Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of HIV Medicine
On-line version ISSN 2078-6751
Print version ISSN 1608-9693
South. Afr. j. HIV med. (Online) vol.15 n.3 Johannesburg Sep. 2014
http://dx.doi.org/10.7196/SAJHIVMED.1091
GUIDELINE
Management of mental health disorders and central nervous system sequelae in HIV-positive children and adolescents
R NassenI; K DonaldI; K WalkerI; S ParukI; M VujovicI; W DuncanI; B LaughtonI; B MoosI; B EleyII; A LachmanII; J WilmshurstII
IPanel members. Southern African HIV Clinicians Society
IIReviewers. Southern African HIV Clinicians Society
ABSTRACT
HIV-positive children and adolescents are at increased risk of both central nervous system (CNS) sequelae and mental disorders owing to a number of factors, including the impact of HIV infection on the brain, social determinants of health (e.g. poverty and orphanhood) and psychosocial stressors related to living with HIV. Every effort should be made to identify perinatally HIV-infected children and initiate them on antiretroviral therapy early in life. HIV clinicians should ideally screen for mental health and neurocognitive problems, as part of the routine monitoring of children attending antiretroviral clinics. This guideline is intended as a reference tool for HIV clinicians to support the early identification, screening and management of mental health disorders and/or CNS impairment in children and adolescents. This guideline covers mental disorders (section 1) and HIV-associated neurocognitive disorders (section 2) among children and adolescents.
Untreated perinatally HIV-infected (PHIV) children are at increased risk of central nervous system (CNS) sequelae compared with HIV-infected children who begin antiretroviral therapy (ART) in infancy. HIV invades the developing CNS earlier and with greater severity than observed in adults and with a more rapid progression to death. In addition, patients receiving ART may remain vulnerable to the effects of HIV on the brain because the CNS may be a reservoir for persistent viral replication. Initiation of ART, therefore, does not fully reverse CNS insults, particularly if treatment is not initiated during infancy.[1] Psychosocial stressors, such as poverty, orphanhood and parental illness (physical and mental), experienced by HIV-positive children living in disadvantaged communities place them at further risk of poor educational and mental health outcomes. Furthermore, the onset of adolescence presents new challenges related to adherence issues, the provision of adolescent-friendly clinical environments, academic problems, mental health problems, and sexual and other risk behaviours.[2]
1. Mental disorders among HIV-infected children and adolescents
PHIV children present with high rates of mental disorders that exceed population norms and rates in other chronically ill children.[3]
1.1 Overview of mental disorders in children and adolescents
Prevalence:
- In HIV-positive children, prevalence rates of 25 - 50%
- Most common: attention deficit hyperactivity disorder (ADHD), mood disorders, anxiety disorders, substance use disorders (SUDs) (adolescents)
- Less common: psychotic disorders, bipolar mood disorder
Risk factors:
- Previous AIDS-defining diagnosis, lower intelligence quotient, caregiver psychiatric disorder, parental loss, limit-setting problems
Effects:
- Untreated psychiatric illness may affect ART adherence, and educational and medical outcomes
- Adolescents vulnerable to depression, non-disclosure, school failure/dropout, sexual risk behaviours and SUDs
1.2 Screening for mental disorders
- Accurate diagnosis requires a thorough history, and assessment of the mental state of the child and of the family.
- Collateral information from the educator and/or extended family provides essential additional information.
- The objective is to detect and refer suspected cases of children presenting with mental health disorders for a more comprehensive assessment. The detection of psychosocial dysfunction is important as it may contribute to non-adherence and later treatment failure.[4]
- When screening for mental health problems, remember multiple interacting factors such as those within the child, home, school and external environment, all of which influence emotions/behaviour.
- No brief screening tool has been validated worldwide specifically for the detection of mental health disorders among HIV-positive children and adolescents. Table 1 presents some well-validated screening tools that may be utilised in primary care settings.
- A rapid screen of the commonly occurring mental disorders should be performed at the ART clinic and patients should be referred for a mental health assessment (Tables 2 and 3).
1.2.1 Referral criteria based on mental health screen
Refer or discuss the child with a mental health professional (mental health nurse, psychologist, child psychiatrist, psychiatrist) if the child presents with the following:
- Symptoms of ADHD
- Frequent or daily symptoms of anxiety that have affected functioning at home and at school
- Frequent or daily symptoms of depression/low mood, which have affected functioning at home and at school
- Suicidal ideas, intentions, plans or previous attempts
- Misuse of cannabis, methamphetamine, alcohol or any other illicit substance
- Confusion or change in behaviour/functioning from baseline
Refer or discuss with a social worker if additional information reveals the following:
- Maltreatment of the child (e.g. physical or sexual abuse)
- Adverse socioeconomic circumstances requiring assistance
- Limited or no parental care (child-headed household)
- Substance abuse
1.3 Assessment and diagnosis of mental disorders
Tables 4 and 5 outline the assessment and diagnosis of ADHD and major depressive episodes, respectively.
1.4 Assessment and diagnosis of anxiety disorders
- Anxiety may present in children in a variety of ways (Table 6):
- General symptoms include withdrawal, worries, fears, anticipation of threat and anxiety-themed dreams. These may be associated with vigilance/caution in anticipation of threat and avoidant behaviour.
- Common physical symptoms include nausea and vomiting, headaches and abdominal cramps. Cardiovascular symptoms such as palpitations and dizziness are less common in children.
- Anxieties may be related to worries about the child's illness, the parent/caregiver, school, placement insecurity or the general environment.
- Anxiety disorders that occur more commonly in childhood include separation anxiety disorder, selective mutism and specific phobias.
- Adolescents may additionally present with social anxiety (social phobia) and panic disorder. The clinical presentation may more closely resemble that of adults. Generalised anxiety disorder may occur across the lifespan.[5]
1.5 Assessment and diagnosis of psychotic disorders
Neuropsychiatric symptoms in an HIV-positive child or adolescent include psychosis, severe mood disturbance, delirium or encephalopathy. Psychotic symptoms (hallucinations, delusions, formal thought disorder) and mania are less common among HIV-positive children and adolescents compared with adults, and therefore have a high index of suspicion of a comorbid medical condition such as a CNS disorder.
- Consider a psychotic disorder if there is a positive family history of mental illness, particularly schizophrenia or bipolar mood disorder.
- Suspect delirium if a patient presents with an acute onset of psychotic symptoms associated with confusion and clouding of consciousness that tends to fluctuate. Exclude general medical conditions (GMCs) such as seizures, meningitis, encephalitis, brain tumour or stroke. Failure to recognise delirium may delay the diagnosis of an underlying medical condition and may lead to an adverse outcome and even death.[5]
1.5.1 Delirium
- Delirium is a nonspecific neuropsychiatric disorder that occurs in medically ill patients, signifying global encephalopathic dysfunction. It commonly occurs across the age extremes (the very young and geriatric patients). However, it can occur in all ages, particularly in seriously ill patients with limited cognitive reserves and/or CNS conditions. It is well recognised in the elderly but underdiagnosed in children.
- Onset confers a poorer prognosis for an underlying medical condition.
- The core features comprise an altered level of consciousness, attention disturbances and diffuse cognitive deficits. Symptoms fluctuate and may present with behavioural disturbances (e.g. aggression) and perceptual disturbances, commonly visual hallucinations.
Children who have not been initiated on ART due to adequate CD4+ counts and who have psychiatric symptoms that are poorly responsive to antipsychotics may have detectible/high CNS viral loads despite undetectable serum viral loads (due to differing mutations in cerebrospinal fluid (CSF) and serum). These children should be initiated on ART, which may contribute to the resolution of psychotic symptoms.
Children already on ART who have psychotic symptoms poorly responsive to antipsychotics should be assessed for a comorbid CNS disorder and/or have their ART regimen reviewed and a CNS penetrating regimen considered.[6] The Montreal Cognitive Assessment may be a useful screening instrument to detect cognitive impairment in adolescents.
- https://pdbp.ninds.nih.gov/assets/crfs/MontrealCognitiveAssessment(MoCA)7_1.pdf
- https://pdbp.ninds.nih.gov/assets/crfs/Montreal%20Cognitive%20Assessment%20Scoring%20and%20Instructions.pdf
1.6 Differential diagnoses to consider
- Schizophreniform disorder
- Schizophrenia
- Bipolar mood disorder: usually a history of a previous episode of elevated mood resulting in abnormal behaviour, e.g. decreased sleep, euphoria, hypersexuality, grandiosity and increased energy
- Mood or psychotic disorder secondary to GMC: HIV encephalopathy, seizures, tumours (frontal lobe), side-effect of efavirenz
- Substance-induced psychotic or mood disorder: cannabis, meth-amphetamine
1.7 Mental status examination of the child or adolescent
The mental status examination of a child comprises observation of play, quality of caregiver-child interactions, verbalisations and also interpretation of drawings. The mental state of an adolescent more closely resembles that of an adult patient.
1.7.1 Recording the mental state examination (MSE)
The MSE is an essential part of the psychiatric evaluation. The objective is to describe the child or adolescent's appearance, behaviour, symptoms and cognitive functioning during the examination.
- Physical appearance: age, grooming, clothes, cleanliness, dysmorphic features, bruising, scars
- Behaviour and manner of relating to caregivers and interviewer: eye contact, ability to co-operate, quality of play, interaction with caregiver
- Mood and affect: range, type and appropriateness of affect (objectively euthymic, depressed, elevated)
- Anxiety: fears, separation difficulties, phobias
- Psychomotor behaviour: activity level, tics, co-ordination
- Content and form of thinking: delusions, preoccupations, ruminations, violence, anxiety themes, thought disorder
- Speech and language: fluency, language skills, volume, rate
- Perceptual abnormalities: evidence of hallucinations (e.g. visual, auditory, olfactory)
- Overall cognitive ability: developmentally appropriate behaviour and drawings, general knowledge, vocabulary
- Attention, concentration and memory: attention and concentration, short- and long-term recall
- Level of consciousness: fluctuation, orientation for time, person and place
- Insight and judgement into own condition: acknowledgement of problem, attitude to receiving help, willingness to adhere to treatment, ability to judge hypothetical situations
The child should ideally be interviewed in his/her first language.
1.8 Management of HIV-positive children and adolescents presenting with mental disorders
See Fig. 1, which summarises the assessment and management of HIV-positive children presenting to primary care services.
1.8.1 Risk assessment
- Risk assessment includes evaluation of the following:
- Risk to self: suicidal thoughts or intent or self-harming behaviour; a patient may require hospitalisation in cases of a serious suicide attempt or intent
- Risk to others: thoughts or intention to harm others
- Risk-taking behaviour such as reckless driving, violence, disinhibited sexual behaviour, antisocial behaviour (engaging in unlawful acts) and unprotected sex
- Additional risk to children is related to adverse child care, e.g. minimal parental/family or social support, neglect, physical, emotional or sexual abuse, abandonment.
1.8.2 Referral
- Be aware of referral pathways in your own facility and local district. Communicate with colleagues providing mental health services at primary and district levels, such as a dedicated mental health nurse practitioner, psychiatric registrar, psychologist, occupational therapist and district psychiatrist.
- Have a high index of suspicion for new-onset psychiatric symptoms that may present as a result of an acute or subacute infection or general medical condition, such as AIDS-defining infections, intracranial viral or bacterial infections, and delirious states due to substance abuse/withdrawal/infection or medication.
- Referral for any suspected mental health problems at primary level care should be to a mental health nurse practitioner (or psychiatric registrar, if available). Less severe or uncomplicated cases may be managed at primary level in discussion with the district psychiatrist and mental health team at specialist level.
- Complex cases (e.g. comorbid psychiatric and medical illness such as seizures, other CNS conditions, comorbid substance misuse and psychotic symptoms, catatonia and severe depression) should be referred to the district psychiatrist or specialist child and adolescent mental health (CAMH) services within the catchment area for assessment and possible hospitalisation.
- Refer suspected cases of child abuse to the facility social worker, who may refer to an external social worker for statutory intervention.
- Refer to an occupational therapist at community level, who may do group-based interventions, or adherence groups and functional assessments.
- Refer to the district psychologist for a psychological evaluation of the child and family.
1.8.3 Liaison
- Communicate with the educator and school psychologist (with the family's consent) to obtain accurate information.
- Liaise with relevant adult services if you suspect parent or caregiver mental health problems.
1.8.4 Attitude to family
- Be sensitive and non-judgemental in your attitude.
- Be aware of and attend to issues about stigma.
- Comply with the rules of confidentiality at all times.
1.8.5 Management of depression and anxiety in HIV-positive children and adolescents
- Conduct a thorough history and clinical assessment. This includes information about functioning at school.
- Interview the child/adolescent alone and with the caregiver.
- Initiate first-line psychosocial intervention, i.e. address precipitating or perpetuating stressors, e.g. bullying, stigma. Refer the child for play/individual/group therapy if resources are available and according to the child's intellectual ability; alternatively, refer to the school counsellor. Refer parents to local parenting groups and/or for their own psychological or psychiatric interventions as necessary.
- For moderate to severe symptoms, initiate selective serotonin re-uptake inhibitor (SSRI) in addition to psychosocial management.
- Initiate with a low dose and titrate slowly, preferably with citalopram 5 mg or 10 mg daily, or fluoxetine 5 mg or 10 mg daily if citalopram is not available. (Administer by opening a capsule into 20 ml of orange juice to create a 1 mg/ml solution. Use a 5 ml or 10 ml syringe to measure out the daily dose. Keep the remainder refrigerated.)
Fluoxetine or citalopram may be prescribed for moderate to severe depression and anxiety disorders. Citalopram is preferable because of potential drug-drug interactions between fluoxetine and certain antiretroviral medications. Fluoxetine can increase agitation and impulsivity, so monitor closely.
- Titrate up to the therapeutic dose (as per EDL).
- Monitor adolescents or older children closely for suicidal ideation and SSRI side-effects, e.g. behavioural disinhibition or activation.
- Review in 1 month. Titrate up to 10 - 20 mg (or beyond up to a maximum of 30 - 40 mg) if indicated and if there are no adverse side-effects.
- Reassure the patient and parent that most side-effects are transient and dose related.
- Refer a child with moderate to severe symptoms and with poor response to treatment to a local child psychiatric service if available, or discuss with a psychiatrist (or child psychiatrist if available).
- Treatment for depression should ideally be for 6 - 12 months after symptom resolution, after which the patient may be weaned off medication. Discuss with a mental health professional or child psychiatrist.
- Treatment duration for anxiety disorders is usually 6 - 12 months after symptom resolution. However, treatment duration and discontinuation of medication management should be individualised according to the specific anxiety disorder, severity, recurrence and treatment response. Discuss with a mental health professional or child psychiatrist.
1.8.6 Management of ADHD in HIV-positive children and adolescents
- Conduct a thorough history and clinical assessment. It is important to include all spheres of the child's environment (including home, school and peers).
- Ask the parent and teacher to complete a Connor's or SNAP report.
- Establish baseline weight and height, and calculate and plot body mass index (BMI).
- Initiate psychosocial intervention, including support for parents and teachers, input on positive reinforcement, and establishing structure and routine in the child's day. Refer parents to a local parenting group if available.
- If indicated, initiate stimulant medication. The dosage should be based on the child's age and weight, i.e 1 mg/kg body weight/day.
- In children 6 years and older, start with 5 mg short-acting methylphenidate 2 - 3 times daily (5 mg every 3 - 3.5 hours), e.g. initiate 5 mg at 07h30, 5 mg at 11h00 and 5 mg at 14h30. Increase weekly by 5 - 10 mg, but do not exceed 30 mg daily.
- Alternatively, in older children or adolescents, initiate long-acting methylphenidate 20 mg daily at 07h30, if available.
- Medication should be initiated only after confirmation of the diagnosis by a psychiatry registrar, medical officer or district psychiatrist.
- Use the lowest effective dosage.
- Educate parents about effects and possible side-effects.
There are no known drug-drug interactions between methylphenidate and antiretroviral medications.
- Review the child in one month. Check pulse and blood pressure. If abnormal, do an electrocardiogram (ECG), lower the dosage and continue to monitor. Medication should be discontinued if an ECG abnormality is detected and/or cardiovascular disease is observed. Refer to a cardiologist if a cardiovascular abnormality is detected.
- Assess response to methylphenidate through direct observation and feedback from teachers and parents.
- Assess weight and height and plot BMI at each visit. If there is loss of appetite, encourage the parent to provide additional calories and snacks such as a peanut butter sandwich at night for extra protein. Stop treatment if growth curve flattens or there is significant weight loss >5 kg.
1.8.7 Management of children presenting with psychotic symptoms and/or mania
- Complex cases should ideally be referred for neuropsychiatric assessment and further investigation (including CNS investigation and neurocognitive testing) at a tertiary-level service.
- Behaviourally disturbed psychotic adolescents should be referred for admission.
- Exclude delirium before considering a primary psychotic illness. Investigations such as chest X-ray, full blood count, temperature, pulse and urine dipsticks can be used to screen for delirium before referring to secondary level for further investigations such as lumbar punctures and/or neuroimaging.
- Antipsychotics may be initiated at low doses, but with caution and after discussion with a psychiatrist. Initiate risperidone 0.5 - 1 mg daily and increase the dose by 0.25 - 0.5 mg daily every 1 - 2 weeks, depending on tolerance and age of the child. Refer for admission to tertiary CAMH or psychiatric unit if doses in excess of 3 mg are required.
1.8.8 Medication management
- Do not prescribe psychotropic medication to children or adolescents if there is diagnostic uncertainty and/or there has not been a thorough psychiatric assessment and consultation with a specialist.
- It is important to be cautious about the use of psychotropic medications in the management of behaviour disorders in the context of HIV because of high pill burden and potential drug interactions. If medications are not seen to be working, they should be discontinued and polypharmacy should be avoided.
- Initiate at lower doses and increase slowly. Monitor for untoward side-effects.
- Be aware of drug-drug interactions between certain antiretroviral and psychotropic medications (particularly SSRIs) (Table 7).
- Be aware of neurological and psychological side-effects of some antiretroviral medications.
1.8.9 Other diagnoses or symptomatology to consider as part of the assessment and management of HIV-positive children and adolescents
1.8.9.1 Suicide
- Definition: deliberate self-harm where the intention is to die.
- A suicide risk assessment is essential in the assessment of all patients with HIV presenting with psychiatric symptoms such as depression, anxiety, psychosis or self-harming behaviour.
- Suicide attempts in children and adolescents may be impulsive and often related to an intercurrent stressor, which may not always be severe. However, the outcome may be fatal.
Suicide risk assessment
High suicide risk is indicated by any one or more of the factors below:
- Previous suicide attempt
- Pre-existing mental illness
- Family history of suicide
- Substance abuse
- Gender (adolescent males are at increased risk of completed suicide; adolescent females make more suicide attempts)
The following may further contribute to risk:
- Stressful life events
- Physical and sexual abuse
- Poor parent-child communication
Management of suicidal ideation
- Assess suicide risk severity.
- Screen for and treat underlying mental illness, especially depression.
- Develop a safety plan in collaboration with the patient and family.
- Consider hospitalisation if assessment indicates high risk.
- Do not discharge without an adequate psychiatric evaluation if high risk.[7]
1.8.9.2 Management of trauma-related disorders in children and adolescents with HIV
- Psychosocial counselling and support strategies include compassionate early debriefing, family support and psychoeducation.
- Psychotherapy: cognitive behaviour therapy is useful.
- Medication such as SSRIs may be indicated if there is a poor response to treatment or severe symptoms.
- Check for alcohol and substance abuse in older adolescents.
- Refer to specialist care if there is a poor response to treatment.[8,9]
Post-traumatic stress disorder
- Post-traumatic stress disorder (PTSD) can occur when a person has experienced, witnessed or been confronted with an event that involves actual or threatened death, harm or injury, to themselves or to others, with resultant shock, fear, helplessness or horror.
- The prevalence of PTSD in adolescents living with HIV is not known, but studies report a prevalence range of 15 - 64% in adult samples, suggesting that PTSD may also be common in adolescents.[9]
- Children may have significant symptoms of PTSD but may not meet full Diagnostic and Statistical Manual of Mental Disorders (5th edition) (DSM-V) criteria (Table 8), as they may have difficulty verbalising their emotions.
1.8.9.3 Adjustment disorders
- An adjustment disorder is the development of a behavioural or emotional response to an identifiable stressor within 3 months of the stressor, resolving within 6 months of termination of the stressor.
- Patients may present with depressive, anxiety and/or behavioural symptoms but do not meet criteria for depression, anxiety or disruptive behaviour disorders.[4]
- Treatment for adjustment disorders includes supportive psychotherapy and improving coping mechanisms. Short-term medication may be considered.
- Children and adolescents with HIV in Africa often have multiple psychosocial challenges/stressful life events that make them more emotionally vulnerable and isolated.[10]
- The effect of the virus is thus compounded by negative life events that further negatively affect neurocognitive development.
Common stressful life events for HIV-positive children
- Ill caregiver who cannot cope with parenting
- Death of caregiver
- Multiple caregivers or child-headed households
- Sick siblings
- Poverty
- Multiple hospital visits
- Disrupted schooling
- Disclosure issues
- Stigma
Grief and bereavement
- Children may lose one or both parents to AIDS and are then often separated from siblings and moved about in an attempt to continue to provide for their basic physical needs.
- These children are often left fearful and anxious or confused.
- In addition, HIV-positive children may have fears about their own mortality.
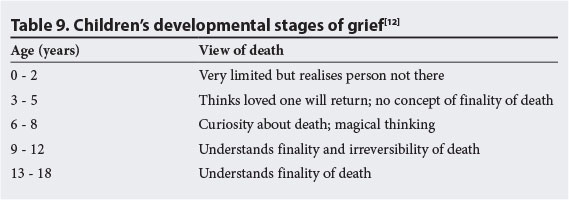
- It is important that children be allowed to express their grief. Grief reactions are influenced by the child's developmental age and coping mechanisms (Table 9).
- Very young bereaved children may experience regression such as thumb sucking, have nightmares or become clingy. They may also present with acting-out behaviours.
- Bereavement in older children may present with aggressive or impulsive behaviour, poor performance at school, and/or poor concentration or emotional outbursts.[11]
- Supportive therapy/counselling at a develop-mentally appropriate level of the child and family is the mainstay of treatment.
1.8.9.4 The disruptive and aggressive child and adolescent
- A high prevalence of challenging or disruptive behaviours exist in HIV-positive children and adolescents, including ADHD, ADHD-like impulsivity and hyperactivity, aggression, oppositionality and conduct disturbances.[2]
- However, aggression and disruptive behaviours may arise from medical problems in the child or adolescent, or may be a manifestation of a mood or anxiety-related problem.
- Adolescents in particular struggle with mood and behavioural regulation.
- There is no direct link between HIV itself and disruptive behaviour. Factors such as poverty, prenatal alcohol and drug exposure, malnutrition, family disruption, social chaos and educational deprivation may play a role.
- There is a further association between behaviour disorders and high rates of neurocognitive and neurodevelopmental delay in HIV-positive children.
- Two disorders that require specific consideration are conduct disorder and oppositional defiant disorder.
Conduct disorder
Definition: a repetitive and persistent pattern of behaviour that violates the basic rights of others or where major age-appropriate societal norms or rules are transgressed (Table 10).[5]
Oppositional defiant disorder
- Definition: a pattern of argumentative/defiant behaviour and angry/irritable mood or vindictiveness lasting at least 6 months.
- Classification requires exhibition of at least four symptoms from any of the categories in Table 11 during an interaction with at least one individual who is not a sibling.[5]
Common co-occurring disorders in children with disruptive or aggressive behaviour
Aggressive and disruptive behaviour may present with co-occurring difficulties such as:
- ADHD
- Learning disorders and language difficulties
- Intellectual disability
- Anxiety and depressive disorders
- Adjustment disorders
- Substance use disorders
- Trauma-related disorders
- Disruptive mood dysregulation disorder
- Bereavement
- Epilepsy
- Sensory integration difficulties
- Delirium (may be secondary to opportunistic infection or a medication)
- Psychotic disorders
Management of behaviour problems in children and adolescents with HIV
- Explore the family's circumstances, particularly parenting practices and harsh discipline.
- Obtain information from the school and/or recent report cards and any other structures that might be involved with the child or the family (e.g. social services, justice).
- Establish an alliance with the child and his/her parent/caregiver; try not to get drawn into the anger and power struggle that often arises out of the child's behaviour.
- Optimise the management of HIV; ensure adherence to antiretroviral medication, establish extent of health and viral suppression and ensure that no intercurrent opportunistic infections have arisen.
- Manage co-occurring problems. These may be more responsive to treatment and addressing them may improve the behavioural 'dyscontrol', i.e. aggression, impulsivity and risk-taking behaviours.
- Address learning and educational problems. This may necessitate more formal psycho-educational assessment and/or referral to local educational authorities, and may be as simple as establishing contact with the school and its support structures.
- Refer to social services if there are concerns of neglect or maltreatment, child-headed households, poverty, household instability or parental illness.
- Encourage participation in prosocial activities and environments in the local community (e.g. sports and cultural activities).
- Psychotropic medication may prove useful, but is seldom the only solution in addressing behaviour disorders in HIV-positive children. Medications are often more successful in treating comorbid problems, e.g. methylphenidate for ADHD, anticonvulsants (sodium valproate, lamotrigine and carbamazepine) for epilepsy, SSRIs for anxiety and depression.
- Seek supervision and get support from your colleagues; working with these children and their families can be demoralising and frustrating.
Management of conduct disorder and oppositional defiant disorder in HIV-positive children and adolescents
- Assess family functioning and parenting, and establish that the child not been maltreated (physical, emotional or sexual abuse or neglect).
- Refer family to a parenting support group or parenting skills training.
- Refer for individual and/or group psychological intervention, depending on the intellectual capacity of the child or adolescent, his/ her capacity to engage in relationship and motivation to participate.
- Risperidone may be useful in reducing aggression and impulsivity, but will need to be carefully monitored for the occurrence of EPSE. A dose of 0.5 - 1 mg/day, with a maximum dose of 1 - 2 mg daily, is recommended. Discuss with a mental health professional if there is a poor response to the maximum dosage.
- Mood stabilisers may be used to aid behavioural management and affective dysregulation associated with behaviour disorders. These should ideally be prescribed by a specialist and monitored carefully.
1.8.10 Psychological interventions
1.8.10.1 Psychosocial support for children
- Psychosocial support can be understood as any type of initiative that seeks to protect or promote the well-being of a child or adolescent, and prevent or treat mental health problems.
- It should form part of a broad framework of care that includes the family, parents, school and community, and that encompasses a range of interventions combined to achieve the best possible outcomes. The provision of psychosocial support involves a range of stakeholders: caregivers, family members, teachers, and healthcare providers including psychological and social services.
- Psychosocial support includes the provision of individual counselling, the availability of facility- and community-based support groups, parenting programmes and peer support initiatives, and information and education workshops.[12]
- To be effective, psychosocial intervention should be tailored to the context and take into account the child's age and stage of development. It is essential that there is focus on enabling an HIV-positive child to establish their identity, manage their care, live positively, cope with challenges and work towards a healthy future.
- HIV-positive children are particularly vulnerable to psychological and social stressors that can affect their development and well-being. Psychosocial support can foster resilience, enabling children and adolescents to bounce back from adverse experiences and to cope better with the multiple stressors related to HIV. Their unique psychosocial needs include assistance to deal with their illness, help to cope with loss and changes of caregiver, and support to overcome isolation associated with stigma and discrimination.[12-14]
1.8.10.2 Therapeutic support
Psychosocial intervention can take various forms including referral to support groups, psychotherapy or counselling (Table 12).[15]
1.8.10.3 Psychosocial support for adolescents
- Interventions for adolescents fall into three categories: therapeutic support, youth-centred interventions and those aimed at fostering independence.
- In the case of the former, support groups, counselling and psychotherapy provide support across a broad range of issues (Table 13).[15]
- Group-based interventions are attractive to the adolescent and are a time- and cost-effective method of delivery.[15]
1.8.10.4 Benefits of group interventions for adolescents
- Enhance self-knowledge and self-acceptance.
- Empower individuals to make change.
- Help individuals to develop coping skills.
- Build communication skills and help in relationships outside of the group.
- Give individuals freedom to express negative feelings in a safe, non-judgemental environment.
- Provide positive reinforcement and emotional support.
- Provide a platform for education, e.g. adherence to treatment.
- Foster a sense of belonging to counter feelings of isolation and inadequate social support.
1.8.11 Youth-centred interventions
- An important aspect of adolescent service provision is ensuring that it is youth friendly.
- Adolescent and Youth-friendly Service (AYFS) provision has been identified as an important aspect of service delivery in South Africa, and has a strong focus on attracting and retaining young people for ongoing care.
- Adolescents are particularly vulnerable to the harmful outcomes of risk behaviours, e.g. unprotected sex and substance abuse, but tend not to seek early treatment. There are a number of reasons for this, such as worry about stigma or fear of harsh treatment at the clinic.
- Paying attention to the health needs of adolescents is crucial. As young people become more independent, they are expected to take more responsibility for their own health. Knowing where and when to get help and feeling confident that they can rely on a service that they trust and feel is there for them is fundamental to a positive outcome.[16]
- A package of services should be available to meet the diverse needs of young people.
- It is important to address obstacles that commonly inhibit the use of healthcare services by adolescents.
1.8.11.1 Overcoming obstacles to providing AFYS
- Providers should be trained to work competently and respectfully with adolescents.
- Services must be confidential, non-judgemental and private.
- Clinic hours should be convenient for young people, e.g. after school.
- Services should be accessible to all adolescents and young people, irrespective of their age, sexual orientation or marital status.
- An effective referral system should be in place.
- Opportunities should be made available for young people to be involved in the design, implementation and evaluation of the programme.
- Services should seek to involve and gain the support of those important in the lives of young people and in their communities, e.g. partners, parents, school.[16]
1.8.12 Adherence in adolescents
- Helping adolescents to achieve independence is important particularly for those transitioning to adult services.
- Part of taking increased responsibility for their healthcare involves adhering to the prescribed treatment regimen.
1.8.12.1 Improving adherence in adolescents
- Poor adherence is normal in adolescence, but the risk of drug resistance, limited treatment options, increased viral load and risks to survival mean that adherence needs to be well supported.
- Reasons for poor adherence among adolescents can be categorised into patient, treatment and socioeconomic factors.
- Stressful life events can contribute to poor adherence, as can treatment fatigue, substance abuse and mental health problems such as depression.
- Psychosocial support in the form of counselling, referrals and group participation can help young people who are finding adherence difficult. Counselling provides opportunities to develop jointly a workable treatment plan that includes treatment reminders and takes into account lifestyle issues that have the potential to interfere with adherence if not addressed.
- Ideally, adolescents should know their HIV status. Adolescents who have not been disclosed to will be unable to appreciate the importance of adherence to treatment and are less likely to understand the risks associated with engaging in unprotected sex. This makes status disclosure an important aspect of care and support.[19]
2. HIV-associated neurocognitive disorders
2.1 Neurocognitive sequelae
- In untreated children, cognitive impairment occurs early and progresses over time, with prevalence rates ranging between 8% and 60%.
- Early invasion of the developing fetal and infant brain is believed to result in the most common primary HIV-related CNS complication, HIV encephalopathy (HIVE), which refersto the disease, damage or malfunction of the brain caused by HIV. This complication can be present before significant immunosuppression. However, its presence in a child infected with HIV constitutes an AIDS-defining illness, reflecting the severity of the condition.
2.1.1 Prevalence and impact of HIV-associated neurocognitive disorders (HANDs) in children
Prevalence:
- In untreated HIV-positive children, 8 - 60% experience cognitive impairment; disorder occurs early and progresses over time.
- Untreated HIV increases risk of CNS sequelae.[17,20,21]
Impact:
- A range of cognitive deficits occur, cognitive scores clustering in low average to borderline range for intellectual functioning.
- Although cognitive functioning improves after ART initiation, scores remain lower than population norms, with poorer academic performance and persistence of language (e.g. verbal fluency), memory, processing speed, visuospatial and attention problems or deficits. Remedial educational interventions are important.[18,22,23]
- Psychosocial stressors (poverty, orphanhood, parental physical/ mental illness or loss) negatively affect adherence, educational and mental health outcomes.
- The concept of a milder form of neurocognitive disturbance in HIV-positive children, such as the adult condition of HAND is recognised but is yet to be defined in children and adolescents. This condition may have significant effects in functional terms on a child's learning potential.[24]
- Many HIV-positive children receiving ART function within normal limits compared with uninfected peers, but a subset with CNS disease follow a distinct pattern of low average cognitive functioning.
- The cognitive deficits in these children may be a result of ongoing viral replication in the brain despite virological control in the periphery or from residual effects of static HIV-1 CNS disease.
- Although HIV-positive children receiving highly active antiretroviral therapy appear to exhibit global measures of intelligence comparable with their uninfected peers, deficits may be present in specific areas such as executive functioning and working memory. Deficits in these areas can impact significantly on learning.
- Children with HAND may demonstrate few clinical signs, but an index of suspicion should be aroused when history reveals delayed motor milestones and when school reports describe school difficulties.
Centers for Disease Control and Prevention: HIV encephalopathy criteria for classification[25]
Must include at least one of the following for at least 2 months in the absence of a concurrent illness:
- Failure to attain or loss of developmental milestones or loss of intellectual ability, verified by standard developmental scale or neuropsychological tests
- Impaired brain growth or acquired microcephaly evident by head circumference measurements or brain atrophy demonstrated by computed tomography or magnetic resonance imaging; serial imaging is required for children <2 years of age
- Acquired symmetric motor deficit manifested by two or more of the following: paresis, pathological reflexes, ataxia or gait disturbance
2.2 Specific neuropsychological deficits
- Neuropsychological testing reveals that executive functioning deficits might be an early indicator of cognitive problems, with deficits in mental processing, sequential processing, comprehension, memory, visuospatial and time orientation tasks.
- One or more of the following must be met for diagnosis of HAND:
- A significant drop in cognitive test scores, but generally still above the delayed range, with or without mild brain imaging abnormalities, with no loss of previously acquired skills and no apparent functional deficits (adaptive behaviour and school performance stable)
- Cognitive test scores in the borderline range, with no significant functional deficits (and no history of significant drop or previous testing)
- Cognitive test scores within normal limits (low average range or above) with no significant functional deficits and moderate to severe brain imaging abnormalities consistent with HIV-related changes
- Abnormal neurological findings but not significantly affecting function.[26]
- Deficits suggestive of frontal lobe dysfunction (e.g. attention, processing speed, motor speed and visuomotor integration) are also detectible in HIV-positive children and adolescents.
- Educational interventions to address these problems are essential to improve the overall health literacy (and adherence) in infected youth as they age and assume greater treatment responsibility.
- Children infected with HIV presenting with cognitive problems may be slow to process information, slow to complete tasks or may be clumsy, and this may affect everyday living. Understanding cognition in children is compounded by the fact that developmental milestones with regard to motor function, co-ordination and the elements of cognition occur at various stages in the development of a child. Screening tools used in adults such as the International HIV Dementia Scale in their current form are thus inappropriate in children and adolescents, as each tool must accommodate the different developmental stages from childhood through to adolescence.
Cognition refers to a group of mental processes that include attention, memory, producing and understanding language, learning, reasoning, problem-solving and decision-making.
2.3 Identification and management of neurocognitive disorders
- Prevention of HIVE, HAND and AIDS-defining conditions via early ART remains the cornerstone of effective management. ART has dramatically decreased the prevalence of HIVE in the US from 35 - 50% to <2%.[27]
- Furthermore, early initiation of ART results in improved neurodevelopmental outcomes compared with deferred initiation.
- Ensuring adherence and providing treatment support are key factors in management.
- A multidisciplinary, tiered approach is recommended for the management of neurocognitive complications (Table 14).
- Referral for pure neurocognitive decline should immediately be to a paediatrician/physician, according to the age of the child.
- However, concern about contributing mental health/behavioural issues may require psychiatric review.
- If cognitive impairment develops once a child is receiving ART, check viral load and adherence.
- If a child's milestones are deteriorating or if an older child has educational or behaviour problems, and there is no obvious explanation, the child should be referred for further evaluation even if HIV infection is well suppressed.
- Treatable conditions can be diagnosed at a primary healthcare level; routine history, examination and blood tests assist in this regard (Table 15).
- Exclude indirect complications of HIV infection such as opportunistic infections (tuberculous meningitis, cytomegalic virus infection), and intrauterine exposure to alcohol and substances.
- Identify environmental and socioeconomic deprivation (orphans, poverty, malnutrition), as this may further affect cognition.
- If other factors (e.g. behavioural, acute illness, other infection) may possibly explain the drop in scores or low cognitive functioning, do not classify as HAND or encephalopathy; re-evaluate at a later stage.
2.3.1 Screening tools to detect neurocognitive impairment
- No international validated screening tools are available to test HIV-positive children for neurocognitive impairment.
- However, screening tools can be helpful in identifying children at risk for developmental problems. Examples of simple tools that can be used are available to download online (http://www.sahivsoc.org/topics?page=1¤tFilter=Mental%20Health). These include a tool for children younger than 5 years and another for schoolgoing children. These tools have not been validated, but together with the Road to Health Developmental Check List (RTHDCL) may provide local tools for use at primary and secondary level care.
- We recommend that all children be screened 6-monthly and more formally at 3 - 4 years and again at 5 - 6 years. This, together with the RTHDCL, should enable flagging of children with potential problems. Early detection of problems paves the way for interventions that would improve the quality of life of these children.
- Screening should occur in the context of general HIV clinics across all levels of healthcare.
- Screening needs to include a history, formal systemic examination and particularly a neurological examination (at least head circumference and motor examination, deep tendon reflexes and gait assessment).
- Any child with delayed developmental milestones should be referred for further assessment.
- It is important to identify contributing factors that can be managed, e.g. nutritional, emotional, poverty and deprivation factors, among others.
Conflict of interest. All expert panel members have completed and submitted conflict of interest disclosure statements. Disclosure information represents the previous 3 years (updated 3 September 2014) and includes relationships with pharmaceutical companies and medical aids: A Lachman reports receiving honoraria from Cipla Medpro and Lilly for speaking engagements; R Nassen reports receiving an honorarium from AstraZeneca for a speaking engagement. All other panel members report no conflict of interest.
Acknowledgement. This work was supported and funded by the Southern African HIV Clinicians Society through unrestricted educational grants.
References
1. Donald K ,Walker K, Riordan G, et al. Neurological complications of HIV/AIDS in childhood. Continuing Medical Education 2011;29(4):156-159. [ Links ]
2. Mellins CA, Malee K. Understanding the mental health of youth living with perinatal HIV infection: Lessons learned and current challenges. J Int AIDS Soc 2013;16:18593. [http://dx.doi.org/10.7448/IAS.16.L18593] [ Links ]
3. Gadow K, Angelidou K. Longitudinal study of emerging mental health concerns in youth perinatally infected with HIV and peer comparisons. J Dev Behav Pediatr 2012;33(6):456-468. [http://dx.doi.org/10.1097/DBP.0b013e31825b8482] [ Links ]
4. Lowenthal E, Lawlerc K, Hararic N, et al. Rapid psychosocial function screening test identified treatment failure in HIV+ African youth. AIDS Care 2012;24(6):722-727. [http://dx.doi.org/10.1080/09540121.2011.644233] [ Links ]
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington, VA, USA: American Psychiatric Publishing, 2013. [ Links ]
6. Canestri A, Lescure F, Jaureguiberry S, et al. Discordance between cerebral spinal fluid and plasma HIV replication in patients with neurological symptoms who are receiving suppressive antiretroviral therapy. Clin Infect Dis 2010:50(5):773-778. [http://dx.doi.org/10.1086/650538] [ Links ]
7. American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with suicidal behaviour. J Am Acad Child Adolesc Psychiatry 2001;40(7 Suppl):24S-51S. [ Links ]
8. Kelly B, Raphael B, Judd F, et al. Posttraumatic stress disorder in response to HIV infection. Gen Hosp Psychiatry 1998;20(6):345-352. [ Links ]
9. Safren SA, Gerhung BS, Hendriksen E. Symptoms of posttraumatic stress disorder and death anxiety in persons with HIV and medication adherence difficulties. AIDS Patient Care STDS 2003;17(12):657-664. [http://dx.doi.org/10.1089/108729103771928717] [ Links ]
10. Sherr L. Young children with HIV/AIDS: Mapping the field. Working paper 33 in early childhood development. The Hague, Netherlands: Bernard Van Leer Foundation, 2005. [ Links ]
11. Sherr L, Mueller J. Where is the evidence base? Mental health issues surrounding bereavement and HIV in children. J Public Ment Health 2009;7(4):31-39. [ Links ]
12. Oneill JF, Selwyn PA, Schietinger H, eds. A clinical guide to supportive and palliative care for HIV/AIDS. Washington, DC: US Department of Health and Human Services, 2003. [ Links ]
13. Department of Health South Africa. Psychosocial Support for Children and Adolescents Infected and Affected by HIV Pretoria: Department of Health, 2012. [ Links ]
14. Anesathasan A, Mcleary-Sills J, Vujovic M, et al. Foundation for the Future: Meeting the Psychosocial Needs of Children Living with HIV in Africa. Arlington, VA: USAID's AIDS Support and Technical Assistance Resources, AIDSTAR-One, Task Order 1, 2011. [ Links ]
15. Cheng K. Psychotherapeutic interventions. In: Cheng K, Myers KM, eds. Child and Adolescent Psychiatry: The Essentials. Philadelphia: Lippincott, 2005:439-457. [ Links ]
16. International Planned Parenthood Federation. Keys to Youth-friendly Services: Celebrating Diversity. London: IPPF, 2011. [ Links ]
17. Van Rie A, Harrington PR, Dow A, Robertson K. Neurologic and neurodevelopmental manifestations of pediatric HIV/AIDS: A global perspective. Eur J Paediatr Neurol 2007;11(1):1-9. [http://dx.doi.org/10.1016/j.ejpn.2006.10.006] [ Links ]
18. Walker SY, Pierre RB, Christie CDC, Chang SM. Neurocognitive function in HIV-positive children in a developing country. Int J Infect Dis 2013;17(10):e862-867. [http://dx.doi.org/10.1016/j.ijid.2013.02.014] [ Links ]
19. Williams P, Storm D, Montepiedra G, et al. Predictors of adherence to antiretroviral medications in children and adolescents with HIV infection. Pediatrics 2006;118(6);e1745-1757. [http://dx.doi.org/10.1542/peds.2006-0493] [ Links ]
20. Laughton B, Cornell M, Grove D, et al. Early antiretroviral therapy improves neurodevelopmental outcomes in infants. AIDS 2012;26(13):1685. [http://dx.doi.org/10.1097/QAD.0b013e328355d0ce] [ Links ]
21. Abubakar A, Van Baar A, Van de Vijver FJ, Holding P, Newton CR. Paediatric HIV and neurodevelopment in sub-Saharan Africa: A systematic review. Trop Med Int Health 2008;13(7):880-887. [http://dx.doi.org/10.1111/j.1365-3156.2008.02079.x] [ Links ]
22. Cooper ER, Hanson C, Diaz C, et al. Encephalopathy and progression of human immunodeficiency virus disease in a cohort of children with perinatally acquired human immunodeficiency virus infection. Women and Infants Transmission Study Group. J Pediatr 1998;132(5):808-812. [ Links ]
23. Laughton B, Cornell M, Boivin M, Van Rie A. Neurodevelopment in perinatally HIV-infected children: A concern for adolescence. J Int AIDS Soc 2013;16:18603. [http://dx.doi.org/10.7448/IAS.16.L18603] [ Links ]
24. Donald KA, Hoare J, Eley B, Wilmshurst JM. Neurologic complications of pediatric human immunodeficiency virus: Implications for clinical practice and management challenges in the African setting. Semin Pediatr Neurol 2014;21(1):3-11. [http://dx.doi.org/10.1016/j.spen.2014.01.004] [ Links ]
25. Centers for Disease Control and Prevention. 1994 Revised Classification System for HIV Infection in Children Less than 13 Years of Age. Atlanta, G, USA: Centers for Disease Control and Prevention, 1994;443(RR12):1-10. [ Links ]
26. Clifford DB, Ances BM. HIV-associated neurocognitive disorder. Lancet Infect Dis 2013;13(11):976-986. [http://dx.doi.org/10.1016/S1473-3099(13)70269-X] [ Links ]
27. Patel K, Ming X, Williams PL, Robertson K, Oleske J, Saege GR. Impact of HAART and CNS-penetrating antiretroviral regimens on HIV-encephalopathy among perinatally infected children and adolescents. AIDS 2009;23(14):1893-1901. [http://dx.doi.org/10.1097/QAD.0b013e32832dc041] [ Links ]
28. Walker SP, Wachs TD, Grantham-McGregor S, et al. Inequality in early childhood: Risk and protective factors for early child development. Lancet 2011;378(9799):1325-1338. [http://dx.doi.org/10.1016/S0140-6736(11)60555-2] [ Links ]
29. Stein A, Desmond C, Garbarino J, et al. Predicting long-term outcomes for children affected by HIV and AIDS: Perspectives from the scientific study of children's development. AIDS 2014;28(Suppl 3):S261-S268. [http://dx.doi.org/10.1097/QAD.0000000000000328] [ Links ]
 Correspondence:
Correspondence:
R Nassen
(rnassen@sun.ac.za)
Disclaimer. Specific recommendations provided here are intended as only a guide to clinical therapy, based on expert consensus and best current evidence. Treatment decisions for patients should be made by their responsible clinicians, with due consideration for individual circumstances. The most current version of this document should always be consulted.














