical signs, symptoms and biochemical markers.2,3,4,5,6,7 It is important to differentiate between the two conditions because patients with obstructive jaundice usually require surgical or radiological intervention.3,8 Ultrasound (US) is the initial screening modality of choice for patients with obstructive jaundice as it assists in the cost-effective management of these patients by determining the need for further imaging.2,3,4,5,8,9 In order to achieve these goals, US reports of these patients should include the presence and degree of bile duct dilatation and the level and cause of obstruction.3,8
Radiology reports are an important method of communication between the radiologist and the referring clinician.10 Structured radiological reporting has been shown to improve the quality of radiological reports. These reports can be integrated with the picture archiving and communication system (PACS), thus improving the service provided by the radiology department and also improving the efficiency of communication between the radiologist and the referring clinician.10,11,12,13
Several studies have been performed to demonstrate the accuracy of US in the assessment of bile duct dilatation and level and cause of obstruction.4,8,14 However, no previous studies have specifically investigated US report adequacy in patients with biliary obstruction. We investigated the quality of information documented in the US reports of patients with obstructive jaundice in our institution without any standardised form of reporting, to assess their communication value to the referring clinician.
Objectives
The objectives of the study were:
• to determine the diagnostic adequacy of US reports by application of a novel scoring system and
• to compare US report adequacy among practitioners of varying levels of experience (sonographers, junior doctors, senior doctors and consultants).
Methods
Our study is a retrospective chart review of US reports of adult (≥ 18 years) patients who presented at Grey's Hospital US Department with a clinical assessment of obstructive jaundice specified on the request form. This included documentation of the presence of clinical jaundice with other additional symptoms such as dark urine, pale stool, right upper quadrant pain and pruritus or documentation of biochemical markers suggestive of obstructive jaundice on liver function tests (LFTs), that is, elevated alkaline phosphatase, gamma-glutamyl transpeptidase and bilirubin.
Request forms of patients who fulfilled our inclusion criteria were obtained from the US Department filing system. US reports of the selected patients were retrieved from the Radiology Information System and PACS. The US examinations were performed on the Toshiba Aplio XG and Philips HD7 XE machines, using a wide-range, low-frequency curved-probe of 3-5 MHz and the C5-2 probe, respectively. The biliary tree was assessed trans-abdominally, using longitudinal and transverse views with the patient in the supine or right anterior oblique position. The bile ducts were considered dilated if the internal diameter of the common bile duct (CBD) was > 7 mm or if the intrahepatic bile ducts were > 2 mm in diameter. All US examinations were performed during working hours. In order to maintain confidentiality, each patient was allocated a study number. Data for a period of 12 months (January to December 2013) were collected. A total number of 130 US reports were analysed. Ethical clearance was obtained from the University of KwaZulu-Natal Biomedical Research Ethics Committee.
Data were collected from the US request forms and US reports using designed data collection sheets, with key parameters pertaining to the aim of the study. Reports of patients with the presence of dilated bile ducts on US were scored by their level of completeness. A report was considered adequate if it mentioned all four of the following:
• the degree of bile duct dilatation;
• the level of obstruction;
• the appearance of the transition zone; and
• the cause of obstruction.
A report missing any of the above items was considered inadequate. Data were analysed using Stata v13 software.
US examinations were performed by radiology consultants, registrars, medical officers (MOs) and sonographers. Report adequacy scores among the different ranks (sonographers, junior doctors [both MOs and registrars with less than 2 years of experience working in a radiology department], senior doctors [both MOs and registrars with more than 2 years of experience working in a radiology department] and consultants) were compared. US reports were also assessed for recommendation of further imaging by the personnel performing the US.
Results
We reviewed 130 US reports of adult patients (age range of 20-89 years; mean 51.3). Ninety were female and 40 were male patients. Of these patients, 51 (39.2%) did not have dilated bile ducts on US, and 79 (60.8%) had dilated bile ducts. Of the 79 reports, 2 (2.5%) were excluded from the report adequacy score assessment because they mentioned the limitation of US examination because of obscuration by gas resulting in difficulty to assess the site of obstruction. Sixty-two percent (48/77) of reports were found to be adequate and 38% (29/77) were inadequate (Table 1). The level of obstruction was the most common component missing from the reports (25%), followed by appearance of the transition zone (18%) and the cause of obstruction (12%) (Table 2). The degree of bile duct dilatation was the most often reported component with 96% of reports commenting on this finding.
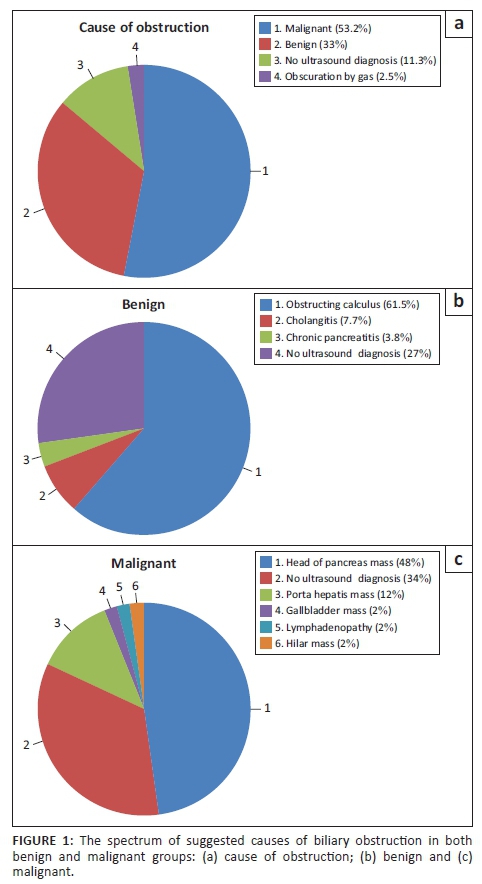
US findings were completely normal in 37% (19/51) of the patients without dilated bile ducts. Cholelithiasis was found in 59% (30/51) of these patients. Of the 79 patients with dilated ducts, 33% (26/79) of the reports suggested a benign cause of obstruction and 53.2% (42/79) reports suggested a malignant cause. Of the 42 patients with a malignant cause of obstruction, 57.1% (24/42) were female patients and 42.9% (18/42) were male patients (age range was 32-89; mean of 60.3). Of the 26 patients with a benign cause of obstruction, 92.3% (24/26) were female patients and 7.7% (2/26) were male patients (age range, 20-79; mean of 43.4). The spectrum of findings is displayed on Figure 1.
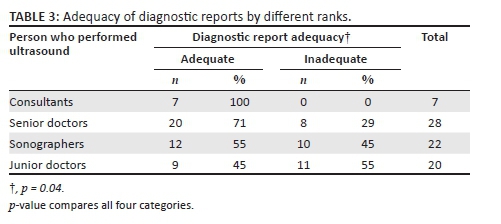
In the total 130 patients who we assessed, 26.9% (35/130) cases were reported by sonographers, 29.2% (38/130) cases were reported by junior doctors, 36.2% (47/130) cases were reported by senior doctors and 7.7% (10/130) cases were reported by consultants (Table 3). Table 3 demonstrates the difference in the report adequacy score of US reports in patients with dilated bile ducts, which demonstrates a significant difference in the level of adequacy of US reports among different ranks, with p = 0.04.
Recommendation for further investigation by the person performing the US examination was uncommon among all the ranks. Junior doctors recommended additional investigation most often (25%) and senior doctors least often (11%). Sonographers and consultants both recommended additional investigations in 14% of reports. None of these group differences were statistically significant.
Discussion
The aim of radiological investigation in patients with obstructive jaundice is to confirm the presence of dilated bile ducts, demonstrate the level and cause of obstruction and assist in assessing tumour resectability in malignant cases.2,3,4,5,6,7,8,9 US has been shown to be accurate in demonstrating the presence of dilated bile ducts with a sensitivity of 55-95% and specificity of 71-96%.1,5 The sensitivity of US continues to increase in determining the cause and level of obstruction with improved image resolution, imaging technique and use of tissue harmonics, all contributing to enhanced image quality.2,4,5,6,7,8 US is reported to have a lower sensitivity in demonstrating the cause of obstruction with accuracy of 23-88%, particularly in the distal CBD.1,2,5,6,7,8,9 False-negative results are seen in patients with obstructive jaundice without dilated bile ducts on US and when there is obscuration of the extrahepatic bile ducts by gas.2,5,6,7 US is used as the initial screening modality in patients with obstructive jaundice because it does not make use of ionising radiation, is easily available, is non-invasive and is inexpensive.1,2,3,4,5,7,8,9,14 Because of the risk of mortality and morbidity and high cost, invasive procedures such as endoscopic retrograde cholangiopancreatography and percutaneous transhepatic cholangiography are usually reserved for therapeutic intervention and tissue diagnosis.2,3,4,5,7,9
Several studies have demonstrated the accuracy of US in the assessment of bile ducts dilatation and level and cause of obstruction.4,8,14 However, no previous studies have specifically investigated the adequacy of US reports in patients with biliary obstruction. We investigated the quality of information documented in US reports at our institution in order to assess their communication value to the referring clinician. An adequate report would mention all four clinical factors mentioned above. Our study demonstrates a high inadequacy rate of 38% of US reports in patients with obstructive jaundice who had dilated bile ducts on US (Table 1).
Radiology reports are the main means of communication between the radiologist and the referring clinician, and they should be clear and precise and address the question raised by the referring clinician.10,11,12,15 The components of a comprehensive radiological report should include patient demographics, imaging procedure descriptions, relevant clinical information, findings, pertinent negative findings, study limitations, comparison studies and reports, impression, differential diagnosis and follow-up or additional diagnostic studies to clarify or confirm the impression.11,12,15 Structured radiology reporting has been shown to enhance the standard of reporting by improving the quality and consistency of radiology reports that are reproducible. This also results in better patient care and decreases cost by eliminating transcription and thus reducing report turnaround time, resulting in a shorter hospital stay.10,11,12,13 Additionally, there is complete documentation of information because the request form, images and the report findings are archived and retrieved electronically.10,11,12 Structured reports can be used by radiologists for teaching, research, clinical quality improvement and for billing.12 The Radiological Society of North America established a radiology report committee that creates a library of report templates for different modalities and procedures, which is aimed at standardising radiological reports using structured reporting.11,12
US has been shown to have low sensitivity in determining the cause of biliary obstruction especially in the distal CBD, mainly because US is dependent on several factors such as operator experience, technical factors and patient body habitus.2,3,14 In our study, only 2.5% (2/79) of reports of patients with dilated bile ducts documented the limitation of the examination because of obscuration by gas. This percentage is significantly lower than the results of the study by Tsang et al., which demonstrated that up to 49% of their patients with obstructive jaundice had limited US examination because of obscuration by gas and an US diagnosis could not be made.1 Turning the patient to an oblique, lateral or upright position or giving water orally and allowing at least 4 hours of fasting before US examination could improve visualisation of the biliary system.3,6,7,14 In our study, lack of documentation of the limitations of US examination, for example, obscuration by gas or patient body habitus, could be one of the reasons for the low number of adequate reports.
The level of obstruction was the most common component missing from the reports at 25%; followed by transition zone at 18% and cause of obstruction at 12% (Table 2). Lack of documentation of limitations of the US study could also be related to the relatively low adequacy in documentation of the level of obstruction, the appearance of the transition zone and cause of obstruction at 75%, 82% and 88%, respectively (Table 2). The importance of documenting the level of obstruction is that it determines the approach of the therapeutic or diagnostic intervention, as more proximal obstruction is better approached percutaneously and distal obstruction endoscopically.2,3,6 Carefully assessing the transition zone gives an indication of the most likely diagnosis, for example, benign strictures usually taper gradually and malignant strictures usually demonstrate an abrupt cut-off (Figure 2).6,9 This information is vital to ensuring the most efficient and thus cost-effective pathway for further investigation and management of the patient.
There were a higher number of inadequate reports among junior doctors and sonographers at 55% and 45%, respectively (Table 3). One of the reasons implicated for poor quality of radiology reports is the lack of supervision and insufficient training in reporting skills for junior staff.11 This poses a challenge in a resource-limited environment like ours, with limited staff. According to Hall et al., lack of formal instruction for residents in reporting skills is because of a lack of consensus about what constitutes a good radiology report.15 In a study by Tsang et al., it was demonstrated that US report auditing with implementation of US skills training improves the accuracy rate of US reports of patients with obstructive jaundice.1 Recommendation of further imaging or other diagnostic tests and intervention is part of an efficient radiological report and helps facilitate further imaging and management of patients, especially when the US report is inconclusive.8,9 Our study demonstrates an overall low-frequency of recommendation for further investigation by the person performing the US examination, ranging from 11% to 25%.
Malignancy was the most common suggested cause of obstruction in our patients, at 53.2% (42/79), which is compatible with other studies4,8,14 (Figure 1). The most common malignant cause of obstruction was a pancreatic head mass at 48%, which correlates with findings from other studies.1,5,14 Interestingly, we found a female predominance of 57.1% (24/42) in the malignant cases. Malignant causes of biliary obstruction including head of pancreas carcinoma are documented to be more common in male patients.8,14 The older age group, age range 32-89 and a mean of 60.3 in our patients, correlates with findings from other studies that the incidence of malignant cause of obstruction increases with advancing age.5,8 Figure 3 illustrates a malignant cause of obstruction secondary to invasion of the CBD by gallbladder carcinoma.
The most common benign cause of obstruction was an obstructing calculus (61.5%), with a female predominance of 92.3% (24/26). There was no US diagnosis in 27% (7/26) of patients with benign cause of obstruction (Figure 1). These findings also correlate with other studies, which indicate that choledocholithiasis is the most common benign cause of biliary obstruction.1,4,9,14 The younger age group with a mean age of 43.4 in our patients also correlates with findings in other studies.8 Figure 4 illustrates a benign cause of obstruction because of choledocholithiasis.
Concluding recommendations
Effective investigation and management of patients with biliary obstruction usually requires multimodality imaging with a stepwise approach of several imaging and therapeutic techniques.3,4,7,8,9 Poor planning and strategising when imaging and managing patients with biliary obstruction may lead to redundant investigations or unnecessary imaging, which will result in increased cost, delayed diagnosis and increased hospital stay and can result in unnecessary morbidity and possibly mortality.3 Several algorithmic approaches have been described, including guidelines from the American College of Radiology (ACR) appropriateness criteria, and they all use US as an initial imaging modality.3,5,9 Figure 5 illustrates our proposed referral approach for further investigation in patients with biliary obstruction confirmed on US in our department. This approach is modified from O'Connor et al., Krige et al. and the ACR appropriateness criteria.3,5,9 We also propose a standard reporting template for US reporting in patients with biliary obstruction in our department (Appendix 1). The impact of this standardised reporting guide on US report adequacy in our institution will be a topic for further research in our department.
Limitations of the study
This study was performed in a single tertiary institution with limited radiology staff. This could result in bias; therefore, our results cannot be generalised. Inherent limitations include potential biases resulting from exclusion of request forms that were illegible, patients with mixed picture on LFT results and patients who had inadequate information provided on the request forms.
Conclusion
Our study demonstrates that at our institution there is a low rate of US report adequacy for patients with obstructive jaundice and a very low rate of recommendation of appropriate further imaging. In an attempt to improve this, we encourage the use of a standard template for US reporting for patients with biliary obstruction as well as a protocol directing further investigation. The impact of this standardised reporting guide on US report adequacy in our institution will be a topic for further research in our department.
Acknowledgements
The authors thank Catherine Connoly for her assistance with data analysis.
Competing interests
The authors declare that they have no financial or personal relationships which may have inappropriately influenced them in writing this article.
Authors' contributions
N.D. was the primary investigator and prepared the manuscript, M.G. was the supervisor for the project, made conceptual contribution and was involved with manuscript editing.
References
1. Tsang YHA, Lau KCH, Tee LMF, Kan E. Performance of ultrasound in evaluating patients with obstructive jaundice. Poster session presented at: European Congress of Radiology 2013. http://dx.doi.org/10.1594/ecr2013/C-1730 [ Links ]
2. Karki S, Joshi KS, Regmi S, Gurung RB, Malla B. Role of ultrasound as compared with ERCP in patient with obstructive jaundice. Kathmadu Univ Med J. 2013;11(43):237-240. [ Links ]
3. Krige JEJ, Beningfield SJ, Shaw JM. Modern imaging in patients with obstructive jaundice. CME [serial online]. [ Links ] 2007 [cited 2016 Mar 21]; 25(7):328-331. Available from: http://www.ajol.info/index.php/cme/article/download/43782/27303
4. Ghimire R, Lohani B, Pradhan S. Accuracy of ultrasonography in evaluation of level and cause of biliary obstruction: A prospective study. Kathmandu Univ Med J. 2005;3(1):17-21. [ Links ]
5. Lalami T, Couto CA, Rosen MP, et al. ACR appropriateness criteria Jaundice. J Am Coll Radiol. 2013;10(6):402-409. http://dx.doi.org/10.1016/j.jacr.2013.02.020 [ Links ]
6. Baron RL, Tublin ME, Peterson MS. Imaging the spectrum of biliary tract disease. Radiol Clin North Am. 2002;40(6):1325-1354. http://dx.doi.org/10.1016/S0033-8389(02)00045-3 [ Links ]
7. Rudralingam P, Sukumar SA. Imaging of jaundiced adult. Imaging. 2013;22:1-16. http://dx.doi.org/10.1259/imaging/51415473 [ Links ]
8. Pandit SP, Panthi M. Ultra-Sonographic prediction of the causes & level of obstruction in the diagnosis of obstructive jaundice. Postgrad Med J NAMS [serial online]. 2011 [cited 2016 Mar 21]; 11(2):8-10. Available from: http://www.pmjn.org.np/index.php/pmjn/article/viewFile/53/52
9. O'Connor OJ, O'Neill S, Maher MM. Imaging of biliary tract disease. AJR. 2011;197(4):W551-W558. http://dx.doi.org/10.2214/ajr.10.4341 [ Links ]
10. Naik SS, Hanbidge A, Wilson SR. Radiology reports: Examining radiologist and clinician preferences regarding style and content. AJR. 2001;176(3):591-598. http://dx.doi.org/10.2214/ajr.176.3.1760591 [ Links ]
11. Govender N, Andronikou S, Goodier MDM. Adequacy of paediatric renal tract ultrasound requests and reports in a general radiology department. Pediatr Radiol. 2012;42(2):188-195. http://dx.doi.org/10.1007/s00247-011-2259-0 [ Links ]
12. Kahn CE Jr, Langlotz CP, Burnside ES, et al. Toward best practices in radiology reporting. Radiology. 2009;252(3):852-856. http://dx.doi.org/10.1148/radiol.2523081992 [ Links ]
13. Berman GD, Gray RN, Lui D, Tyhurst JJ. Structured radiology reporting: A 4 - year case study of 160,000 reports. Paper presented at: Integrating the Healthcare Enterprise (IHE) Symposium of the RSNA 2001 Annual Meeting; Nov 25-30 [homepage on the Internet]. [ Links ] [cited 2016 Mar 21]. Available from: http://www.structuredreporting.com/structurad-rsna-01.pdf
14. Al-Obaid S, Al- Hilli MRA, Fadhel AA. The role of ultrasound and magnetic resonance imaging in the diagnosis of obstructive jaundice. Iraqi Postgrad Med J. 2007;6(1):7-17. [ Links ]
Hall FM. Language of the radiology report: Primer for residents and wayward radiologists. AJR. 2000;175(5):1239-1242. http://dx.doi.org/10.2214/ajr.175.5.1751239 [ Links ]
 Correspondence:
Correspondence:
Nondumiso Dlamini
nnmdlamini@hotmail.com
Received: 12 May 2016
Accepted: 28 July 2016
Published: 22 Sept. 2016















