Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of HIV Medicine
On-line version ISSN 2078-6751
Print version ISSN 1608-9693
South. Afr. j. HIV med. (Online) vol.15 n.4 Johannesburg Dec. 2014
http://dx.doi.org/10.7196/sajhivmed.1050
ORIGINAL ARTICLE
Safety of the surgeon: 'Double-gloving' during surgical procedures
O A ArowoloI; E A AgbakwuruII; G C ObonnaI; C U OnyiaIII; A A AkinkuolieI; J G OlaogunIII
IFWACS; Department of Surgery, Faculty of Clinical Sciences, Obafemi Awolowo University, Ile-Ife, Nigeria
IIFMCS; Department of Surgery, Faculty of Clinical Sciences, Obafemi Awolowo University, Ile-Ife, Nigeria
IIIMBBS; Department of Surgery, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria
ABSTRACT
BACKGROUND: In the face of increasing HIV/AIDS prevalence in subSaharan Africa, we evaluate the effectiveness of 'double-gloving' during surgery as a means of protecting the surgeon operating on patients with a known or unknown HIV status.
METHODS: A prospective study was conducted to determine the rate of glove puncture and intraoperative injury in categories of patients with known positive, known negative or unknown HIV status.
RESULTS: The surgeon and the first assistant double-gloved in all the 1 050 procedures performed between 2009 and 2013, and a total of 8 400 surgical gloves were used. Sixty-nine patients (6.6%) were HIV-positive, 29 patients (2.8%) were HIV-negative, and the HIV status was unknown for the remaining 952 patients (90.7%). The overall glove puncture rate in the study was 14.5%. The glove puncture rate was 0%, 31% and 15% for HIV-positive, HIV-negative and HIV status unknown, respectively, and this difference was statistically significant. The mean operating time in the group with glove punctures was 148 min (95% confidence interval (CI) 135 - 161), while mean operating time in the group without glove puncture was 88 min (95% CI 84 - 92).
CONCLUSION: Double-gloving offers protection against intraoperative injury. Knowing the HIV status of the patient offers additional protection to the operating surgeon. While we recommend routine double-gloving for surgeons working in HIV-prevalent patient populations, we also advocate for the routine screening for HIV in all surgical patients.
Surgical gloves were originally developed to protect the patient from organisms on the physician's hands.[1] Recently, the protection of physicians and other medical personnel from the percutaneous transmission of HIV, hepatitis-B virus and other pathogens by direct contact with infected patients has become a major concern of the medical community.[2-6] Since medical history and examination cannot reliably identify all patients harbouring blood-borne pathogens, universal precautions during exposure to blood and body fluids are now mandatory. Intact surgical gloves can help to prevent HIV transmission, but breaches in glove material may expose operating room staff to risk of infection, particularly if there are cuts or abrasions on the skin. Breached gloves do not only indicate the potential for infection via the skin, but also indicate the possibility of needlestick injury and thus inoculation with infected blood.[6,7]
There have been numerous reports on the rising prevalence of HIV infection in subSaharan Africa, especially in Nigeria. [8,9] The reason for this rising prevalence has partly been due to the widespread use of antiretroviral drugs, which has increased the life expectancy of HIV-infected patients. Stemming from this increasing prevalence, it is expected that more HIV-infected patients will be presenting with conditions needing surgical intervention in the near future, thus increasing the surgeon's exposure to this group of patients. Owing to lack of clear guidelines and comprehensive policy formulation on patients with HIV infection,[8-10] patients undergoing surgery in Nigeria and many other African countries are not routinely screened for HIV. Coupled with this is the lack of a full complement of protective armamentaria against HIV infection for surgeons who are working in low-resource countries such as Nigeria, leaving them more vulnerable to contracting this disease from their patients.
The principle for most practising surgeons in this region is to take full universal precautions while performing surgery on all patients, as if they are already infected with HIV. The problem with this attitude is that taking full precautions when operating on all patients is likely to become a routine exercise that may be taken for granted. It is therefore questionable if the routine application of universal precautions can offer maximum protection to surgeons practising in such an environment. If a patient is known to be HIV-infected, the attending surgeon will definitely take more-than-routine universal precautions while performing surgery.
It is believed that part of the additional precautions to be taken while carrying out surgical operations on patients with HIV/AIDS infection is for the surgeon to 'double-glove' - wear two standard gloves on each hand. While this is common practice, there are few data on the rate of surgical glove puncture while performing surgery on patients of known or unknown HIV status. Several studies have shown that double-gloving protects the surgeon from blood-borne diseases more than a single glove, and this has led to routine use of double-gloving by operating surgeons.[11-13] Studies on the effect of awareness of patient's HIV status on the rate of perforation and puncture of the operating glove during surgery remain sparse. We examined whether awareness of the HIV status of a patient by the operating surgeon affects the glove puncture rate. We also assess the efficacy of double-gloving in preventing glove puncture and perforation injury while operating on patients with or without HIV infection.
Methods
This prospective study was carried out at the General Surgery Unit of Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), comprising the Ife Hospital Unit (IHU) in Ile-Ife, and the Wesley Guild Hospital (WGH) in Ilesha, both in the southwestern region of Nigeria. The hospitals serve as referral centres to the rural and semi-urban agrarian communities in this part of Nigeria, covering a population of ~7.7 million people. The study period spanned a 4-year period from March 2009 to March 2013. With ethical approval from our institutional ethics board, consecutive patients with elective or emergency general surgical procedures were recruited into the study. The patients were not routinely screened for HIV status as part of the study, but where there was clinical indication to do so, patients were screened accordingly. This meant that there were three categories of patients in terms of HIV status: negative, positive and unknown. The HIV status (or lack of knowledge thereof) of the patient was made known to the operating surgeon and all other theatre staff. However, only the surgeon and the first assistant were included in the study. The gloves used in all surgical cases were made of latex, and the surgeon and the assistant double-gloved in all the cases.
After surgery, the used inner and outer gloves were tested separately in accordance with the water-infusion method of the Food and Drug Administration to detect perforation.[7] The gloves were filled with 1 000 mL of water and were suspended from the occluded cuff 5 ft (15.2 m) from the ground. The digits were pressurised differentially when a volume of water was squeezed into each one, and were observed for perforations. With this technique, even minute punctures were detected. In addition, at the end of the surgical procedure, an independent observer inspected the hands of the surgeon and the first assistant for the presence of blood or body fluids as evidence of a break in the integrity of the latex gloves.
Results
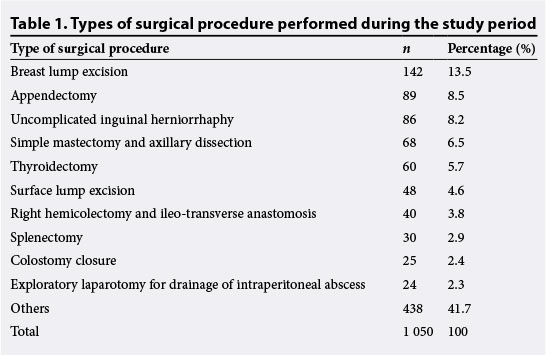
A total number of 8 400 surgical gloves used in 1 050 surgical procedures were analysed. The surgeons double-gloved during all the surgical procedures performed (Table 1). Breast lump excision was the most common surgical procedure, accounting for 142 cases (13.5%). Table 2 outlines the indications and surgical procedures performed on the HIV/AIDS-positive patients. Pyomyositis (n=18 (26%)) and appendicitis (n=10 (14.5%)) were the most common surgical conditions in the HIV/ AIDS patients. As a result, incision, drainage and appendectomies were the most common surgical procedures performed on these patients. Out of the 1 050 patients operated on during the study period, 98 patients were tested for HIV infection based on clinical suspicion, and 69 patients (6.8%) tested positive. The remaining 952 patients (88%) were not tested (Table 3).
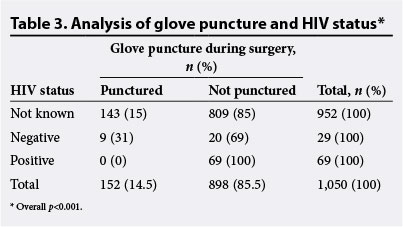
The overall glove puncture rate in this study was 152 (14.5%) across the three groups of patients. In the group of patients who were HIV-infected, no glove puncture was recorded. The glove puncture rate was 9 (0.86%) in the group of patients who tested negative for HIV, and 143 (13.6%) in the group with an unknown HIV status (Table 3); the difference in these rates was statistically significant (p<0.001). The mean operating time in the group with a punctured glove was 148 min (95% confidence interval (CI) 135 - 161), while mean operating time in the group without glove puncture was 88 min (95% CI 84 - 92).
The pattern of glove puncture in the surgeon and assistants' hands is shown in Table 4. The surgeon's left-hand outer glove was the most punctured (n=127), accounting for 12.1% of the total glove punctures recorded in the study. The most common site of glove perforation was on the index finger of the left hand (n=114), accounting for 76% of all perforations recorded. The second most common was the left middle finger (n=11), accounting for 7.3% of total perforations (Table 5).
Discussion
Glove perforation is relatively common during surgery. The overall glove puncture rate per numbers of patients operated upon was 152 (14.5%) (Table 3), while the overall glove perforation observed per total number of gloves used was 197 (18.8%) (Table 4), which is consistent with perforation rates reported in other studies, with the frequency ranging from 18 to 61% during various surgical procedures.[11-14] The rate of glove puncture has been extensively documented in different operative scenarios, including single-gloving and double-gloving.[13,15] The highest frequencies of glove puncture have been reported in orthopaedic, trauma and thoracic surgery; this is likely to be because in these fields the surgeon handles sharp fractured bones or bony structures.[12,16,17] The rate of glove puncture in hand and foot surgery has also been documented.[18,19] Studies on glove puncture rates while operating on HIV-infected patients were largely lacking in the literature. In 1987, the Centers for Disease Control issued guidelines, called 'universal precautions', designed to minimise the risk of transmission of HIV in the healthcare setting.[4] These guidelines are also appropriate for reducing the transmission of other blood-borne infections.[20] However, there are few studies from low- and middle-income countries documenting the rate of glove puncture during surgery when operating on patients with known or unknown HIV status, with universal precautions applied in both settings. As a result, there are no data on the efficacy of universal precautions in preventing glove punctures and HIV transmission in the operating surgery environment, which has recently witnessed an upsurge in the prevalence and incidence of HIV infection.
In this study, the rate of glove puncture while operating on patients with a known preoperative status of HIV-positive was zero (0%), compared with the rates of 143 (13.6%) and 9 (0.9%) in patients with unknown preoperative HIV status and patients with negative preoperative HIV status, respectively. This should be interpreted with caution, bearing in mind the small sample size of HIV-infected patients in this study, which limits statistical power. In most other studies, there has been a relatively small and stable number of HIV-infected patients undergoing surgery.[21-23] However, the prevalence of HIV-infected patients undergoing surgery in Nigeria and many other parts of Africa is expected to increase significantly, because of the efficacy and widespread use of antiretroviral drugs. As HIV-infected patients live longer, more will present in hospital with surgical conditions. In turn, there is need for anticipatory policies that will protect surgeons operating in the environments with high HIV prevalence. That there was no glove puncture while performing surgery in the group of patients who were HIV-infected suggests that awareness of a patient's HIV status may enhance the intraoperative safety of surgeons.
The problem of glove perforation remains a major cause of exposure to contaminated body fluids and is yet to be solved satisfactorily.[24] Our study re-emphasises that double-gloving offers significantly better protection than single-gloving. The outer glove alone was punctured in 119 cases (11.3%), while both gloves were punctured in 29 cases (2.8%). Therefore, in 8.6% of cases, when the outer glove was perforated, the inner glove protected the surgeon's hand from contamination; subsequent visible skin contamination would also be much lower with double gloves. These are similar to observations in other studies.[7,17-19] This study also showed that the majority of glove perforation occurred in the index finger of the left hand, which accounted for 10.9% of total perforation, followed by perforation in the left middle finger (1.6%) and left thumb (1.0%) (Table 5). This has also been reported in similar studies.[7,17-19] The reason for this may be due to the fact that the index finger and the thumb are more actively used during tissue dissection and during hand exploration than other fingers. As the majority of glove perforations go unnoticed, we recommend the routine use of double gloves in all surgical procedures, or where chances of needlestick injury are high.
Conclusion
These data point to the potential benefits of double-gloving during surgery in settings where HIV is prevalent. More generally, we recommend a comprehensive review of policy frameworks that guide surgeons operating in high-HIV prevalence environments, such as Nigeria and other African countries, in order to allow for the routine screening of patients in addition to taking universal precautions, which on their own are not adequate for optimal protection of the surgeon.
References
1. Misteli H, Weber WP, Reck S, et al. Surgical glove perforation and the risk of surgical site infection. Arch Surg 2009;144(6):553-558. [http://dx.doi.org/10.1001/archsurg.2009.60] [ Links ]
2. Sanders R, Fortin P, Ross E. Helfest D. Outer gloves in orthopaedic procedures. Cloth compared with latex. J Bone Joint Surg Am 1990;72(6):914-917. [ Links ]
3. Grady GF. Hepatitis B from medical professions. How rare? How preventable. N Engl J Med 1977;296(17):995-996. [ Links ]
4. Kelen GD, DiGiovanna TA, Celentano DD, et al. Adherence to universal (barrier) precautions during interventions on critically ill and injured emergency department patients. J Acquir Immune Defic Syndr 1990;3(10):987-994. [ Links ]
5. Dxodds RD, Guy PJ, Peacock AM, et al. Surgical glove perforation. Br J Surg 1988;75(10):966-968. [ Links ]
6. Zhang M, Wang H, Miao J, Du X, Li T, Wu Z. Occupational exposure to blood and body fluids among healthcare workers in a general hospital, China. Am J Ind Med 2009;52(2):89-98. [http://dx.doi.org/10.1002/ajim.20645] [ Links ]
7. Thomas S, Agarwal M, Mehta G. Intraoperative glove perforation: Single v. double-gloving in protection against skin contamination. Postgrad Med J 2001;77(909):458-460. [http://dx.doi.org/10.1136/pmj.77.909.458] [ Links ]
8. Adebamowo CA, Ezeome ER, Ajuwon JA, Ogundiran TO. Survey of the knowledge, attitude and practice of Nigerian surgery trainees to HIV-infected persons and AIDS patients. BMC Surg 2002;2:7. [http://dx.doi.org/10.1186/1471-2482-2-7] [ Links ]
9. Owotade FJ, Ogunbodede EO, Sowande OA. HIV/AIDS pandemic and surgical practice in a Nigerian teaching hospital. Trop Doct 2003;33(4):228-231. [ Links ]
10. Adelekan ML, Jolayemi SO, Ndom RJ, et al. Caring for people with AIDS in a Nigerian teaching hospital: Staff attitudes and knowledge. AIDS Care 1995;7(Suppl 1):S63-S72. [ Links ]
11. Yinusa W, Li YH, Chow W, et al. Glove punctures in orthopaedic surgery. Int Orthop 2004;28(1):36-39. [http://dx.doi.org/10.1007/s00264-003-0510-5] [ Links ]
12. Laine T, Aarnio P. How often does glove perforation occur in surgery? Comparison between single gloves and a double-gloving system. Am J Surg 2001;181(6):564-566. [http://dx.doi.org/S0002-9610(01)00626-2. [ Links ]]
13. Na'aya HU, Madziga AG, Eni UE. Prospective randomised assessment of single v. double-gloving for general surgical procedures. Niger J Med 2009;18(1):73-74. [ Links ]
14. Sebold EJ, Jordan LR. Intraoperative glove perforation. A comparative analysis. Clin Orthop Relat Res 1993;297:242-244. [ Links ]
15. Alrawi S, Houshan L, Satheesan R, et al. Glove reinforcement: An alternative to double-gloving. Infect Control Hosp Epidemiol 2001;22(8):526-527. [http://dx.doi.org/10.1086/501947] [ Links ]
16. Driever R, Beie M, Schmitz E, et al. Surgical glove perforation in cardiac surgery. Thorac Cardiovasc Surg 2001;49(6):328-330. [http://dx.doi.org/10.1055/s-2001-19006] [ Links ]
17. Maffulli N, Capasso G, Testa V. Glove perforation in pediatric orthopaedic surgery. J Pediatr Orthop 1991;11(1):25-27. [ Links ]
18. Maffulli N, Testa V, Capasso G. Glove perforation in hand surgery. J Hand Surg Am 1991;16(6):1034-1037. [ Links ]
19. Maffulli N, Testa V, Capasso G. Glove perforation in foot surgery. Foot Ankle 1991;11(4):228-230. [ Links ]
20. Bennett NT, Howard RJ. Quantity of blood inoculated in a needlestick injury from suture needles. J Am Coll Surg 1994;178(2):107-110. [ Links ]
21. Adeolu AA, Malomo AO, Shokunbi MT, Shokunbi WA, Obajimi MO, Komolafe EO. Cranial computed tomographic (CT) findings in HIV-positive Nigerian patients presenting for neurosurgical evaluation. West Afr J Med 2006;25(1):69-74. [ Links ]
22. Cacala SR, Mafana E, Thomson SR, Smith A. Prevalence of HIV status and CD4 counts in a surgical cohort: Their relationship to clinical outcome. Ann R Coll Surg Engl 2006;88(1):46-51. [http://dx.doi.org/10.1308/003588406X83050] [ Links ]
23. Ukponmwan CU, Egbagbe EE, Osahon AI. Prevalence of human immunodeficiency virus in ophthalmic surgical patients. Niger J Clin Pract 2009;12(2):120-123. [ Links ]
24. Nelson JB, Mital, A. An ergonomic evaluation of dexterity and tactility with increase in examination glove thickness. Ergonomics 1995;38:723-733. [ Links ]
 Correspondence:
Correspondence:
A O Adeolu
(arowolodoctor1@yahoo.com)














