Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SA Journal of Radiology
versão On-line ISSN 2078-6778
versão impressa ISSN 1027-202X
S. Afr. J. radiol. (Online) vol.19 no.2 Johannesburg 2015
http://dx.doi.org/10.4102/sajr.v19i2.919
REVIEW ARTICLE
Image Gently: A campaign to promote radiation protection for children worldwide
Kimberly Applegate
Department of Radiology and Imaging Sciences, Emory University School of Medicine, United States of America
ABSTRACT
With the goal of raising awareness and developing stakeholder educational tools for the appropriate imaging of children, the Image Gently campaign was launched in 2007. This campaign is a product of a multidisciplinary alliance with international representation which now numbers nearly 100 medical and dental professional societies and organisations, and includes regulatory organisations. The alliance focuses on increasing awareness and developing education materials that support the protection of children worldwide from unnecessary radiation in medicine. The alliance members work with agencies and regulatory bodies to improve standards and measures that are specific to children. The campaign has produced open source modules for all stakeholders regarding CT, fluoroscopy, nuclear medicine, interventional radiology, digital radiography and dental imaging. The philosophy of the Image Gently steering committee is to collaborate, to share information freely, to keep messaging simple and to commit to lifelong learning. Many healthcare practitioners may not understand how to decrease children's radiation exposure; the goal of Image Gently is to increase all stakeholders' understanding of both the benefits and the risks and to encourage radiation reduction strategies. This article summarises the rationale and goals of the global campaign to date.
Introduction
Unquestionably, diagnostic imaging has revolutionised modern medicine. Many studies show that the appropriate use of radiology imaging tests saves lives and improves patient care. Examples include computed tomography (CT) scans to diagnose or exclude appendicitis, trauma and acute vascular disorders.1 However, patients, especially young children, may face a potential cancer risk from repeated low-dose exposure to routine diagnostic medical imaging.2 The remarkable advance of imaging technology and its exponential increase in use over the past 25 years has led to an unanticipated increase in human exposure to radiation worldwide, including the population of the United States.3 Determining the correct examination and dose is most important for children and adolescents, who are often more sensitive than adults to radiation, are potentially exposed to more lifetime risk from either early or ongoing exposures, and have a longer lifetime during which cancer from radiation exposure can develop. This article reviews the rationale behind the creation of the Image Gently campaign and the strategies used (awareness, advocacy and education) to reduce children's exposure to radiation from diagnostic imaging.
Why reducing children's and adolescents' exposure to radiation from medical imaging matters
Medical radiation is used for both diagnostic and therapeutic purposes. Diagnostic imaging tests that use ionising radiation include the X-ray (or radiograph), fluoroscopy (and interventional cardiology and radiology) and CT scans. Most importantly, radiation exposure may increase a child's risk of cancer later in adult life, although definitive data are lacking, and exposure from medical imaging is a modifiable risk factor.2,4,5,6 Other epidemiological data regarding the longterm effects of low-level radiation (100-150 milliSeverts (mSv)) exposure comes from the wellknown life span study of atomic bomb survivors in Japan.The Internaional Council on Radiation Protection continues to uphold its stance that the linear non-threshold dose response assumption for extrapolating from high-dose exposures to the low doses used in medical imaging is the best interpretation of radiation-induced cancer risk for protection purposes.7,8 Though controversial, this conservative model states that the risk from exposure to ionising radiation is estimated to be linear, from the known exposures during higher-dose events (e.g. atomic bombs dropped in Japan and the nuclear power plant explosions in Chernobyl) to exposures during low-dose events such as those that occur during medical imaging.
A single abdominal CT scan exposes a teenaged patient to a low dose - typically no more than 10 mSv of ionising radiation - although the dose depends on the reason for the CT scan and how it is performed.1,3 Bear in mind that the overall lifetime risk of death due to cancer in developed nations is 20%-25%.3 The estimated increased risk of cancer over a lifetime from a single CT scan is estimated as being a tiny fraction of this risk (0.03%-0.05%).8,9 To put this percentage in perspective, researchers have estimated that the risk from one abdominal CT scan is about equal to the risk of a crash occurring if a car were driven 7500 miles (12 070 km) or a motorcycle 1000 miles (1609 km).10 Given this small estimated risk, the critical principle is to determine which radiological examinations are necessary, when they are necessary, and how to ensure they are done with the lowest radiation dose to answer the clinical question.
Increased use of medical imaging
The reason for focusing on CT scanning is that it is becoming an increasingly large source of radiation exposure - and it is a modifiable potential risk of cancer induction. Diagnostic radiation accounts for approximately half of the United States population's total annual radiation exposure.3 CT scans contribute the highest dose and they account for approximately half of adult medical radiation exposure and two-thirds of paediatric medical exposure.3 Worldwide, an estimated 320 million CT scans are performed annually. The United States accounts for approximately one-quarter of all CT scans worldwide, representing more than 80 million each year.1,2,3,4,5,6 If we apply a recent estimate that 11% of CT scans being performed are on children, then the number of annual paediatric CT scans would be estimated to be up to 7.1 million in the United States.11
When the average effective dose per person in the United States increased from 3.6 mSv in the 1980s to 6.2 mSv in 2006, the percentage of the received dose from medical imaging increased from 15% to 48%.3
After establishing that radiation exposure from imaging is increasing, we must consider children's unique situation. Depending on their age, organ, and tumor type, children are reported to be on average 2-3 times more sensitive to radiation than adults, and the younger the infant or child, the more radiosensitive at high doses they are. However, a recent UNSCEAR report found that only 35% of cancers are associated with increased sensitivity in children compared to adults.8 In addition, children have a longer lifetime during which cancer may develop from exposure to radiation.6,12,7,8 For these reasons, we tend to have a more cautious approach to the use of ionising radiation imaging in children than in adults.
The rate of CT use increases throughout the paediatric years and is the highest in the adolescent population - for example, imaging from trauma and to evaluate for suspicion of appendicitis.11 Adolescent girls undergoing breast development have higher breast radiosensitivity at high doses compared to younger children or to adult women. Adolescents also have higher thyroid radiosensitivity at high doses.8
Although the individual risk estimates are small, the population risks from the rapid increase in CT use is of growing concern. Small individual risks applied to an increasingly large population may create a public health issue some years in the future. In 2010, the American College of Radiology developed a policy statement to respond to public media concern:
The expanding use of imaging modalities using ionizing radiation may eventually result in an increased incidence of cancer in the exposed population; this problem can likely be minimized by preventing the inappropriate use of such imaging and by optimizing imaging tests that are performed to obtain the best image quality with the lowest radiation dose.13
It is with this goal in mind that the Image Gently campaign seeks to educate concerned patients, families and healthcare professionals and to share information that will help to reduce radiation exposure to children and adolescents resulting from imaging.
The image gently campaign
Initiated by a group of paediatric radiologists in 2007, Image Gently is an educational, awareness and advocacy campaign of the Alliance for Radiation Safety in Pediatric Imaging. The alliance is a coalition of healthcare, regulatory and guidance organisations dedicated to providing safe, high-quality paediatric imaging worldwide. The primary objective of the Alliance is to raise awareness in the imaging community of the need to adjust the radiation dose when imaging children. The ultimate goal of the alliance is to change clinical practice so as to reduce radiation exposure.
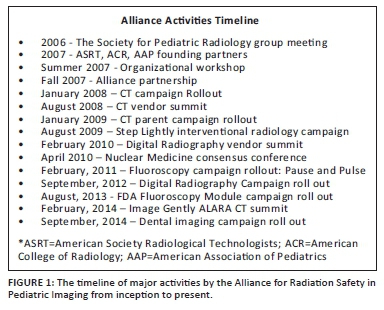
Image Gently is directed and run by a steering committee of volunteers with small financial contributions from the four founding organisations (the American Association of Physicists in Medicine, American College of Radiology, American Society of Radiologic Technologists and Society for Pediatric Radiology). Comprising nearly 100 healthcare organisations and regulatory agencies,10 Image Gently attempts to include all stakeholders involved in paediatric imaging, including parents and families. Stakeholders include more than 1 000 000 professionals throughout the world, including radiologists, technologists, medical physicists, dentists and paediatricians. All educational and promotional materials for the Image Gently campaign are provided free of charge (cf. http://www.imagegently.org). The timeline of major activities of the campaign is provided in Figure 1.
Key principles of radiation protection
One of the most important goals of Image Gently is to raise all stakeholders' awareness about the three key principles of radiation protection: justification, optimisation and dose limits. These principles are based on the International Council for Radiation Protection guidelines.7 Justification focuses on appropriateness. We need to ask ourselves whether the benefits outweigh the risks of performing the imaging test on the individual patient. Risks include potential harm such as later cancer induction from ionising radiation. In addition, in some instances, alternative diagnostic tests that do not use ionising radiation - such as ultrasound (US) or magnetic resonance imaging (MRI) - can provide the same information as CT scans. Image Gently initiatives include producing and disseminating parent education brochures and informing the medical community about which imaging tests are best suited to common clinical indications and when alternative modalities such as MRI and US may be substituted for ionising radiation tests.
The second key principle of radiation protection is optimisation. Image Gently focuses on providing guidance so that imaging tests using ionising radiation are done to provide sufficient diagnostic information while at the same time limiting radiation exposure. For example, the Alliance worked with its members to create CT imaging protocols that can be adjusted for the size of the infant and child rather than a one-size-fits-all protocol. There are free training modules for CT technologists to learn how to apply a number of important physics and technical parameters when imaging children in order to use the lowest possible radiation dose to achieve the necessary image quality. Along these same lines, Image Gently provides members with periodic email updates on the latest educational modules, information from collaborative organisations, convenes summits and works with regulatory bodies (e.g. the Food and Drug Administration [FDA], Joint Commission, Nuclear Regulatory Commission) to develop and promote appropriate dose standardisation and dose limits. These outcomes are aligned with the third key principle of radiation protection. Dose limits in medicine are relative; surveys are used to develop dose reference levels for common imaging examinations, and audits should be performed to ensure compliance with good-quality practice. Image Gently efforts include partnering with equipment vendors and regulators to convene summits and discuss standard dose metrics across vendors, to explain the importance of accurate metrics for infants and children, and to have all stakeholders understand the consequences of radiation exposures in this unique population.
Finally, when we educate patients and caregivers and encourage a shared decision-making environment in healthcare, the health outcomes improve.14
Campaign Key Goals
The steering committee identified six key goals during its first five years of volunteer work.15 The first was to provide educational materials to parents to help them understand the benefits and potential risks of medical imaging before their child underwent a test or procedure. These materials include questions for them to ask the referring physician and achieve the outcome of shared decision-making. The second goal was to tailor the imaging equipment for use in children. This effort involved vendor summits that brought together radiologists, physicists, radiographers, educators, the FDA and members from MITA (the Medical Imaging and Technology Alliance). The third goal was to provide educational materials to users of imaging equipment. These materials included web modules and slide presentations that were developed for meetings and local presentations to medical practitioners, including radiographers. The fourth goal was to develop a radiation dose estimate for individual CT scans based on the specific size of the patient. With the collaboration of the Image Gently Alliance, in 2011, the AAPM (American Association of Physicists in Medicine) published a method to adjust for the patient's trunk size (chest, abdomen and/or pelvis) by converting the volume CT dose index (CTDIvol) into a size-specific dose estimate (SSDE).16 The SSDE uses the scout image from the CT imaging to calculate the adjusted dose estimate automatically. The fifth goal was to provide a way for patients and their families to track examinations, and eventually doses. Image Gently provides a written guide for patients and families to track examinations and dates without needing to understand the dose indices. Currently, healthcare facilities are required or encouraged to track doses. New software will make this more widely possible. The sixth and final goal was the development of dose reference levels (DRLs) for common paediatric imaging examinations. CT and nuclear medicine examination DRLs have been developed but more need to be generated using the expansion of the American College of Radiology Dose Index Registry programme and/or the European Union DRLs.
Campaign messaging for each modality
An educational and awareness campaign should capture the attention of its intended audience. The messaging uses the science of social marketing techniques to provide educational materials that are open source to eliminate barriers to best practices at the local level.15 The simple message of the initial CT scan educational rollout to the medical community states that 'one size does not fit all' (Figure 2). The campaign has a few important, eye-catching messages. First, imaging is a positive force in medicine. Second, we all must be aware of the radiation protection principles when we use ionising radiation, especially in children. And third, the following are a few simple things we all can do when we perform ionising radiation imaging tests (e.g. CT scans) that will reduce childhood radiation exposure:
Clearly, imaging saves children's lives, but when we image, radiation matters. Children are more sensitive to radiation [than adults]. What we do now lasts a lifetime. So when we image, let's image gently. More often is not better. When using ionizing radiation for pediatric imaging, remember the following: (1) take into account the patient's age and size and then dose accordingly, (2) most information can be gained from a single study, please do not repeat studies unnecessarily, and (3) image only the indicated area.10
The Image Gently campaign has created educational information for each ionising radiation modality (CT scan, fluoroscopy, radiography, nuclear medicine, interventional radiology and dental imaging), beginning with CT scans. Each educational module provides information for all stakeholders involved in paediatric diagnostic imaging: (1) the radiologists, medical physicists and technologists who plan, carry out and interpret imaging tests, (2) the referring providers who order imaging tests, and (3) the patients, parents and caregivers. In addition, Image Gently advocates best practices specifically for children because educational efforts and national guidelines alone cannot achieve the goals of radiation protection.
Examples of educational strategies include a brochure for parents and patients: 'What parents should know about CT scans for children: medical radiation safety' (Figure 3). This brochure is available in many languages, and it describes in lay language what an X-ray and a CT scan are, and presents imaging alternatives to CT. It also suggests questions that patients or caregivers can ask healthcare workers about the quality of an imaging facility (e.g. questions about licensing, credentialing and accreditation) and provides data on relative radiation doses and potential cancer risk. There are also addresses of websites for those who want further information. Image Gently encourages radiology departments, emergency departments and paediatric offices to hand out these brochures to patients and patients' caregivers. Alternatively, if resources are limited, the brochures may be displayed in the facility waiting area.
To educate practitioners, Image Gently describes the ALARA ('as low as reasonably achievable') principle on its website. This principle is one of minimising radiation exposure to both patients and radiation workers. For workers, ALARA is typically linked to a dose limit. For patients, we use diagnostic reference levels for common imaging tests that patient doses should generally not exceed.
Conclusion
Diagnostic imaging using ionising radiation, and in particular CT, is commonly used for children's and adolescents' medical care. Radiological tests have many medical benefits, yet these imaging tests must be justified, optimised and audited for children's care. It is with this knowledge in mind that Image Gently seeks to promote education and awareness of best practices and shared decision-making with concerned patients, families and healthcare professionals. Such work has led to decreased radiation doses in paediatric CT protocols and to partnerships with regulators with the aim of promoting best practices. Image Gently embodies the Hippocratic oath ideal, in that while agreeing that diagnostic imaging is an exceptional medical tool, healthcare practitioners must also agree to use it judiciously in order to minimise the risks to patients, and to remember: 'first, do no harm.'
Acknowledgements
Competing interests
The author is a member of the Steering Committee of Image Gently.
References
1. Rubin GD. Computed tomography: Revolutionizing the practice of medicine for 40 years. Radiology. 2014;273:S45-S74. PMID: 25340438,http://dx.doi.org/10.1148/radiol.14141356 [ Links ]
2. Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: Data linkage study of 11 million Australians. BMJ. 2013;346:f2360. PMID: 23694687, http://dx.doi.org/10.1136/bmj.f2360 [ Links ]
3. Schauer DA, Linton OW. NCRP Report No. 160, Ionizing Radiation exposure of the population of the United States, medical exposure-Are we doing less with more, and is there a role for health physicists? Health Phys. 2009;97(1):1-5. PMID: 19509507, http://dx.doi.org/10.1097/01.HP.0000356672.44380.b7 [ Links ]
4. Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet. 2012;380:499-505. PMID: 22681860, http://dx.doi.org/10.1016/S0140-6736(12)60815-0 [ Links ]
5. Huang WY, Muo CH, Lin CY, et al. Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: A nation-wide population-based cohort study. Br J Cancer. 2014;110(9):2354-2360. PMID: 24569470, http://dx.doi.org/10.1038/bjc.2014.103 [ Links ]
6. Boice JD. Radiation epidemiology and recent paediatric computed tomography studies. Ann ICRP. 2015;44(1 Suppl):236-248.http://dx.doi.org/10.1177/0146645315575877 [ Links ]
7. International Commission on Radiological Protection. 2007 Recommendations. ICRP Publication 103. Ann. ICRP 37 (2-4). Oxford: Elsevier; 2007. [ Links ]
8. UNSCEAR. Sources, effects and risks of ionizing radiation. Annex B: Uncertainties in risk estimates for radiation-induced cancer. United Nations Scientific Committee on the Effects of Atomic Radiation. New York: United Nations; 2012. [ Links ]
9. Berrington de Gonzalez A, Darby S. Risk of cancer from diagnostic X-rays: Estimates for the UK and 14 other countries. Lancet. 2004;363(9406):345-351. PMID: 15070562. [ Links ]
10. Home. Image Gently Campaign. Available from: http://www.imagegently.org/Procedures/ComputedTomography.aspx [ Links ]
11. Dorfman AL, Fazel R, Einstein AJ, et al. Use of medical imaging procedures with ionizing radiation in children: A population-based study. Arch Pediatr Adolesc Med. 2011;165(5):458-464. PMID: 21199972, http://dx.doi.org/10.1001/archpediatrics.2010.270 [ Links ]
12. Pierce DA, Preston DL. Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res. 2000;154(2):178-186. http://dx.doi.org/10.1667/0033-7587(2000)154[0178:RRCRAL]2.0.CO;2 [ Links ]
13. Amis ES, Jr., Butler PF. ACR white paper on radiation dose in medicine: Three years later. J Am Coll Radiol. 2010;7(11):865-870. PMID: 21040868,http://dx.doi.org/10.1016/j.jacr.2010.04.006 [ Links ]
14. Bulas D, Goske M, Applegate K, Wood B. Image Gently: Improving health literacy for parents about CT scans for children. Pediatr Radiol. 2009;39(2):112-116. PMID: 19083213, http://dx.doi.org/10.1007/s00247-008-1101-9 [ Links ]
15. Goske MJ, Applegate KE, Bulas DF, et al. Image Gently 5 years later: What goals remain to be accomplished in radiation protection for children? AJR. 2012;199(3):477-479. PMID: 22915386, http://dx.doi.org/10.2214/AJR.12.9655 [ Links ]
16. Boone JM, Strauss KJ, Cody DD, et al. Size-specific dose estimate (SSDE) in paediatric and adult body CT examinations. AAPM Report No. 204. 2011. Available from:www.aapm.org/pubs/reports/rpt_204.pdf [ Links ]
 Correspondence:
Correspondence:
Kimberly Applegate
Department of Radiology and Imaging Sciences, Emory University School of Medicine
The Emory Clinic, Inc., Building C, 1365 Clifton Road, NE, Room CT-076
Atlanta, GA 30322, United States of America
keapple@emory.edu
Received: 02 Aug. 2015
Accepted: 13 Oct. 2015
Published: 14 Dec. 2015














