Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of HIV Medicine
On-line version ISSN 2078-6751
Print version ISSN 1608-9693
South. Afr. j. HIV med. (Online) vol.15 n.3 Johannesburg Sep. 2014
http://dx.doi.org/10.7196/SAJHIVMED.1065
CASE REPORT
The diagnostic value of lymph node biopsy to detect Castleman's disease
P SomaI; S KaraII
IMB ChB, MSc (Clinical Epidemiology); Department of Physiology, Faculty of Health Sciences, University of Pretoria, South Africa
IIMB ChB; Department of Internal Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
ABSTRACT
HIV is not indicated in the aetiology of Castleman's disease. However, it impacts on the prevalence and natural history of this disease and significantly on the disease progression. Castleman's disease is a uni- or multicentric disease of the lymph node with or without polyclonal proliferation of B-cells. It is a morphologically distinct form of lymph node hyperplasia and is characterised by significant architectural changes in all lymphatic compartments. Histopathologically, the disease is classified into two major subtypes: the hyaline-vascular type and the plasma-cell type. A mixed type is also identified, as there are frequent transitions between the types. The diagnosis of Castleman's disease needs to be made histologically. Treatment modalities include surgery, which is curative for unicentric disease, and systemic therapy, which is needed for multicentric disease. This case highlights the diagnostic value of lymph node excision biopsy in HIV-infected patients.
A 49-year-old male patient presented to our emergency department with a 5-day history of a non-productive cough, fever, chills, shortness of breath and lower abdominal pain with associated nausea and vomiting. His background history was that of longstanding diabetes mellitus and hypertension, but he did not report an HIV diagnosis or antiretroviral use. Upon examination, the patient did not appear chronically ill. His vitals included a blood pressure of 163/73 mmHg, a respiratory rate of 25 breaths per minute and a temperature of 37.5°C. Generalised lymphadenopathy was also detected, especially in the cervical and right axillary areas. The lymph nodes were hard, non-tender, mobile and measured 1 - 2 cm in diameter. Examination of the heart and lungs revealed no abnormalities. Palpation of the abdomen conirmed splenomegaly, suprapubic tenderness and right renal angle tenderness.
Abnormal laboratory findings included haematuria, haemoglobin at 9.2 g/dl (normal range 14.3 - 18.3 g/dl), and microscopic examination of the urine-cultured Klebsiella. An HIV enzyme-linked immunosorbent assay was positive, and the initial CD4+was 233 x 106/l. Three specimens of nasogastric aspirates were negative for tuberculosis. A lymph node biopsy was done and the histological findings confirmed features that were in keeping with early human herpesvirus type 8 (HHV-8)-associated multicentric Castleman's disease. Also present was predominantly sinusoidal vascular proliferation in keeping with Kaposi's sarcoma. In addition, the surrounding lymphoid tissue showed against the background of what appeared to be preceding follicular hyperplasia features of marked folliculolysis, and increased plasmacytoid cells and plasma cells were also seen populating some of the follicles.
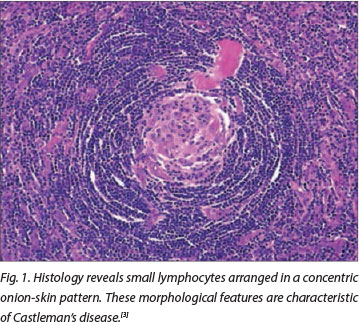
Other features of Castleman's disease included the 'onion skin' arrangement of the surrounding lymphocyte (Fig. 1).
Discussion
Multicentric Castleman's disease (MCD) is an uncommon, aggressive lymphoproliferative disorder with an increased prevalence in people living with HIV.[1] It was first described in a case report by Castleman and Towne in 1954.[2] Classification of disease types is based on histopathological features, and two major subtypes are identiied: the hyaline-vascular type and the plasma-cell type. A mixed type is also identified, as there are frequent transitions between the two types.[3] Based on clinical features, Castleman's disease can be divided into solitary and multicentric types. Common sites for the solitary type are in the mediastinum, neck, lung, mesentery, axillary lymph nodes, peritoneum, soft tissues and nasopharynx, where a mass forms. The dominant histopathological type, in over 90% of cases of the solitary type, is the hyaline-vascular type. The plasma-cell type is found mostly in the multicentric or systemic form of the disease. In the hyaline-vascular type, affected lymph nodes are characterised by follicular and interfollicular vascular proliferation. A wide variety of follicle sizes have been identified, and most of them contain small hyalinised blood vessels that penetrate the germinal centres in an outward concentric fashion from the perifollicular area, giving it the characteristic appearance shown in Fig. 1. Numerous capillaries and cells, especially lymphocytes, admix with some plasma cells, and in rare cases, immunoblasts ill the interfollicular areas. In contrast, in the plasma-cell type, the main features are sheets of plasma cells with large and hyperplastic follicles.[4]
In a study by O'Leary et al.,[5] researchers looked at 16 patients with Castleman's disease and examined the correlation between HHV-8 and Castleman's disease lymph node angiogenesis. Of the study sample, five MCD and two solitary Castleman's disease biopsies were positive for HHV-8. This represented 43% of the patients, a small proportion that may suggest a reactivation of latent HHV-8 infection in patients with Castleman's disease. Detailed analysis confirmed that HHV-8 was identified in 10% of the B-lymphocytes in the endothelial cells and in subcapsular spindle cell proliferations. A mechanism implicated in the pathogenesis of angiogenesis in Castleman's disease is via the production of HHV-8 viral interleukin 6 (IL-6).[5]
To facilitate risk stratification, prognosis and choice of treatment, staging of the disease is recommended. Three crucial aspects need to be addressed: (i) extent of the disease, which can be evaluated by imaging; (ii) the histopathological classification, as this has implications regarding therapy; and (iii) viral aetiology, determined by blood tests to clarify HIV status, serology to establish presence of EpsteinBarr virus, and immunostaining to detect viral IL-6.[3] Even though clinical presentation is usually nonspecific, symptoms fall into four categories: (i) local compression effects caused by enlarged lymph nodes; (ii) systemic symptoms such as fever, weight loss, night sweats, weakness and fatigue caused by B-cell involvement and related cytokine activation; (iii) fluid retention-associated symptoms such as oedema, ascites and pleural effusion; and (iv) clinical features as a result of associated complication, e.g. lymphoma.[3] As a general rule, when local compression symptoms are present, it is likely to be unicentric hyaline-vascular Castleman's disease, while when systemic symptoms are present, multicentric plasma-cell type should be considered.
Specific clinical parameters have been identified by Oksenhendler[6] to increase the rate of diagnosing Castleman's disease in HIV-positive individuals, including fever, diffuse lymphadenopathy, splenomegaly, severe cytopenia, high serum C-reactive protein levels, elevated HHV-8 DNA levels in peripheral blood mononuclear cells, extreme plasmacytosis in lymph nodes or bone marrow, nasal obstruction, respiratory symptoms, Kaposi's sarcoma lesions, a previous similar episode with spontaneous resolution, positive Coombs' test and haemophagocytic syndrome. Castleman's disease is also associated with Kaposi's sarcoma, non-Hodgkin lymphoma, paraneoplastic pemphigus and POEMS syndrome (peripheral neuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin signs).[3]
Modality of treatment is strongly guided by clinical classification, in particular whether a patient has unicentric or multicentric disease.
Unicentric type is usually cured by surgical removal of the affected lymph nodes or local radiotherapy for sites that are unresectable; multicentric disease necessitates systemic therapy.[3] In patients who are HIV-negative, multicentric disease is often symptomatic. The treatment regimen for the HIV-negative group included: (i) treating underlying infection such as HHV-8 (with drugs such as ganciclovir, valganciclovir or foscarnet); (ii) decreasing cytokine acceleration with tocilizumab (a monoclonal antibody that blocks the IL-6 receptor) or corticosteroids (not a popular choice in view of its side-effects); (iii) reducing proliferation of B-cells; and (iv) shrinking tumour mass. Chemotherapeutic agents in combination or single agents such as cyclophosphamide, vinblastine and etoposide can be prescribed for systemic disease.[3]
A study by Mylona et al.[7] illustrated that life expectancy in multicentric disease appears to have improved, with the fatality rate among patients receiving antiretroviral therapy (ART) at 29% compared with the fatality rate of 75% among pre-ART patients. Another significant finding in their study was that patients on ART at the time of diagnosis of MCD had a better immunological profile and were less likely to have concurrent Kaposi's sarcoma than those commencing ART after the diagnosis of MCD was made. Despite the clinical differences between the patients receiving and those not receiving ART, their mortality rates did not vary significantly.[7] The administration of monoclonal antibodies also forms part of treatment options. Rituximab, an anti-CD20 monoclonal antibody, has been tried and a good response has been documented.[1,3,7] The safety of rituximab as a single therapeutic agent demands ongoing studies.[3]
Conclusion
Taking into consideration the high prevalence of HIV in South Africa (SA), a high clinical index of suspicion should be held when patients present with lymphadenopathy accompanied by nonspeciic systemic signs, as this will increase the likelihood of diagnosing Castleman's disease. A critical aspect is careful examination so that diseases with similar clinical presentation are excluded. This case highlights the need for lymph node biopsy especially in our SA setting. As described, MCD can be associated with serious medical conditions; prompt diagnosis is thus essential. More research is needed to establish the optimal therapy for this rare disease, particularly in the context of HIV infection.
References
1. Waterston A, Bower M. Fifty years of multicentric Castleman's disease. Acta Oncol 2004;43(8):698-704. [http://dx.doi.org/10.1080/02841860410002752] [ Links ]
2. Castleman B, Towne VW. Case records of the Massachusetts General hospital; weekly clinicopathological exercises; found by Richard C Cabot. N Engl J Med 1954;251(10):396-400. [http://dx.doi.org/10.1056/NEJM195409022511008] [ Links ]
3. Schulte KM, Talat N. Castleman's disease: A two compartment model of HHV 8 infection. Nat Rev Clin Oncol 2010;7(9):533-543. [http://dx.doi.org/10.1038/nrclinonc.2010.103] [ Links ]
4. Keller AR, Hochholzer L, Castleman B. Hyaline-vascular and plasma-cell types of giant lymph node hyperplasia of the mediastinum and other locations. Cancer 1972;29(3):670-683. [ Links ]
5. O'Leary J, Kennedy M, Howells D, et al. Cellular localisation of HHV-8 in Castleman's disease: Is there a link with lymph node vascularity? Mol Pathol 2000;53(2):69-76. [ Links ]
6. Oksenhendler E. HIV-associated multicentric Castleman disease. Curr Opin HIV AIDS 2009;4(1):16-21. [http://dx.doi.org/10.1097/COH.0b013e328319bca9] [ Links ]
7. Mylona EE, Baraboutis IG, Lekakis LJ, Georgiou O, Papastamopoulos V, Skoutelis A. Multicentric Castleman's disease in HIV infection: A systematic review of the literature. AIDS Rev 2008;10(1):25-35. [ Links ]
 Correspondence:
Correspondence:
P Soma
(prashilla.soma@up.ac.za)














