Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Journal of Radiology
On-line version ISSN 2078-6778
Print version ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.20 n.1 Johannesburg 2016
http://dx.doi.org/10.4102/sajr.v20i1.959
ORIGINAL RESEARCH
Uterine artery embolisation as an effective choice for symptomatic fibroids: Five-year outcome
Paul Rischbieter; Christine Sinclair; Andrew Lawson; Samia Ahmad
Department of Radiology, University of Pretoria, South Africa
ABSTRACT
BACKGROUND: Uterine artery embolisation for the treatment of symptomatic uterine fibroids is a relatively new but internationally recognised procedure. The present study seeks to report the results of the largest South African series of uterine artery embolisations for symptomatic fibroids to date. It is the fourth article to be published in South Africa on the outcomes of this procedure, and the largest South African series to date.
OBJECTIVE: To evaluate the long-term efficacy of uterine artery embolisation in women with symptomatic fibroids in a tertiary hospital in South Africa.
METHODS: Eighty-two women who presented for uterine artery embolisation at a single site in South Africa for symptomatic fibroids were retrospectively studied. Outcomes included recurrence and re-intervention rates, patient satisfaction and complication rate.
RESULTS: Two patients required repeat embolisation, and one patient experienced fibroid recurrence without further intervention. No repeat myomectomies were performed. Eighty percent of patients reported being satisfied, 12% partially satisfied and 7% not satisfied. No major complications were reported.
CONCLUSION: Uterine artery embolisation was shown to be a good choice in the treatment of symptomatic fibroids and presents favourable long-term outcomes in the South African population.
Introduction
Uterine artery embolisation (UAE) is a minimally invasive, uterine-sparing treatment option in the management of uterine leiomyomas (fibroids). Since the first UAE was described in 1995,1 an increasing body of international research has sought to understand its place in clinical practice. There is now a growing need to further investigate clinical results at five years post procedure, when recurrence and re-intervention rates become more important.
African black women are more frequently affected by uterine fibroids and experience more severe symptoms than white or Asian women.2,3 This fact, in addition to the cultural stigma of hysterectomy within African communities, makes uterine artery embolisation a potentially important treatment option in the South African context. Two previous studies in the South African population have shown good, relatively short-term results.4,5
The present study investigated the long-term outcomes of uterine artery embolisation as a treatment option for symptomatic fibroids within the South African clinical environment.
Background
Symptomatic uterine leiomyomas can cause pain, heavy bleeding, pressure effects and reduced fertility. Traditionally, definitive treatment has been through hysterectomy or myomectomy. Today, UAE has become a standard procedure for the treatment of uterine fibroids around the world.6 More than 100 000 procedures have been performed globally and ongoing research continues to contribute to our knowledge of this procedure. A Cochrane review by Gupta et al.7 showed that UAE had overall patient satisfaction rates similar to those of myomectomy and hysterectomy for the same indication, with faster recovery times, shorter hospital stays, and a quicker return to routine activities. Kröncke et al.8 recently published the results of the 4th Radiology-Gynaecology Experts Meeting in Europe, which provides up-to-date consensus guidelines for the incorporation of UAE into routine practice, and the Society of Interventional Radiology (SIR) Standards of Practice Committee recently released the updated 'Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata',6 showing clear data to guide the ongoing support of this procedure.
Methods
The present retrospective observational study was performed at Steve Biko Academic Hospital, Pretoria, and conducted on all patients treated between 2006 and 2014 for symptomatic fibroids with uterine artery embolisation. Embolisation was performed on a total of 82 patients. All patients presented initially to the Department of Obstetrics and Gynaecology with symptomatic fibroids and were selected on the basis of their clinical suitability for the procedure. A multi-disciplinary team comprising gynaecologists, anaesthetists and radiologists provided operative and peri-operative care. As part of the pre-operative workup, all patients underwent pelvic sonography to assess the number and size of uterine fibroids. All patients attended outpatient follow-up at six months and one year post-procedure, at which time follow-up sonography was performed. All patients were contacted telephonically one to eight years after the procedure to determine their well-being.
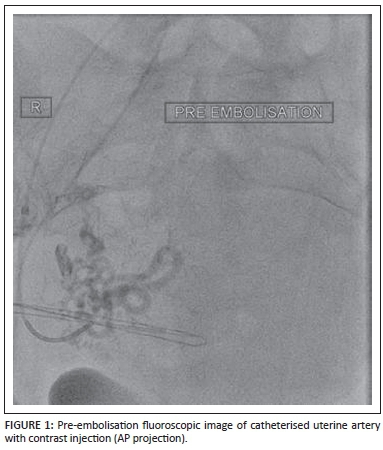
All uterine artery embolisations were performed in the interventional radiology suite at Steve Biko Academic Hospital. Patients were given either spinal or general anaesthesia at the discretion of the attending anaesthetist as per the protocol of the Department of Anaesthesia. Right common femoral arterial puncture was performed, followed by arteriography of the pelvic vessels. The uterine arteries were sequentially catheterised using a Roberts catheter (Cook Inc., Bloomington, Indiana, USA). The embolic agents in all cases were a combination of non-absorbable polyvinyl alcohol particles (300μm - 500m) and gelfoam. In all procedures, both uterine arteries were successfully embolised (Figure 1, Figure 2). Post-embolisation anaesthesia was provided at the discretion of the anaesthetist as a combination of opioids and benzodiazepines.

In addition to the objective clinical outcomes measured, and particularly any re-intervention procedures, patients were assessed on their overall subjective satisfaction with the procedure. Patients were assessed as 'satisfied' with UAE if they felt that they were relieved of their presenting symptoms; 'partially satisfied' if they were still mildly symptomatic; and 'dissatisfied' if there were no relief of major symptoms. Specific symptoms that were sought in the assessment of the degree of satisfaction were persistent menorrhagia, persistent bloating and constipation, and persistent dysmenorrhoea. At the time of the telephonic interview, patients were also asked if they had experienced any urinary incontinence or loss of defecation function. Patients were also asked if they would recommend the procedure to another person suffering from the same condition.
Post-surgical complications were divided into 'major' and 'minor' categories. Major complications were those that required surgical intervention or were potentially life threatening. Minor complications referred to all other reported complications.
All results were reported using descriptive statistics. No advanced statistical modelling was performed.
Results
Eighty-two women were identified within the study population. Fifty-two (63%) women were followed up between five and eight years post procedure with an average follow-up period of 79 months (six-and-a-half years) and were therefore selected for the long-term follow-up group. The median age of this group at the time of procedure was 46 years. A second group of 30 (37%) women was followed up between three and five years with an average follow-up period of 49 months (4 years).
The median age of this group at the time of the procedure was also 46 years. The average gravidity for the long-term group was 2.7 and average parity 2 (Table 1). There were no patients included with a follow-up period < 3 years. Thirty (37%) patients were lost to planned clinical follow-up. All patients were, however, successfully contacted telephonically.
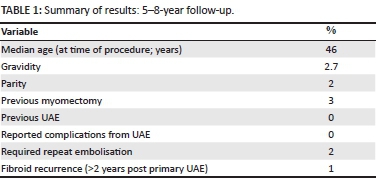
Of the long-term follow-up group, three women had undergone previous myomectomy. No patient had undergone a previous UAE before the start of the study period. There were no major complications and no incidences of sepsis following the procedure.
Recurrence and re-intervention
Two patients required repeat embolisation for insufficient improvement of persistent menorrhagia. Both patients had undergone technically successful primary procedures and underwent secondary embolisation between 12 and 18 months after their primary intervention. Both patients were followed up more than three years after the secondary intervention and reported complete resolution of symptoms.
One patient experienced fibroid recurrence four years post primary procedure with the development of new onset mild dysmenorrhoea. The patient has continued on medical therapy. No interval myomectomies were performed.
Patient satisfaction
Sixty-six (80.5%) patients reported being satisfied with the procedure. Ten (12.2%) patients reported being partially satisfied, and six (7.3%) patients reported being dissatisfied (Table 2).
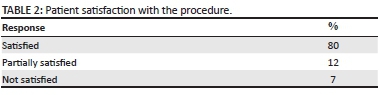
In the dissatisfied group, all patients complained of only partial resolution of menorrhagia and dysmenorrhoea. However, only one patient found the persistent symptoms to be severe enough to seek additional medical consultation.
In the partially satisfied group, eight patients reported a degree of ongoing dysmenorrhoea, and no further menorrhagia. Two patients who returned for successful UAE re-intervention procedures for persistent menorrhagia reported being partially satisfied as a result of the re-intervention procedure; their symptoms resolved after the second intervention.
Excluding the patient who experienced fibroid recurrence at four years, no patients within the study population reported using ongoing medication for bleeding control or pain management. No patients reported loss of urinary continence or defecation function. Ninety percent of patients would recommend the procedure to another patient. Only one pregnancy was reported in the patient cohort post embolisation (pregnancy carried to term). The patient was 36 years old at the time of pregnancy.
Indications and imaging
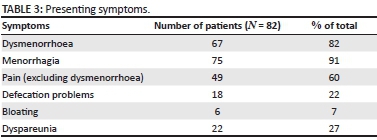
The indications for UAE varied across the patient population, with most patients having several indications (Table 3). Menorrhagia was reported in 84% and 59% reported dysmenorrhoea.
The pre-operative ultrasound imaging confirmed the presence of fibroids and did not detect any adnexal disease. The retrospective nature of this study and lack of standardised follow-up data capture via sonography did not allow accurate and uniform assessment of uterine volume and fibroid size pre and post embolisation. MRI is not part of the diagnostic workup for uterine fibroids at Steve Biko Academic Hospital.
Complications
No major complications were reported in our patient population and no patients underwent hysterectomy. All patients reported a degree of post-operative pain, nausea and pyrexia consistent with post-embolisation syndrome.9
Discussion
Minimally invasive treatment has gained substantial popularity, amongst both the medical fraternity and the public. Given the correct clinical indications and in skilled hands, UAE has been accepted by the international community as part of the standard of care that should be offered to patients with symptomatic fibroids.6, 8 Prior studies conducted in South Africa in 20044 showed that UAE could be considered as an effective treatment option in South African centres with adequate training and expertise. A more recent prospective study5 again showed results consistent with previous local experience and in line with international reports.10,11
The present retrospective analysis focused on the long-term outcomes of UAE with respect to symptom resolution and whether patients required any form of re-intervention, be it medical or surgical. In this study of 82 women with symptomatic fibroids, bilateral uterine artery embolisation was technically successful in all patients. No major complications were encountered. Post-operative pain still remains a big challenge in the peri-operative setting.9
The pathophysiology of fibroids is poorly understood, and it is well recognised that they generally cause no symptoms. Fifty-two patients had been followed-up for between five and eight years and, although none of these patients received follow-up imaging, they reported that they had remained symptom free. It is a limitation of the present study that there was no indication whether the fibroids had objectively involuted and no proof that none had re-appeared in asymptomatic patients. Better understanding of the imaging and clinical picture might in future predict which fibroids could respond better to certain treatment strategies. The link between bulk and pressure symptoms is certainly easier to understand than fibroids resulting in menorrhagia.10
Menorrhagia is more common with submucosal fibroids but occurs with fibroids in other anatomical locations as well. Production of cytokines and vasoactive agents differ between women with fibroids and those without, which may explain the increased menstrual blood loss. There is no evidence of a relationship between fibroid vascularity and menstrual blood loss, and it is over-simplistic to assume that complete fibroid infarction would cure menorrhagia. In any fibroid group, there will always be some patients with dysfunctional uterine bleeding where the fibroids are simply a coincidental association.10
No identifiable cause was found in the two patients with recurrence leading to re-intervention. A postulated cause could have been unrecognised uterine artery spasm, resulting in inadvertent under-embolisation. Our recurrence rate of 2.4% is well below the observed value of 15%.6 The single patient who experienced demonstrable fibroid recurrence with dysmenorrhoea at four years chose conservative medical therapy and has remained without further, or worsening, symptoms.
Patients who have undergone myomectomy are also at risk of developing recurrent symptomatic fibroids.12,13 The reported incidence varies between 10% and 62%.13 In the present series, three patients who had already had myomectomy presented for embolisation. All three of these patients were followed up at three years and remain symptom free.
The average patient age at the time of embolization was 46 years. The gynaecology unit was not a specialist infertility centre, so no emphasis was placed on objective or biochemical measurements of ovarian function or reserve such as luteinising hormone (LH), follicle stimulating hormone (FSH) or anti-mullerian hormone (AMH). The review did therefore not focus on ovarian function post UAE.
A limitation of the present study is the poor clinical follow-up, with 30 patients lost to planned outpatient follow-up. All patients were successfully contacted telephonically which gives some reassurance as to the unlikelihood of severe symptom recurrence. Our findings may nevertheless underestimate the real recurrence rate. Previous international studies have reported re-intervention rates as high as 33%.14 A number of factors may explain the lower figures reported in this study. Patients were not assessed for transition into menopause; the average age of the patient cohort was high; and low recurrence might, at least in part, have been a result of transition into menopause. Patients may also avoid reporting recurrent symptoms for fear of hysterectomy or further surgical intervention, as well as owing to financial limitations in seeking further hospital treatment.
Our follow-up imaging data were limited mainly by socioeconomic factors. Once the patients had formally been discharged from the gynaecology clinic, usually at the 6-month follow-up, they were referred back to primary health care facilities in the community. These clinics do not have the staff or resources to offer basic imaging services such as ultrasound. Long-term data acquisition was mostly determined via telephonic consultation.
The present retrospective review again shows UAE to be a good choice in the treatment of symptomatic fibroids and presents favourable long-term outcomes. Long-term imaging follow-up was not available to objectively measure the fibroids post embolisation. In our setting, the clinical improvement and reduction in morbidity associated with fibroids was considered adequate to advocate the usage of UAE in South Africa in centres with the appropriate skill and clinical support.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
P.R. (University of Pretoria) was the lead author, C.S. (University of Pretoria) assisted with compiling clinical data, A.L. (University of Pretoria) assisted with project design, review and analysis, and S.A. (University of Pretoria) was the supervisor.
References
1. Ravina JH, Ciraru-Vigneron N, Bouret JM, et al. Arterial embolisation to treat uterine myomata. Lancet. 1995;346(8976):671-672. http://dx.doi.org/10.1016/S0140-6736(95)92282-2 [ Links ]
2. Catherino WH, Eltoukhi HM, Al-Hendy A. Racial and ethnic differences in the pathogenesis and clinical manifestations of uterine leiomyoma. Semin Reprod Med. 2013;31:370-379. http://dx.doi.org/10.1055/s-0033-1348896 [ Links ]
3. Stewart EA, Nicholson WK, Bradley L, Borah BJ. The burden of uterine fibroids for African-American women: Results of a national survey. J Women's Health. 2013;22:807-816. http://dx.doi.org/10.1089/jwh.2013.4334 [ Links ]
4. Prollius A, De Vries C, Loggenberg E, et al. Uterine artery embolization for symptomatic fibroids. International Journal of Gynecology & Obstetrics. 2004;84: 236-240. http://dx.doi.org/10.1016/j.ijgo.2003.09.006 [ Links ]
5. Lawson A, Cluver C, Olarogun J, et al. Uterine artery embolisation for uterine leiomyomas. South African Journal of Obstetrics and Gynaecology. 2014;40: 18-21. http://dx.doi.org/10.7196/sajog.798 [ Links ]
6. Dariushnia SR, Nikolic B, Stokes LS, Spies JB. Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata. J Vasc Interv Radiol. 2014;25:1737-1747. http://dx.doi.org/10.1016/j.jvir.2014.08.029 [ Links ]
7. Gupta JK, Sinha A, Lumsden MA, Hickey M. Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database Syst Rev. 2014;12:Cd005073. http://dx.doi.org/10.1002/14651858.cd005073.pub4 [ Links ]
8. Kröncke T, David M. Uterine artery embolisation (UAE) for treatment of myomas. Geburtshilfe und Frauenheilkunde. 2014;74:433-435. http://dx.doi.org/10.1055/s-0033-1350827 [ Links ]
9. van Overhagen H, Reekers JA. Uterine artery embolization for symptomatic leiomyomata. Cardiovasc Intervent Radiol. 2015;38:536-542. http://dx.doi.org/10.1007/s00270-014-1031-x [ Links ]
10. Moss J, Cooper K, Khaund A, et al. Randomised comparison of uterine artery embolisation (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG. 2011;118:936-944. http://dx.doi.org/10.1111/j.1471-0528.2011.02952.x [ Links ]
11. van der Kooij SM, Hehenkamp WJK, Volkers NA, Birnie E, Ankum WM, Reekers JA. Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroids: 5-year outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2010;203:105. e1-e13. [ Links ]
12. Walker WJ, Barton-Smith P. Long-term follow up of uterine artery embolisation an effective alternative in the treatment of fibroids. BJOG. 2006;113:464-468. http://dx.doi.org/10.1111/j.1471-0528.2006.00885.x [ Links ]
13. Hanafi M. Predictors of leiomyoma recurrence after myomectomy. Obst Gynecol. 2005;105:877-881. http://dx.doi.org/10.1097/01.AOG.0000156298.74317.62 [ Links ]
14. Ananthakrishnan G, Murray L, Ritchie M, et al. Randomized comparison of uterine artery embolization (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): Subanalysis of 5-year MRI findings. Cardiovasc Intervent Radiol. 2013;36:676-681. http://dx.doi.org/10.1007/s00270-012-0485-y [ Links ]
 Correspondence:
Correspondence:
Paul Rischbieter
rischbieter.p@gmail.com
Received: 23 Nov. 2015
Accepted: 05 Jan. 2015
Published: 31 Mar. 2016














