Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Journal of Radiology
versão On-line ISSN 2078-6778
versão impressa ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.20 no.1 Johannesburg 2016
http://dx.doi.org/10.4102/sajr.v20i1.990
ORIGINAL RESEARCH
http://dx.doi.org/10.4102/sajr.v20i1.990
Assessment of the impact of application of single-photon emission computed tomography and SPECT-CT on lesion categorisation in bone scintigraphy
Garba H. YunusaI; Anita BrinkII, III
INuclear Medicine Division, Department of Radiation Medicine, University of Cape Town, South Africa
IINuclear Medicine Division, Department of Paediatrics, University of Cape Town, South Africa
IIIRed Cross Memorial Children's Hospital, Cape Town, South Africa
ABSTRACT
OBJECTIVES: To assess initial experience with the use of a new single-photon emission computed tomography-computed tomography (SPECT-CT) in the evaluation of lesions
METHODS: The folder number, radiopharmaceutical used and type of scan of patients examined with a new Siemens T6 SPECT-CT between 02 April 2016 and 31 December 2013 were retrieved. The number of 99mTc-MDP bone scans was sufficient for a detailed analysis. The scans were re-processed and reported by the observer before he was given any clinical information. Whole body planar, whole body planar plus SPECT and whole body planar plus SPECT-CT images were assessed successively in three separate sessions at least 2 weeks apart. At each session, the certainties of detection, localisation and categorisation of each lesion were recorded
RESULTS: A total of 539 lesions were seen on the whole body, SPECT and computed tomography (CT) images in 133 patients. The whole body images showed no lesions in 3 patients and 378 lesions in 130 patients. SPECT detected 122 additional lesions in 79 patients. Thirty-nine (12.2%) lesions were seen only on CT in 32 (24.1%) patients. For the 261 lesions seen on the planar images in the SPECT field of view, lesion detection was definite in 233 (89.3%), localisation definite in 151 (57.9%) and categorisation definite in 123 (47.1%) lesions. On the SPECT, definite lesion detection, localisation and categorisation were recorded, respectively, for 259 (99.2%), 228 (87.4%) and 176 (67.4%) of the 261 lesions. Lesion detection, localisation and categorisation certainties were definite for 100%, 99.1% and 94.7% of the SPECT-CT lesions, respectively
CONCLUSION: SPECT markedly improves lesion detection and localisation, and CT enhances lesion categorisation
Introduction
The use of hybrid imaging consisting of single-photon emission computed tomography (SPECT) and X-ray transmission computed tomography (CT) scan is increasing globally. It has the advantage of providing functional and morphologic information for a given lesion. Radionuclide imaging has high sensitivity early in the disease before morphological changes become visible on other imaging modalities.1 The addition of CT provides morphological information with high spatial resolution. The combination of SPECT and CT has improved staging of disease as well as the prognostic and treatment monitoring potentials of the functional and metabolic information provided by conventional nuclear medicine examinations.2,3
Over the years, the use of SPECT-CT has been shown to accurately reclassify lesions previously classified as indeterminate on planar and SPECT imaging in both skeletal and non-skeletal nuclear medicine examinations with certainties of 88%-100%.4,5,6,7 However, the limitations in previous studies included the low resolution of the CT used which did not reveal the exact anatomical sites of abnormal radiotracer accumulation, and the prolonged CT acquisition time of 10-15 min by the dual slice CT scanners that resulted in increased patient motion and degradation of image quality.8 These factors have implications on the observer's confidence. Prolonged acquisition time and poor spatial resolution have been addressed by the recent introduction of multi-slice CT scanners in newer versions of the SPECT-CT systems.7,8 Therefore, the use of a faster higher resolution CT may improve observer's confidence.
A new SPECT machine integrated with a helical 6-slice CT was installed in the Department of Nuclear Medicine at Groote Schuur Hospital in March 2012. The objectives of this study were to assess the initial experience with the use of SPECT-guided CT in the evaluation of lesions, the impact of SPECT and addition of 6-slice CT in SPECT-CT on lesion categorisation, and the difference between the use of SPECT alone and fused SPECT-CT in lesion localisation and categorisation.
Methods
Approval for the study was obtained from the Research Ethics Committee of the Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital. All of the scans were done for clinical purposes and the initial reports issued used for patient management. Patients' confidentiality was observed throughout the study by the use of a coding system.
The folder number, radiopharmaceutical used and type of scan of all patients examined on the new stand-alone Siemens T6 SPECT-CT (Siemens Medical Solutions SW, Erlangen) machine between 02 April 2012 and 31 December 2013 were retrieved from the electronic archives of the Nuclear Medicine Department. A filter was then applied to identify all bone scans for which SPECT-CT was performed. In patients who had multiple studies, only the first study was included.
Each patient had planar whole body and selected static images. SPECT and subsequently CT images of the region of clinical interest were recorded depending on the abnormalities seen on the initial images or the indication for the study as deemed fit by the supervising nuclear medicine registrar or consultant at the time of image acquisition.
Whole body images were acquired using a low-energy high-resolution collimator with a matrix size of 256 × 256 and a scan speed of 14 cm/s. SPECT images were obtained using a 128 × 128 matrix with 25 s per step acquiring 64 projections with 180° rotation for each gamma camera head. CT images were acquired using a low-dose protocol without intravenous contrast administration. The low-dose CT parameters used were: 2.5 mAs-30 mAs, 120 kV, slice thickness of 1.25 mm-5 mm and pitch of 1.2-1.5.
SPECT images were reconstructed using the Flash 3D ordered subset expectation maximisation (OSEM) iterative reconstruction algorithm in four subsets and eight iterations, and smoothed with a spatial Gaussian filter 6.0 (FWHM). The CT images were reconstructed using high-resolution reconstruction algorithms (B08s kernel) while the images were viewed using the Siemens B80s kernel, for bone and B31s kernel for soft tissues.
For the purposes of this study, all examinations were re-processed and reported on the Siemens (Syngo VE32B, 2008, Siemens Medical Solutions, SW, Erlangen) and Hermes (version V1.0, 2005, Hermes Medical Systems, Sweden) physicians' workstations by a single observer who is a qualified radiologist and a nuclear medicine senior registrar. During the reconstruction and review of the images for this study, the observer was blinded to the history, clinical examination findings, laboratory and histology results as well as the previous reports issued. A four-point score (unknown, possible, probable or definite) was assigned for each lesion for the certainty of lesion detection, localisation and categorisation. Lesion 'detection' refers to visualisation of the lesion; 'localisation' refers to its anatomical location, while categorisation refers to ascribing the lesion to a specific morphology, pathology or physiological process. The lesions were assessed successively in separate reading sessions on planar, planar plus SPECT and planar plus SPECT-CT images with at least two weeks in between the sessions. The information on patient demographics and indications for the study were made available for the observer.
Data analysis was performed on per lesion and per patient basis. Assessments were made on per lesion and per patient bases for lesion detection, localisation, and categorisation. Analysis of levels of certainty for lesion detection, localisation and categorisation was made for planar, planar plus SPECT and planar plus SPECT-CT.
Results
Within the period under review, from 02 April 2012 to 31 December 2013, 241 SPECT-CT scans were done. After exclusion of 50 follow-up scans, four technically poor-quality studies and two with an incomplete data set, 185 studies were left for analysis.
The 133 patients referred for 99mTc-MDP bone scintigraphy comprised 92 (69.2%) females and 41 (30.8%) males with a mean age of 53.3 ± 15.7 years. The majority of the patients were referred for metastatic survey (42.9%), or because of musculoskeletal pain (29.3%) or suspected infection and/or inflammation (16.5%).
Lesion detection: A total of 539 lesions were seen on the whole body, SPECT and CT images (Table 1). There were three patients in whom no lesions were seen on the whole body images. SPECT and SPECT-CT were done because of clinical information: one patient was a 49-year-old female with breast carcinoma who complained of back pain; the second patient was a 28-year-old female with three month history of wrist pain, while the third patient was a 39-year-old female with history of injury to the right knee, four weeks prior to presentation. In the remaining 130 patients, 378 lesions were detected on the whole body images, 261 (69.0%) lesions within the field of view (FOV) of the SPECT images. Of the total number of lesions detected on SPECT, 122 (31.9%) were not seen on the whole body images. These additional lesions were detected in 79 patients. SPECT-CT detected 318 lesions, 39 (12.2%) of which were seen only on CT in 32 (24.1%) patients.
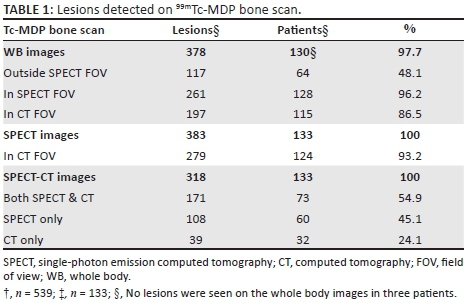
Lesion detection, localisation and categorisation certainty: For the 261 lesions seen on the planar images in the SPECT FOV, lesion detection was definite in 233 (89.3%), localisation was definite in 151 (57.9%) and categorisation was definite in 123 (47.1%) lesions (Tables 2, 3 and 4). On the SPECT, definite lesion detection, localisation and categorisation were recorded for 259 (99.2%), 228 (87.4%) and 176 (67.4%) of the 261 lesions, respectively.
On SPECT, out of the 383 lesions detected the certainty of lesion detection, localisation and categorisation were definite for 381 (99.5%), 328 (85.6%) and 267 (69.7%) lesions, respectively. For the 279 SPECT lesions seen in the CT FOV the lesion detection, localisation and categorisation was definite in 279 (100%), 276 (98.9%) and 262 (93.9%) lesions, respectively.
Lesion detection certainty was definite for all the 318 (100%) SPECT-CT lesions, while lesion localisation and categorisation certainties were definite in 99.1% and 94.7% of the lesions, respectively.
Of the 42 lesions categorised as indeterminate on planar, 20/42 (47.6%) and 35/42 (83.3%) were re-categorised following the addition of SPECT and SPECT-CT, respectively.
Discussion
This study reports the initial experience with new multi-slice SPECT-CT scanner as well as the impact of the addition of SPECT with and without a low-dose CT in the evaluation of lesions in patients referred for 99mTc-MDP bone scintigraphy.
SPECT not only improved the ability of radionuclide imaging to detect lesions by revealing more lesions, it also increased observer's confidence regarding lesion localisation. This is in agreement with earlier reports that showed SPECT is more sensitive than planar in detecting and localising lesions, particularly vertebral lesions with a 20%-50% increase in lesion detection.1,9,10,11,12 The addition of SPECT has been shown to increase the accuracy of lesion categorisation by improving localisation, especially in complex skeletal structures such as spine, skull and pelvis.1,11,12,13 In this study, the addition of SPECT has markedly improved the observer's confidence with regard to lesion detection, localisation and categorisation by increasing certainty when compared with planar imaging.
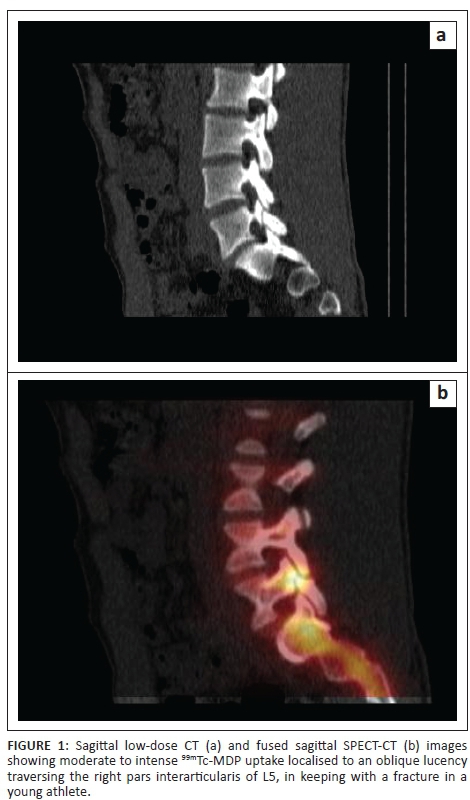
The addition of CT detected more lesions in a quarter of the patients while SPECT-CT markedly increased the interpreter's confidence with respect to lesion localisation and categorisation in comparison with SPECT and planar images (Figures 1 and 2). This agrees with the reports from other studies.2,4,5,6,7,14,15 In addition, some of these studies reported marked reduction of indeterminate lesions from a rate of between 48% and 72% using whole body planar scintigraphy with or without SPECT, to a rate between 0% and 15%.4,5,6 The current study showed a reduction in the indeterminate lesion rate among patients referred for 99mTc-MDP bone scintigraphy from 21.3% on planar alone to 11.2% and 3.6% following the addition of SPECT and SPECT-CT, respectively. While the proportion of SPECT-CT indeterminate lesions in this study is similar to that found in the study reported by Palmedo et al.,15 the lower rate found on the planar images in the current study may be due to the criteria used when referring patients for scintigraphy.
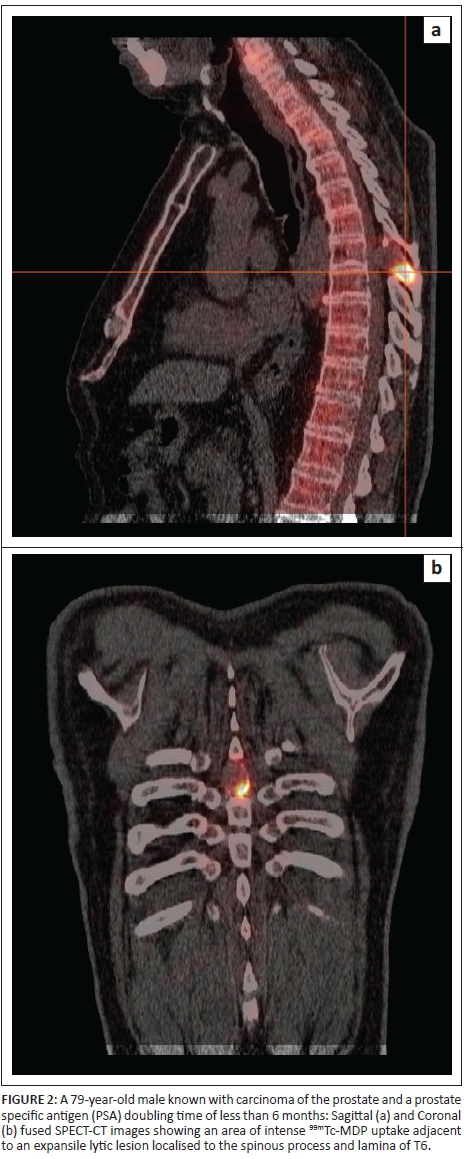
The CT component of the hybrid imaging SPECT-CT systems can assist in the diagnosis of benign skeletal findings, such as osteophytes or degenerative changes, or haemangiomas causing abnormal tracer uptake in patients referred for metastatic survey. However, it is important to note that foci of increased tracer uptake on bone scintigraphy due to metastatic bone lesions may not show any morphologic abnormality on CT. Likewise, lytic bone lesions with increased tracer uptake on bone scintigraphy may only be visualised on CT after they have destroyed 50-75% of the trabecular bone.1,3,4,11Therefore, under these circumstances the lack of anatomical abnormalities despite abnormal tracer uptake suggests medullary disease, and hence SPECT-CT improves specificity. Improved lesion categorisation on SPECT-CT makes a difference with regard to patient management decisions especially in patients referred for skeletal survey for metastases or musculoskeletal pain in patients with known malignancy.4,5,6,7,11,15
Some of the limitations of this study include the retrospective nature of the study as well as the lack of independent standards such as histological correlation, or clinical or imaging follow-up.
Conclusion
In conclusion, this study is consistent with prior research that found SPECT improved lesion detection and observer's confidence regarding lesion localisation and that SPECT-CT has a marked impact on lesion categorisation as well as improved observer's confidence. Our study thus adds to the existing body of literature on the incremental value of SPECT-CT in skeletal pathology. Better lesion categorisation has important implications on patient management decision especially among cancer patients referred for bone scintigraphy for suspected skeletal metastases or musculoskeletal pain.
Acknowledgements
The authors acknowledge the support of Prof. M.D. Mann for his invaluable contribution during the design and conduct of this study. They also thank Dr T. Kotze, the head of Nuclear Medicine at Groote Schuur Hospital, for the support throughout the period of the study.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
G.H.Y. was responsible for study conception, design, data analysis and manuscript writing. A.B. made conceptual contributions and reviewed the manuscript.
References
1. Horger M, Bares R. The role of single-photon emission computed tomography/computed tomography in benign and malignant bone disease. Semin Nucl Med. 2006;36(4):286-294. http://dx.doi.org/10.1053/j.semnuclmed.2006.05.001 [ Links ]
2. Jacene HA, Goetze S, Patel H, Wahl RL, Ziessman HA. Advantages of Hybrid SPECT/CT alone. Open Med Imag J. 2008;2:67-9.http://dx.doi.org/10.2174/1874347100802010067 [ Links ]
3. Mariani G, Bruselli L, Kuwert T, et al. A review on the clinical uses of SPECT-CT. Eur J Nucl Med Mol Imaging. 2010;37(10):1959-1985.http://dx.doi.org/10.1007/s00259-010-1390-8 [ Links ]
4. Romer W, Nomayr A, Uder M, Bauz W, Kuwert T. SPECT-guided CT for evaluating foci of increased bone metabolism classified as indeterminate on SPECT in cancer patients. J Nucl Med. 2006;47(7):1102-1106 [ Links ]
5. Helyar V, Mohan HK, Baewick T, et al. The added value of multislice SPECT-CT in patients with equivocal bony metastasis from carcinoma of the prostate. Eur J Nucl Med Mol Imaging. 2010;37(4):706-713. http://dx.doi.org/10.1007/s00259-009-1334-3 [ Links ]
6. Sharma P, Kumar R, Singh H, et al. Indeterminate lesions on planar bone scintigraphy in lung cancer patients: SPECT, CT or SPECT-CT? Skeletal Radiol. 2012;41(7):843-850. http://dx.doi.org/10.1007/s00256-011-1304-2 [ Links ]
7. Zhao Z, Li L, Li F, Zhao L. Single photon emission computed tomography/spiral computed tomography fusion imaging for the diagnosis of bone metastasis in patients with known cancer. Skeletal Radiol. 2010;39:147-153. http://dx.doi.org/10.1007/s00256-009-0764-0 [ Links ]
8. Seo Y, Mari C, Hasegawa BH. Technological development and advances in single-photon emission computed tomography/computed tomography. Semin Nucl Med. 2008;38(3):177-198. http://dx.doi.org/10.1053/j.semnuclmed.2008.01.001 [ Links ]
9. Chua S, Gnanasegaran G, Cook GJ. Miscellaneous cancers (lung, thyroid, renal cancer, myeloma, and neuroendocrine tumors): Role of SPECT and PET in imaging bone metastases. Semin Nucl Med. 2009;39(6):416-430. http://dx.doi.org/10.1053/j.semnuclmed.2009.07.002 [ Links ]
10. Brenner AI, Koshy J, Morey J, Lin C, DiPoce J. The bone scan. Semin Nucl Med. 2012;42(1):11-26.http://dx.doi.org/10.1053/j.semnuclmed.2011.07.005 [ Links ]
11. Ben-Haim S, Israel O. Breast cancer: Role of SPECT and PET in imaging bone metastases. Semin Nucl Med. 2009;39(6):408-415.http://dx.doi.org/10.1053/j.semnuclmed.2009.05.002 [ Links ]
12. Gnanasegaran G, Barwick T, Adamson K, Mohan H, Sharp D, Fogelman I. Multislice SPECT-CT in benign and malignant bone disease: When the ordinary turns into the extraordinary. Semin Nucl Med. 2009;39(6):431-442. http://dx.doi.org/10.1053/j.semnuclmed.2009.07.005 [ Links ]
13. Even-Sapir E, Flusser G, Lerman H, Lievshitz G, Metser U. SPECT/multislice low-dose CT: A clinically relevant constituent in the imaging algorithm of non-oncologic patients referred for bone scintigraphy. J Nucl Med. 2007;48(2): 319-324. [ Links ]
14. Strobel K, Burger C, Seifert B, Husarik DB, Soyka JD, Hany TF. Characterisation of focal bone lesions in the axial skeleton: Performance of planar bone scintigraphy compared with SPECT and SPECT fused with CT. AJR Am J Roentgenol. 2007;188(5):W467-474.http://dx.doi.org/10.2214/AJR.06.1215 [ Links ]
15. Palmedo H, Marx C, Ebert A, et al. Whole-body SPECT-CT for bone scintigraphy: Diagnostic value and effect on patient management in oncological patients. Eur J Nucl Med Mol Imaging. 2014;41(1):59-67. http://dx.doi.org/10.1007/s00259-013-2532-6 [ Links ]
 Correspondence:
Correspondence:
Garba Yunusa
garusa2001@gmail.com
Received: 16 Feb. 2016
Accepted: 15 Mar. 2016
Published: 29 June 2016














