Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of HIV Medicine
On-line version ISSN 2078-6751
Print version ISSN 1608-9693
South. Afr. j. HIV med. (Online) vol.22 n.1 Johannesburg 2021
http://dx.doi.org/10.4102/sajhivmed.v22i1.1292
ORIGINAL RESEARCH
Group counselling for adherence support among young people failing first-line antiretroviral therapy in Zimbabwe
Bahati KasimonjeI; Tinei ShamuI, II, III; Tinashe MudzvitiI, IV; Ruedi LuethyI
INewlands Clinic, Harare, Zimbabwe
IIInstitute of Social and Preventive Medicine, University of Bern, Bern, Switzerland
IIIGraduate School of Health Sciences, University of Bern, Bern, Switzerland
IVDepartment of Pharmacy and Pharmaceutical Sciences, University of Zimbabwe, Harare, Zimbabwe
ABSTRACT
BACKGROUND: Sub-optimal adherence to antiretroviral therapy (ART) is reportedly worse amongst young people living with HIV (YPLHIV). Group adherence counselling can be useful to improve adherence
OBJECTIVES: We evaluated an enhanced adherence counselling group intervention (EACGI) amongst YPLHIV failing a non-nucleoside reverse transcriptase (NNRTI)-based first-line ART regimen
METHOD: This was a retrospective cohort study using routinely collected data of YPLHIV failing NNRTI-based first-line ART. Patients with confirmed virological failure were referred for EACGI, a 12-week curriculum of weekly, 1.5-h sessions accommodating 8-15 people per group. It aimed to facilitate readiness to switch to second-line ART and improve adherence through a mental health intervention. Viral loads of HIV were measured pre-EACGI; at baseline; 3, 6 and 12 months post switch
RESULTS: Fifty-seven patients aged 13-25 years were invited to EACGI and followed for up to 48 weeks. Thirty-three (58%) patients attended at least four sessions, whilst 24 (42%) attended none. Amongst those who attended none, two (8%) were transferred out, three (13%) were lost to follow-up and two (8%) had died by week 48 of follow-up, whilst all who attended were still in care. By week 48, amongst patients still in care, 29%, 44% and 67% of those who attended no sessions, 4-9 and 10-12 sessions, respectively, had viral loads of < 50 copies/mL
CONCLUSION: An EACGI is a promising intervention for YPLHIV failing ART prior to treatment switch, leading to improved adherence. This study's findings support the need for further enquiry into rigorous, evidence-based multilevel adherence interventions that are acceptable and effective for YPLHIV
Keywords: enhanced adherence counselling; adolescents; mental health; antiretroviral therapy; virological failure.
Introduction
Sub-optimal adherence to antiretroviral therapy (ART) amongst people living with HIV (PLHIV) is the leading cause of virological failure (VF).1,2 This is reported to be more pronounced in young people and to some extent 'characteristic' during this growth phase.3,4,5,6 Young people are a diverse group of the population and are defined in this study to be in the age range of 13-25 years. One of the major challenges that healthcare professionals face is helping young people adhere to ART despite its well-known benefits in improving the overall health and quality of life.7,8 Globally, HIV is a leading cause of death amongst young people, which is associated with inadequate adherence support and poor retention in care.9,10,11 Given the high risk of VF, disease progression, drug resistance, limited treatment options and the ultimate threat to survival, understanding and examining adherence strategies that delve beyond a traditional clinical approach is imperative.12 This is more so in countries in sub-Saharan Africa, where more than 80% of the world's 2.1 million adolescents infected with HIV live.4
Part of young people's HIV management and care involves treatment switching from a failing ART regimen to a different class of antiretrovirals when VF occurs, most often because of inconsistent adherence.13,14 The fundamental goal of regimen switching is to achieve and sustain virological suppression without compromising future treatment options.1,14 Although treatment switching is an established clinical practice, there are limited data on the virological status of young people following a treatment switch.15
Group adherence counselling is often utilised as an intervention to improve adherence in routine HIV care.16 Studies have shown mixed results in its effectiveness and were mainly conducted in adult populations.11 A randomised controlled trial in Thailand found a statistically significant difference in treatment outcomes in 15- to 24-year-olds for the intervention group,17 whilst in South Africa there was no difference in treatment outcomes for a group adherence strategy delivered to young people and their caregivers.18 Experiences and outcomes of group psychotherapy as an adherence support intervention in young people have not been widely documented. In this study, we report virological suppression outcomes amongst adolescents and young people who were invited to an Enhanced Adherence Counselling Group Intervention (EACGI) after failing a non-nucleoside reverse transcriptase (NNRTI) based first-line ART regimen.
Methods
Study design and setting
This was a retrospective cohort study using routinely collected data of adolescents and young PLHIV (13-25 years) failing NNRTI-based first-line ART at Newlands Clinic during the period 2015-2016. This study sought to evaluate an EACGI for young PLHIV on ART adherence. Newlands Clinic is an urban HIV treatment centre in Zimbabwe and a referral outpatient clinic providing comprehensive HIV care, which is supported by the Ruedi Luethy Foundation, a private voluntary organisation. The model of care is nurse-led, doctor supervised, with four nurses and two doctors dedicated to the care of over a 1000 adolescents and young people predominately from marginalised communities.19 Psychological support offered by a psychologist and peer counsellor is provided for patients struggling to cope with issues that affect their treatment success. The clinic had 1102 patients aged 13-25 years in care as of 31 December 2020.
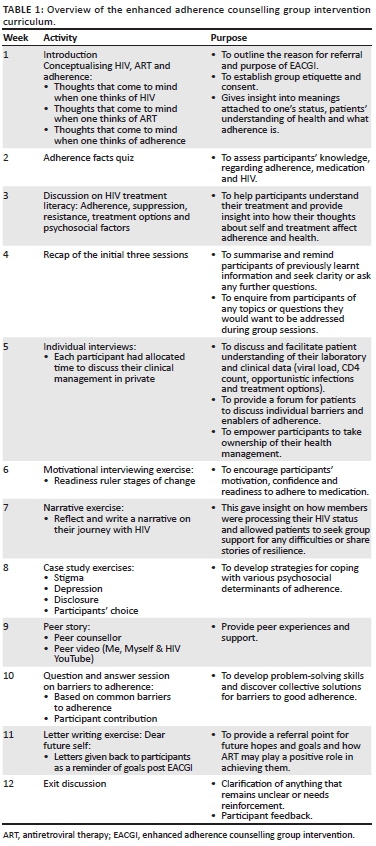
Viral load measurements were conducted using the COBAS® Ampliprep®/Taqman48® platform and the Roche HIV1 version 2.0 assay. According to the clinical guidelines, virological treatment failure was defined as two consecutive viral load measurements > 200 copies/mL at least 3 months apart. Virological suppression was defined as achieving a viral load < 50 copies/mL. Patients with low-level viraemia (51 copies/mL - 200 copies/mL) were managed by their respective nurses and were not referred to EACGI. Once virological treatment failure on first-line ART was confirmed, patients were referred for the EACGI, which was part of routine care, aimed to facilitate readiness to switch treatment to second-line ART, and improve adherence through phenomenological, motivational interviewing and cognitive behavioural therapy principles. All patients who were referred for EACGI were included in the study. The EACGI was a 12-week curriculum of weekly, 1.5-h sessions that accommodated 8-15 people per group during the period 2015-2016. The intervention was developed locally in the clinic by the psychologist through adapting the past experiences of clinicians, peer counsellors and patients. These experiences were then used to design the intervention to best meet the needs of adolescents failing treatment. Participants were conveniently selected to a group based on their respective ages (13-17 years and 18-24 years). Participants were informed and invited to attend EACGI by their respective nurse and peer counsellor. Group sessions were facilitated by a resident psychologist and a peer counsellor in English, the local dialect (Shona) and a youth friendly language. The peer counsellor was trained under the Africaid's Community Adolescent Treatment Support programme.20 Each session began with an icebreaker to help to establish rapport, and create a positive group atmosphere and cohesion. Participants were offered bus fare and refreshments after each session. All participants who missed the initial EACGI sessions were followed up telephonically or at their clinic visit by their peer counsellor to establish barriers to attendance. Reasons for missing visits for those who attended the EACGI were asked during the individual interviews or at group session recaps. An overview of the EACGI curriculum is displayed in Table 1. This approach is published elsewhere.21
After undergoing EACGI, the patients who achieved virological suppression continued their current regimen, whilst those who were unsuppressed were switched to a second-line protease inhibitor-based regimen. Viral loads of HIV were measured pre-EACGI at the end of the 12-week sessions (time of switching to second-line ART), and at 3, 6, 9 and 12 months post switch to assess virological outcomes.
All patient data were recorded in the clinic's electronic medical record (EMR), which is only accessible to authorised personnel and is password protected.
Statistical analysis
We used frequencies and proportions to describe patient distributions in categories. For the description of central tendency, we used medians and interquartile ranges for variables not normally distributed. We measured normality of continuous variables using the Shapiro-Wilk test. Attendance rates were analysed as no attendance, < 75% and at least 75% attendance. The initial nine EACGI curriculum sessions covered the fundamental aspects of treatment literacy, whilst the final sessions reinforced taught material. We used logarithm transformed viral load measurements before comparing using two-sample t-tests. We used Stata version 13.1 (College Station, Texas, United States) and DABEST package (version 0.3.0) in R studio (R version 4.0.4 [2021 Feb 15]) for statistical analysis.22
Ethical considerations
This study was approved by the Newlands Clinic Research Unit and the Medical Research Council of Zimbabwe (MRCZ/E/205).
All participants aged 18 years and older provided written informed consent before participating in this study. Participants younger than 18 years provided written assent, and their parents or guardians provided written informed consent.
Results
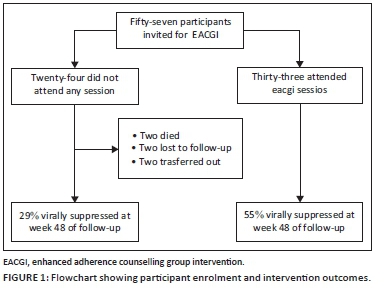
Fifty-seven patients (n = 34, 60.0% female) aged 13-25 years were invited to the EACGI and followed up for 48 weeks. The median duration of first-line ART was 6 years (interquartile range [IQR]: 4-8) at the time of invitation to EACGI. Thirty-three (57.9%) patients attended at least four EACGI sessions, whilst the other 24 (42.1%) patients did not attend any session. Of the 33 patients who attended the EACGI, 25 (75.8%) were female patients, whilst 15 (62.5%) of those who did not attend were male patients. The main reasons for not attending the EACGI include a lack of interest and school or work commitments. Main reasons reported by patients for a low attendance rate to EACGI amongst those who attended were hopelessness, family dysfunction, perception of not having an illness, an aversion to a daily routine attached to stigma and prior experience of medication side effects. Amongst those who did not attend the EACGI, two (8%) were transferred out, three (13.0%) were lost to follow-up and two (8.0%) had died by week 48 of follow-up, whilst all who attended were still in care (Figure 1).
As shown in Table 2, the baseline demographic and treatment characteristics of the patients invited to attend the EACGI are listed.
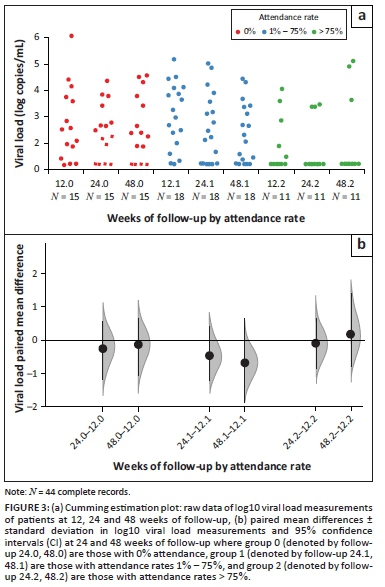
Overall, there was a mean decline in the viral load of participants after EACGI before switching to second-line ART by 1.03 log copies/mL (standard error [SE]: 0.22, p < 0.001). Those who attended EACGI had the highest decline of 1.24 log copies/mL (SE: 0.29, p < 0.001) compared with 0.76 log copies/mL (SE: 0.34, p = 0.028) amongst those who did not attend.
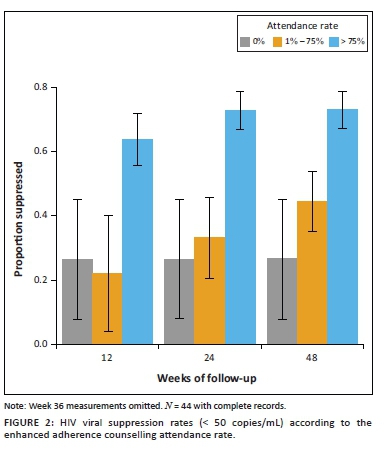
Amongst patients who attended > 75% of sessions, the viral suppression rate was 73% by week 12, but reduced to 64% at week 24 and to 67% at week 48 on second-line ART. Amongst those who attended four to nine sessions, the viral suppression rate increased from 17% to 44% by week 48. Virological suppression at week 48 was lowest amongst those who did not attend any of the sessions at 29% (Figure 2). Less than half of the participants had week 36 viral load measurements and, therefore, are not reported. Although viral loads were lowest amongst patients who attended the most sessions and highest amongst those who did not attend, a few patients who attended > 75% of sessions were failing second-line ART by week 48 (Figure 3).
Discussion
We present the virological response of young people who were invited to an EACGI over one year of follow-up. The mental health adherence support intervention enabled improved adherence to ART and consequently positive virological outcomes on second line in young people who regularly attended group counselling sessions. Additionally, the difference in virological suppression was sustained over one year post intervention. All participants who attended the group intervention were retained in care during the 48 weeks of follow-up. It is especially noteworthy that this was achieved in young people who are ART experienced. Whilst the effect of an ART regimen switch alone may be sufficient to elicit positive virological outcomes because of the use of a more potent regimen, an EACGI could provide additional treatment support for adolescent patients.
Compared with other age groups in HIV care, adolescents show poorer adherence.3,23 A study in South Africa that investigated ART outcomes in young people attending public sector HIV clinics across two main provinces revealed that young people are more likely to have a detectable viral load 6 months post ART initiation compared with adults.24 The study also found that youth were more at risk of treatment failure when compared with adults.24 The findings of this study contribute to the literature on the intricacies of adolescent HIV care, the risk of adherence relapses and the likelihood of continued challenges with treatment outcomes in this population, which is characterised by social autonomy, increased risk-taking behaviour and a present bias, where immediate gratification, such as a 'drug holiday', is prized over the future long-term consequences of poor adherence.15,25
We postulate that offering more than the traditional biomedical education on the importance of adherence and including mental health in the intervention were significant mediating factors in contributing to adherence behaviour change and observed virological outcomes. Group sessions in the current study not only facilitated improved treatment literacy but also actively encouraged young people to take ownership and participate in their healthcare. Sessions also provided a space where mental health drivers of poor adherence were recognised, and participants were equipped with psychosocial skills to develop coping strategies. Peer support was also available throughout the intervention. Furthermore, the Newlands Clinic model is founded on comprehensive care consisting of a mental and social health service, which provides a context, in which young people experiencing difficulties with adherence can benefit from constant support to maintain adherence behaviour change. This aligns with the theoretical framework of offering youth friendly services, motivational interviewing, and cognitive behavioural therapy to change behaviour.26,27,28 These findings are consistent with the Thai study that showed the potential of an empowerment programme for youth in improving adherence to ART.17
The study results showed that young people who never attended the EACGI showed the lowest rates of suppression on the switched regimen. This finding highlights how, although essential, in the context of treatment failure, a regimen switch may not yield intended suppression results and may potentially increase the risk of drug resistance if adherence difficulties are not addressed. Unsuppressed viraemia in young people on second-line treatment may translate to potential public health consequences, as young people have the highest HIV incident and mortality rates, and the transmission of resistant strains leaves the newly infected with limited treatment options.9,29 This has healthcare costs in low-resource settings as subsequent treatment lines are significantly more expensive.
As already highlighted, group attendance was associated with viral response. Not all adolescents chose or were able to regularly attend sessions. This is reflective of young people's realities where competing factors, such as seeking autonomy, an active social life, and educational and financial responsibilities, contend with HIV care engagement.23,30 Economic considerations in HIV support interventions have previously been described as pivotal for successful HIV management, given the prioritisation of income-generating opportunities that may interfere with attending facility-based interventions.30,31 In their study, they suggest that young people living with HIV (YPLHIV) are mainly from low-resourced communities such as those in the current study and, therefore, it is plausible that income-generating opportunities may interfere with attending facility-based interventions. These findings highlight the importance of offering differentiated adherence interventions. This phenomenon may affect male patients more as observed in this study where fewer male patients attended the EACGI regularly. Group counselling interventions may not always achieve similar results in young men living with HIV, highlighting the need for further research in this area.
There are some differentiated treatment strategies that have been developed to try and improve HIV treatment outcomes in adolescents and young people. Teen clubs are one such model that have achieved mixed outcomes in different settings. These clubs have been rolled out and evaluated in a few treatment programmes around Africa.32 Adolescents receiving care and enrolled in teen clubs in Windhoek, Namibia, did not show improved treatment outcomes compared, with the standard of care.33 Whilst there was marginal improvement in adherence (adjusted odds ratio [aOR]: 1.48, 95% CI: 1.16-1.90, p < 0.01) to ART in a Malawian study utilising teen clubs.32 The introduction of an EACGI, which has shown positive results in the Zimbabwean setting, could very well complement the differentiated models being rolled out for young people requiring adherence support.
The strength of this work was that adherence behaviour change was measured by viral load, an objective clinical marker of adherence and clinical outcomes. The strength of this study's results also lies in the ability to measure viral progression longitudinally in young people after group counselling intervention, which is difficult to conduct in low- and middle-income countries. One of the limitations with this approach is that the observed viral suppression after switching to second-line ART could be as a result of switching to a more potent treatment regimen.
Biomarkers are not the only important factors in making clinical decisions in routine HIV management, especially in key populations.34 This study's findings support these recommendations and provide a possible preliminary framework on support for young people being prepared for a treatment switch post treatment failure.
This study was conducted using routinely collected data where patients were not randomised into groups. Willingness to attend group sessions may have affected the rate of attendance and virological outcomes. The EACGI referrals were initiated by clinicians' judgement and could have introduced a selection bias. However, this is reflective of typical HIV primary care. This study focused on individual-related factors of adherence; yet, adherence is complex with multiple interacting adherence risk factors.31 The EACGI can be included in HIV treatment programmes with the inclusion of trained personnel.
Conclusion
Adherence support interventions, which include a mental health framework such as EACGI, in preparing young adult patients for second-line treatment seems to be a promising tool, increasing the likelihood of improved adherence and treatment outcomes. All participants who attended EACGI were retained in care. This study's findings support the need for further enquiry into rigorous, evidence-based multilevel adherence interventions that are acceptable and effective for diverse young PLWHIV.
Acknowledgements
The authors acknowledge the staff and patients of Newlands Clinic who participated in this study, as well as Radoslaw Panczak for statistical support.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
B.K. contributed to the conceptualisation, literature search, study design and methods, project administration, data extraction, data analysis, data interpretation, writing, tables and figures, and review and editing of the manuscript. T.S. contributed to the literature search, data extraction, data analysis, data interpretation, writing, and review and editing of the manuscript. T.M. contributed to the literature search, data extraction, data analysis, data interpretation, and review and editing of the manuscript. R.L. contributed to the conceptualisation, study design and methods, and review and editing of the manuscript. All authors had full access to all study data and had final responsibility for the decision to submit for publication.
Funding information
This research study did not receive any separate funding. The study was carried out as part of routine clinic work funded by the Ruedi Luethy Foundation.
Data availability
The authors used data from routine clinical care records of patients with HIV stored in an electronic medical record database at Newlands Clinic. Individual de-identified participant data used for this study are available through figshare at https://figshare.com/s/1193817aa9740bcdf441, and the study protocol will be made available upon request via email to the corresponding author's institution (info@newlandsclinic.org.zw).
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated institutions of the authors.
References
1. Bezabhe WM, Chalmers L, Bereznicki L, Peterson G. Adherence to antiretroviral therapy and virologic failure: A meta-analysis. Medicine. 2016;95(15):e3361. https://doi.org/10.1097/MD.0000000000003361 [ Links ]
2. Haas AD, Radin E, Hakim AJ, et al. Prevalence of nonsuppressed viral load and associated factors among HIV-positive adults receiving antiretroviral therapy in Eswatini, Lesotho, Malawi, Zambia and Zimbabwe (2015 to 2017): Results from population-based nationally representative surveys. J Int AIDS Soc. 2020;23(11):e25631. https://doi.org/10.1101/2020.07.13.20152553 [ Links ]
3. Adejumo OA, Malee KM, Ryscavage P, Hunter SJ, Taiwo BO. Contemporary issues on the epidemiology and antiretroviral adherence of HIV-infected adolescents in sub-Saharan Africa: A narrative review. J Int AIDS Soc. 2015;18:20049. https://doi.org/10.7448/IAS.18.1.20049 [ Links ]
4. Lall P, Lim SH, Khairuddin N, Kamarulzaman A. Review: An urgent need for research on factors impacting adherence to and retention in care among HIV-positive youth and adolescents from key populations. J Int AIDS Soc. 2015;18(2 Suppl 1):19393. https://doi.org/10.7448/IAS.18.2.19393 [ Links ]
5. Ferrand RA, Simms V, Dauya E, et al. The effect of community-based support for caregivers on the risk of virological failure in children and adolescents with HIV in Harare, Zimbabwe (ZENITH): An open-label, randomised controlled trial. Lancet Child Adolesc Health. 2017;1(3):175-183. https://doi.org/10.1016/S2352-4642(17)30051-2 [ Links ]
6. Natukunda J, Kirabira P, Ong KIC, Shibanuma A, Jimba M. Virologic failure in HIV-positive adolescents with perfect adherence in Uganda: A cross-sectional study. Trop Med Health. 2019;47:8. https://doi.org/10.1186/s41182-019-0135-z [ Links ]
7. Bernays S, Paparini S, Gibb D, Seeley J. When information does not suffice: Young people living with HIV and communication about ART adherence in the clinic. Vulnerable Child Youth Stud. 2016;11(1):60-68. https://doi.org/10.1080/17450128.2015.1128581 [ Links ]
8. Van Wyk BE, Davids LC. Challenges to HIV treatment adherence amongst adolescents in a low socio-economic setting in Cape Town. S Afr J HIV Med. 2019;20(1):1002. https://doi.org/10.4102/sajhivmed.v20i1.1002 [ Links ]
9. Slogrove AL, Sohn AH. The global epidemiology of adolescents living with HIV: Time for more granular data to improve adolescent health outcomes. Curr Opin HIV AIDS. 2018;13(3):170-178. https://doi.org/10.1097/COH.0000000000000449 [ Links ]
10. Denison JA, Banda H, Dennis AC, et al. 'The sky is the limit': Adhering to antiretroviral therapy and HIV self-management from the perspectives of adolescents living with HIV and their adult caregivers. J Int AIDS Soc. 2015;18:19358. https://doi.org/10.7448/IAS.18.1.19358 [ Links ]
11. Reif LK, Abrams EJ, Arpadi S, et al. Interventions to improve antiretroviral therapy adherence among adolescents and youth in low- and middle-income countries: A systematic review 2015-2019. AIDS Behav. 2020;24(10):2797-2810. https://doi.org/10.1007/s10461-020-02822-4 [ Links ]
12. Cluver LD, Hodes RJ, Sherr L, et al. Social protection: Potential for improving HIV outcomes among adolescents. J Int AIDS Soc. 2015;18(Suppl 6):20260. https://doi.org/10.7448/IAS.18.7.20260 [ Links ]
13. Fairlie L, Karalius B, Patel K, et al. CD4+ and viral load outcomes of antiretroviral therapy switch strategies after virologic failure of combination antiretroviral therapy in perinatally HIV-infected youth in the United States. AIDS. 2015;29(16):2109-2119. https://doi.org/10.1097/QAD.0000000000000809 [ Links ]
14. Cutrell J, Jodlowski T, Bedimo R. The management of treatment-experienced HIV patients (including virologic failure and switches). Ther Adv Infect Dis. 2020;7:1-15. https://doi.org/10.1177/2049936120901395 [ Links ]
15. Marcus R, Ferrand RA, Kranzer K, Bekker LG. The case for viral load testing in adolescents in resource-limited settings. J Int AIDS Soc. 2017;20(Suppl 7):e25002. https://doi.org/10.1002/jia2.25002 [ Links ]
16. MacPherson P, Munthali C, Ferguson J, et al. Service delivery interventions to improve adolescents' linkage, retention and adherence to antiretroviral therapy and HIV care. Trop Med Int Health. 2015;20(8):1015-1032. https://doi.org/10.1111/tmi.12517 [ Links ]
17. Kaihin R, Kasatpibal N, Chitreechuer J, Grimes RM. Effect of an empowerment intervention on antiretroviral drug adherence in Thai youth. Behav Med. 2015;41(4):186-194. https://doi.org/10.1080/08964289.2014.911717 [ Links ]
18. Bhana A, Mellins CA, Petersen I, et al. The VUKA family program: Piloting a family-based psychosocial intervention to promote health and mental health among HIV infected early adolescents in South Africa. AIDS Care. 2014;26(1):1-11. https://doi.org/10.1080/09540121.2013.806770 [ Links ]
19. Shamu T, Chimbetete C, Shawarira-Bote S, Mudzviti T, Luthy R. Outcomes of an HIV cohort after a decade of comprehensive care at Newlands Clinic in Harare, Zimbabwe: TENART cohort. PLoS One. 2017;12(10):e0186726. https://doi.org/10.1371/journal.pone.0186726 [ Links ]
20. Willis N, Milanzi A, Mawodzeke M, et al. Effectiveness of community adolescent treatment supporters (CATS) interventions in improving linkage and retention in care, adherence to ART and psychosocial well-being: A randomised trial among adolescents living with HIV in rural Zimbabwe. BMC Public Health. 2019;19(1):117. https://doi.org/10.1186/s12889-019-6447-4 [ Links ]
21. Chimbetete C. HIV drug resistance and third line treatment outcomes in patients failing: Protease Inhibitor based second-line antiretroviral therapy in Zimbabwe, in Faculty of Medicine. Geneva: University of Geneva, 2020; p. 74. [ Links ]
22. Ho J, Tumkaya T, Aryal S, Choi H, Claridge-Chang A. Moving beyond P values: Data analysis with estimation graphics. Nat Methods. 2019;16:565-566. https://doi.org/10.1038/s41592-019-0470-3 [ Links ]
23. Sithole Z, Mbizvo E, Chonzi P, et al. Virological failure among adolescents on ART, Harare City, 2017 - A case-control study. BMC Infect Dis. 2018;18(1):469. https://doi.org/10.1186/s12879-018-3372-6 [ Links ]
24. Evans D, Menezes C, Mahomed K, et al. Treatment outcomes of HIV-infected adolescents attending public-sector HIV clinics across Gauteng and Mpumalanga, South Africa. AIDS Res Hum Retrovir. 2013;29(6):892-900. https://doi.org/10.1089/aid.2012.0215 [ Links ]
25. Blakemore SJ. Development of the social brain in adolescence. J R Soc Med. 2012;105(3):111-116. https://doi.org/10.1258/jrsm.2011.110221 [ Links ]
26. Lee L, Yehia BR, Gaur AH, et al. The impact of youth-friendly structures of care on retention among HIV-infected youth. AIDS Patient Care STDS. 2016;30(4):170-177. https://doi.org/10.1089/apc.2015.0263 [ Links ]
27. Naar-King S, Earnshaw P, Breckon J. Toward a universal maintenance intervention: Integrating cognitive-behavioral treatment with motivational interviewing for maintenance of behavior change. J Cogn Psychother. 2013;27(2):126-137. https://doi.org/10.1891/0889-8391.27.2.126 [ Links ]
28. Hogan A, Catley D, Goggin K, Evangeli M. Mechanisms of motivational interviewing for antiretroviral medication adherence in people with HIV. AIDS Behav. 2020;24(10):2956-2965. https://doi.org/10.1007/s10461-020-02846-w [ Links ]
29. Kim MH, Mazenga AC, Yu X, et al. High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: Barriers and associated factors. J Int AIDS Soc. 2017;20(1):21437. https://doi.org/10.7448/IAS.20.1.21437 [ Links ]
30. Bermudez LG, Ssewamala FM, Neilands TB, et al. Does economic strengthening improve viral suppression among adolescents living with HIV? Results from a cluster randomized trial in Uganda. AIDS Behav. 2018;22(11):3763-3772. https://doi.org/10.1007/s10461-018-2173-7 [ Links ]
31. Cluver LD, Orkin FM, Campeau L, et al. Improving lives by accelerating progress towards the UN sustainable development goals for adolescents living with HIV: A prospective cohort study. Lancet Child Adolesc Health. 2019;3(4):245-254. https://doi.org/10.1016/S2352-4642(19)30033-1 [ Links ]
32. McBride K, Parent J, Mmanga K, et al. ART adherence among Malawian youth enrolled in teen clubs: A retrospective chart review. AIDS Behav. 2019;23(9):2629-2633. https://doi.org/10.1007/s10461-019-02580-y [ Links ]
33. Munyayi FK, Van Wyk BE. The comparison of teen clubs vs. standard care on treatment outcomes for adolescents on antiretroviral therapy in Windhoek, Namibia. AIDS Res Treat. 2020;2020:8604276. https://doi.org/10.1155/2020/8604276 [ Links ]
34. UNAIDS. 2019-global-AIDS-update. Geneva: Communities at the Centre, 2019; p. 121-138. [ Links ]
 Correspondence:
Correspondence:
Bahati Kasimonje
bahatik@newlandsclinic.org.zw
Received: 05 Aug. 2021
Accepted: 17 Sept. 2021
Published: 29 Oct. 2021














